Trait Anxiety and Unhealthy Eating in Adult Women: The Mediating Role of Cognitive Instability
Abstract
1. Introduction
1.1. Emotional State and Unhealthy Eating
1.2. Impulsivity and Unhealthy Eating
1.3. The Objective of the Present Study: Impulsivity, Anxiety, and Unhealthy Eating
2. Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Trait Anxiety
2.2.2. Unhealthy Eating (Eating Behaviors)
2.2.3. Cognitive Impulsiveness Component: Cognitive Instability
2.3. Statistical Analysis
3. Results
3.1. Preliminary analyses
3.2. Correlation Analysis
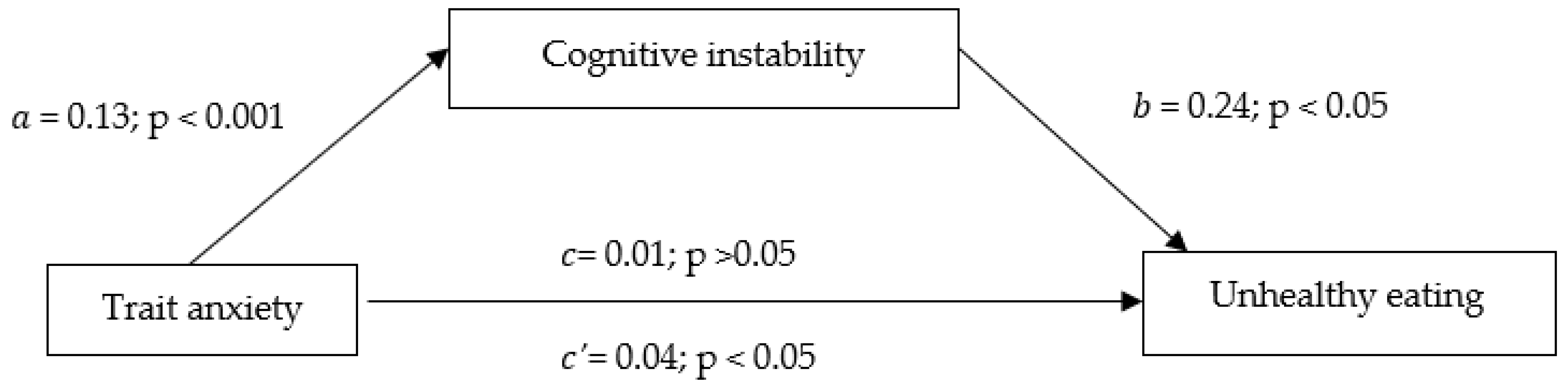
3.3. Mediation Analysis
4. Discussion
4.1. Relationship between Trait Anxiety and Cognitive Instability: Path a
4.2. Relationship between Cognitive Instability and Unhealthy Eating: Path b
4.3. Relationship between Trait Anxiety and Unhealthy Eating: Path c
4.4. The Mediating Role of Cognitive Impulsiveness in the Relationship between Trait Anxiety and Unhealthy Eating in Adult Women Sample: Path c’
4.5. Limitations of the Study and Future Directions
4.6. Strengths of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Salazar-Fernández, C.; Palet, D.; Haeger, P.A.; Mella, F.R. The Perceived Impact of COVID-19 on Comfort Food Consumption over Time: The Mediational Role of Emotional Distress. Nutrients 2021, 13, 1910. [Google Scholar] [CrossRef]
- Aucoin, M.; Lachance, L.; Naidoo, U.; Remy, D.; Shekdar, T.; Sayar, N.; Cardozo, V.; Rawana, T.; Chan, I.; Cooley, K. Diet and Anxiety: A Scoping Review. Nutrients 2021, 13, 4418. [Google Scholar] [CrossRef] [PubMed]
- Wright, R.S.; Gerassimakis, C.; Bygrave, D.; Waldstein, S.R. Dietary Factors and Cognitive Function in Poor Urban Settings. Curr. Nutr. Rep. 2017, 6, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Francis, H.; Stevenson, R. The Longer-Term Impacts of Western Diet on Human Cognition and the Brain. Appetite 2013, 63, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, M.F.; Mason, M.A.; Allegro, D.; Zonderman, A.B.; Evans, M.K. Diet Quality Is Inversely Associated with C-Reactive Protein Levels in Urban, Low-Income African-American and White Adults. J. Acad. Nutr. Diet. 2013, 113, 1620–1631. [Google Scholar] [CrossRef]
- Devonport, T.J.; Nicholls, W.; Fullerton, C. A Systematic Review of the Association between Emotions and Eating Behaviour in Normal and Overweight Adult Populations. J. Health Psychol. 2019, 24, 3–24. [Google Scholar] [CrossRef]
- Liao, Y.; Schembre, S.M.; O’Connor, S.G.; Belcher, B.R.; Maher, J.P.; Dzubur, E.; Dunton, G.F. An Electronic Ecological Momentary Assessment Study to Examine the Consumption of High-Fat/High-Sugar Foods, Fruits/Vegetables, and Affective States Among Women. J. Nutr. Educ. Behav. 2018, 50, 626–631. [Google Scholar] [CrossRef]
- Smith, K.E.; Mason, T.B.; Crosby, R.D.; Engel, S.G.; Crow, S.J.; Wonderlich, S.A.; Peterson, C.B. State and Trait Positive and Negative Affectivity in Relation to Restraint Intention and Binge Eating among Adults with Obesity. Appetite 2018, 120, 327–334. [Google Scholar] [CrossRef]
- Macht, M. How Emotions Affect Eating: A Five-Way Model. Appetite 2008, 50, 1–11. [Google Scholar] [CrossRef]
- Cardi, V.; Leppanen, J.; Treasure, J. The Effects of Negative and Positive Mood Induction on Eating Behaviour: A Meta-Analysis of Laboratory Studies in the Healthy Population and Eating and Weight Disorders. Neurosci. Biobehav. Rev. 2015, 57, 299–309. [Google Scholar] [CrossRef]
- Evers, C.; Dingemans, A.; Junghans, A.F.; Boevé, A. Feeling Bad or Feeling Good, Does Emotion Affect Your Consumption of Food? A Meta-Analysis of the Experimental Evidence. Neurosci. Biobehav. Rev. 2018, 92, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Kose, J.; Cheung, A.; Fezeu, L.K.; Péneau, S.; Debras, C.; Touvier, M.; Hercberg, S.; Galan, P.; Andreeva, V.A. A Comparison of Sugar Intake between Individuals with High and Low Trait Anxiety: Results from the NutriNet-Santé Study. Nutrients 2021, 13, 1526. [Google Scholar] [CrossRef] [PubMed]
- Kose, J.; Fezeu, L.K.; Touvier, M.; Péneau, S.; Hercberg, S.; Galan, P.; Andreeva, V.A. Dietary Macronutrient Intake According to Sex and Trait Anxiety Level among Non-Diabetic Adults: A Cross-Sectional Study. Nutr. J. 2021, 20, 78. [Google Scholar] [CrossRef] [PubMed]
- Moeller, F.G.; Barratt, E.S.; Dougherty, D.M.; Schmitz, J.M.; Swann, A.C. Psychiatric Aspects of Impulsivity. Am. J. Psychiatry 2001, 158, 1783–1793. [Google Scholar] [CrossRef]
- Bénard, M.; Bellisle, F.; Kesse-Guyot, E.; Julia, C.; Andreeva, V.A.; Etilé, F.; Reach, G.; Dechelotte, P.; Tavolacci, M.P.; Hercberg, S.; et al. Impulsivity Is Associated with Food Intake, Snacking, and Eating Disorders in a General Population. Am. J. Clin. Nutr. 2019, 109, 117–126. [Google Scholar] [CrossRef]
- Bénard, M.; Bellisle, F.; Etilé, F.; Reach, G.; Kesse-Guyot, E.; Hercberg, S.; Péneau, S. Impulsivity and Consideration of Future Consequences as Moderators of the Association between Emotional Eating and Body Weight Status. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 84. [Google Scholar] [CrossRef]
- Marques, I.C.F.; Ting, M.; Cedillo-Martínez, D.; Pérez-Cueto, F.J.A. Effect of Impulsivity Traits on Food Choice within a Nudging Intervention. Nutrients 2020, 12, 1402. [Google Scholar] [CrossRef]
- Jasinska, A.J.; Yasuda, M.; Burant, C.F.; Gregor, N.; Khatri, S.; Sweet, M.; Falk, E.B. Impulsivity and Inhibitory Control Deficits Are Associated with Unhealthy Eating in Young Adults. Appetite 2012, 59, 738–747. [Google Scholar] [CrossRef]
- Stanford, M.S.; Mathias, C.W.; Dougherty, D.M.; Lake, S.L.; Anderson, N.E.; Patton, J.H. Fifty Years of the Barratt Impulsiveness Scale: An Update and Review. Personal. Individ. Differ. 2009, 47, 385–395. [Google Scholar] [CrossRef]
- Reise, S.P.; Moore, T.M.; Sabb, F.W.; Brown, A.K.; London, E.D. The Barratt Impulsiveness Scale-11: Reassessment of Its Structure in a Community Sample. Psychol. Assess. 2013, 25, 631–642. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S. Emotion Regulation and Psychopathology: The Role of Gender. Annu. Rev. Clin. Psychol. 2012, 8, 161–187. [Google Scholar] [CrossRef] [PubMed]
- Hantsoo, L.; Epperson, C.N. Anxiety Disorders Among Women: A Female Lifespan Approach. Focus 2017, 15, 162–172. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.-S.; Zheng, D.H.; Liu, M.M. Trait Impulsivity and Choice Impulsivity in Young Adult Students With Probable Binge Eating Disorder. Front. Psychiatry 2022, 13, 433. [Google Scholar] [CrossRef] [PubMed]
- Lyke, J.A.; Spinella, M. Associations among Aspects of Impulsivity and Eating Factors in a Non-clinical Sample. Int. J. Eat. Disord. 2004, 36, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Kelly, N.R.; Cotter, E.W.; Mazzeo, S.E. Examining the Role of Distress Tolerance and Negative Urgency in Binge Eating Behavior among Women. Eat. Behav. 2014, 15, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Bilevicius, E.; van Landeghem, C.; Stewart, S.H.; Sherry, S.B.; Keough, M.T. Trait Impulsivity Impedes Maturing Out of Problem Drinking Among Socially Anxious Undergraduates. Alcohol Alcohol. 2021, 56, 101–108. [Google Scholar] [CrossRef]
- da Fonseca, N.K.d.O.; Molle, R.D.; Costa, M.d.A.; Gonçalves, F.G.; Silva, A.C.; Rodrigues, Y.; Price, M.; Silveira, P.P.; Manfro, G.G. Impulsivity Influences Food Intake in Women with Generalised Anxiety Disorder. Rev. Bras. Psiquiatr. 2020, 42, 382–388. [Google Scholar] [CrossRef]
- Constant, A.; Gautier, Y.; Coquery, N.; Thibault, R.; Moirand, R.; Val-Laillet, D. Emotional Overeating Is Common and Negatively Associated with Alcohol Use in Normal-Weight Female University Students. Appetite 2018, 129, 186–191. [Google Scholar] [CrossRef]
- Bourdier, L.; Morvan, Y.; Kotbagi, G.; Kern, L.; Romo, L.; Berthoz, S. Examination of Emotion-Induced Changes in Eating: A Latent Profile Analysis of the Emotional Appetite Questionnaire. Appetite 2018, 123, 72–81. [Google Scholar] [CrossRef]
- Aoun, C.; Nassar, L.; Soumi, S.; El Osta, N.; Papazian, T.; Rabbaa Khabbaz, L. The Cognitive, Behavioral, and Emotional Aspects of Eating Habits and Association with Impulsivity, Chronotype, Anxiety, and Depression: A Cross-Sectional Study. Front. Behav. Neurosci. 2019, 13, 204. [Google Scholar] [CrossRef]
- Carter, F.A.; Jansen, A. Improving Psychological Treatment for Obesity. Which Eating Behaviours Should We Target? Appetite 2012, 58, 1063–1069. [Google Scholar] [CrossRef] [PubMed]
- Organisation, W.H. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. In World Health Organization Technical Report Series; WHO: Geneva, Switzerland, 2000; Volume 894, pp. 1–253. [Google Scholar]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar] [PubMed]
- Brytek-Matera, A. Negative Affect and Maladaptive Eating Behavior as a Regulation Strategy in Normal-Weight Individuals: A Narrative Review. Sustainability 2021, 13, 13704. [Google Scholar] [CrossRef]
- Waliłko, J.; Bronowicka, P.; He, J.; Brytek-Matera, A.; Rocha-Rodrigues, S.; Afonso, J.; Sousa, M. Dieting and Disinhibited Eating Patterns in Adult Women with Normal Body Weight: Does Rumination Matter? Nutrients 2021, 13, 2475. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R.; Jacobs, G.A. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Wrześniewski, K.; Sosnowski, T.; Matusik, D. Inwentarz Stanu i Cechy Lęku STAI. Polska Adaptacja STAI. Podręcznik. (State-Trait Anxiety Inventory Manual—Polish Adaptation); PTP: Warsaw, Poland, 2002. [Google Scholar]
- Wadolowska, L. Walidacja Kwestionariusza Czestotliwosci Spozycia Zywnosci—FFQ. Ocena Powtarzalnosci [Validation of Food Frequency Questionnaire [FFQ]. Reproducibility Assessment]. Bromatol. I Chem. Toksykol. 2005, 38, 27–33. [Google Scholar]
- Institute, N.C. Food Frequency Questionnaire at a Glance | Dietary Assessment Primer. Available online: https://dietassessmentprimer.cancer.gov/profiles/questionnaire/ (accessed on 1 September 2022).
- Patton, J.H.; Stanford, M.S.; Barratt, E.S. Factor Structure of the Barratt Impulsiveness Scale. J. Clin. Psychol. 1995, 51, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Grzesiak, M.; Beszłej, J.; Szechiński, M. Skala Impulsywności Barratta. Adv. Psychiatry Neurol. 2008, 17, 61–64. [Google Scholar]
- Barratt, E.S. Factor Analysis of Some Psychometric Measures of Impulsiveness and Anxiety. Psychol. Rep. 1965, 16, 547–554. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- O’Leary, D.; Smith, A.; Salehi, E.; Gross, J.J. Negative Affect, Affect Regulation, and Food Choice: A Value-Based Decision-Making Analysis. Soc. Psychol. Personal. Sci. 2022. [Google Scholar] [CrossRef]
- Kaiser, H.F. The Application of Electronic Computers to Factor Analysis. Educ. Psychol. Meas. 1960, 20, 141–151. [Google Scholar] [CrossRef]
- Moustafa, A.A.; Tindle, R.; Frydecka, D.; Misiak, B. Impulsivity and Its Relationship with Anxiety, Depression and Stress. Compr. Psychiatry 2017, 74, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Phillipou, A.; Abel, L.A.; Castle, D.J.; Gurvich, C.; Hughes, M.E.; Rossell, S.L. Self-Reported and Behavioural Impulsivity in Anorexia Nervosa. World J. Psychiatry 2016, 6, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Guerrieri, R.; Nederkoorn, C.; Schrooten, M.; Martijn, C.; Jansen, A. Inducing Impulsivity Leads High and Low Restrained Eaters into Overeating, Whereas Current Dieters Stick to Their Diet. Appetite 2009, 53, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Mestre, Z.L.; Melhorn, S.J.; Askren, M.K.; Tyagi, V.; Gatenby, C.; Young, L.; Mehta, S.; Webb, M.F.; Grabowski, T.J.; Schur, E.A. Effects of Anxiety on Caloric Intake and Satiety-Related Brain Activation in Women and Men. Psychosom. Med. 2016, 78, 454–464. [Google Scholar] [CrossRef] [PubMed]
- van Strien, T.; Gibson, E.L.; Baños, R.; Cebolla, A.; Winkens, L.H.H. Is Comfort Food Actually Comforting for Emotional Eaters? A (Moderated) Mediation Analysis. Physiol. Behav. 2019, 211, 112671. [Google Scholar] [CrossRef]
- Yau, Y.H.C.; Potenza, M.N. Stress and Eating Behaviors. Minerva Endocrinol. 2013, 38, 255. [Google Scholar]
- Kandiah, J.; Yake, M.; Jones, J.; Meyer, M. Stress Influences Appetite and Comfort Food Preferences in College Women. Nutr. Res. 2006, 26, 118–123. [Google Scholar] [CrossRef]
- Evers, C.; Stok, F.; de Ridder, D.T.D. Feeding Your Feelings: Emotion Regulation Strategies and Emotional Eating. Personal. Soc. Psychol. Bull. 2010, 36, 792–804. [Google Scholar] [CrossRef]
- Van Blyderveen, S.; Lafrance, A.; Emond, M.; Kosmerly, S.; O’Connor, M.; Chang, F. Personality Differences in the Susceptibility to Stress-Eating: The Influence of Emotional Control and Impulsivity. Eat. Behav. 2016, 23, 76–81. [Google Scholar] [CrossRef]
- Gross, J.J. The Emerging Field of Emotion Regulation: An Integrative Review. Rev. Gen. Psychol. 1998, 2, 271–299. [Google Scholar] [CrossRef]
- Herren, O.M.; Agurs-Collins, T.; Dwyer, L.A.; Perna, F.M.; Ferrer, R. Emotion Suppression, Coping Strategies, Dietary Patterns, and BMI. Eat. Behav. 2021, 41, 101500. [Google Scholar] [CrossRef] [PubMed]
- Forcano, L.; Mata, F.; de la Torre, R.; Verdejo-Garcia, A. Cognitive and Neuromodulation Strategies for Unhealthy Eating and Obesity: Systematic Review and Discussion of Neurocognitive Mechanisms. Neurosci. Biobehav. Rev. 2018, 87, 161–191. [Google Scholar] [CrossRef] [PubMed]
- Rubia, K.; Russell, T.; Overmeyer, S.; Brammer, M.J.; Bullmore, E.T.; Sharma, T.; Simmons, A.; Williams, S.C.R.; Giampietro, V.; Andrew, C.M.; et al. Mapping Motor Inhibition: Conjunctive Brain Activations across Different Versions of Go/No-Go and Stop Tasks. Neuroimage 2001, 13, 250–261. [Google Scholar] [CrossRef] [PubMed]
- Loxton, N.J.; Tipman, R.J. Reward Sensitivity and Food Addiction in Women. Appetite 2017, 115, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Juszczyk, A.; Dragan, M.; Grajewski, P.; Holas, P. Prevalence of Adjustment Disorder in Poland during the COVID-19 Pandemic and Its Association with Symptoms of Anxiety and Depression. Adv. Psychiatry Neurol. Postępy Psychiatr. I Neurol. 2021, 30, 141–153. [Google Scholar] [CrossRef]
| Measure | Mean | SD | Min | Max | Skewness | Kurtosis | ||
|---|---|---|---|---|---|---|---|---|
| Statistic | Std. Error | Statistic | Std. Error | |||||
| Age | 29.70 | 9.23 | 20 | 60 | 1.06 | 0.16 | 0.05 | 0.32 |
| BMI | 23.39 | 4.43 | 18.57 | 42.45 | 1.45 | 0.16 | 3.12 | 0.32 |
| During the past 2 months, how often have you eaten or drank... |
| … low calorie foods? |
| … fresh foods? |
| … well-balanced diet? |
| … low carbohydrate foods? |
| … organic foods? |
| … low fat foods? |
| … natural foods? |
| … whole grains? |
| … low sugar foods? |
| … vegetarian/vegan? |
| … gluten-free foods? |
| … low sodium foods? |
| … locally sourced foods? |
| … vegetables? |
| … fruits? |
| … something sweet and unhealthy (i.e., candy or cake)? |
| … soft drinks or soda? |
| … alcoholic beverages? |
| … snack foods? |
| … fast foods? |
| … water? |
| Variable | Number | Percent |
|---|---|---|
| Body Mass Index range | ||
| Healthy Weight range (18.5 to 24.9 kg/m2) | 162 | 72.0 |
| Overweight range (25.0 to 29.9 kg/m2) | 46 | 20.4 |
| Obese range (≥30.0 kg/m2) | 17 | 7.6 |
| Education level | ||
| Secondary | 69 | 30.7 |
| University | 156 | 69.3 |
| Socioeconomic status | ||
| Social class of the participant’s family | ||
| Lower class | 1 | 0.4 |
| Working class | 14 | 6.2 |
| Lower-middle class | 43 | 19.1 |
| Middle class | 127 | 56.4 |
| Upper-middle class | 38 | 16.9 |
| Upper class | 2 | 0.9 |
| Having a job (either part-time or full-time) | ||
| Yes | 163 | 72.4 |
| No | 62 | 27.6 |
| Number of people residing in participant’s family of origin household | ||
| 1 | 39 | 17.3 |
| 2–3 | 111 | 49.3 |
| 4–5 | 66 | 29.3 |
| 6 or more | 9 | 4.0 |
| Eating habits | ||
| Being currently on a diet | ||
| Yes | 31 | 13.8 |
| No | 194 | 86.2 |
| Considering oneself a healthy eater | ||
| Very slightly or not at all | 7 | 3.1 |
| Somewhat | 25 | 11.1 |
| Moderately so | 105 | 46.7 |
| Mostly | 80 | 35.6 |
| Definitely | 8 | 3.6 |
| Measure | Mean | SD | Min | Max | Skewness | Kurtosis | ||
|---|---|---|---|---|---|---|---|---|
| Statistic | Std. Error | Statistic | Std. Error | |||||
| Trait anxiety | 43.32 | 8.66 | 23 | 71 | 0.36 | 0.16 | −0.05 | 0.32 |
| Cognitive instability | 6.41 | 1.88 | 3 | 12 | 1.88 | 0.16 | −0.27 | 0.32 |
| Unhealthy eating | 6.78 | 2.49 | 2 | 16 | 0.57 | 0.16 | 0.71 | 0.32 |
| Component | |||||
|---|---|---|---|---|---|
| Total Variance Explained | 1 | 2 | 3 | 4 | |
| Initial eigenvalues | Total | 3.193 | 1.467 | 1.333 | 1.013 |
| % of variance | 29.032 | 13.338 | 12.117 | 9.206 | |
| Cumulative % | 29.032 | 42.369 | 54.487 | 63.692 | |
| Extraction sums of squared loadings | Total | 3.193 | 1.467 | 1.333 | 1.013 |
| % of variance | 29.032 | 13.338 | 12.117 | 9.206 | |
| Cumulative % | 29.032 | 42.369 | 54.487 | 63.692 | |
| Rotation sums of squared loadings | Total | 2.463 | 1.871 | 1.490 | 1.038 |
| % of variance | 22.391 | 17.011 | 13.543 | 9.432 | |
| Cumulative % | 22.391 | 39.402 | 52.945 | 62.377 | |
| Individual FFQ Question: During the Past 2 Months How Often Have You Eaten or Drunk ….? | Component | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Fruit | 0.878 | |||
| Vegetables | 0.729 | |||
| Whole grains | 0.726 | |||
| Fresh foods | 0.697 | |||
| Gluten-free foods | 0.778 | |||
| Low sodium foods | 0.764 | |||
| Organic foods | 0.720 | |||
| Something sweet and unhealthy (i.e., candy or cake) | 0.853 | |||
| Snack food | 0.842 | |||
| Water | 0.954 | |||
| Variable/Effect | b | SE | t | p | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Trait anxiety → Unhealthy eating | 0.010 | 0.024 | −0.430 | 0.667 | −0.059 | 0.038 |
| Trait anxiety → Cognitive instability | 0.139 | 0.011 | 12.496 | p < 0.001 | 0.117 | 0.161 |
| Trait anxiety → Cognitive instability → Unhealthy eating | 0.244 | 0.113 | −2.153 | 0.032 | −0.468 | −0.020 |
| Effects | ||||||
| Direct | 0.010 | 0.024 | −0.430 | 0.667 | −0.059 | 0.038 |
| Indirect | 0.034 | 0.016 | −0.065 | −0.002 | ||
| Total | 0.044 | 0.019 | −2.345 | 0.019 | −0.082 | −0.007 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mróz, M.; Gross, J.J.; Brytek-Matera, A. Trait Anxiety and Unhealthy Eating in Adult Women: The Mediating Role of Cognitive Instability. Int. J. Environ. Res. Public Health 2023, 20, 296. https://doi.org/10.3390/ijerph20010296
Mróz M, Gross JJ, Brytek-Matera A. Trait Anxiety and Unhealthy Eating in Adult Women: The Mediating Role of Cognitive Instability. International Journal of Environmental Research and Public Health. 2023; 20(1):296. https://doi.org/10.3390/ijerph20010296
Chicago/Turabian StyleMróz, Magdalena, James J. Gross, and Anna Brytek-Matera. 2023. "Trait Anxiety and Unhealthy Eating in Adult Women: The Mediating Role of Cognitive Instability" International Journal of Environmental Research and Public Health 20, no. 1: 296. https://doi.org/10.3390/ijerph20010296
APA StyleMróz, M., Gross, J. J., & Brytek-Matera, A. (2023). Trait Anxiety and Unhealthy Eating in Adult Women: The Mediating Role of Cognitive Instability. International Journal of Environmental Research and Public Health, 20(1), 296. https://doi.org/10.3390/ijerph20010296






