Standard Values and Concurrent Validity of a Newly Developed Occlusal Force-Measuring Device among Community-Dwelling Older Adults: The Otassha Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design, Setting, and Participants
2.2. OF Measurements
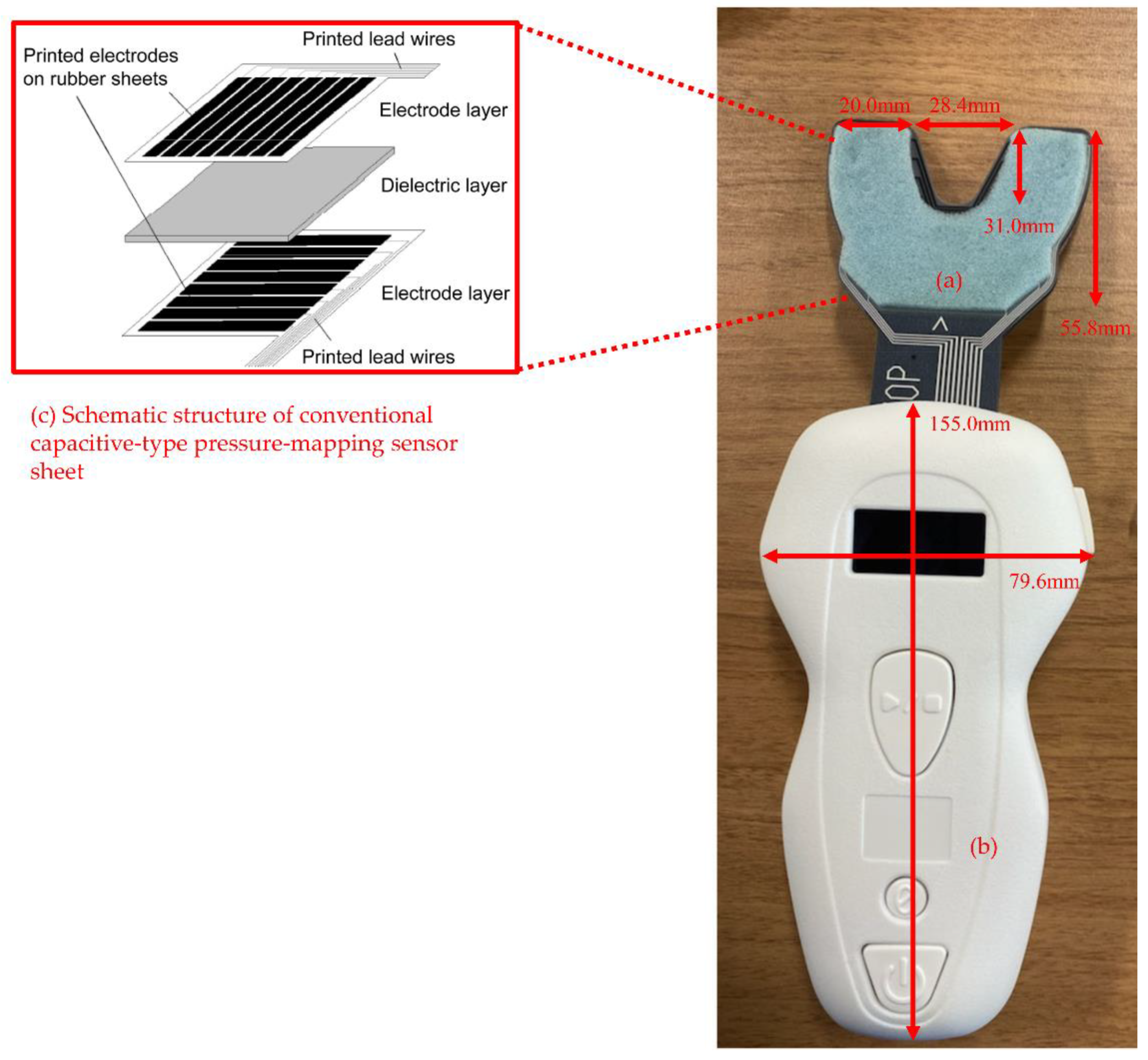
2.2.1. OF Measurements Using an OFMD-CPS
2.2.2. OF Measurements Using the Dental Prescale II
2.3. Dental Examination
2.4. Other Characteristics
2.5. Statistical Analyses
3. Results
3.1. Study Population
3.2. Descriptive Statistics for OFMD-CPS-Measured OF
3.3. Correlations among OF, the Numbers of Natural Teeth and Functional Teeth, and Age
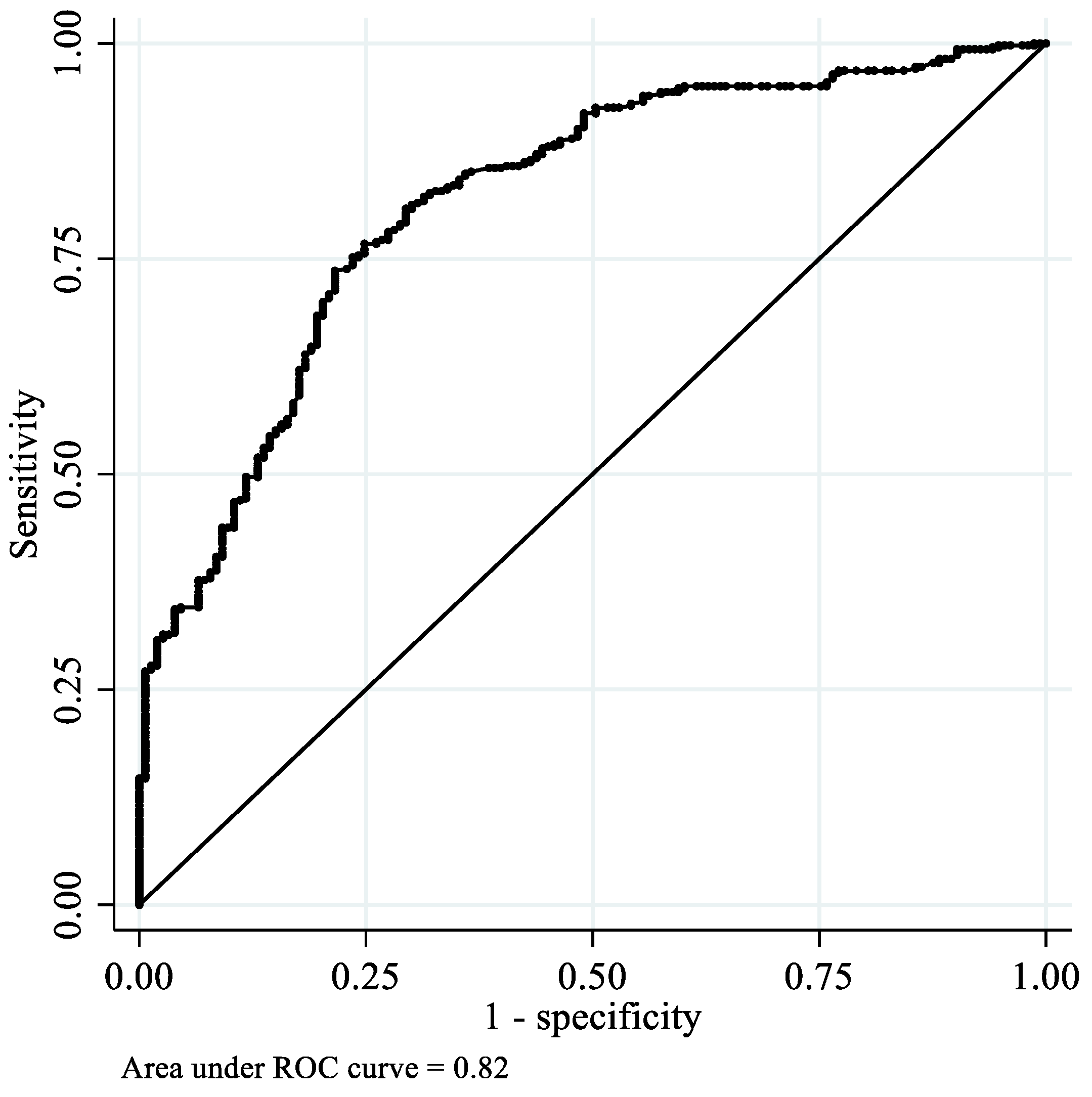
3.4. Predictive Value of OFMD-CPS-Measured OF
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hatch, J.P.; Shinkai, R.S.; Sakai, S.; Rugh, J.D.; Paunovich, E.D. Determinants of masticatory performance in dentate adults. Arch. Oral Biol. 2001, 46, 641–648. [Google Scholar] [CrossRef]
- Ikebe, K.; Matsuda, K.; Kagawa, R.; Enoki, K.; Okada, T.; Yoshida, M.; Maeda, Y. Masticatory performance in older subjects with varying degrees of tooth loss. J. Dent. 2012, 40, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Kosaka, T.; Ono, T.; Kida, M.; Kikui, M.; Yamamoto, M.; Yasui, S.; Nokubi, T.; Maeda, Y.; Kokubo, Y.; Watanabe, M.; et al. A multifactorial model of masticatory performance: The Suita study. J. Oral Rehabil. 2016, 43, 340–347. [Google Scholar] [CrossRef] [PubMed]
- The Ministry of Health, Labour, and Welfare. Survey of Dental Diseases, 2016 (In Japanese). Available online: https://www.mhlw.go.jp/toukei/list/dl/62-28-02.pdf. (accessed on 30 March 2022).
- Minakuchi, S.; Tsuga, K.; Ikebe, K.; Ueda, T.; Tamura, F.; Nagao, K.; Furuya, J.; Matsuo, K.; Yamamoto, K.; Kanazawa, M.; et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology 2018, 35, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Maeda, I.; Kokubo, Y.; Tanaka, Y.; Ueno, T.; Takahashi, W.; Watanabe, Y.; Hirano, H. Capacitive-type pressure-mapping sensor for measuring bite force. Int. J. Environ. Res. Public Health 2022, 19, 1273. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, Y.; Suzuki, H.; Kawai, H.; Hirano, H.; Yoshida, H.; Kojima, M.; Ihara, K.; Obuchi, S. Physical and sociopsychological characteristics of older community residents with mild cognitive impairment as assessed by the Japanese version of the Montreal Cognitive Assessment. J. Geriatr. Psychiatry Neurol. 2013, 26, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Agilent Technologies. Agilent Impedance Measurement Handbook. Available online: https://indico.cern.ch/event/216963/sessions/35851/attachments/347577/484629/impedancemeasurementhandbook_2.pdf (accessed on 22 March 2022).
- Horibe, Y.; Matsuo, K.; Ikebe, K.; Minakuchi, S.; Sato, Y.; Sakurai, K.; Ueda, T. Relationship between two pressure-sensitive films for testing reduced occlusal force in diagnostic criteria for oral hypofunction. Gerodontology 2021, 39, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Murakami, M.; Iijima, K.; Watanabe, Y.; Tanaka, T.; Iwasa, Y.; Edahiro, A.; Ohara, Y.; Motokawa, K.; Shirobe, M.; Hirano, H. Development of a simple method to measure masseter muscle mass. Gerodontology 2020, 37, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Carra, M.C.; Gueguen, A.; Thomas, F.; Pannier, B.; Caligiuri, G.; Steg, P.G.; Zins, M.; Bouchard, P. Self-report assessment of severe periodontitis: Periodontal screening score development. J. Clin. Periodontol. 2018, 45, 818–831. [Google Scholar] [CrossRef] [PubMed]
- Ikebe, K.; Gondo, Y.; Kamide, K.; Masui, Y.; Ishizaki, T.; Arai, Y.; Inagaki, H.; Nakagawa, T.; Kabayama, M.; Ryuno, H.; et al. Occlusal force is correlated with cognitive function directly as well as indirectly via food intake in community-dwelling older Japanese: From the SONIC study. PLoS ONE 2018, 13, e0190741. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inomata, C.; Ikebe, K.; Kagawa, R.; Okubo, H.; Sasaki, S.; Okada, T.; Takeshita, H.; Tada, S.; Matsuda, K.; Kurushima, Y.; et al. Significance of occlusal force for dietary fibre and vitamin intakes in independently living 70-year-old Japanese: From SONIC Study. J. Dent. 2014, 42, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Ohi, T.; Komiyama, T.; Miyoshi, Y.; Murakami, T.; Tsuboi, A.; Tomata, Y.; Tsuji, I.; Watanabe, M.; Hattori, Y. Maximum occlusal force and incident functional disability in older adults: The Tsurugaya project. JDR Clin. Trans. Res. 2018, 3, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Okada, T.; Ikebe, K.; Kagawa, R.; Inomata, C.; Takeshita, H.; Gondo, Y.; Ishioka, Y.; Okubo, H.; Kamide, K.; Masui, Y.; et al. Lower protein intake mediates association between lower occlusal force and slower walking speed: From the septuagenarians, octogenarians, nonagenarians investigation with centenarians study. J. Am. Geriatr. Soc. 2015, 63, 2382–2387. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Yoshihara, A.; Sato, N.; Sato, M.; Taylor, G.W.; Ansai, T.; Ono, T.; Miyazaki, H. Maximum bite force at age 70 years predicts all-cause mortality during the following 13 years in Japanese men. J. Oral Rehabil. 2016, 43, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Dibello, V.; Zupo, R.; Sardone, R.; Lozupone, M.; Castellana, F.; Dibello, A.; Daniele, A.; De Pergola, G.; Bortone, I.; Lampignano, L.; et al. Oral frailty and its determinants in older age: A systematic review. Lancet Healthy Longev. 2021, 2, e507–e520. [Google Scholar] [CrossRef]
- Tanaka, T.; Takahashi, K.; Hirano, H.; Kikutani, T.; Watanabe, Y.; Ohara, Y.; Furuya, H.; Tetsuo, T.; Akishita, M.; Iijima, K. Oral Frailty as a Risk Factor for Physical Frailty and Mortality in Community-Dwelling Elderly. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1661–1667. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Hirano, H.; Ohara, Y.; Motokawa, K. The association of oral function with dietary intake and nutritional status among older adults: Latest evidence from epidemiological studies. Jpn. Dent. Sci. Rev. 2021, 57, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Motokawa, K.; Watanabe, Y.; Shirobe, M.; Ohara, Y.; Edahiro, A.; Kawai, H.; Fujiwara, Y.; Kim, H.; Ihara, K.; et al. Oral hypofunction and malnutrition among community—dwelling older adults: Evidence from the Otassha study. Gerodontology 2021, 39, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E.; Kandelman, D.; Arpin, S.; Ogawa, H. Global oral health of older people--call for public health action. Community Dent Health 2010, 27, 257–267. [Google Scholar] [PubMed]
- Shimadzu Cooperation. Shimadzu Universal Testers. Available online: https://www.quark-gulf.com/quark/public/storage/Products/gynGTetHuFjf0qnYm1f2BDZekbESroVJdtgRWX8n.pdf. (accessed on 30 March 2022).
- Kan, M.; Yoshida, H.; Fujiwara, Y.; Watanabe, N.; Tsuchiya, Y.; Shinkai, S. Longitudinal analysis of factors associated with participation in community-based mass screening for the frail elderly in need of care. Jpn. J. Public Health 2006, 53, 688–701. [Google Scholar]

| Total | Women | Men | p Value | |
|---|---|---|---|---|
| N = 596 | N = 360 | N = 236 | ||
| OFMD-CPS-measured OF (N) * | 500.3 (250.9) | 446.9 (209.9) | 581.6 (284.6) | <0.01 |
| CV of OFMD-CPS-measured OF | 0.50 | 0.47 | 0.49 | - |
| Dental Prescale II-measured OF (N) * | 814.6 (526.5) | 710.9 (439.3) | 972.7 (604.5) | <0.01 |
| CV of Dental Prescale II-measured OF | 0.65 | 0.62 | 0.62 | - |
| Dental Prescale II-measured OF <350 N † | 118 (19.8%) | 84 (23.3%) | 34 (14.4%) | 0.01 |
| No. of natural teeth ‡ | 25 (19–28) | 25 (20–27) | 25 (18–28) | 0.65 |
| <20 † natural teeth | 153 (25.7%) | 89 (24.7%) | 64 (27.1%) | 0.51 |
| No. of functional teeth ‡ | 28 (26–28) | 28 (26–28) | 28 (27–28) | 0.31 |
| Age * | 73.7 (6.7) | 73.4 (6.6) | 74.0 (6.9) | 0.34 |
| Age Group (Years) | |||||||
|---|---|---|---|---|---|---|---|
| Total | 65–69 | 70–74 | 75–79 | 80–84 | ≥85 | p for Trend | |
| Men | |||||||
| No. | 236 | 72 | 70 | 38 | 36 | 20 | |
| OF (N) * | 581.6 (284.6) | 681.4 (262.1) | 603.6 (283.3) | 551.0 (293.5) | 531.2 (265.6) | 294.7 (151.8) | <0.01 |
| Women | |||||||
| No. | 360 | 124 | 93 | 56 | 71 | 16 | |
| OF (N) * | 446.9 (209.9) | 497.3 (205.1) | 433.3 (208.5) | 465.6 (210.2) | 385.2 (201.8) | 344.8 (196.0) | <0.01 |
| Age Group (Years) | |||||||
|---|---|---|---|---|---|---|---|
| Decile | Total | 65–69 | 70–74 | 75–79 | 80–84 | ≥85 | |
| Men (No. = 236) | |||||||
| 90th | 944 | 954 | 944 | 945 | 811 | 526 | |
| 80th | 855 | 906 | 873 | 795 | 761 | 440 | |
| 70th | 763 | 855 | 787 | 752 | 684 | 406 | |
| 60th | 657 | 763 | 687 | 670 | 551 | 302 | |
| 50th (Median) | 568 | 668 | 587 | 530 | 497 | 244 | |
| 40th | 484 | 626 | 520 | 426 | 461 | 230 | |
| 30th | 413 | 550 | 451 | 339 | 327 | 174 | |
| 20th | 310 | 428 | 372 | 254 | 287 | 149 | |
| 10th | 215 | 347 | 208 | 197 | 232 | 135 | |
| Women (No. = 360) | |||||||
| 90th | 743 | 751 | 756 | 770 | 667 | 640 | |
| 80th | 608 | 660 | 585 | 652 | 547 | 510 | |
| 70th | 549 | 573 | 500 | 579 | 496 | 491 | |
| 60th | 483 | 541 | 472 | 512 | 455 | 401 | |
| 50th (Median) | 435 | 478 | 424 | 430 | 399 | 316 | |
| 40th | 390 | 442 | 371 | 401 | 312 | 226 | |
| 30th | 329 | 392 | 329 | 350 | 246 | 212 | |
| 20th | 262 | 325 | 278 | 301 | 158 | 188 | |
| 10th | 158 | 247 | 151 | 186 | 145 | 118 | |
| Variables | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|
| 1 | OFMD-CPS-measured OF | ||||
| 2 | Dental Prescale II-measured OF | 0.73 * | |||
| 3 | No. of natural teeth | 0.53 * | 0.55 * | ||
| 4 | No. of functional teeth | 0.16 * | 0.18 * | 0.47 * | |
| 5 | Age | −0.25 * | −0.14 * | −0.31 * | −0.07 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iwasaki, M.; Maeda, I.; Kokubo, Y.; Tanaka, Y.; Ueno, T.; Ohara, Y.; Motokawa, K.; Hayakawa, M.; Shirobe, M.; Edahiro, A.; et al. Standard Values and Concurrent Validity of a Newly Developed Occlusal Force-Measuring Device among Community-Dwelling Older Adults: The Otassha Study. Int. J. Environ. Res. Public Health 2022, 19, 5588. https://doi.org/10.3390/ijerph19095588
Iwasaki M, Maeda I, Kokubo Y, Tanaka Y, Ueno T, Ohara Y, Motokawa K, Hayakawa M, Shirobe M, Edahiro A, et al. Standard Values and Concurrent Validity of a Newly Developed Occlusal Force-Measuring Device among Community-Dwelling Older Adults: The Otassha Study. International Journal of Environmental Research and Public Health. 2022; 19(9):5588. https://doi.org/10.3390/ijerph19095588
Chicago/Turabian StyleIwasaki, Masanori, Ichinosuke Maeda, Yota Kokubo, Yoshitomo Tanaka, Tetsuji Ueno, Yuki Ohara, Keiko Motokawa, Misato Hayakawa, Maki Shirobe, Ayako Edahiro, and et al. 2022. "Standard Values and Concurrent Validity of a Newly Developed Occlusal Force-Measuring Device among Community-Dwelling Older Adults: The Otassha Study" International Journal of Environmental Research and Public Health 19, no. 9: 5588. https://doi.org/10.3390/ijerph19095588
APA StyleIwasaki, M., Maeda, I., Kokubo, Y., Tanaka, Y., Ueno, T., Ohara, Y., Motokawa, K., Hayakawa, M., Shirobe, M., Edahiro, A., Kawai, H., Fujiwara, Y., Ihara, K., Kim, H., Watanabe, Y., Obuchi, S., & Hirano, H. (2022). Standard Values and Concurrent Validity of a Newly Developed Occlusal Force-Measuring Device among Community-Dwelling Older Adults: The Otassha Study. International Journal of Environmental Research and Public Health, 19(9), 5588. https://doi.org/10.3390/ijerph19095588






