The Role of Job Resources in the Relationship between Job Demands and Work-Related Musculoskeletal Disorders among Hospital Nurses in Thua Thien Hue Province, Vietnam
Abstract
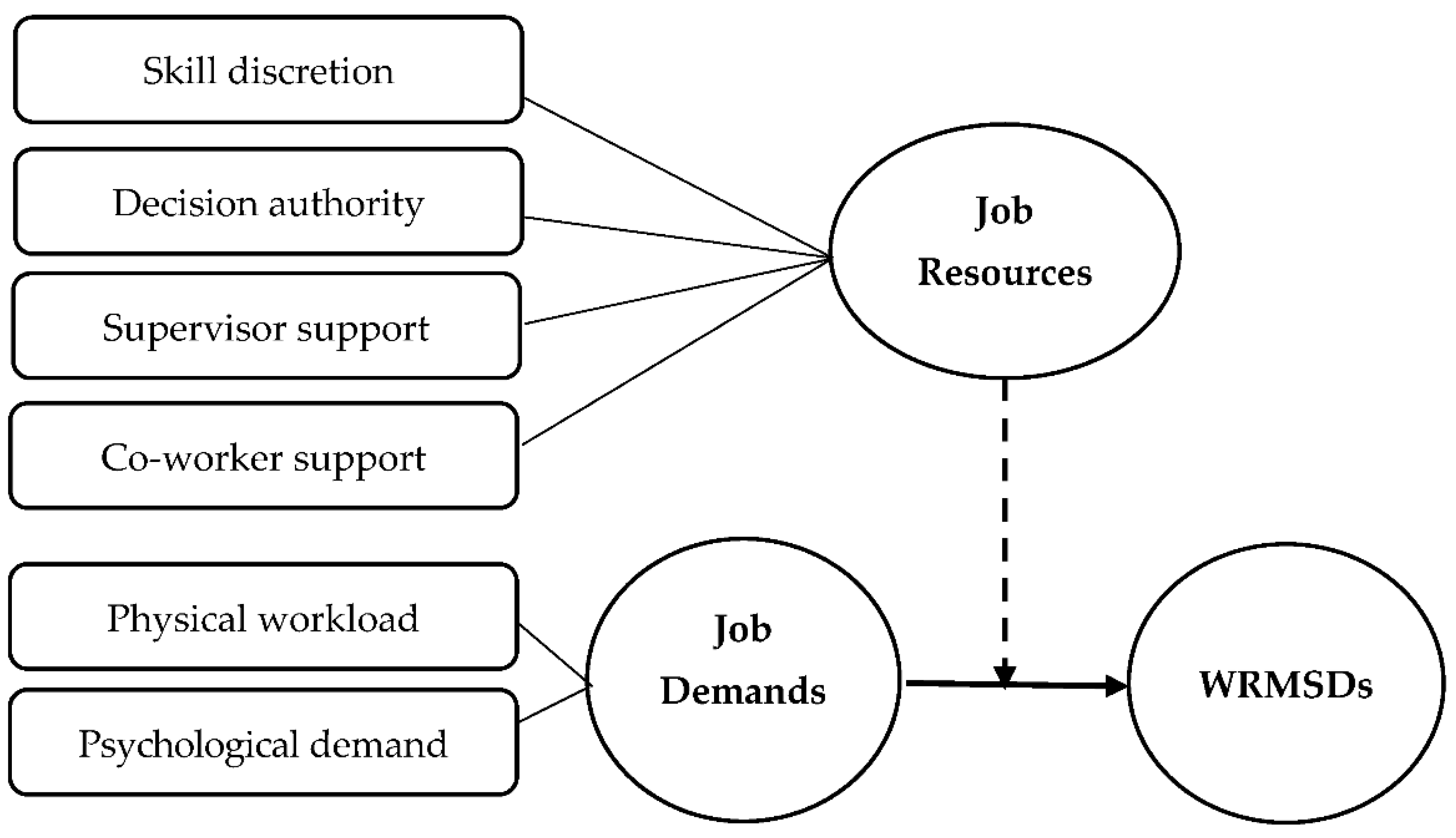
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Data Collection
2.3. Measurements
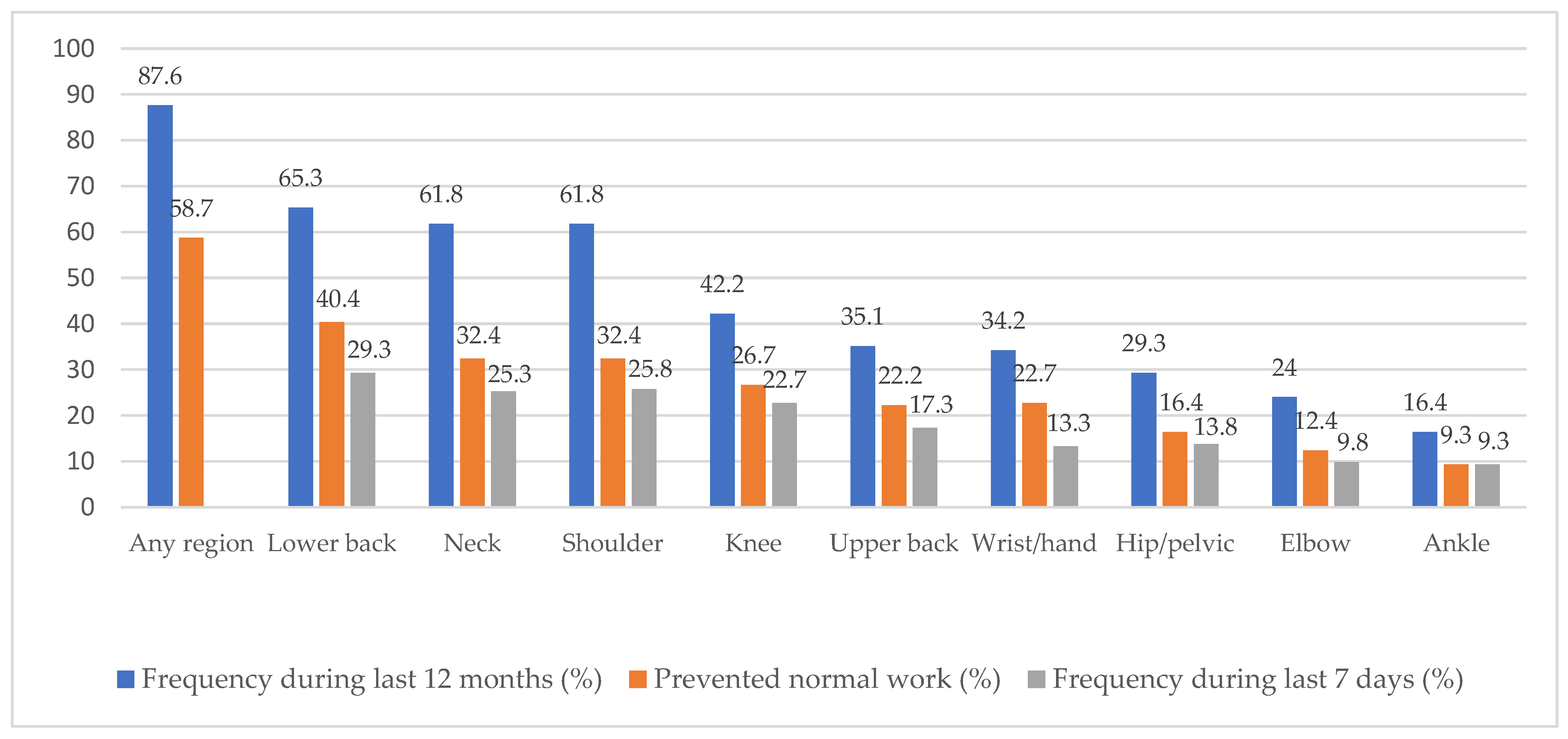
2.3.1. Work-Related Musculoskeletal Disorders
2.3.2. Job Demands
2.3.3. Job Resources
2.3.4. Demographics
2.4. Data Analysis
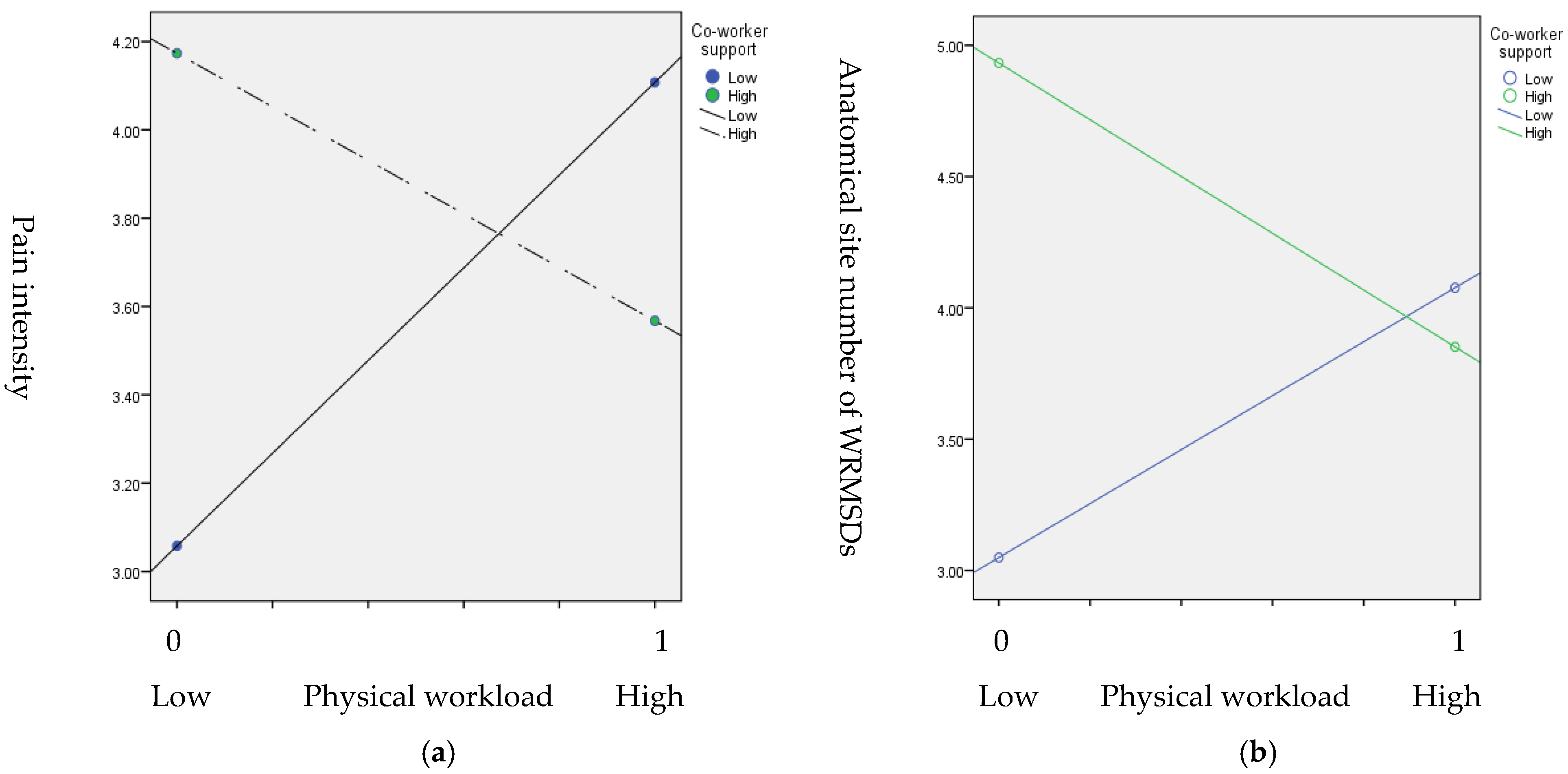
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Januskevicius, V. Work-Related Musculoskeletal Disorders among Hospital Workers: OSHwiki Networking Knowledge. 2020. Available online: https://oshwiki.eu/wiki/Work-related_musculoskeletal_disorders_among_hospital_workers (accessed on 13 August 2020).
- Akodu, A.K.; Ashalejo, Z.O. Work-related musculoskeletal disorders and work ability among hospital nurses. J. Taibah Univ. Med. Sci. 2019, 14, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Davis, K.G.; Kotowski, S.E. Prevalence of Musculoskeletal Disorders for Nurses in Hospitals, Long-Term Care Facilities, and Home Health Care: A Comprehensive Review. Hum. Factors 2015, 57, 754–792. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Lu, J.; Zeng, J.; Wang, L.; Li, Y. Prevalence and Risk Factors of Work-Related Musculoskeletal Disorders Among Intensive Care Unit Nurses in China. Workplace Health Saf. 2019, 67, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Camerino, D.; Cesana, G.C.; Molteni, G.; De Vito, G.; Evaristi, C.; Latocca, R. Job strain and musculoskeletal disorders of Italian nurses. Occup. Ergon. 2001, 2, 215–223. [Google Scholar] [CrossRef]
- Thinkhamrop, W.; Sawaengdee, K.; Tangcharoensathien, V.; Theerawit, T.; Laohasiriwong, W.; Saengsuwan, J.; Hurst, C.P. Burden of musculoskeletal disorders among registered nurses: Evidence from the Thai nurse cohort study. BMC Nurs. 2017, 16, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Bernal, D.; Campos-Serna, J.; Tobías, A.; Vargas-Prada, S.; Benavides, F.G.; Serra, C. Work-related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2015, 52, 635–648. [Google Scholar] [CrossRef]
- Menzel, N.N. Psychosocial Factors in Musculoskeletal Disorders. Crit. Care Nurs. Clin. N. Am. 2007, 19, 145–153. [Google Scholar] [CrossRef]
- dos Santos, H.E.C.; Marziale, M.H.P.; Felli, V.E.A. Presenteeism and musculoskeletal symptoms among nursing professionals. Rev. Lat. Am. Enferm. 2018, 26, e3006. [Google Scholar] [CrossRef] [Green Version]
- D’Errico, A.; Viotti, S.; Baratti, A.; Mottura, B.; Barocelli, A.P.; Tagna, M.; Sgambelluri, B.; Battaglino, P.; Converso, D. Low Back Pain and Associated Presenteeism among Hospital Nursing Staff. J. Occup. Health 2013, 55, 276–283. [Google Scholar] [CrossRef]
- Letvak, S.A.; Ruhm, C.J.; Gupta, S.N. Nurses’ Presenteeism and Its Effects on Self-Reported Quality of Care and Costs. Am. J. Nurs. 2012, 112, 30–38. [Google Scholar] [CrossRef]
- da Costa, B.R.; Vieira, E.R. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. Am. J. Ind. Med. 2010, 53, 285–323. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, N.D.R.; Fernandes, R.D.C.P. Factors related to musculoskeletal disorders in nursing workers. Rev. Lat. Am. Enferm. 2010, 18, 1076–1083. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, J.; Zhang, L.; Xu, C.; Qiao, J. Relationship Between the Exposure to Occupation-related Psychosocial and Physical Exertion and Upper Body Musculoskeletal Diseases in Hospital Nurses: A Systematic Review and Meta-analysis. Asian Nurs. Res. 2021, 15, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Karasek, R.A., Jr. Job Demands, Job Decision Latitude, and Mental Strain: Implications for Job Redesign. Adm. Sci. Q. 1979, 24, 285–308. [Google Scholar] [CrossRef]
- Karasek, R.; Theorell, T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life; Basic Books: New York, NY, USA, 1990. [Google Scholar]
- Bakker, A.B.; Demerouti, E. The Job Demands-Resources model: State of the art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef] [Green Version]
- Demerouti, E.; Bakker, A.B. The Job Demands–Resources model: Challenges for future research. SA J. Ind. Psychol. 2011, 37, 1–9. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands-resources model of burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef]
- Crawford, E.R.; LePine, J.A.; Rich, B.L. Linking job demands and resources to employee engagement and burnout: A theoretical extension and meta-analytic test. J. Appl. Psychol. 2010, 95, 834–848. [Google Scholar] [CrossRef]
- Falco, A.; Corso, L.D.; Girardi, D.; De Carlo, A.; Comar, M. The moderating role of job resources in the relationship between job demands and interleukin-6 in an Italian healthcare organization. Res. Nurs. Health 2018, 41, 39–48. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E.; Euwema, M.C. Job resources buffer the impact of job demands on burnout. J. Occup. Health Psychol. 2005, 10, 170. [Google Scholar] [CrossRef] [Green Version]
- Del Pozo-Antúnez, J.J.; Ariza-Montes, A.; Fernández-Navarro, F.; Molina-Sánchez, H. Effect of a Job Demand-Control-Social Support Model on Accounting Professionals’ Health Perception. Int. J. Environ. Res. Public Health 2018, 15, 2437. [Google Scholar] [CrossRef] [Green Version]
- Skovlund, S.V.; Bláfoss, R.; Sundstrup, E.; Thomassen, K.; Andersen, L.L. Joint association of physical work demands and leg pain intensity for work limitations due to pain in senior workers: Cross-sectional study. BMC Public Health 2020, 20, 1741. [Google Scholar] [CrossRef] [PubMed]
- Byström, P.; Hanse, J.J.; Kjellberg, A. Appraised psychological workload, musculoskeletal symptoms, and the mediating effect of fatigue: A structural equation modeling approach. Scand. J. Psychol. 2004, 45, 331–341. [Google Scholar] [CrossRef]
- Mehralizadeh, S.; Dehdashti, A.; Kashani, M.M. Structural equation model of interactions between risk factors and work-related musculoskeletal complaints among Iranian hospital nurses. Work 2017, 57, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Park, B.-C.; Cheong, H.-K.; Kim, E.-A.; Kim, S.G. Risk Factors of Work-related Upper Extremity Musculoskeletal Disorders in Male Shipyard Workers: Structural Equation Model Analysis. Saf. Health Work 2010, 1, 124–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luan, H.D.; Hai, N.T.; Xanh, P.T.; Giang, H.T.; Van Thuc, P.; Hong, N.M.; Khue, P.M. Musculoskeletal Disorders: Prevalence and Associated Factors among District Hospital Nurses in Haiphong, Vietnam. BioMed Res. Int. 2018, 2018, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Vietnam Ministry of Health. Decision No. 2992/QD-BYT Dated 17/07/2015 of the Ministry of Health Approving the Plan for Human Resource Development in the Medical Examination and Treatment System for the Period 2015–2020. 2015. Available online: http://kcb.vn/vanban/quyet-dinh-so-2992qd-byt-ngay-17072015-cua-bo-y-te-ve-phe-duyet-ke-hoach-phat-trien-nhan-luc-tronghe-thong-kham-benh-chua-benh-giai-doan-2015-2020 (accessed on 10 April 2021).
- Health Solution Service. How Many Patients Is It Appropriate for a Nurse to Take Care of? 2020. Available online: https://hss.asia/en/posts/1-dieu-duong-cham-soc-bao-nhieu-benh-nhan-thi-phu-hop-p514 (accessed on 31 May 2021).
- Ministry of Health Portal. Medical Officers and Staff under Heavy Work Pressure. 2020. Available online: https://moh.gov.vn/web/phong-chong-benh-nghe-nghiep/tuyen-truyen-huan-luyen/-/asset_publisher/jxI3QJtkofQT/content/can-bo-nhan-vien-y-te-chiu-ap-luc-cong-viec-nang-ne?inheritRedirect=false&redirect=https%3A%2F%2Fmoh.gov.vn%3A443%2Fweb%2Fphong-chong-benh-nghe-nghiep%2Ftuyen-truyen-huan-luyen%3Fp_p_id%3D101_INSTANCE_jxI3QJtkofQT%26p_p_lifecycle%3D0%26p_p_state%3Dnormal%26p_p_mode%3Dview%26p_p_col_id%3Drow-0-column-2%26p_p_col_count%3D1 (accessed on 18 June 2020).
- Tran, T.T.T.; Nguyen, N.B.; Luong, M.A.; Bui, T.H.A.; Phan, T.D.; Tran, V.O.; Ngo, T.H.; Minas, H.; Nguyen, T.Q. Stress, anxiety and depression in clinical nurses in Vietnam: A cross-sectional survey and cluster analysis. Int. J. Ment. Health Syst. 2019, 13, 3. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, T.H.; Hoang, D.L.; Hoang, T.G.; Pham, M.K.; Bodin, J.; Dewitte, J.D.; Roquelaure, Y. Prevalence and Characteristics of Multisite Musculoskeletal Symptoms among District Hospital Nurses in Haiphong, Vietnam. BioMed Res. Int. 2020, 2020, 3254605. [Google Scholar] [CrossRef]
- Vietnam Ministry of Health. Circular on Regulations on Occupational Diseases Covered by Social Insurance—15/2016/TT-BYT. 2016. Available online: https://thuvienphapluat.vn/van-ban/Bao-hiem/Thong-tu-15-2016-TT-BYTbenh-nghe-nghiep-duoc-huong-bao-hiem-xa-hoi-319385.aspx (accessed on 16 March 2020).
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Hollmann, S.; Klimmer, F.; Schmidt, K.-H.; Kylian, H. Validation of a questionnaire for assessing physical work load. Scand. J. Work. Environ. Health 1999, 25, 105–114. [Google Scholar] [CrossRef]
- Karasek, R.A. Job Content Questionnaire; University of Southern California, Department of Industrial and Systems Engineering: Los Angeles, CA, USA, 1985. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Arsalani, N.; Fallahi-Khoshknab, M.; Josephson, M.; Lagerström, M. Musculoskeletal Disorders and Working Conditions Among Iranian Nursing Personnel. Int. J. Occup. Saf. Ergon. 2014, 20, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Attar, S.M. Frequency and risk factors of musculoskeletal pain in nurses at a tertiary centre in Jeddah, Saudi Arabia: A cross sectional study. BMC Res. Notes 2014, 7, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, P.; Li, F.; Zhang, L.; Yang, Y.; Huang, A.; Wang, Y.; Yao, H. Prevalence of Work-Related Musculoskeletal Disorders in the Nurses Working in Hospitals of Xinjiang Uygur Autonomous Region. Pain Res. Manag. 2017, 2017, 5757108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, S.; Srisaenpang, S.; Pinitsoontorn, S.; Eungpinichpong, W. Prevalence of work-related musculoskeletal disorders among registered nurses in srinagarindhospital, Thailand. J. Health Res. 2011, 25, 61–68. [Google Scholar]
- Barzideh, M.; Choobineh, A.; Tabatabaee, H. Job stress dimensions and their relationship to musculoskeletal disorders in Iranian nurses. Work 2014, 47, 423–429. [Google Scholar] [CrossRef]
- Amin, N.A.; Nordin, R.B.; Noah, R.; Oxley, J.A.; Fatt, Q.K. Work Related Musculoskeletal Disorders in Female Nursing Personnel: Prevalence and Impact. Int. J. Collab. Res. Intern. Med. Public Health 2016, 8, 294–315. [Google Scholar]
- Hsien, H.K.; Wen, C.L.; Chia, C.H.; Hsien, W.K. Factors Affecting of Musculoskeletal Disorders in Nurses from a Taiwan Hospital. World Acad. Sci. Eng. Technol. Int. J. Nurs. Health Sci. 2016, 10, 9. [Google Scholar]
- Cantley, L.F.; Tessier-Sherman, B.; Slade, M.D.; Galusha, D.; Cullen, M.R. Expert ratings of job demand and job control as predictors of injury and musculoskeletal disorder risk in a manufacturing cohort. Occup. Environ. Med. 2016, 73, 229–236. [Google Scholar] [CrossRef] [Green Version]
- Sherehiy, B.; Karwowski, W.; Marek, T. Relationship between risk factors and musculoskeletal disorders in the nursing profession: A systematic review. Occup. Ergon. 2004, 4, 241–279. [Google Scholar] [CrossRef]
- Parkes, K.R. Social Support and Musculoskeletal Disorders: Literature Review and Data Analysis; Health and Safety Executive: Bootle, UK, 2008.
- Huynh, T.P.H. The Positioning of Nurses in Health Care in Vietnam: Interactions, Organizations and Space; Queensland University of Technology: Brisbane City, Australia, 2020. [Google Scholar]
- Feeney, B.C.; Collins, N.L. A new look at social support: A theoretical perspective on thriving through relationships. Pers. Soc. Psychol. Rev. 2015, 19, 113–147. [Google Scholar] [CrossRef]
- Pekkarinen, L.; Elovainio, M.; Sinervo, T.; Heponiemi, T.; Aalto, A.-M.; Noro, A.; Finne-Soveri, H. Job demands and musculoskeletal symptoms among female geriatric nurses: The moderating role of psychosocial resources. J. Occup. Health Psychol. 2013, 18, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Shen, Y.-M.; Zhu, M.; Liu, Y.; Deng, J.; Chen, Q.; See, L.-C. Effects of Co-Worker and Supervisor Support on Job Stress and Presenteeism in an Aging Workforce: A Structural Equation Modelling Approach. Int. J. Environ. Res. Public Health 2015, 13, 72. [Google Scholar] [CrossRef] [PubMed]
- Blomberg, S.; Rosander, M. Exposure to bullying behaviours and support from co-workers and supervisors: A three-way interaction and the effect on health and well-being. Int. Arch. Occup. Environ. Health 2020, 93, 479–490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bakker, A.B.; Demerouti, E. Job Demands-Resources Theory. Wellbeing 2014, 1–28. [Google Scholar] [CrossRef]
- Viotti, S.; Converso, D. Relationship between job demands and psychological outcomes among nurses: Does skill discretion matter? Int. J. Occup. Med. Environ. Health 2016, 29, 439–460. [Google Scholar] [CrossRef]
- Yang, M.-H.; Jhan, C.-J.; Hsieh, P.-C.; Kao, C.-C. A Study on the Correlations between Musculoskeletal Disorders and Work-Related Psychosocial Factors among Nursing Aides in Long-Term Care Facilities. Int. J. Environ. Res. Public Health 2021, 19, 255. [Google Scholar] [CrossRef]
| Variables | Category | N (%) | Mean (SD) |
|---|---|---|---|
| Gender | Male | 24 (10.7) | |
| Female | 201 (89.3) | ||
| Age | <30 age | 61 (27.1) | |
| 30–40 age | 119 (52.9) | ||
| >40 age | 45 (20.0) | ||
| BMI | Underweight (<18.5) | 15 (6.7) | |
| Normal (18.5–22.9) | 172 (76.4) | ||
| Overweight and obese (>23) | 38 (16.9) | ||
| Working department | General ward | 135 (60.0) | |
| ER-ICU-OP * | 48 (21.3) | ||
| Other | 42 (18.7) | ||
| Working experience | <5 years | 37 (16.4) | |
| 5–20 years | 170 (75.6) | ||
| >20 | 18 (8.0) | ||
| Working hour per shift | <8 h | 138 (61.3) | |
| >8–12 h | 62 (27.6) | ||
| >12 h | 25 (11.1) | ||
| Job demands | Physical workload [0–56.17] | 22.84 (9.64) | |
| Psychological demand [12–48] | 32.32 (4.73) | ||
| Job resources | Skill discretion [12–48] | 34.60 (2.99) | |
| Decision authority [12–48] | 33.49 (4.20) | ||
| Supervisor support [4–16] | 11.87 (1.64) | ||
| Coworker support [4–16] | 12.56 (1.27) | ||
| Severity of WRMSDs | Pain intensity | 4.11 (1.75) | |
| Anatomical site number | 4.23 (2.38) |
| Variables | Mean | SD | WRMSD Severity (DVs) | |||
|---|---|---|---|---|---|---|
| Pain Intensity | Anatomical Sites Number | |||||
| r | p | r | p | |||
| Job demand (IVs) | ||||||
| 1. Physical workload | 22.84 | 9.6 | 0.20 | <0.01 | 0.19 | <0.01 |
| 2. Psychological demand | 32.32 | 4.7 | 0.32 | <0.01 | 0.16 | <0.05 |
| Job resources (W) | ||||||
| 3. Skill discretion | 34 | 2.99 | 0.13 | >0.05 | 0.08 | >0.05 |
| 4. Decision authority | 33 | 4.20 | −0.01 | >0.05 | 0.05 | >0.05 |
| 5. Supervisor support | 11.87 | 1.64 | −0.06 | >0.05 | −0.01 | >0.05 |
| 6. Coworker support | 12.56 | 1.30 | 0.08 | >0.05 | 0.16 | <0.05 |
| Variables | WRMSD Severity | |||
|---|---|---|---|---|
| Pain Intensity | Anatomical Site Number | |||
| Model # | B | SE | B | SE |
| Moderating model 1 | R2 = 0.16, F(10, 214) = 2.80 *** | R2 = 0.15, F(10, 214) = 2.64 *** | ||
| Physical workload (PW) | 0.44 | 0.40 | 0.77 | 0.48 |
| Skill Discretion (SKD) | 0.33 | 0.50 | 0.68 | 0.48 |
| PW × SKD | 0.29 | 0.63 | −0.70 | 0.72 |
| Moderating model 2 | R2 = 0.15, F(10, 214) = 2.70 *** | R2 = 0.16, F(10, 214) = 2.72 *** | ||
| Physical workload (PW) | 0.37 | 0.37 | 0.25 | 0.43 |
| Decision Authority (DA) | −0.15 | 0.42 | 0.21 | 0.47 |
| PW × DA | 0.61 | 0.59 | 0.69 | 0.70 |
| Moderating model 3 | R2 = 0.15, F(10, 214) = 2.73 *** | R2 = 0.16, F(10, 214) = 2.86 *** | ||
| Physical workload (PW) | 0.49 | 0.34 | 0.62 | 0.42 |
| Supervisor support (SS) | −0.19 | 0.53 | 0.99 | 0.69 |
| PW × SS | 0.71 | 0.74 | −0.45 | 0.94 |
| Moderating model 4 | R2 = 0.17, F(10, 214) = 3.13 *** | R2 = 0.14, F(10, 214) = 4.81 *** | ||
| Physical workload (PW) | 1.05 * | 0.35 | 1.49 * | 0.41 |
| Coworker support (CS) | 1.12 * | 0.60 | 1.03 ** | 0.59 |
| PW × CS | −1.65 * | 0.72 | −2.11 ** | 0.78 |
| Conditional effects of the PW at values of the moderator of CS on WRMSD severity | ||||
| Coworker support | Effect (Boot SE) | Boot 95% CI | ||
| Low | 1.05 (0.35) | 0.37; 1.73 | 1.03 (0.41) | 0.21; 1.84 |
| High | −0.61 (0.64) | −1.87; 0.66 | −1.08 (0.70) | −2.46; 0.30 |
| Variables | WRMSD Severity | |||
|---|---|---|---|---|
| Pain Intensity | Anatomical Site Number | |||
| Model # | B | SE | B | SE |
| Moderating model 1 | R2 = 0.17, F(18, 206) = 2.89 *** | R2 = 0.14, F(18, 206) = 2.33 ** | ||
| Psychological demand (PD) | 0.72 | 0.39 | 0.21 | 0.50 |
| Skill discretion (SD) | 0.14 | 0.43 | 0.58 | 0.58 |
| PD × SD | 0.30 | 0.61 | −0.43 | 0.78 |
| Moderating model 2 | R2 = 0.17, F(18, 206) = 2.92 *** | R2 = 0.16, F(18, 206) = 2.55 *** | ||
| Psychological demand (PD) | 1.20 ** | 0.36 | 0.62 | 0.79 |
| Decision authority (DA) | 0.40 | 0.39 | 0.28 | 0.53 |
| DL × DA | −0.64 | 0.56 | −0.56 | 0.86 |
| Moderating model 3 | R2 = 0.10, F(18, 206) = 3.03 *** | R2 = 0.15, F(18, 206) = 2.64 *** | ||
| Psychological demand (PD) | 0.91 ** | 0.32 | 0.27 | 0.39 |
| Supervisor support (SS) | 0.13 | 0.53 | 1.12 | 0.71 |
| PD × SS | 0.10 | 0.71 | −0.74 | 0.85 |
| Moderating model 4 | R2 = 0.17, F(18, 206) = 2.84 *** | R2 = 0.15, F(18, 206) = 2.57 *** | ||
| Psychological demand (PD) | 0.75 * | 0.33 | 0.24 | 0.42 |
| Coworker support (CS) | −0.22 | 0.47 | 0.99 | 0.63 |
| PD × CS | 0.63 | 0.65 | −0.57 | 0.82 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mai, H.B.; Kim, J. The Role of Job Resources in the Relationship between Job Demands and Work-Related Musculoskeletal Disorders among Hospital Nurses in Thua Thien Hue Province, Vietnam. Int. J. Environ. Res. Public Health 2022, 19, 4774. https://doi.org/10.3390/ijerph19084774
Mai HB, Kim J. The Role of Job Resources in the Relationship between Job Demands and Work-Related Musculoskeletal Disorders among Hospital Nurses in Thua Thien Hue Province, Vietnam. International Journal of Environmental Research and Public Health. 2022; 19(8):4774. https://doi.org/10.3390/ijerph19084774
Chicago/Turabian StyleMai, Hai Ba, and Jiyun Kim. 2022. "The Role of Job Resources in the Relationship between Job Demands and Work-Related Musculoskeletal Disorders among Hospital Nurses in Thua Thien Hue Province, Vietnam" International Journal of Environmental Research and Public Health 19, no. 8: 4774. https://doi.org/10.3390/ijerph19084774
APA StyleMai, H. B., & Kim, J. (2022). The Role of Job Resources in the Relationship between Job Demands and Work-Related Musculoskeletal Disorders among Hospital Nurses in Thua Thien Hue Province, Vietnam. International Journal of Environmental Research and Public Health, 19(8), 4774. https://doi.org/10.3390/ijerph19084774







