What Is the Relationship between Trunk Control Function and Arm Coordination in Adults with Severe-to-Moderate Quadriplegic Cerebral Palsy?
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.2.1. Manual Dexterity Tests
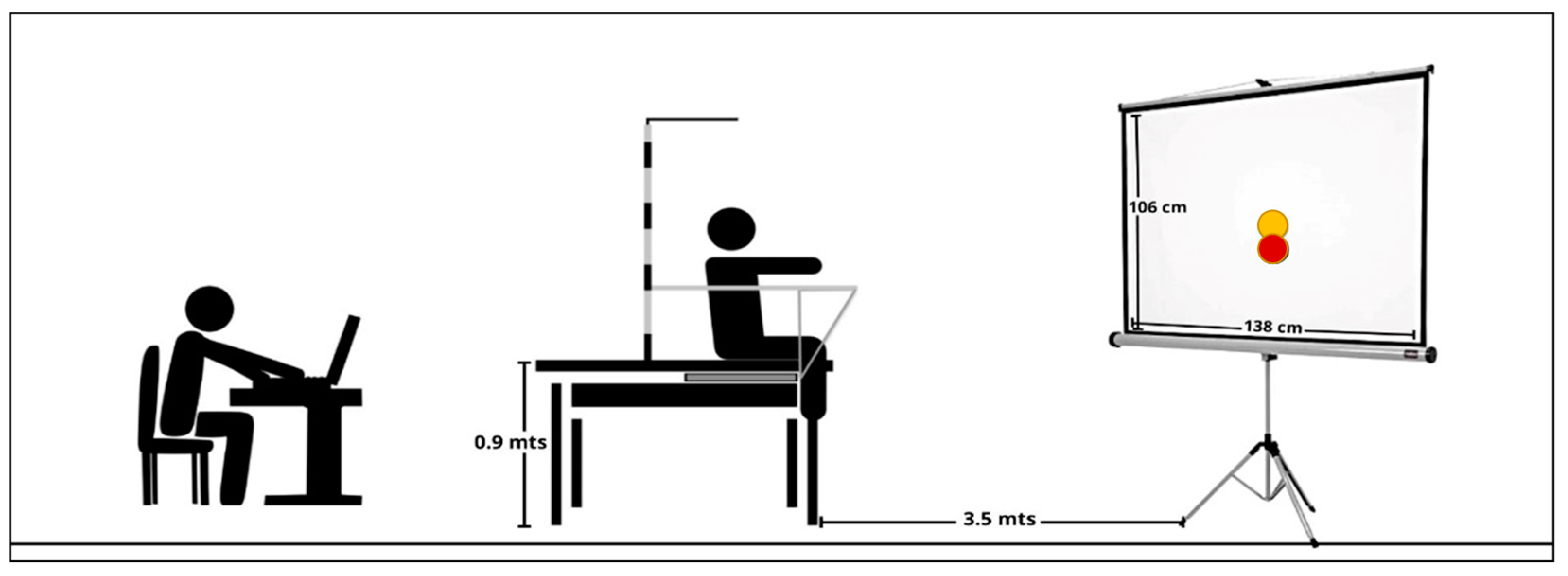
2.2.2. Intra-Limb Coordination Test
2.2.3. Trunk Control Test
2.3. Posturography Data Reduction
2.4. Statistical Analysis
3. Results
4. Discussions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.G.B. Development and Reliability of a System to Classify Gross Motor Function in Children with Cerebral Palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; An, D.H.; Yoo, W.G. The Relationship between Trunk Control and Upper Limb Function in Children with Cerebral Palsy. Technol. Health Care 2018, 26, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Abd-Elfattah, H.M.; Aly, S.M. Effect of Core Stability Exercises on Hand Functions in Children with Hemiplegic Cerebral Palsy. Ann. Rehabil. Med. 2021, 45, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Kusumoto, Y.; Takaki, K.; Matsuda, T.; Nitta, O. Relevant Factors of Self-Care in Children and Adolescents with Spastic Cerebral Palsy. PLoS ONE 2021, 16, e0254899. [Google Scholar] [CrossRef]
- van der Slot, W.M.A.; Roebroeck, M.E.; Landkroon, A.P.; Terburg, M.; van den Berg-Emons, R.J.G.; Stam, H.J. Everyday Physical Activity and Community Participation of Adults with Hemiplegic Cerebral Palsy. Disabil. Rehabil. 2007, 29, 179–189. [Google Scholar] [CrossRef]
- Yi, Y.G.; Jung, S.H.; Bang, M.S. Emerging Issues in Cerebral Palsy Associated with Aging: A Physiatrist Perspective. Ann. Rehabil. Med. 2019, 43, 241–249. [Google Scholar] [CrossRef]
- Lauruschkus, K.; Nordmark, E.; Hallström, I. “It’s Fun, but...” Children with Cerebral Palsy and Their Experiences of Participation in Physical Activities. Disabil. Rehabil. 2015, 37, 283–289. [Google Scholar] [CrossRef]
- WorldBoccia BISFed International Boccia Rules. 2021. Available online: https://www.worldboccia.com/wp-content/uploads/2021/10/Boccia-Classification-Rules-5th-Edition-September-2021287.pdf (accessed on 10 November 2022).
- Huang, P.C.; Pan, P.J.; Ou, Y.C.; Yu, Y.C.; Tsai, Y.S. Motion Analysis of Throwing Boccia Balls in Children with Cerebral Palsy. Res. Dev. Disabil. 2014, 35, 393–399. [Google Scholar] [CrossRef]
- Kukke, S.N.; Curatalo, L.A.; De Campos, A.C.; Hallett, M.; Alter, K.E.; Damiano, D.L. Coordination of Reach-to-Grasp Kinematics in Individuals with Childhood-Onset Dystonia Due to Hemiplegic Cerebral Palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 582–590. [Google Scholar] [CrossRef]
- Connick, M.J.; Beckman, E.; Deuble, R.; Tweedy, S.M. Developing Tests of Impaired Coordination for Paralympic Classification: Normative Values and Test–Retest Reliability. Sport. Eng. 2016, 19, 147–154. [Google Scholar] [CrossRef]
- Roldan, A.; Sabido, R.; Barbado, D.; Caballero, C.; Reina, R. Manual Dexterity and Intralimb Coordination Assessment to Distinguish Different Levels of Impairment in Boccia Players with Cerebral Palsy. Front. Neurol. 2017, 8, 582. [Google Scholar] [CrossRef] [PubMed]
- Makofske, B. Manual Dexterity BT—Encyclopedia of Clinical Neuropsychology; Kreutzer, J.S., DeLuca, J., Caplan, B., Eds.; Springer: New York, NY, USA, 2011; pp. 1522–1523. ISBN 978-0-387-79948-3. [Google Scholar]
- Golubović, Š.; Slavković, S. Manual Ability and Manual Dexterity in Children with Cerebral Palsy. Hippokratia 2014, 18, 310–314. [Google Scholar] [PubMed]
- Klingels, K.; Demeyere, I.; Jaspers, E.; De Cock, P.; Molenaers, G.; Boyd, R.; Feys, H. Upper Limb Impairments and Their Impact on Activity Measures in Children with Unilateral Cerebral Palsy. Eur. J. Paediatr. Neurol. 2012, 16, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Tseng, M.H.; Chen, K.L.; Shieh, J.Y.; Lu, L.; Huang, C.Y. The Determinants of Daily Function in Children with Cerebral Palsy. Res. Dev. Disabil. 2011, 32, 235–245. [Google Scholar] [CrossRef]
- Arnould, C.; Penta, M.; Renders, A.; Thonnard, J.L. ABILHAND-Kids: A Measure of Manual Ability in Children with Cerebral Palsy. Neurology 2004, 63, 1045–1052. [Google Scholar] [CrossRef]
- Oliveira, C.; Almeida Santos, C.; Freitas, L.; Santana, R.; Fernandes, G.; Junior, P.; Moura, R. Use of the Box and Block Test for the Evaluation of Manual Dexterity in Individuals with Central Nervous System Disorders: A Systematic Review. Man. Ther. Posturology Rehabil. J. 2016, 14, 436. [Google Scholar] [CrossRef]
- Chanubol, R.; Wongphaet, P.; Chavanich, N.; Chira-Adisai, W.; Kuptniratsaikul, P.; Jitpraphai, C. Correlation between the Action Research Arm Test and the Box and Block Test of Upper Extremity Function in Stroke Patients. J. Med. Assoc. Thail. 2012, 95, 590–597. [Google Scholar] [CrossRef]
- Dong, Y.; Liu, X.; Tang, M.; Huo, H.; Chen, D.; Wu, Z.; An, R.; Fan, Y. Design a Haptic-Combined Virtual Reality System to Improve Box and Block Test (BBT) for Upper Extremity Function Assessment. Res. Sq. 2020, 1–19. [Google Scholar] [CrossRef]
- Araneda, R.; Ebner-Karestinos, D.; Paradis, J.; Saussez, G.; Friel, K.M.; Gordon, A.M.; Bleyenheuft, Y. Reliability and Responsiveness of the Jebsen-Taylor Test of Hand Function and the Box and Block Test for Children with Cerebral Palsy. Dev. Med. Child Neurol. 2019, 61, 1182–1188. [Google Scholar] [CrossRef]
- Barbado, D.; Reina, R.; Roldan, A.; McCulloch, K.; Campayo-Piernas, M.; Vera-Garcia, F.J. How Much Trunk Control Is Affected in Adults with Moderate-to-Severe Cerebral Palsy? J. Biomech. 2019, 82, 368–374. [Google Scholar] [CrossRef]
- Santamaria, V.; Rachwani, J.; Saussez, G.; Bleyenheuft, Y.; Dutkowsky, J.; Gordon, A.M.; Woollacott, M.H. The Seated Postural & Reaching Control Test in Cerebral Palsy: A Validation Study. Phys. Occup. Ther. Pediatr. 2020, 40, 441–469. [Google Scholar] [CrossRef] [PubMed]
- Assaiante, C.; Mallau, S.; Viel, S.; Jover, M.; Schmitz, C. Development of Postural Control in Healthy Children: A Functional Approach. Neural Plast. 2005, 12, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Cankurtaran, D.; Abidin, N.; Akyuz, E.U.; Tezel, N. An Investigation into the Factors Which Affect the Sitting Balance of Non-Ambulatory Children with Cerebral Palsy. Neurol. Asia 2021, 26, 575–583. [Google Scholar] [CrossRef]
- Peeters, L.H.C.; de Groot, I.J.M.; Geurts, A.C.H. Trunk Involvement in Performing Upper Extremity Activities While Seated in Neurological Patients with a Flaccid Trunk—A Review. Gait Posture 2018, 62, 46–55. [Google Scholar] [CrossRef]
- Ju, Y.H.; You, J.Y.; Cherng, R.J. Effect of Task Constraint on Reaching Performance in Children with Spastic Diplegic Cerebral Palsy. Res. Dev. Disabil. 2010, 31, 1076–1082. [Google Scholar] [CrossRef]
- van der Heide, J.C.; Begeer, C.; Fock, J.M.; Otten, B.; Stremmelaar, E.; van Eykern, L.A.; Hadders-Algra, M. Postural Control during Reaching in Preterm Children with Cerebral Palsy. Dev. Med. Child Neurol. 2004, 46, 253–266. [Google Scholar] [CrossRef]
- Park, H.; Choi, J.Y.; Yi, S.H.; Park, E.S.; Shim, D.; Choi, T.Y.; Rha, D.W. Relationship between the More-Affected Upper Limb Function and Daily Activity Performance in Children with Cerebral Palsy: A Cross-Sectional Study. BMC Pediatr. 2021, 21, 1–8. [Google Scholar] [CrossRef]
- Kataoka, M.; Okuda, K.; Iwata, A.; Imura, S.; Yahagi, K.; Matsuo, Y. Throwing Distance and Competitive Performance of Boccia Players. J. Phys. Ther. Sci. 2020, 32, 574–577. [Google Scholar] [CrossRef]
- Mathiowetz, V.; Federman, S.; Wiemer, D. Box and Block Test of Manual Dexterity: Norms for 6–19 Year Olds. Can. J. Occup. Ther. 1985, 52, 241–245. [Google Scholar] [CrossRef]
- Deuble, R.L.; Connick, M.J.; Beckman, E.M.; Abernethy, B.; Tweedy, S.M. Using Fitts’ Law to Detect Intentional Misrepresentation. J. Mot. Behav. 2016, 48, 164–171. [Google Scholar] [CrossRef]
- Barbado, D.; Barbado, L.C.; Elvira, J.L.L.; van Dieën, J.H.; Vera-Garcia, F.J. Sports-Related Testing Protocols Are Required to Reveal Trunk Stability Adaptations in High-Level Athletes. Gait Posture 2016, 49, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Roldan, A.; Barbado, D.; Vera-Garcia, F.J.; Sarabia, J.M.; Reina, R. Inter-Rater Reliability, Concurrent Validity and Sensitivity of Current Methods to Assess Trunk Function in Boccia Player with Cerebral Palsy. Brain Sci. 2020, 10, 130. [Google Scholar] [CrossRef] [PubMed]
- Hancock, G.R.; Butler, M.S.; Fischman, M.G. On the Problem of Two-Dimensional Error Scores: Measures and Analyses of Accuracy, Bias, and Consistency. J. Mot. Behav. 1995, 27, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.H.; Hwang, I.S.; Cherng, R.J. Postural Adjustment of Children with Spastic Diplegic Cerebral Palsy during Seated Hand Reaching in Different Directions. Arch. Phys. Med. Rehabil. 2012, 93, 471–479. [Google Scholar] [CrossRef]
- Reina, R.; Domínguez-Díez, M.; Urbán, T.; Roldán, A. Throwing Distance Constraints Regarding Kinematics and Accuracy in High-Level Boccia Players. Sci. Sport. 2018, 33, 299–306. [Google Scholar] [CrossRef]
- Angsupaisal, M.; Maathuis, C.G.B.; Hadders-Algra, M. Adaptive Seating Systems in Children with Severe Cerebral Palsy across International Classification of Functioning, Disability and Health for Children and Youth Version Domains: A Systematic Review. Dev. Med. Child Neurol. 2015, 57, 919–930. [Google Scholar] [CrossRef]
- Santamaria, V.; Rachwani, J.; Saavedra, S.; Woollacott, M. Effect of Segmental Trunk Support on Posture and Reaching in Children With Cerebral Palsy. Pediatr. Phys. Ther. Off. Publ. Sect. Pediatr. Am. Phys. Ther. Assoc. 2016, 28, 285–293. [Google Scholar] [CrossRef]
- Yildiz, A.; Yildiz, R.; Elbasan, B. Trunk Control in Children with Cerebral Palsy and Its Association with Upper Extremity Functions. J. Dev. Phys. Disabil. 2018, 30, 669–676. [Google Scholar] [CrossRef]
| Task | Mean | SD | |
|---|---|---|---|
| MD tests | |||
| BB (N blocks) | 22.78 | ± | 8.52 |
| BBL (N balls) | 30.89 | ± | 12.35 |
| ILC tests | |||
| DHFT (s) | 896.07 | ± | 544.40 |
| DVTB (s) | 969.82 | ± | 607.96 |
| CVTB (N contacts) | 39.47 | ± | 16.99 |
| Trunk control tests | |||
| Static (mm) | 4.67 | ± | 3.66 |
| Dynamic (mm) | 9.59 | ± | 4.52 |
| Task | Static Control Test | Dynamic Control Test | ||
|---|---|---|---|---|
| r | p | r | p | |
| MD tests | ||||
| BB (N blocks) | −0.553 | 0.002 ** | −0.405 | 0.032 * |
| BBL (N balls) | −0.537 | 0.004 ** | −0.290 | 0.142 |
| ILC tests | ||||
| DHFT (s) | 0.769 | 0.001 ** | 0.677 | 0.006 * |
| DVTB (s) | 0.739 | 0.009 * | 0.529 | 0.094 |
| CVTB (N contacts) | −0.616 | 0.044 * | −0.120 | 0.726 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cornejo, M.I.; Roldan, A.; Reina, R. What Is the Relationship between Trunk Control Function and Arm Coordination in Adults with Severe-to-Moderate Quadriplegic Cerebral Palsy? Int. J. Environ. Res. Public Health 2023, 20, 141. https://doi.org/10.3390/ijerph20010141
Cornejo MI, Roldan A, Reina R. What Is the Relationship between Trunk Control Function and Arm Coordination in Adults with Severe-to-Moderate Quadriplegic Cerebral Palsy? International Journal of Environmental Research and Public Health. 2023; 20(1):141. https://doi.org/10.3390/ijerph20010141
Chicago/Turabian StyleCornejo, María Isabel, Alba Roldan, and Raul Reina. 2023. "What Is the Relationship between Trunk Control Function and Arm Coordination in Adults with Severe-to-Moderate Quadriplegic Cerebral Palsy?" International Journal of Environmental Research and Public Health 20, no. 1: 141. https://doi.org/10.3390/ijerph20010141
APA StyleCornejo, M. I., Roldan, A., & Reina, R. (2023). What Is the Relationship between Trunk Control Function and Arm Coordination in Adults with Severe-to-Moderate Quadriplegic Cerebral Palsy? International Journal of Environmental Research and Public Health, 20(1), 141. https://doi.org/10.3390/ijerph20010141








