Effects of the Mobility-Fit Physical Activity Program on Strength and Mobility in Older Adults in Assisted Living: A Feasibility Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
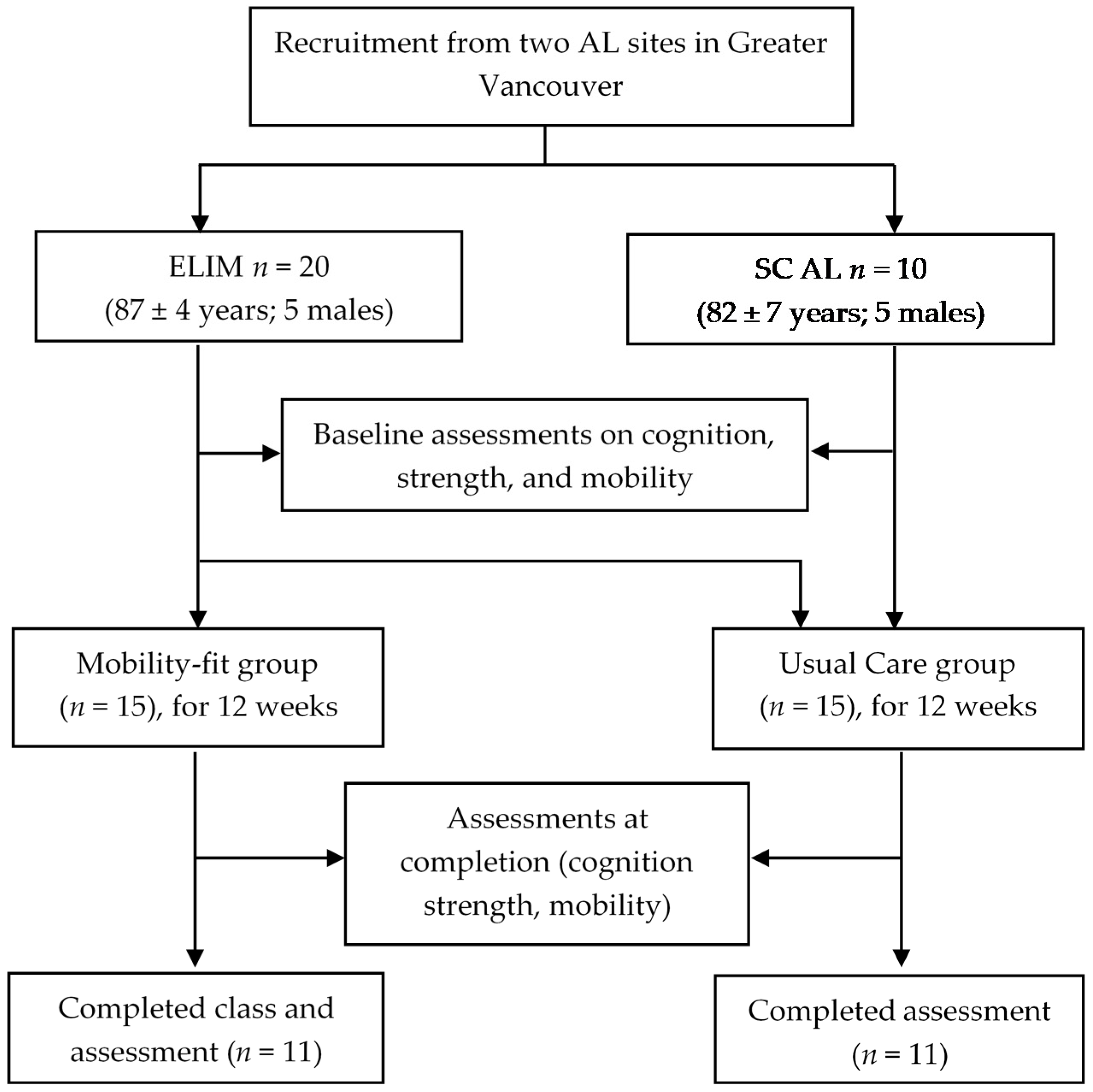
2.2. Study Design and Recruitment
2.3. Sample Size Consideration
2.4. Participant Recruitment and Group Allocation
2.5. Development and Delivery of Mobility-Fit
2.6. Quantitative Outcome Measures
2.7. Statistical Analysis
2.8. Qualitative (Implementation) Outcome Measures
3. Results
3.1. Participants Characteristics
3.2. Quantitative Outcomes
3.3. Implementation Outcomes
4. Discussion
4.1. Effects of the Mobility-Fit
4.2. Feasibility of Delivery of the Mobility-Fit
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Postl, B.; Wright, J.; Boileau, L.; Dahl, M.; Davidson, J.; Eaglem, C.; Ferguson, D.; Goel, V.; Lalumière, D.; McGarry, J.; et al. Health Care in Canada 2011—A Focus on Seniors and Aging; Canadian Institute for Health Information: Ottawa, ON, Canada, 2011. [Google Scholar]
- Aud, M.A.; Rantz, M.J. Admissions to skilled nursing facilities from assisted living facilities. J. Nurs. Care Qual. 2005, 20, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Leung, P.M.; Ejupi, A.; van Schooten, K.S.; Aziz, O.; Feldman, F.; Mackey, D.C.; Ashe, M.C.; Robinovitch, S.N. Association between Sedentary Behaviour and Physical, Cognitive, and Psychosocial Status among Older Adults in Assisted Living. Biomed. Res. Int. 2017, 2017, 9160504. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Chen, K.Y.; Freedson, P.S.; Buchowski, M.S.; Beech, B.M.; Pate, R.R.; Troiano, R.P. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008, 167, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; van Schooten, K.S.; Symes, B.; Sims-Gould, J.; McKay, H.; Leung, M.; Feldman, F.; Robinovitch, S. Recreation Therapy to Promote Mobility among Older Adults in Long-Term Care: Overview of Scientific Evidence and Current Care; Canadian Association for Long Term Care: Ottawa, ON, Canada, 2018; p. 46. [Google Scholar]
- Maki, B.E.; McIlroy, W.E. Control of rapid limb movements for balance recovery: Age-related changes and implications for fall prevention. Age Ageing 2006, 35 (Suppl. S2), ii12–ii18. [Google Scholar] [CrossRef] [PubMed]
- Janssen, W.G.; Bussmann, H.B.; Stam, H.J. Determinants of the sit-to-stand movement: A review. Phys. Ther. 2002, 82, 866–879. [Google Scholar] [CrossRef] [PubMed]
- Schonnop, R.; Yang, Y.; Feldman, F.; Robinson, E.; Loughin, M.; Robinovitch, S.N. Prevalence of and factors associated with head impact during falls in older adults in long-term care. CMAJ 2013, 185, E803–E810. [Google Scholar] [CrossRef]
- Robinovitch, S.N.; Feldman, F.; Yang, Y.; Schonnop, R.; Leung, P.M.; Sarraf, T.; Sims-Gould, J.; Loughin, M. Video capture of the circumstances of falls in elderly people residing in long-term care: An observational study. Lancet 2013, 381, 47–54. [Google Scholar] [CrossRef]
- Yang, Y.; Mackey, D.C.; Liu-Ambrose, T.; Leung, P.M.; Feldman, F.; Robinovitch, S.N. Clinical Risk Factors for Head Impact During Falls in Older Adults: A Prospective Cohort Study in Long-Term Care. J. Head Trauma Rehabil. 2017, 32, 168–177. [Google Scholar] [CrossRef]
- Carter, N.D.; Khan, K.M.; McKay, H.A.; Petit, M.A.; Waterman, C.; Heinonen, A.; Janssen, P.A.; Donaldson, M.G.; Mallinson, A.; Riddell, L.; et al. Community-based exercise program reduces risk factors for falls in 65- to 75-year-old women with osteoporosis: Randomized controlled trial. CMAJ 2002, 167, 997–1004. [Google Scholar]
- Arnold, C.M.; Walker-Johnston, J.; Lanovaz, J.L.; Lattimer, L.J. Does Fall Arrest Strategy Training Added to a Fall Prevention Programme Improve Balance, Strength, and Agility in Older Women? A Pilot Study. Physiother. Can. 2017, 69, 323–332. [Google Scholar] [CrossRef]
- Lancaster, G.A. Pilot and feasibility studies come of age! Pilot Feasibility Stud. 2015, 1, 1. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and analysis of pilot studies: Recommendations for good practice. J. Eval. Clin. Pract. 2004, 10, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Pluijm, S.M.; Smit, J.H.; Tromp, E.A.; Stel, V.S.; Deeg, D.J.; Bouter, L.M.; Lips, P. A risk profile for identifying community-dwelling elderly with a high risk of recurrent falling: Results of a 3-year prospective study. Osteoporos. Int. 2006, 17, 417–425. [Google Scholar] [CrossRef]
- Peeters, G.M.; Pluijm, S.M.; van Schoor, N.M.; Elders, P.J.; Bouter, L.M.; Lips, P. Validation of the LASA fall risk profile for recurrent falling in older recent fallers. J. Clin. Epidemiol. 2010, 63, 1242–1248. [Google Scholar] [CrossRef][Green Version]
- Kempen, G.I.; Yardley, L.; Van Haastregt, J.C.; Zijlstra, G.R.; Beyer, N.; Hauer, K.; Todd, C. The Short FES-I: A shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 2008, 37, 45–50. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Lord, S.R.; Menz, H.B.; Tiedemann, A. A physiological profile approach to falls risk assessment and prevention. Phys. Ther. 2003, 83, 237–252. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef]
- Kerby, D.S. The simple difference formula: An approach to teaching nonparametric correlation. Compr. Psychol. 2014, 3, 11-IT. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Harvey, J.A.; Chastin, S.F.; Skelton, D.A. How Sedentary are Older People? A Systematic Review of the Amount of Sedentary Behavior. J. Aging Phys. Act. 2015, 23, 471–487. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.; Castell, S. Effect of exercise on balance, strength and reaction time in older people. Aust. J. Physiother. 1994, 40, 83–88. [Google Scholar] [CrossRef]
- Ma, H.I.; Trombly, C.A. Effects of task complexity on reaction time and movement kinematics in elderly people. Am. J. Occup. Ther. 2004, 58, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Irez, G.B.; Ozdemir, R.A.; Evin, R.; Irez, S.G.; Korkusuz, F. Integrating pilates exercise into an exercise program for 65+ year-old women to reduce falls. J. Sports Sci. Med. 2011, 10, 105–111. [Google Scholar]
- Sran, M.M.; Stotz, P.J.; Normandin, S.C.; Robinovitch, S.N. Age differences in energy absorption in the upper extremity during a descent movement: Implications for arresting a fall. J. Gerontol. Biol. Sci. Med. Sci. 2010, 65, 312–317. [Google Scholar] [CrossRef]
- Choi, W.J.; Wakeling, J.M.; Robinovitch, S.N. Kinematic analysis of video-captured falls experienced by older adults in long-term care. J. Biomech. 2015, 48, 911–920. [Google Scholar] [CrossRef]
- Bossers, W.J.; Scherder, E.J.; Boersma, F.; Hortobagyi, T.; van der Woude, L.H.; van Heuvelen, M.J. Feasibility of a combined aerobic and strength training program and its effects on cognitive and physical function in institutionalized dementia patients. A pilot study. PLoS ONE 2014, 9, e97577. [Google Scholar] [CrossRef]
- Kwon, S.; Perera, S.; Pahor, M.; Katula, J.A.; King, A.C.; Groessl, E.J.; Studenski, S.A. What is a meaningful change in physical performance? Findings from a clinical trial in older adults (the LIFE-P study). J. Nutr. Health Aging 2009, 13, 538–544. [Google Scholar] [CrossRef]
- Litchke, L.G.; Hodges, J.S.; Reardon, R.F. Benefits of Chair Yoga for Persons with Mild to Severe Alzheimer’s Disease. Act. Adapt. Aging 2012, 36, 317–328. [Google Scholar] [CrossRef]
- Brill, P.A.; Matthews, M.; Mason, J.; Davis, D.; Mustafa, T.A.; Macera, C. Improving functional performance through a group-based free weight strength training program in residents of two assisted living communities. Phys. Occup. Ther. Geriatr. 1998, 15, 57–69. [Google Scholar] [CrossRef]
- Wallmann, H.; Schuerman, S.; Kruskall, L.; Alpert, P.T. Administration of an exercise regimen in assisted-living facilities to improve balance and activities of daily living: A pilot study. Home Health Care Manag. Care 2009, 21, 419–426. [Google Scholar] [CrossRef]
- Tak, E.C.; van Hespen, A.; van Dommelen, P.; Hopman-Rock, M. Does improved functional performance help to reduce urinary incontinence in institutionalized older women? A multicenter randomized clinical trial. BMC Geriatr. 2012, 12, 51. [Google Scholar] [CrossRef]
- Fu, A.S.; Gao, K.L.; Tung, A.K.; Tsang, W.W.; Kwan, M.M. Effectiveness of Exergaming Training in Reducing Risk and Incidence of Falls in Frail Older Adults with a History of Falls. Arch. Phys. Med. Rehabil. 2015, 96, 2096–2102. [Google Scholar] [CrossRef]
- Chen, K.-M.; Chen, W.-T.; Wang, J.-J.; Huang, M.-F. Frail elders’ views of Tai Chi. J. Nurs. Res. 2005, 13, 11–20. [Google Scholar] [CrossRef]
| Baseline Characteristics | Mobility-Fit (n = 15) | Usual Care (n = 15) | p-Value |
|---|---|---|---|
| Age (years; mean, SD) | 87 (5.1) | 84 (6.7) | 0.084 |
| Female (n, %) | 11 (73.3%) | 9 (60.0%) | 0.700 |
| Length of stay (years; mean, SD) | 3.1 (3.0) | 1.8 (1.1) | 0.132 |
| Use of mobility aids (n, %) | 6 (40.0%) | 10 (66.7%) | 0.272 |
| Body mass index (mean, SD) | 23.2 (3.1) | 27.9 (5.8) | 0.020 |
| Self-reported having fall(s) in past year (n, %) | 5 (33.3%) | 9 (60.0%) | 0.272 |
| Mobility-Fit (n = 11) | Usual Care (n = 11) | Comparison | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-Test (T0) | Post-Test (T1) | Change from T0 to T1 | Pre-Test (T0) | Post-Test (T1) | Change from T0 to T1 | Mann Whitney U | Common Language Effect Size f | p-Value | |
| Fall risk and cognitive function | |||||||||
| LASA fall risk score | 4.2 (2.8–5.7) | 3.6 (2.2–4.9) | −14% | 4.7 (2.4–8.0) | 5.2 (3.4–7.1) | 11% | 31.00 | 0.26 m | 0.056 |
| FES-I score | 5.2 (3.2–7.3) | 3.8 (2.6–5.3) | −28% | 9.3 (7.6–11.1) | 9.4 (8.1–11.2) | 1% | 33.00 | 0.27 m | 0.076 |
| MoCA score | 21.3 (10.8–25.1) | 22.4 (19.4–25.3) | 5% | 21.7 (20.1–23.3) | 22.1 (20.7–23.6) | 2% | 75.00 | 0.62 l | 0.365 |
| Strength | |||||||||
| Dominant hand grip (kg) * | 20.9 (17.2–26.3) | 20.9 (17.9–24.7) | 0% | 21.9 (16.2–28.9) | 20.6 (14.3–28.0) | −6% | 91.00 | 0.75 l | 0.047 |
| Knee extension strength (kg) *,# | 20.9 (18.0–23.8) | 22.2 (18.9–25.6) | 6% | 23.4 (18.9–28.6) | 21.5 (16.6–27.4) | −8% | 78.00 | 0.79 l | 0.031 |
| Mobility | |||||||||
| Timed Up and Go (s) | 12.9 (11.0–15.4) | 13.0 (10.9–15.6) | 1% | 20.6 (16.9–24.1) | 23.0 (17.6–28.8) | 12% | 46.00 | 0.38 m | 0.365 |
| SPPB score | 8.3 (6.9–9.5) | 8.6 (7.6–9.4) | 4% | 5.0 (4.2–5.8) | 5.0 (4.3–5.7) | 0% | 70.50 | 0.58 l | 0.519 |
| 5 time sit-to-stand (s) * | 19.8 (16.6–23.3) | 16.9 (15.3–18.6) | −15% | 21.4 (18.5–24.6) | 25.2 (20.1–30.4) | 18% | 28.00 | 0.23 m | 0.034 |
| 10-m gait speed (m/s) | 1.08 (0.90–1.24) | 1.11 (0.94–1.27) | 3% | 0.73 (0.62–0.85) | 0.75 (0.64–0.87) | 3% | 59.00 | 0.49 l | 0.949 |
| Reaction time (s) * | 0.38 (0.30–0.46) | 0.32 (0.26–0.39) | −16% | 0.31 (0.25–0.36) | 0.37 (0.29–0.48) | 19% | 24.00 | 0.20 m | 0.016 |
| Question | Rating by Participants | ||||
|---|---|---|---|---|---|
| How did you like the program? | Excellent (0%) | Very good (66.7%) | Good (22.2%) | Average (0%) | Fair (11.1%) |
| Did the program benefit you? | Extremely (0%) | Very much (55.6%) | Somewhat (44.4%) | Minimally (0%) | No benefit (0%) |
| How often did you participate? | All the time (11.1%) | Most of the time (88.9%) | Sometimes (0%) | Barely (0%) | Never (0%) |
| Timing of the class? | Very convenient (11.1%) | Convenient (66.7%) | Somewhat (22.2%) | Not convenient (0%) | |
| Any lifestyle changes? | Definitely yes (0%) | Most likely (44.4%) | Maybe (44.4%) | Most likely not (11.1%) | Definitely not (0%) |
| Would you participate again? | Definitely yes (55.6%) | Most likely (33.3%) | Maybe (11.1%) | Most likely not (0%) | Definitely not (0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.; van Schooten, K.S.; Komisar, V.; McKay, H.A.; Sims-Gould, J.; Cheong, D.; Robinovitch, S.N. Effects of the Mobility-Fit Physical Activity Program on Strength and Mobility in Older Adults in Assisted Living: A Feasibility Study. Int. J. Environ. Res. Public Health 2022, 19, 5453. https://doi.org/10.3390/ijerph19095453
Yang Y, van Schooten KS, Komisar V, McKay HA, Sims-Gould J, Cheong D, Robinovitch SN. Effects of the Mobility-Fit Physical Activity Program on Strength and Mobility in Older Adults in Assisted Living: A Feasibility Study. International Journal of Environmental Research and Public Health. 2022; 19(9):5453. https://doi.org/10.3390/ijerph19095453
Chicago/Turabian StyleYang, Yijian, Kimberley S. van Schooten, Vicki Komisar, Heather A. McKay, Joanie Sims-Gould, Debbie Cheong, and Stephen N. Robinovitch. 2022. "Effects of the Mobility-Fit Physical Activity Program on Strength and Mobility in Older Adults in Assisted Living: A Feasibility Study" International Journal of Environmental Research and Public Health 19, no. 9: 5453. https://doi.org/10.3390/ijerph19095453
APA StyleYang, Y., van Schooten, K. S., Komisar, V., McKay, H. A., Sims-Gould, J., Cheong, D., & Robinovitch, S. N. (2022). Effects of the Mobility-Fit Physical Activity Program on Strength and Mobility in Older Adults in Assisted Living: A Feasibility Study. International Journal of Environmental Research and Public Health, 19(9), 5453. https://doi.org/10.3390/ijerph19095453








