Predictors of Uncertainty and Unwillingness to Receive the COVID-19 Vaccine in Men Who Have Sex with Men in France
Abstract
:1. Introduction
2. Materials and Methods
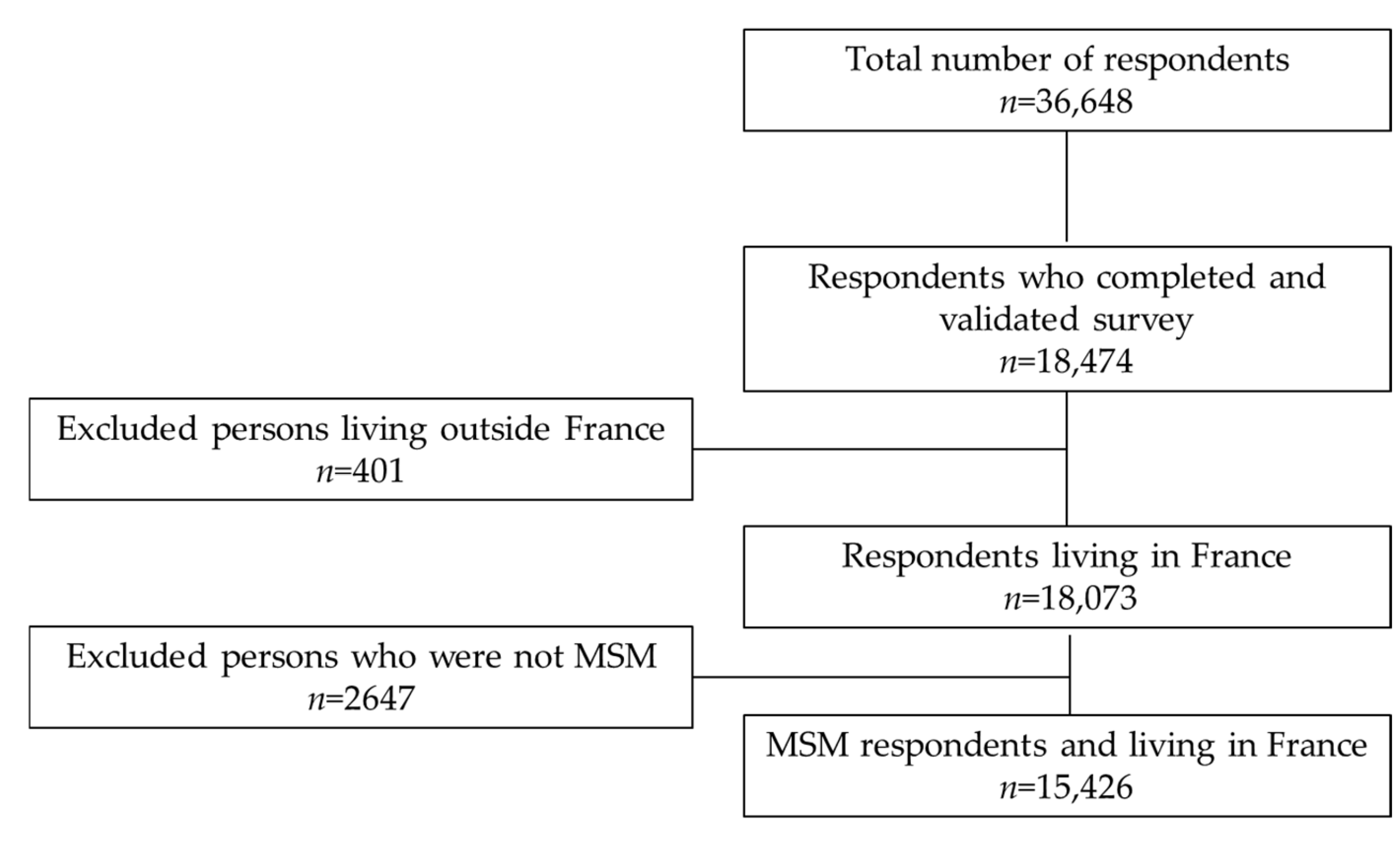
2.1. Study Design and Participants
2.2. Data Collection
2.2.1. Outcome: Intention to Vaccinate against COVID-19
2.2.2. Independent Variables
2.3. Statistical Analysis
3. Results
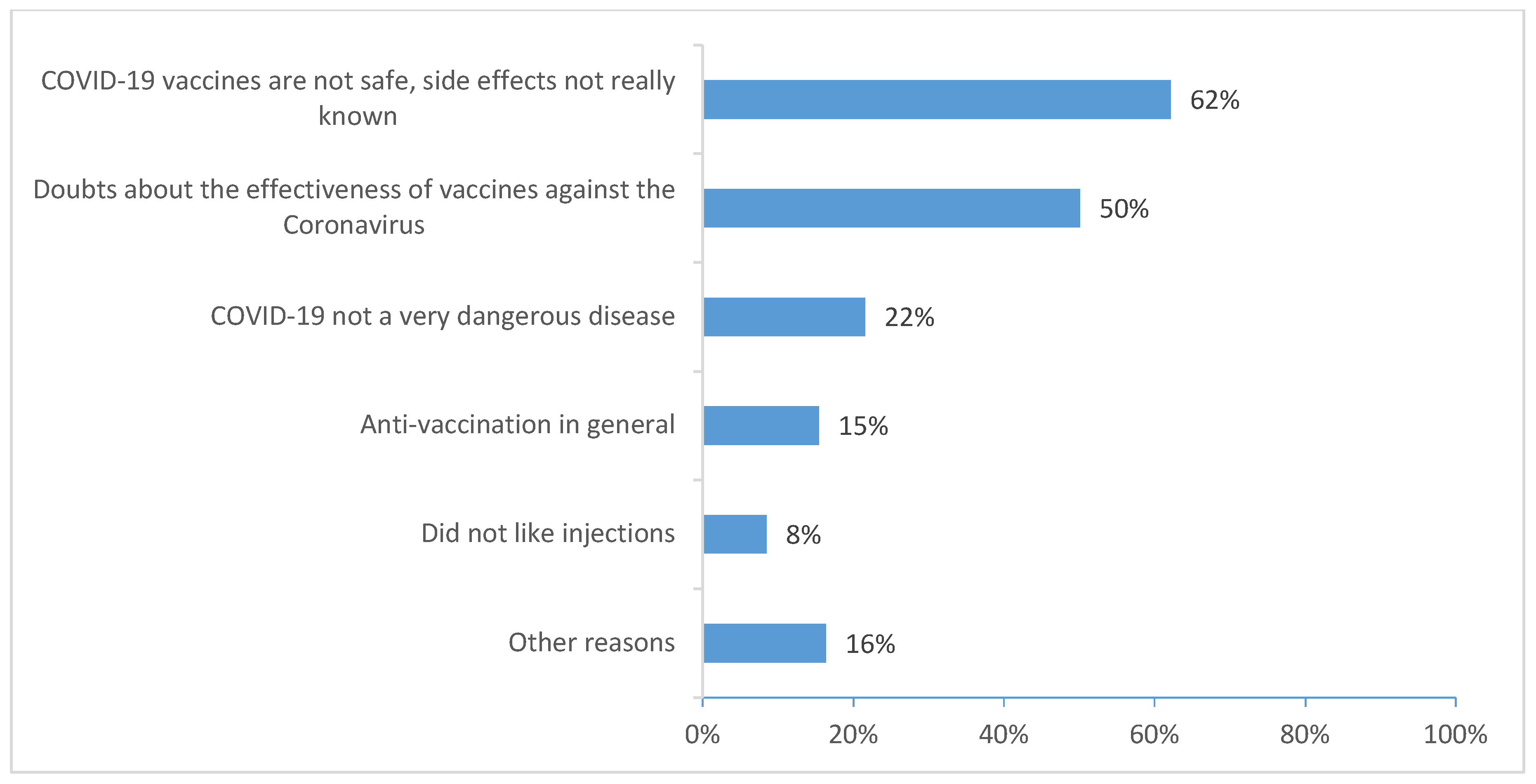
Factors Associated with Uncertainty and Unwillingness to Receive the COVID-19 Vaccine
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the MRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 MRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and Efficacy of the ChAdOx1 NCoV-19 Vaccine (AZD1222) against SARS-CoV-2: An Interim Analysis of Four Randomised Controlled Trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Jabłońska, K.; Aballéa, S.; Toumi, M. The Real-Life Impact of Vaccination on COVID-19 Mortality in Europe and Israel. Public Health 2021, 198, 230–237. [Google Scholar] [CrossRef]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 2021, 9, 16. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A Global Survey of Potential Acceptance of a COVID-19 Vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Alleaume, C.; Verger, P.; Dib, F.; Ward, J.K.; Launay, O.; Peretti-Watel, P. Intention to Get Vaccinated against COVID-19 among the General Population in France: Associated Factors and Gender Disparities. Hum. Vaccines Immunother. 2021, 17, 3421–3432. [Google Scholar] [CrossRef]
- Nguyen, K.H.; Nguyen, K.; Corlin, L.; Allen, J.D.; Chung, M. Changes in COVID-19 Vaccination Receipt and Intention to Vaccinate by Socioeconomic Characteristics and Geographic Area, United States, January 6–March 29, 2021. Ann. Med. 2021, 53, 1419–1428. [Google Scholar] [CrossRef]
- Melin, K.; Zhang, C.; Zapata, J.P.; Rivera, Y.M.; Fernandez, K.; Shacham, E.; Malavé-Rivera, S.M.; Rodriguez-Diaz, C.E. Factors Associated with Intention to Receive Vaccination against COVID-19 in Puerto Rico: An Online Survey of Adults. Int. J. Environ. Res. Public Health 2021, 18, 7743. [Google Scholar] [CrossRef]
- Ruiz, J.B.; Bell, R.A. Predictors of Intention to Vaccinate against COVID-19: Results of a Nationwide Survey. Vaccine 2021, 39, 1080–1086. [Google Scholar] [CrossRef]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 Vaccine Hesitancy in a Representative Working-Age Population in France: A Survey Experiment Based on Vaccine Characteristics. Lancet Public Health 2021, 6, e210–e221. [Google Scholar] [CrossRef]
- Velter, A.; Champenois, K.; Castro, D.; Lydie, N. Perceived Impact of the COVID-19 Pandemic on Men Who Have Sex with Men in France. Eras COVID-19 Survey, 30 June-15 July 2020.(Dépistage Du VIH: Nouvelles Expérimentations, Données de Surveillance et Impact de La COVID.) [French]. Bull. Epidemiol. Hebd. 2020, 33, 666–672. [Google Scholar]
- Santos, G.-M.; Ackerman, B.; Rao, A.; Wallach, S.; Ayala, G.; Lamontage, E.; Garner, A.; Holloway, I.W.; Arreola, S.; Silenzio, V. Economic, Mental Health, HIV Prevention and HIV Treatment Impacts of COVID-19 and the COVID-19 Response on a Global Sample of Cisgender Gay Men and Other Men Who Have Sex with Men. AIDS Behav. 2021, 25, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Camargo, E.L.S.; de Oliveira, B.I.A.; Siffoni, I.F.; de Sousa, A.R.; Teixeira, J.R.B.; Mendes, I.A.C.; de Sousa, Á.F.L. Low Psychological Well-Being in Men Who Have Sex with Men (MSM) During the Shelter-in-Place Orders to Prevent the COVID-19 Spread: Results from a Nationwide Study. Sex. Res. Soc. Policy 2021, 19, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Torres, T.S.; Hoagland, B.; Bezerra, D.R.; Garner, A.; Jalil, E.M.; Coelho, L.E.; Benedetti, M.; Pimenta, C.; Grinsztejn, B.; Veloso, V.G. Impact of COVID-19 Pandemic on Sexual Minority Populations in Brazil: An Analysis of Social/Racial Disparities in Maintaining Social Distancing and a Description of Sexual Behavior. AIDS Behav. 2021, 25, 73–84. [Google Scholar] [CrossRef]
- Gibb, J.K.; DuBois, L.Z.; Williams, S.; McKerracher, L.; Juster, R.-P.; Fields, J. Sexual and Gender Minority Health Vulnerabilities during the COVID-19 Health Crisis. Am. J. Hum. Biol. Off. J. Hum. Biol. Counc. 2020, 32, e23499. [Google Scholar] [CrossRef]
- Pachankis, J.; Hatzenbuehler, M.; Berg, R.; Fernández-Dávila, P.; Mirandola, M.; Marcus, U.; Weatherburn, P.; Schmidt, A. An Intersectional Analysis of Sexual Minority Men’s HIV Risk When Migrating to or within Europe. Eur. J. Public Health 2018, 28, cky213.790. [Google Scholar] [CrossRef]
- Ross, M.W.; Berg, R.C.; Schmidt, A.J.; Hospers, H.J.; Breveglieri, M.; Furegato, M.; Weatherburn, P. Internalised Homonegativity Predicts HIV-Associated Risk Behavior in European Men Who Have Sex with Men in a 38-Country Cross-Sectional Study: Some Public Health Implications of Homophobia. BMJ Open 2013, 3, e001928. [Google Scholar] [CrossRef] [Green Version]
- Montagni, I.; Ouazzani-Touhami, K.; Mebarki, A.; Texier, N.; Schück, S.; Tzourio, C. Acceptance of a COVID-19 Vaccine Is Associated with Ability to Detect Fake News and Health Literacy. J. Public Health Oxf. Engl. 2021, 43, 695–702. [Google Scholar] [CrossRef]
- Turhan, Z.; Dilcen, H.Y.; Dolu, İ. The Mediating Role of Health Literacy on the Relationship between Health Care System Distrust and Vaccine Hesitancy during COVID-19 Pandemic. Curr. Psychol. 2021, 1–10. [Google Scholar] [CrossRef]
- Lin, Y.-J.; Chang, Y.-P.; Chou, W.-J.; Yen, C.-F. Explicit and Intrinsic Intention to Receive COVID-19 Vaccination among Heterosexuals and Sexual Minorities in Taiwan. Int. J. Environ. Res. Public. Health 2021, 18, 7260. [Google Scholar] [CrossRef] [PubMed]
- Teixeira da Silva, D.; Biello, K.; Lin, W.Y.; Valente, P.K.; Mayer, K.H.; Hightow-Weidman, L.; Bauermeister, J.A. COVID-19 Vaccine Acceptance among an Online Sample of Sexual and Gender Minority Men and Transgender Women. Vaccines 2021, 9, 204. [Google Scholar] [CrossRef] [PubMed]
- Osborne, R.H.; Batterham, R.W.; Elsworth, G.R.; Hawkins, M.; Buchbinder, R. The Grounded Psychometric Development and Initial Validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013, 13, 658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Debussche, X.; Lenclume, V.; Balcou-Debussche, M.; Alakian, D.; Sokolowsky, C.; Ballet, D.; Elsworth, G.R.; Osborne, R.H.; Huiart, L. Characterisation of Health Literacy Strengths and Weaknesses among People at Metabolic and Cardiovascular Risk: Validity Testing of the Health Literacy Questionnaire. SAGE Open Med. 2018, 6, 2050312118801250. [Google Scholar] [CrossRef] [Green Version]
- Public Health England Disparities in the Risk and Outcomes of COVID-19; Public Health England: London, UK, 2020.
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once We Have It, Will We Use It? A European Survey on Willingness to Be Vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef]
- CoviPrev: Une Enquête Pour Suivre L’évolution des Comportements et de la Santé Mentale Pendant L’épidémie de COVID-19. Available online: https://www.santepubliquefrance.fr/etudes-et-enquetes/coviprev-une-enquête-pour-suivre-l’évolution-des-comportements-et-de-la-sante-mentale-pendant-l-epidemie-de-covid-19 (accessed on 2 November 2021).
- Al-Amer, R.; Maneze, D.; Everett, B.; Montayre, J.; Villarosa, A.R.; Dwekat, E.; Salamonson, Y. COVID-19 Vaccination Intention in the First Year of the Pandemic: A Systematic Review. J. Clin. Nurs. 2022, 31, 62–86. [Google Scholar] [CrossRef]
- Jung, H.; Albarracín, D. Concerns for Others Increase the Likelihood of Vaccination against Influenza and COVID-19 More in Sparsely Rather than Densely Populated Areas. Proc. Natl. Acad. Sci. USA 2021, 118, e2007538118. [Google Scholar] [CrossRef]
- Dodd, R.H.; Cvejic, E.; Bonner, C.; Pickles, K.; McCaffery, K.J.; Ayre, J.; Batcup, C.; Copp, T.; Cornell, S.; Dakin, T.; et al. Willingness to Vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021, 21, 318–319. [Google Scholar] [CrossRef]
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlôt, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 Vaccination Intention in the UK: Results from the COVID-19 Vaccination Acceptability Study (CoVAccS), a Nationally Representative Cross-Sectional Survey. Hum. Vaccines Immunother. 2021, 17, 1612–1621. [Google Scholar] [CrossRef]
- Ala, A.; Wilder, J.; Jonassaint, N.L.; Coffin, C.S.; Brady, C.; Reynolds, A.; Schilsky, M.L. COVID-19 and the Uncovering of Health Care Disparities in the United States, United Kingdom and Canada: Call to Action. Hepatol. Commun. 2021, 5, 1791–1800. [Google Scholar] [CrossRef]
- Alcendor, D.J.; Juarez, P.D.; Matthews-Juarez, P.; Simon, S.; Nash, C.; Lewis, K.; Smoot, D. Meharry Medical College Mobile Vaccination Program: Implications for Increasing COVID-19 Vaccine Uptake among Minority Communities in Middle Tennessee. Vaccines 2022, 10, 211. [Google Scholar] [CrossRef] [PubMed]
- Ribera-Cano, A.; Dupont, M.; Houzé-Cerfon, C.-H.; Houzé-Cerfon, V.; Hart, A.; Hertelendy, A.J.; Ciottone, G.; Bounes, V. Evaluation of a Prototype Decontamination Mobile Unit (UMDEO) for COVID-19 Vaccination: A Cross-Sectional Survey in France. Vaccine 2021, 39, 7441–7445. [Google Scholar] [CrossRef] [PubMed]
- Prah, P.; Hickson, F.; Bonell, C.; McDaid, L.M.; Johnson, A.M.; Wayal, S.; Clifton, S.; Sonnenberg, P.; Nardone, A.; Erens, B.; et al. Men Who Have Sex with Men in Great Britain: Comparing Methods and Estimates from Probability and Convenience Sample Surveys. Sex. Transm. Infect. 2016, 92, 455–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Velter, A.; Saboni, L.; Bouyssou, A.; Bernillon, P.; Sommen, C.; Semaille, C. Echantillons de Convenance Par Internet et Par La Presse—Enquête Presse Gays et Lesbiennes 2011. Bull. Sociol. Methodol. Méthodologie Sociol. 2015, 126, 46–66. [Google Scholar] [CrossRef]
- Beyrer, C.; Baral, S.D.; van Griensven, F.; Goodreau, S.M.; Chariyalertsak, S.; Wirtz, A.L.; Brookmeyer, R. Global Epidemiology of HIV Infection in Men Who Have Sex with Men. Lancet Lond. Engl. 2012, 380, 367–377. [Google Scholar] [CrossRef] [Green Version]
- Point Epidémiologique COVID-19 du 21 Octobre 2021—Augmentation de L’incidence du SARS-CoV-2: La Plus Grande Vigilance Doit être Apportée Dans un Contexte de Circulation des Virus Hivernaux. Available online: https://www.santepubliquefrance.fr/presse/2021/point-epidemiologique-covid-19-du-21-octobre-2021-augmentation-de-l-incidence-du-sars-cov-2-la-plus-grande-vigilance-doit-etre-apportee-dans-un (accessed on 5 November 2021).
| n | % | |
|---|---|---|
| Age, median [IQR] (years) | 33 [25–44] | |
| 18–24 | 3828 | 24.8 |
| 25–29 | 2557 | 16.6 |
| 30–44 | 5238 | 34 |
| ≥45 | 3803 | 24.7 |
| Place of birth | ||
| Outside France | 834 | 5.4 |
| France | 14,592 | 94.6 |
| Area of residence | ||
| Rural | 2653 | 17.2 |
| Urban | 12,773 | 82.8 |
| Education level | ||
| Lower than upper secondary school certificate | 2328 | 15.1 |
| Upper secondary school certificate | 2583 | 16.7 |
| Third-level | 10,515 | 68.2 |
| Health literacy | ||
| Low | 4804 | 31.1 |
| Adequate | 10,622 | 68.9 |
| In a steady relationship with a man | ||
| No (Single/separated/other) | 8207 | 46.8 |
| Yes (Married/cohabitation/civil partnership) | 7219 | 53.2 |
| Occupation | ||
| Employee, self-employed | 10,164 | 65.9 |
| Unemployed, not active or retired | 2324 | 15.1 |
| Student | 2938 | 19 |
| Perceived financial situation | ||
| Comfortable | 8978 | 58.2 |
| Need to be careful | 4294 | 27.8 |
| Difficulty and debt | 2154 | 14 |
| Biomedical status | ||
| HIV negative and PrEP user | 1504 | 9.7 |
| HIV negative | 10,002 | 64.8 |
| HIV positive | 1023 | 6.6 |
| Unknown HIV status | 2897 | 18.8 |
| Had COVID-19-type symptoms | ||
| No | 8877 | 57.5 |
| Yes | 6549 | 42.5 |
| Diagnosed with COVID-19 | ||
| No | 13,937 | 90.3 |
| Yes | 1489 | 9.7 |
| Vaccination history (vaccinated against Hepatitis A or B) | ||
| No | 5279 | 34.2 |
| Yes | 10,147 | 65.8 |
| Intention to vaccinate against COVID-19 | ||
| Willing (already vaccinated and intended) | 9335 | 60.5 |
| Uncertain | 3399 | 22 |
| Unwilling | 2692 | 17.5 |
| Intention to Get Vaccinations against COVID-19 | |||||||
|---|---|---|---|---|---|---|---|
| Willing n = 9335 | Uncertainly n = 3399 | Unwillingness n = 2692 | |||||
| n | % | n | % | n | % | p-Value | |
| Age (years) | *** | ||||||
| 18–24 | 2008 | 52.5 | 1029 | 26.9 | 791 | 20.7 | |
| 25–29 | 1391 | 54.4 | 595 | 23.3 | 571 | 22.3 | |
| 30–44 | 3077 | 58.7 | 1218 | 23.3 | 943 | 18 | |
| ≥45 | 2859 | 75.2 | 557 | 14.6 | 387 | 10.2 | |
| Place of birth | *** | ||||||
| Outside France | 595 | 71.3 | 149 | 17.9 | 90 | 10.8 | |
| France | 8740 | 59.9 | 3250 | 22.3 | 2602 | 17.8 | |
| Area of residence | *** | ||||||
| Rural | 1287 | 48.5 | 686 | 25.9 | 680 | 25.6 | |
| Urban | 8048 | 63 | 2713 | 21.2 | 2012 | 15.8 | |
| Education level | *** | ||||||
| Lower than upper secondary school certificate | 1010 | 43.4 | 627 | 26.9 | 691 | 29.7 | |
| Upper secondary school certificate | 1228 | 47.5 | 716 | 27.7 | 639 | 24.7 | |
| Third-level | 7097 | 67.5 | 2056 | 19.6 | 1362 | 13 | |
| Health literacy | *** | ||||||
| Low | 2679 | 55.8 | 1179 | 24.5 | 946 | 19.7 | |
| Adequate | 6656 | 62.7 | 2220 | 20.9 | 1746 | 16.4 | |
| In a steady relationship with a man | *** | ||||||
| No (Single/separated/other) | 4724 | 57.6 | 1903 | 23.2 | 1580 | 19.3 | |
| Yes (Married/cohabitation/civil partnership) | 4611 | 63.9 | 1496 | 20.7 | 1112 | 15.4 | |
| Occupation | *** | ||||||
| Employee, self-employed | 6316 | 62.1 | 2155 | 21.2 | 1693 | 16.7 | |
| Unemployed, not active or retired | 1304 | 56.1 | 506 | 21.8 | 514 | 22.1 | |
| Student | 1715 | 58.4 | 738 | 25.1 | 485 | 16.5 | |
| Perceived financial situation | *** | ||||||
| Comfortable | 6021 | 67.1 | 1771 | 19.7 | 1186 | 13.2 | |
| Need to be careful | 2328 | 54.2 | 1065 | 24.8 | 901 | 21 | |
| Difficulty and debt | 986 | 45.8 | 563 | 26.1 | 605 | 28.1 | |
| Biomedical status | *** | ||||||
| HIV negative and PrEP user | 1134 | 75.4 | 250 | 16.6 | 120 | 8 | |
| HIV negative | 5946 | 59.4 | 2253 | 22.5 | 1803 | 18 | |
| HIV positive | 801 | 78.3 | 134 | 13.1 | 88 | 8.6 | |
| Unknown HIV status | 1454 | 50.2 | 762 | 26.3 | 681 | 23.5 | |
| Vaccination history (vaccinated against Hepatitis A or B) | *** | ||||||
| No | 2739 | 51.9 | 1353 | 25.6 | 1187 | 22.5 | |
| Yes | 6596 | 65 | 2046 | 20.2 | 1505 | 14.8 | |
| Had symptoms or signs of COVID-19 | *** | ||||||
| No | 5290 | 59.6 | 1944 | 21.9 | 1643 | 18.5 | |
| Yes | 4045 | 61.8 | 1455 | 22.2 | 1049 | 16 | |
| Diagnosed with COVID-19 | *** | ||||||
| No | 8351 | 59.9 | 3105 | 22.3 | 2481 | 17.8 | |
| Yes | 984 | 66.1 | 294 | 19.7 | 211 | 14.2 | |
| Uncertainly vs. Acceptance | Unwillingness vs. Acceptance | |||
|---|---|---|---|---|
| ORa | 95%CI | ORa | 95%CI | |
| Age (years) | ||||
| 18–24 | 1.26 | 1.09–1.45 | 1.34 | 1.15–1.56 |
| 25–29 | 1.10 | 0.98–1.24 | 1.41 | 1.24–1.61 |
| 30–44 | 1 | 1 | ||
| ≥45 | 0.44 | 0.39–0.50 | 0.36 | 0.31–0.42 |
| Place of birth | ||||
| Outside France | 1 | 1 | ||
| France | 1.33 | 1.10–1.61 | 1.67 | 1.32–2.12 |
| Area of residence | ||||
| Rural | 1.40 | 1.26–1.56 | 1.71 | 1.52–1.91 |
| Urban | 1 | 1 | ||
| Education level | ||||
| Lower than upper secondary school certificate | 2.12 | 1.88–2.39 | 3.09 | 2.72–3.51 |
| Upper secondary school certificate | 1.78 | 1.60–1.99 | 2.11 | 1.87–2.38 |
| Third-level | 1 | 1 | ||
| Health literacy | ||||
| Low | 1.21 | 1.11–1.32 | 1.19 | 1.08–1.32 |
| Adequate | 1 | 1 | ||
| In a steady relationship with a man | ||||
| No (Single/separated/other) | 1 | 1 | ||
| Yes (Married/cohabitant/civil partnership) | 0.86 | 0.79–0.94 | 0.79 | 0.72–0.87 |
| Occupation | ||||
| Employee, self-employed | 1 | 1 | ||
| Unemployed, not active or retired | 0.98 | 0.86–1.11 | 1.08 | 0.95–1.23 |
| Student | 0.83 | 0.72–0.96 | 0.66 | 0.56–0.77 |
| Perceived financial situation | ||||
| Comfortable | 1 | 1 | ||
| Need to be careful | 1.39 | 1.26–1.52 | 1.65 | 1.49–1.84 |
| Difficulty and debt | 1.61 | 1.42–1.83 | 2.31 | 2.02–2.63 |
| HIV status | ||||
| HIV negative and PrEP user | 0.74 | 0.62–0.89 | 0.45 | 0.36–0.57 |
| HIV negative | 0.98 | 0.88–1.10 | 0.93 | 0.83–1.05 |
| HIV positive | 0.57 | 0.46–0.71 | 0.44 | 0.34–0.58 |
| Unknown HIV status | 1 | 1 | ||
| Vaccination history (vaccinated against Hepatitis A or B or HPV) | ||||
| No | 1 | 1 | ||
| Yes | 0.74 | 0.67–0.80 | 0.67 | 0.61–0.74 |
| Had symptoms or signs of COVID-19 | ||||
| No | 1 | 1 | ||
| Yes | 0.93 | 0.85–1.01 | 0.81 | 0.74–0.89 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ousseine, Y.M.; Vaux, S.; Vandentorren, S.; Bonmarin, I.; Champenois, K.; Lydié, N.; Velter, A. Predictors of Uncertainty and Unwillingness to Receive the COVID-19 Vaccine in Men Who Have Sex with Men in France. Int. J. Environ. Res. Public Health 2022, 19, 5372. https://doi.org/10.3390/ijerph19095372
Ousseine YM, Vaux S, Vandentorren S, Bonmarin I, Champenois K, Lydié N, Velter A. Predictors of Uncertainty and Unwillingness to Receive the COVID-19 Vaccine in Men Who Have Sex with Men in France. International Journal of Environmental Research and Public Health. 2022; 19(9):5372. https://doi.org/10.3390/ijerph19095372
Chicago/Turabian StyleOusseine, Youssoufa M., Sophie Vaux, Stéphanie Vandentorren, Isabelle Bonmarin, Karen Champenois, Nathalie Lydié, and Annie Velter. 2022. "Predictors of Uncertainty and Unwillingness to Receive the COVID-19 Vaccine in Men Who Have Sex with Men in France" International Journal of Environmental Research and Public Health 19, no. 9: 5372. https://doi.org/10.3390/ijerph19095372
APA StyleOusseine, Y. M., Vaux, S., Vandentorren, S., Bonmarin, I., Champenois, K., Lydié, N., & Velter, A. (2022). Predictors of Uncertainty and Unwillingness to Receive the COVID-19 Vaccine in Men Who Have Sex with Men in France. International Journal of Environmental Research and Public Health, 19(9), 5372. https://doi.org/10.3390/ijerph19095372







