Socioeconomic Inequalities in Women’s Undernutrition: Evidence from Nationally Representative Cross-Sectional Bangladesh Demographic and Health Survey 2017–2018
Abstract
:1. Introduction
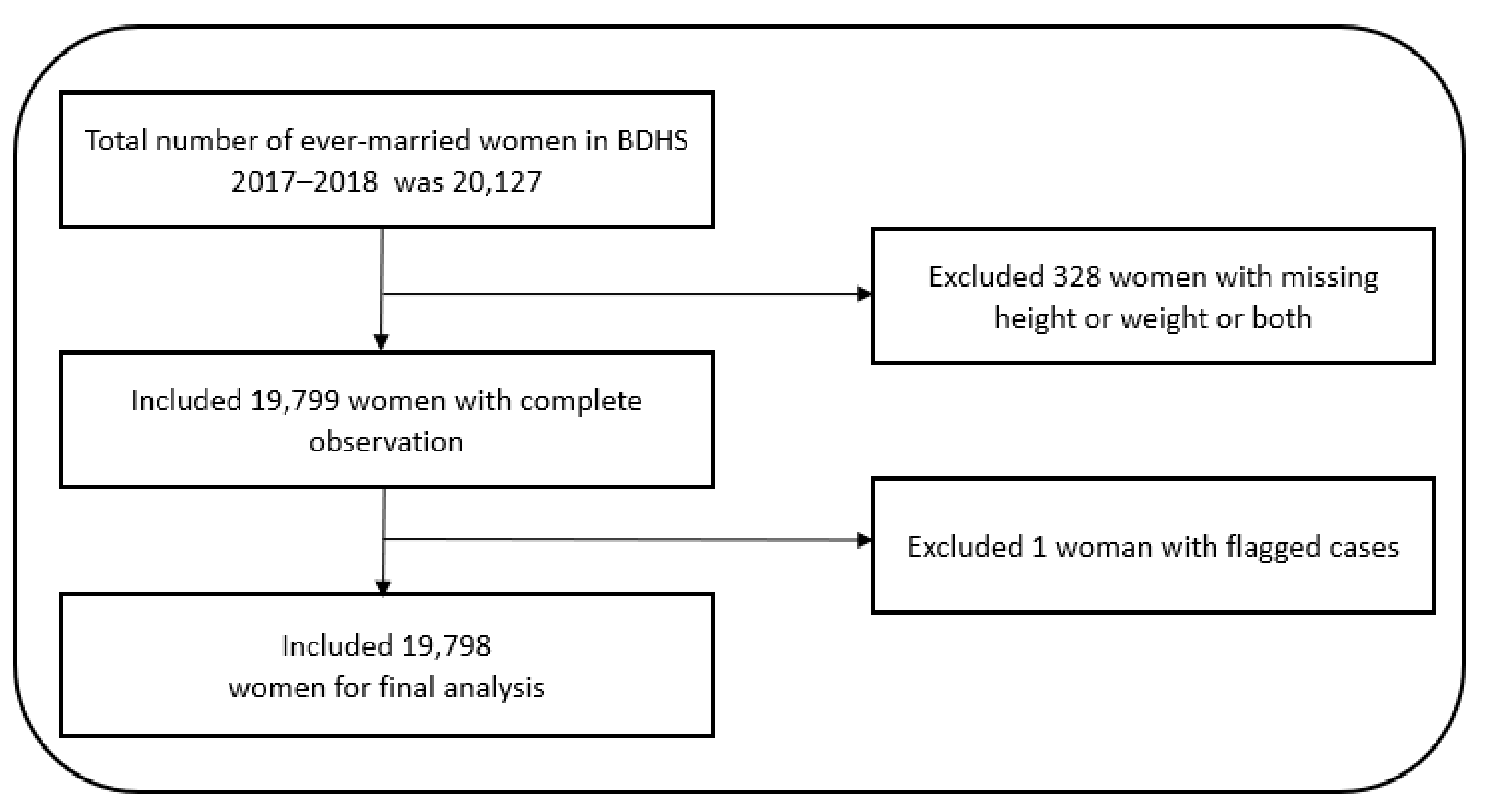
2. Materials and Methods
2.1. Data Source
2.2. Outcome Measure
2.3. Covariates Measure
2.4. Statistical Analyses
3. Results
3.1. Sample Characteristics
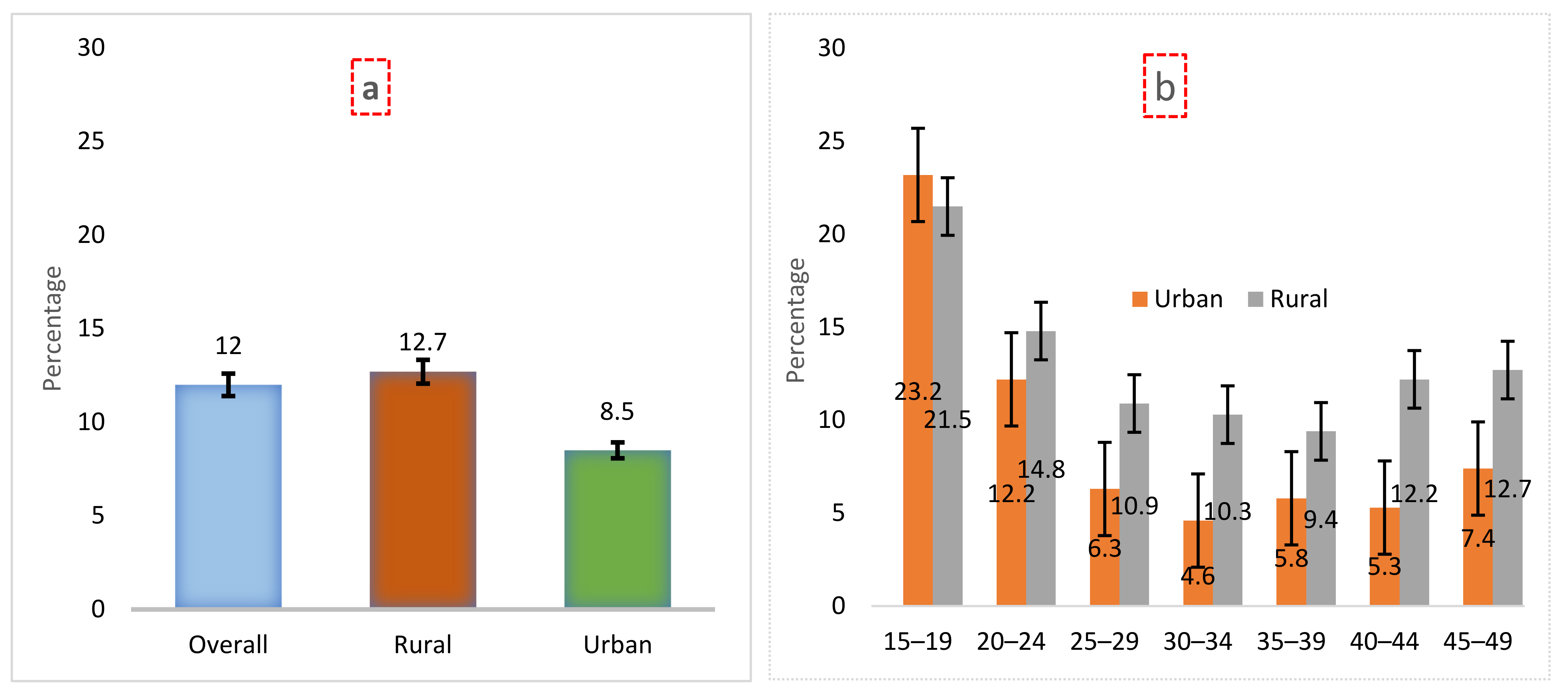
3.2. Prevalence of Undernutrition
3.3. Prevalence and Association of Undernutrition by Sample Characteristics
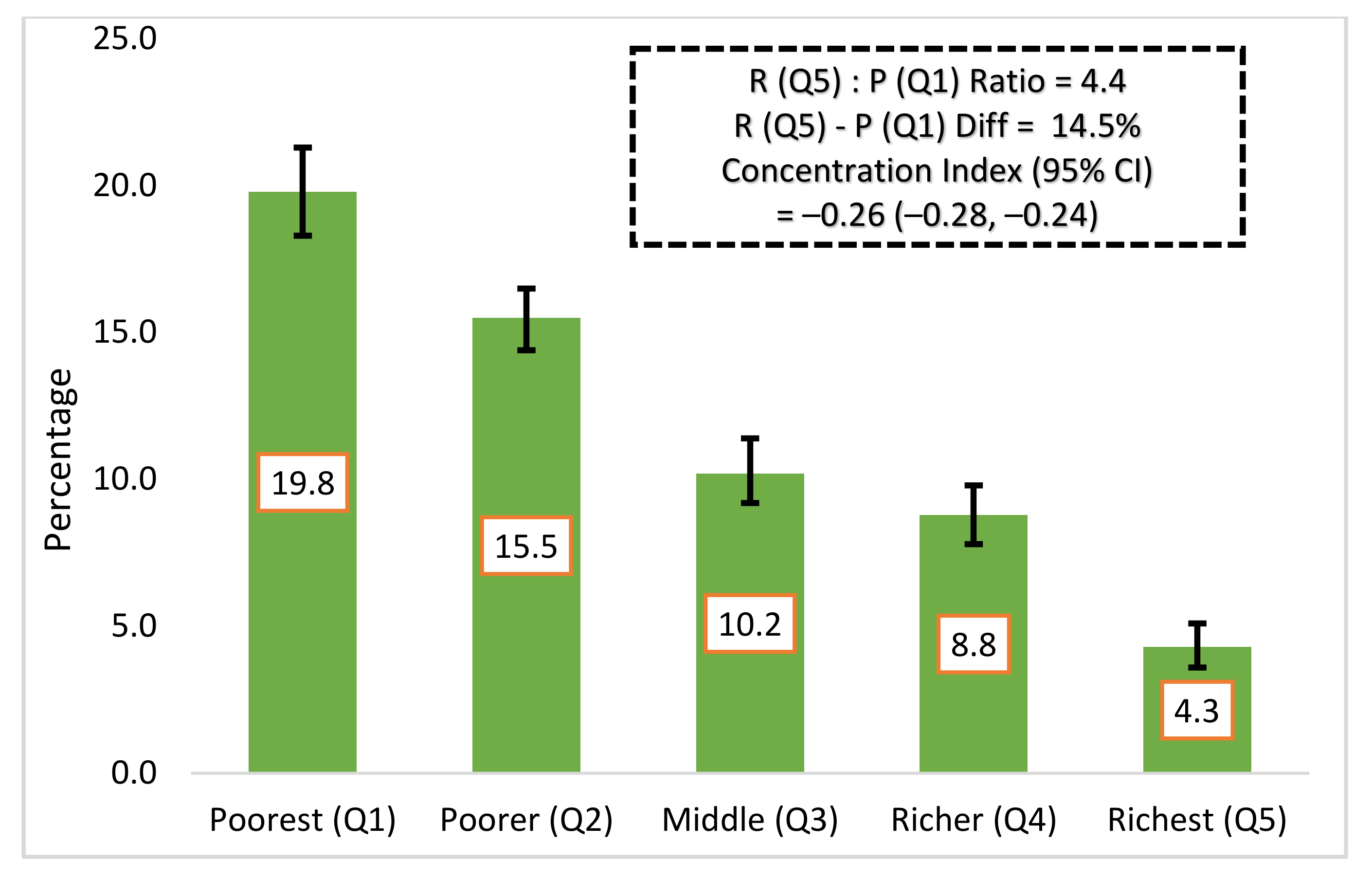
3.4. Socioeconomic Inequalities of Undernutrition
3.5. Factors Associated with Women’s Undernutrition
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Global Health Risks. 2009. Available online: https://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf (accessed on 16 December 2021).
- Grebmer, V.K.; Bernstein, J.; Patterson, F. Global Hunger Index. 2019. Available online: https://www.globalhungerindex.org/pdf/en/2019.pdf (accessed on 16 December 2021).
- Ahmed, T.; Hossain, M.; Sanin, K.I. Global burden of maternal and child undernutrition and micronutrient deficiencies. Ann. Nutr. Metab. 2012, 61, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-Mcgregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Osmond, C.; Barker, D.J.P.; Winter, P.D.; Fall, C.H.D.; Simmonds, S.J. Early growth and death from cardiovascular disease in women. Br. Med. J. 1993, 307, 1519–1524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whincup, P.H.; Kaye, S.J.; Owen, C.G. Birth Weight and Risk of Type 2 Diabetes A Systematic Review. JAMA 2008, 300, 2886–2897. [Google Scholar] [CrossRef]
- Adair, L.S.; Fall, C.H.D.; Osmond, C.; Stein, A.D.; Martorell, R.; Ramirez-Zea, M.; Sachdev, H.S.; Dahly, D.L.; Bas, I.; Norris, S.A.; et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: Findings from five birth cohort studies. Lancet 2013, 382, 525–534. [Google Scholar] [CrossRef] [Green Version]
- Mason, J.B.; Shrimpton, R.; Saldanha, L.S.; Ramakrishnan, U.; Victora, C.G.; Girard, A.W.; McFarland, D.A.; Martorell, R. The first 500 days of life: Policies to support maternal nutrition. Glob. Health Action 2014, 7, 23623. [Google Scholar] [CrossRef] [Green Version]
- Danaei, G.; Andrews, K.G.; Sudfeld, C.R.; Fink, G.; McCoy, D.C.; Peet, E.; Sania, A.; Smith Fawzi, M.C.; Ezzati, M.; Fawzi, W.W. Risk Factors for Childhood Stunting in 137 Developing Countries: A Comparative Risk Assessment Analysis at Global, Regional, and Country Levels. PLoS Med. 2016, 13, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Smith, L.C.; Ramakrishnan, U.; Ndiaye, A.; Haddad, L.; Martorell, R. The importance of women’s status for child nutrition in developing countries. Res. Rep. Int. Food Policy Res. Inst. 2003, 24, 1–164. [Google Scholar] [CrossRef]
- Sarker, A.R.; Sultana, M.; Nurnabi, S.; Raisul, A. Inequality of childhood undernutrition in Bangladesh: A decomposition approach. Intern. J. Health Plan. Manag. 2019, 35, 441–468. [Google Scholar] [CrossRef]
- GHI. Global Hunger Index. 2021. Available online: https://www.globalhungerindex.org/pdf/en/2021.pdf (accessed on 16 December 2021).
- USAID. Agriculture and Food Security; USAID: Washinton, DC, USA, 2022. Available online: https://www.usaid.gov/bangladesh/agriculture-and-food-security (accessed on 16 December 2021).
- Economist Intelligence Unit Global Food Security Index 2017: Measuring Food Security and the Impact of Resource Risks. Econ. Intell. Unit Ltd. 2017, 2017, 1–56.
- WB. The World Bank in Bangladesh; World Bank: Washington, DC, USA, 2021. [Google Scholar]
- Ahmed, T.; Mahfuz, M.; Ireen, S.; Shamsir Ahmed, A.M.; Rahman, S.; Munirul Islam, M.; Alam, N.; Iqbal Hossain, M.; Mustafizur Rahman, S.M.; Mohsin Ali, M.; et al. Nutrition of children and women in Bangladesh: Trends and directions for the future. J. Health Popul. Nutr. 2012, 30, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shekar, M.; Condo, J.; Pate, M.A.; Nishtar, S. Maternal and child undernutrition: Progress hinges on supporting women and more implementation research. Lancet 2021, 397, 1329–1331. [Google Scholar] [CrossRef]
- Hossain, M.M.; Islam, M.R.; Sarkar, A.S.R.; Khan, M.M.A. Prevalence and determinants risk factors of underweight and overweight among women in Bangladesh. Obedity Med. 2018, 11, 1–5. [Google Scholar] [CrossRef]
- Chowdhury, M.A.B.; Adnan, M.M.; Hassan, M.Z. Trends, prevalence and risk factors of overweight and obesity among women of reproductive age in Bangladesh: A pooled analysis of five national cross-sectional surveys. BMJ Open 2018, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Nutrition Landscape Information System (NLiS); WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Ahmed, K.Y.; Rwabilimbo, A.G.; Abrha, S.; Page, A.; Arora, A.; Tadese, F.; Beyene, T.Y.; Seiko, A.; Endris, A.A.; Agho, K.E.; et al. Factors associated with underweight, overweight, and obesity in reproductive age Tanzanian women. PLoS ONE 2020, 15, e0237720. [Google Scholar] [CrossRef]
- Al Kibria, G.M.; Swasey, K.; Hasan, M.Z.; Sharmeen, A.; Day, B. Prevalence and factors associated with underweight, overweight and obesity among women of reproductive age in India. Glob. Health Res. Policy 2019, 4, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Biswas, R.K.; Rahman, N.; Khanam, R.; Baqui, A.H.; Ahmed, S. Double burden of underweight and overweight among women of reproductive age in Bangladesh. Public Health Nutr. 2019, 22, 3163–3174. [Google Scholar] [CrossRef]
- Mengesha Kassie, A.; Beletew Abate, B.; Wudu Kassaw, M.; Gebremeskel Aragie, T. Prevalence of Underweight and Its Associated Factors among Reproductive Age Group Women in Ethiopia: Analysis of the 2016 Ethiopian Demographic and Health Survey Data. J. Environ. Public Health 2020, 2020, 9718714. [Google Scholar] [CrossRef]
- Kamal, S.M.M.; Hassan, C.H.; Alam, G.M. Dual burden of underweight and overweight among women in Bangladesh: Patterns, prevalence, and sociodemographic correlates. J. Health Popul. Nutr. 2015, 33, 92–105. [Google Scholar] [CrossRef]
- Mtumwa, A.H.; Paul, E.; Vuai, S.A.H. Determinants of undernutrition among women of reproductive age in Tanzania mainland. South Afr. J. Clin. Nutr. 2016, 29, 75–81. [Google Scholar] [CrossRef]
- Rutstein, O.S.; Johnson, K. DHS Comaparative Reports, The DHS Wealth Index; USAID: Rockville, MD, USA, 2004. [Google Scholar]
- Ásgeirsdóttir, T.L.; Ragnarsdóttir, D.Ó. Determinants of relative and absolute concentration indices: Evidence from 26 European countries. Int. J. Equity Health 2013, 12, 53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koolman, X.; van Doorslaer, E. On the interpretation of a concentration index of inequality. Health Econ. 2004, 13, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Reyes Matos, U.; Mesenburg, M.A.; Victora, C.G. Socioeconomic inequalities in the prevalence of underweight, overweight, and obesity among women aged 20–49 in low- and middle-income countries. Int. J. Obes. 2020, 44, 609–616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, S.; Hasan, M.M.; Ahmed, W.; Chowdhury, M.A.H. Socio-economic Inequity of Malnutrition among Under-Five Children and Women at Reproductive Age in Bangladesh. J. Nutr. Health 2013, 1, 18–22. [Google Scholar] [CrossRef]
- Hong, R.; Hong, R. Economic inequality and undernutrition in women: Multilevel analysis of individual, household, and community levels in Cambodia. Food Nutr. Bull. 2007, 28, 59–66. [Google Scholar] [CrossRef]
- van den Bold, M.; Quisumbing, A.R.; Gillespie, S. Women’s Empowerment and Nutrition: An Evidence Review. SSRN Electron. J. 2013. [Google Scholar] [CrossRef] [Green Version]
- Rustad, C.; Smith, C. Nutrition Knowledge and Associated Behavior Changes in a Holistic, Short-term Nutrition Education Intervention with Low-income Women. J. Nutr. Educ. Behav. 2013, 45, 490–498. [Google Scholar] [CrossRef]
- Tanner, J.M.; Whitehouse, R.H. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch. Dis. Child. 1976, 51, 170–179. [Google Scholar] [CrossRef] [Green Version]
- Patton, G.C.; Olsson, C.A.; Skirbekk, V.; Saffery, R.; Wlodek, M.E.; Azzopardi, P.S.; Stonawski, M.; Rasmussen, B.; Spry, E.; Francis, K.; et al. Adolescence and the next generation. Nature 2018, 554, 458–466. [Google Scholar] [CrossRef] [Green Version]
| Characteristics | Number | Percentage | 95% CI |
|---|---|---|---|
| Number of household members | |||
| <5 | 8648 | 44.6 | 43.5, 45.8 |
| ≥5 | 11,150 | 55.4 | 54.2, 56.5 |
| Age of respondents | |||
| 15–19 years | 1916 | 10.2 | 9.7, 10.8 |
| 20–24 years | 3455 | 17.6 | 17.0, 18.3 |
| 25–29 years | 3518 | 17.8 | 17.2, 18.4 |
| 30–34 years | 3410 | 17.2 | 16.6, 17.9 |
| 35–39 years | 2902 | 14.3 | 13.8, 14.8 |
| 40–44 years | 2287 | 11.4 | 10.9, 11.9 |
| 45–49 years | 2310 | 11.4 | 10.9, 11.8 |
| Respondents’ education | |||
| No formal education | 3202 | 16.6 | 15.8, 17.5 |
| Primary | 6340 | 31.4 | 30.5, 32.4 |
| Secondary or higher | 10,585 | 52.0 | 50.6, 53.3 |
| Respondents’ marital status | |||
| Others (widowed/divorced/separated) | 1232 | 5.7 | 5.3, 6.0 |
| Married | 18,895 | 94.4 | 94.0, 94.7 |
| Respondents’ current employment status | |||
| Unemployed | 10,280 | 52.1 | 50.2, 53.9 |
| Employed | 9518 | 47.9 | 46.1, 49.8 |
| Number of living children | |||
| No child | 2044 | 10.5 | 10.0, 11.0 |
| One child | 4559 | 22.7 | 22.0, 23.4 |
| Two children | 6141 | 30.8 | 29.9, 31.7 |
| Three or more children | 7054 | 36.0 | 35.0, 37.0 |
| Mass media exposure | |||
| No | 6888 | 34.1 | 32.3, 36.0 |
| Yes | 12,910 | 65.9 | 64.0, 67.7 |
| Type of place of residence | |||
| Urban | 7193 | 28.1 | 27.3, 29.0 |
| Rural | 12,605 | 71.9 | 71.0, 72.7 |
| Wealth quintile | |||
| Poorest | 3784 | 18.7 | 17.2, 20.3 |
| Poorer | 3798 | 19.8 | 18.8, 20.9 |
| Middle | 3849 | 20.3 | 19.3, 21.4 |
| Richer | 4037 | 20.9 | 19.7, 22.1 |
| Richest | 4330 | 20.3 | 18.9, 21.8 |
| Administrative division | |||
| Barisal | 2126 | 5.6 | 5.3, 5.9 |
| Chattogram | 2840 | 17.9 | 17.2, 18.6 |
| Dhaka | 2873 | 25.1 | 24.3, 26 |
| Khulna | 2599 | 11.7 | 11.2, 12.1 |
| Mymensingh | 2148 | 7.8 | 7.2, 8.3 |
| Rajshahi | 2553 | 14.0 | 13.5, 14.7 |
| Rangpur | 2470 | 11.9 | 11.4, 12.5 |
| Sylhet | 2189 | 5.9 | 5.7, 6.2 |
| Variables | COR | 95% CI | p-Value | AOR | 95% CI | p-Value |
|---|---|---|---|---|---|---|
| Household size (Ref. <5) | ||||||
| ≥5 | 1.09 | 0.99, 1.2 | 0.071 | |||
| Age of the respondents (Ref. 45–49) | ||||||
| 15–19 | 2.30 | 1.92, 2.74 | <0.001 | 2.81 | 2.23, 3.55 | <0.001 |
| 20–24 | 1.35 | 1.16, 1.57 | <0.001 | 1.73 | 1.41, 2.12 | <0.001 |
| 25–29 | 0.91 | 0.77, 1.08 | 0.285 | 1.17 | 0.96, 1.42 | 0.115 |
| 30–34 | 0.75 | 0.63, 0.9 | 0.002 | 0.90 | 0.74, 1.09 | 0.273 |
| 35–39 | 0.78 | 0.65, 0.94 | 0.008 | 0.85 | 0.70, 1.02 | 0.086 |
| 40–44 | 0.95 | 0.79, 1.15 | 0.626 | 0.99 | 0.82, 1.19 | 0.885 |
| Education level (Ref. No formal education) | ||||||
| Primary | 0.81 | 0.72, 0.91 | 0.001 | 0.81 | 0.72, 0.91 | 0.001 |
| Secondary or higher | 0.55 | 0.49, 0.61 | <0.001 | 0.55 | 0.49, 0.61 | <0.001 |
| Marital status (Ref. Others) | ||||||
| Married | 0.69 | 0.59, 0.81 | <0.001 | 0.72 | 0.61, 0.86 | <0.001 |
| Employment status (Ref. Unemployed) | ||||||
| Employed | 1.18 | 1.08, 1.29 | <0.001 | 1.13 | 1.03, 1.24 | 0.013 |
| Type of place of residence (Ref. Urban) | ||||||
| Rural | 1.62 | 1.47, 1.78 | <0.001 | 0.98 | 0.88, 1.09 | 0.743 |
| Mass media exposure (Ref. No) | ||||||
| Yes | 0.52 | 0.48, 0.57 | <0.001 | 0.87 | 0.79, 0.97 | 0.012 |
| Number of living children (Ref. No child) | ||||||
| One | 0.79 | 0.68, 0.91 | 0.001 | 0.93 | 0.80, 1.09 | 0.356 |
| Two | 0.52 | 0.45, 0.60 | <0.001 | 0.80 | 0.67, 0.95 | 0.012 |
| Three or more | 0.63 | 0.55, 0.72 | <0.001 | 0.87 | 0.72, 1.06 | 0.168 |
| Wealth quintile (Ref. Richest) | ||||||
| Poorest | 5.44 | 4.61, 6.41 | <0.001 | 3.93 | 3.21, 4.81 | <0.001 |
| Poorer | 4.23 | 3.58, 5.0 | <0.001 | 3.27 | 2.69, 3.97 | <0.001 |
| Middle | 2.65 | 2.22, 3.16 | <0.001 | 2.30 | 1.90, 2.78 | <0.001 |
| Richer | 2.09 | 1.75, 2.51 | <0.001 | 1.83 | 1.52, 2.21 | <0.001 |
| Division (Ref. Barisal) | ||||||
| Chattogram | 0.67 | 0.55, 0.81 | <0.001 | 0.85 | 0.70, 1.05 | 0.127 |
| Dhaka | 0.84 | 0.69, 1.01 | 0.064 | 1.23 | 1.01, 1.51 | 0.038 |
| Khulna | 0.95 | 0.78, 1.14 | 0.572 | 1.20 | 0.99, 1.46 | 0.066 |
| Mymensingh | 1.72 | 1.44, 2.06 | <0.001 | 1.66 | 1.38, 1.99 | <0.001 |
| Rajshahi | 1.10 | 0.92, 1.33 | 0.292 | 1.23 | 1.01, 1.49 | 0.036 |
| Rangpur | 1.28 | 1.06, 1.53 | 0.008 | 1.19 | 0.98, 1.43 | 0.075 |
| Sylhet | 2.07 | 1.74, 2.46 | <0.001 | 2.38 | 1.98, 2.86 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahman, M.; Tariqujjaman, M.; Islam, M.R.; Sheikh, S.P.; Sultana, N.; Ahmed, T.; Ahmed, S.; Sarma, H. Socioeconomic Inequalities in Women’s Undernutrition: Evidence from Nationally Representative Cross-Sectional Bangladesh Demographic and Health Survey 2017–2018. Int. J. Environ. Res. Public Health 2022, 19, 4698. https://doi.org/10.3390/ijerph19084698
Rahman M, Tariqujjaman M, Islam MR, Sheikh SP, Sultana N, Ahmed T, Ahmed S, Sarma H. Socioeconomic Inequalities in Women’s Undernutrition: Evidence from Nationally Representative Cross-Sectional Bangladesh Demographic and Health Survey 2017–2018. International Journal of Environmental Research and Public Health. 2022; 19(8):4698. https://doi.org/10.3390/ijerph19084698
Chicago/Turabian StyleRahman, Mahfuzur, Md. Tariqujjaman, Md. Rayhanul Islam, Sifat Parveen Sheikh, Nadia Sultana, Tahmeed Ahmed, Sayem Ahmed, and Haribondhu Sarma. 2022. "Socioeconomic Inequalities in Women’s Undernutrition: Evidence from Nationally Representative Cross-Sectional Bangladesh Demographic and Health Survey 2017–2018" International Journal of Environmental Research and Public Health 19, no. 8: 4698. https://doi.org/10.3390/ijerph19084698
APA StyleRahman, M., Tariqujjaman, M., Islam, M. R., Sheikh, S. P., Sultana, N., Ahmed, T., Ahmed, S., & Sarma, H. (2022). Socioeconomic Inequalities in Women’s Undernutrition: Evidence from Nationally Representative Cross-Sectional Bangladesh Demographic and Health Survey 2017–2018. International Journal of Environmental Research and Public Health, 19(8), 4698. https://doi.org/10.3390/ijerph19084698






