Effects of High-Intensity Aquatic or Bicycling Training in Athletes with Unilateral Patellofemoral Pain Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Participants
2.3. Graded Exercise Test
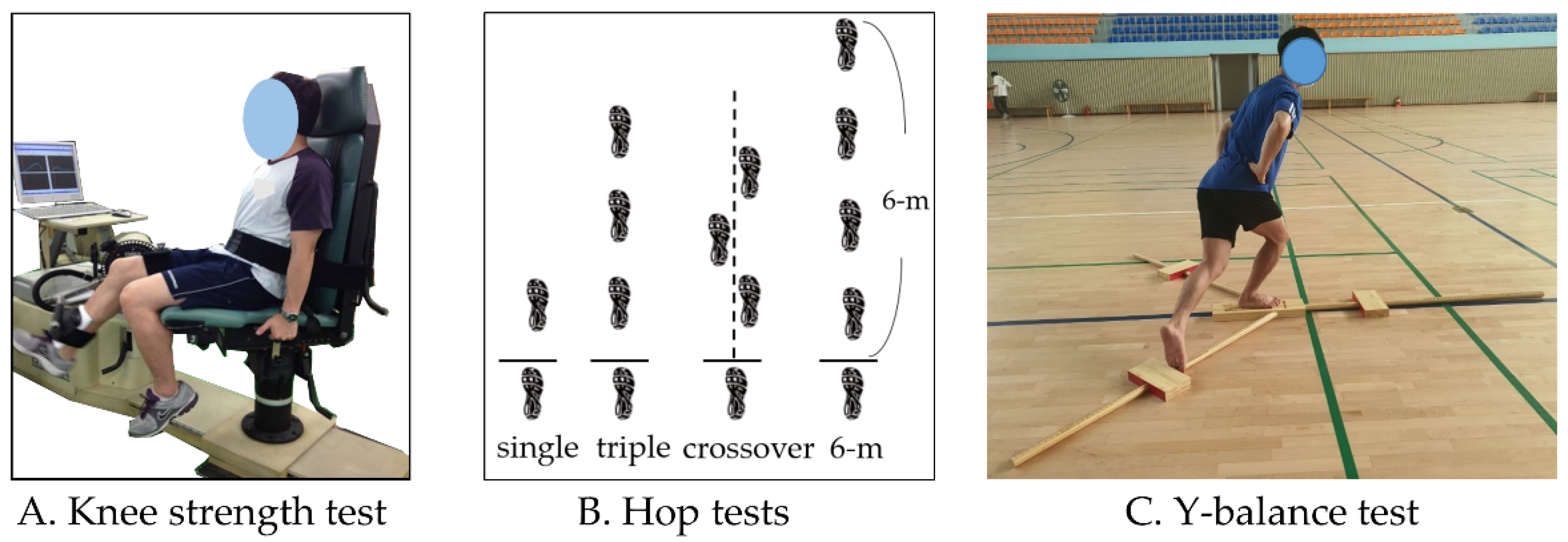
2.4. Knee Muscle Strength Test
2.5. Hop Tests
2.6. Y-Balance Tests
2.7. Subjective Knee Score
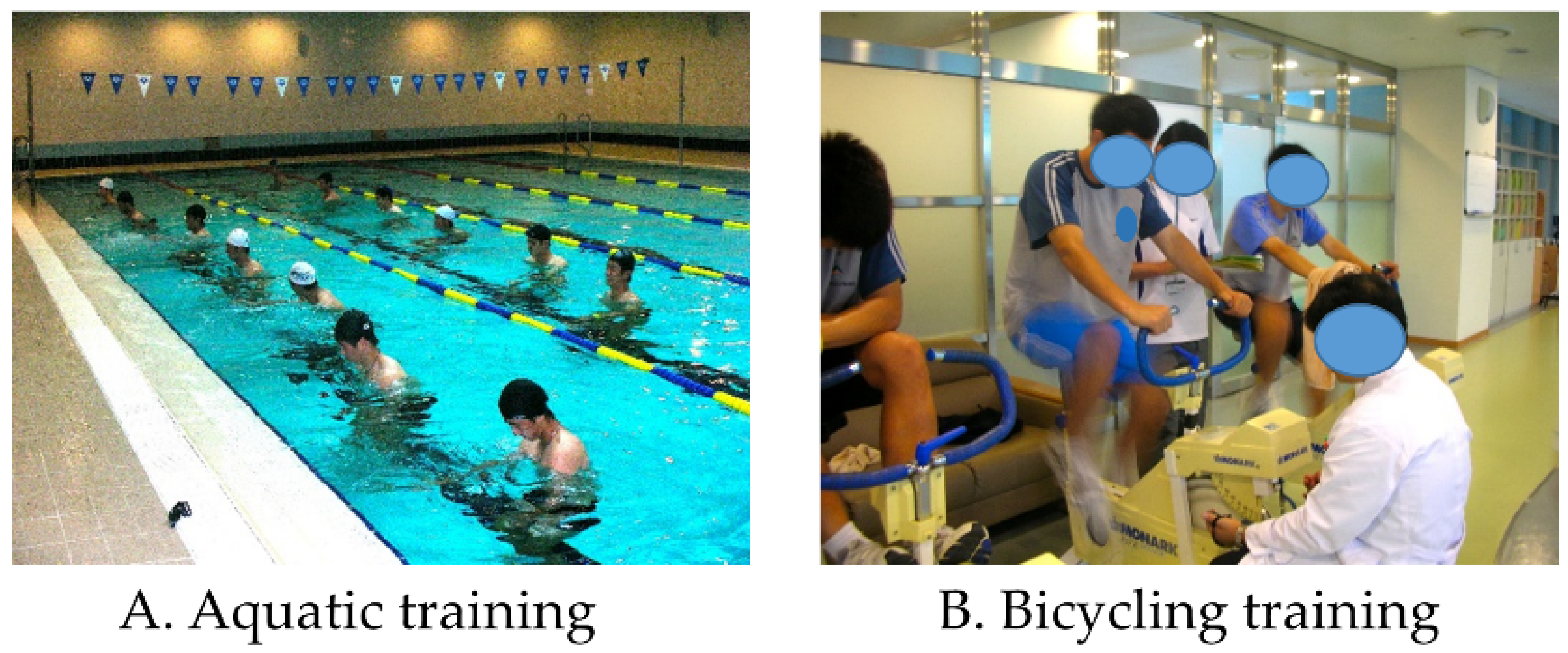
2.8. Training Program
2.8.1. Aquatic Training
2.8.2. Bicycling Training
2.8.3. Muscle Strength Training
2.9. Statistical Analysis
3. Results
3.1. General Characteristics of Participants
3.2. Cardiorespiratory Fitness
3.3. Isokinetic Knee Strength
3.4. Hop Tests
3.5. Y-Balance Test
3.6. Subjective Knee Score
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Petersen, W.; Ellermann, A.; Gösele-Koppenburg, A.; Best, R.; Rembitzki, I.V.; Brüggemann, G.-P.; Liebau, C. Patellofemoral pain syndrome. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2264–2274. [Google Scholar] [CrossRef] [PubMed]
- Bolgla, L.A.; Boling, M.C. An update for the conservative management of patellofemoral pain syndrome: A systematic review of the literature from 2000 to 2010. Int. J. Sports Phys. Ther. 2011, 6, 112–125. [Google Scholar] [PubMed]
- Devereaux, M.; Lachmann, S. Patello-femoral arthralgia in athletes attending a Sports Injury Clinic. Br. J. Sports Med. 1984, 18, 18–21. [Google Scholar] [CrossRef]
- Petersen, W.; Rembitzki, I.; Liebau, C. Patellofemoral pain in athletes. Open Access J. Sports Med. 2017, 8, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Lankhorst, N.E.; Bierma-Zeinstra, S.M.; van Middelkoop, M. Factors associated with patellofemoral pain syndrome: A systematic review. Br. J. Sports Med. 2013, 47, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Davis, I.S.; Powers, C. Patellofemoral pain syndrome: Proximal, distal, and local factors—international research retreat, April 30–may 2, 2009, Baltimore, Maryland. J. Orthop. Sports Phys. Ther. 2010, 40, A1–A48. [Google Scholar] [CrossRef] [PubMed]
- Goharpey, S.; Shaterzadeh, M.; Emrani, A.; Khalesi, V. Relationship between functional tests and knee muscular isokinetic parameters in patients with patellofemoral pain syndrome. J. Med. Sci. 2007, 7, 1315–1319. [Google Scholar] [CrossRef]
- Callaghan, M.; Oldham, J. Quadriceps atrophy: To what extent does it exist in patellofemoral pain syndrome? Br. J. Sports Med. 2004, 38, 295–299. [Google Scholar] [CrossRef]
- Lee, S.-E.; Cho, S.-H. The effect of McConnell taping on vastus medialis and lateralis activity during squatting in adults with patellofemoral pain syndrome. J. Exerc. Rehabil. 2013, 9, 326–330. [Google Scholar] [CrossRef]
- Besier, T.F.; Fredericson, M.; Gold, G.E.; Beaupré, G.S.; Delp, S.L. Knee muscle forces during walking and running in patellofemoral pain patients and pain-free controls. J. Biomech. 2009, 42, 898–905. [Google Scholar] [CrossRef]
- DeHaven, K.E.; Lintner, D.M. Athletic injuries: Comparison by age, sport, and gender. Am. J. Sports Med. 1986, 14, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Meckel, Y.; Machnai, O.; Eliakim, A. Relationship among repeated sprint tests, aerobic fitness, and anaerobic fitness in elite adolescent soccer players. J. Strength Cond. Res. 2009, 23, 163–169. [Google Scholar] [CrossRef]
- Schelling, X.; Torres-Ronda, L. Conditioning for basketball: Quality and quantity of training. Strength Cond. J. 2013, 35, 89–94. [Google Scholar] [CrossRef]
- Iaia, F.M.; Ermanno, R.; Bangsbo, J. High-intensity training in football. Int. J. Sports Physiol. Perform. 2009, 4, 291–306. [Google Scholar] [CrossRef] [PubMed]
- Haff, G.G. Aquatic Cross Training for Athletes: Part I. Strength Cond. J. 2008, 30, 18–26. [Google Scholar] [CrossRef]
- Nagle, E.F.; Sanders, M.E.; Franklin, B.A. Aquatic high intensity interval training for cardiometabolic health: Benefits and training design. Am. J. Lifestyle Med. 2017, 11, 64–76. [Google Scholar] [CrossRef] [PubMed]
- Lack, S.; Barton, C.; Sohan, O.; Crossley, K.; Morrissey, D. Proximal muscle rehabilitation is effective for patellofemoral pain: A systematic review with meta-analysis. Br. J. Sports Med. 2015, 49, 1365–1376. [Google Scholar] [CrossRef]
- Dutton, R.A.; Khadavi, M.J.; Fredericson, M. Update on rehabilitation of patellofemoral pain. Curr. Sports Med. Rep. 2014, 13, 172–178. [Google Scholar] [CrossRef]
- Crouse, S.F.; Tolson, H.; Lytle, J.; Johnson, K.A.; Martin, S.E.; Green, J.S.; Oliver, J.; Carbuhn, A.; Lambert, B.; Bramhall, J.P. Predicting VO2max from treadmill performance in American-style football athletes. J. Strength Cond. Res. 2019, 33, 1028–1034. [Google Scholar]
- Berglund, I.J.; Sørås, S.E.; Relling, B.E.; Lundgren, K.M.; Kiel, I.A.; Moholdt, T. The relationship between maximum heart rate in a cardiorespiratory fitness test and in a maximum heart rate test. J. Sci. Med. Sport 2019, 22, 607–610. [Google Scholar] [CrossRef]
- Rovai, S.; Magini, A.; Cittar, M.; Masè, M.; Carriere, C.; Contini, M.; Vignati, C.; Sinagra, G.; Agostoni, P. Evidence of a double anaerobic threshold in healthy subjects. Eur. J. Prev. Cardiol. 2021, 29, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Habets, B.; Staal, J.B.; Tijssen, M.; van Cingel, R. Intrarater reliability of the Humac NORM isokinetic dynamometer for strength measurements of the knee and shoulder muscles. BMC Res. Notes 2018, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Corum, M.; Basoglu, C.; Yakal, S.; Sahinkaya, T.; Aksoy, C. Effects of whole body vibration training on isokinetic muscular performance, pain, function, and quality of life in female patients with patellofemoral pain: A randomized controlled trial. J. Musculoskelet. Neuronal Interact. 2018, 18, 473–484. [Google Scholar] [PubMed]
- Dingenen, B.; Truijen, J.; Bellemans, J.; Gokeler, A. Test–retest reliability and discriminative ability of forward, medial and rotational single-leg hop tests. Knee 2019, 26, 978–987. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Westrick, R.; Diebal, A.; Marks, C.; Gerber, J.P. Immediate effects of lumbopelvic manipulation and lateral gluteal kinesio taping on unilateral patellofemoral pain syndrome: A pilot study. Sports Health 2013, 5, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Coughlan, G.F.; Fullam, K.; Delahunt, E.; Gissane, C.; Caulfield, B.M. A comparison between performance on selected directions of the star excursion balance test and the Y balance test. J. Athl. Train. 2012, 47, 366–371. [Google Scholar] [CrossRef]
- Anderson, A.F.; Irrgang, J.J.; Kocher, M.S.; Mann, B.J.; Harrast, J.J.; Committee, I.K.D. The International Knee Documentation Committee subjective knee evaluation form: Normative data. Am. J. Sports Med. 2006, 34, 128–135. [Google Scholar] [CrossRef]
- Kim, J.G.; Ha, J.K.; Lee, J.Y.; Seo, S.S.; Choi, C.H.; Lee, M.C. Translation and validation of the Korean version of the international knee documentation committee subjective knee form. Knee Surg. Relat. Res. 2013, 25, 106–111. [Google Scholar] [CrossRef][Green Version]
- Higgins, L.D.; Taylor, M.K.; Park, D.; Ghodadra, N.; Marchant, M.; Pietrobon, R.; Cook, C. Reliability and validity of the International Knee Documentation Committee (IKDC) subjective knee form. Jt. Bone Spine 2007, 74, 594–599. [Google Scholar] [CrossRef]
- Kruel, L.F.M.; Posser, M.S.; Alberton, C.L.; Pinto, S.S.; Oliveira, A.D.S. Comparison of energy expenditure between continuous and interval water aerobic routines. Int. J. Aquat. Res. Educ. 2009, 3, 9. [Google Scholar] [CrossRef]
- ACSM. ACSM’s Health-Related Physical Fitness Assessment Manual; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Herman, L.; Foster, C.; Maher, M.; Mikat, R.; Porcari, J. Validity and reliability of the session RPE method for monitoring exercise training intensity. S. Afr. J. Sports Med. 2006, 18, 14–17. [Google Scholar] [CrossRef]
- Andersen, A.B.; Bejder, J.; Bonne, T.; Olsen, N.V.; Nordsborg, N. Repeated Wingate sprints is a feasible high-quality training strategy in moderate hypoxia. PLoS ONE 2020, 15, e0242439–e0242452. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liang, L.; Wang, D.; Tang, Y.; Wu, X.; Li, L.; Liu, Y. Cycling with low saddle height is related to increased knee adduction moments in healthy recreational cyclists. Eur. J. Sport Sci. 2020, 20, 461–467. [Google Scholar] [CrossRef]
- Pescatello, L.S.; Riebe, D.; Thompson, P.D. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Neal, B.S.; Lack, S.D.; Lankhorst, N.E.; Raye, A.; Morrissey, D.; Van Middelkoop, M. Risk factors for patellofemoral pain: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 270–281. [Google Scholar] [CrossRef] [PubMed]
- Holmberg, P.M.; Gorman, A.D.; Jenkins, D.G.; Kelly, V.G. Lower-Body Aquatic Training Prescription for Athletes. J. Strength Cond. Res. 2021, 35, 859–869. [Google Scholar] [CrossRef]
- Ahmed, T.A.E.; Seleem, H.A.I.; Elsayed, G.M.Y. Effects of Eight Weeks Aquatic-Non-aquatic Training program on Aerobic Fitness and Physical preparation in junior Basketball Player. Life Sci. J. 2019, 16, 111–118. [Google Scholar]
- Arazi, H.; Eston, R.; Asadi, A.; Roozbeh, B.; Zarei, A.S. Type of ground surface during plyometric training affects the severity of exercise-induced muscle damage. Sports 2016, 4, 15. [Google Scholar] [CrossRef]
- Miller, M.G.; Cheatham, C.C.; Porter, A.R.; Ricard, M.D.; Hennigar, D.; Berry, D.C. Chest-and waist-deep aquatic plyometric training and average force, power, and vertical-jump performance. Int. J. Aquat. Res. Educ. 2007, 1, 6–18. [Google Scholar] [CrossRef][Green Version]
- Alkatan, M.; Machin, D.R.; Baker, J.R.; Akkari, A.S.; Park, W.; Tanaka, H. Effects of swimming and cycling exercise intervention on vascular function in patients with osteoarthritis. Am. J. Cardiol. 2016, 117, 141–145. [Google Scholar] [CrossRef]
- Salacinski, A.J.; Krohn, K.; Lewis, S.F.; Holland, M.L.; Ireland, K.; Marchetti, G. The effects of group cycling on gait and pain-related disability in individuals with mild-to-moderate knee osteoarthritis: A randomized controlled trial. J. Orthop. Sports Phys. Ther. 2012, 42, 985–995. [Google Scholar] [CrossRef]
- Asplund, C.; St Pierre, P. Knee pain and bicycling: Fitting concepts for clinicians. Physician Sportsmed. 2004, 32, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Versey, N.G.; Halson, S.L.; Dawson, B.T. Water immersion recovery for athletes: Effect on exercise performance and practical recommendations. Sports Med. 2013, 43, 1101–1130. [Google Scholar] [CrossRef] [PubMed]
- Wilcock, I.M.; Cronin, J.B.; Hing, W.A. Physiological response to water immersion. Sports Med. 2006, 36, 747–765. [Google Scholar] [CrossRef]
- Torres-Ronda, L.; i del Alcázar, X.S. The properties of water and their applications for training. J. Hum. Kinet. 2014, 44, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Guney, H.; Yuksel, I.; Kaya, D.; Doral, M.N. The relationship between quadriceps strength and joint position sense, functional outcome and painful activities in patellofemoral pain syndrome. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2966–2972. [Google Scholar] [CrossRef]
- Kaya, D.; Citaker, S.; Kerimoglu, U.; Atay, O.A.; Nyland, J.; Callaghan, M.; Yakut, Y.; Yüksel, I.; Doral, M.N. Women with patellofemoral pain syndrome have quadriceps femoris volume and strength deficiency. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Dvir, Z.; Halperin, N.; Shklar, A.; Robinson, D. Quadriceps function and patellofemoral pain syndrome. Part I: Pain provocation during concentric and eccentric isokinetic activity. Isokinet. Exerc. Sci. 1991, 1, 26–30. [Google Scholar] [CrossRef]
- Ko, D.-H.; Choi, Y.-C.; Lee, D.-S. The Effect of Short-Term Wingate-Based High Intensity Interval Training on Anaerobic Power and Isokinetic Muscle Function in Adolescent Badminton Players. Children 2021, 8, 458. [Google Scholar] [CrossRef]
- Fang, B.; Kim, Y.; Choi, M. Effect of Cycle-Based High-Intensity Interval Training and Moderate to Moderate-Intensity Continuous Training in Adolescent Soccer Players. Healthcare 2021, 9, 1628. [Google Scholar] [CrossRef]
- Fältström, A.; Hägglund, M.; Hedevik, H.; Kvist, J. Poor Validity of Functional Performance Tests to Predict Knee Injury in Female Soccer Players With or Without Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2021, 49, 1441–1450. [Google Scholar] [CrossRef]
- Wilk, K.E.; Romaniello, W.T.; Soscia, S.M.; Arrigo, C.A.; Andrews, J.R. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J. Orthop. Sports Phys. Ther. 1994, 20, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-K.; Ahn, S.-H. Effects of balance evaluation comparison of dynamic balance and Y balance. J. Exerc. Rehabil. 2018, 14, 939–943. [Google Scholar] [CrossRef] [PubMed]
- Ringhof, S.; Stein, T. Biomechanical assessment of dynamic balance: Specificity of different balance tests. Hum. Mov. Sci. 2018, 58, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, E.T.; Barle, M.; Glassmann, E.; Jung, M.-K. Interrater and test-retest reliability of the Y balance test in healthy, early adolescent female athletes. Int. J. Sports Phys. Ther. 2019, 14, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Powden, C.J.; Dodds, T.K.; Gabriel, E.H. The reliability of the star excursion balance test and lower quarter Y-balance test in healthy adults: A systematic review. Int. J. Sports Phys. Ther. 2019, 14, 683–694. [Google Scholar] [CrossRef]
- Veldema, J.; Jansen, P. Aquatic therapy in stroke rehabilitation: Systematic review and meta-analysis. Acta Neurol. Scand. 2021, 143, 221–241. [Google Scholar] [CrossRef] [PubMed]
- Pinto, C.; Salazar, A.P.; Marchese, R.R.; Stein, C.; Pagnussat, A.S. The effects of hydrotherapy on balance, functional mobility, motor status, and quality of life in patients with Parkinson disease: A systematic review and meta-analysis. PMR 2019, 11, 278–291. [Google Scholar] [CrossRef]
- Bento, P.C.B.; Lopes, M.D.F.A.; Cebolla, E.C.; Wolf, R.; Rodacki, A.L. Effects of water-based training on static and dynamic balance of older women. Rejuvenation Res. 2015, 18, 326–331. [Google Scholar] [CrossRef]
- Takacs, J.; Carpenter, M.G.; Garland, S.J.; Hunt, M.A. The role of neuromuscular changes in aging and knee osteoarthritis on dynamic postural control. Aging Dis. 2013, 4, 84–89. [Google Scholar]
- Sanchez-Ramirez, D.C.; van der Leeden, M.; Knol, D.L.; van der Esch, M.; Roorda, L.D.; Verschueren, S.; van Dieën, J.; Lems, W.F.; Dekker, J. Association of postural control with muscle strength, proprioception, self-reported knee instability and activity limitations in patients with knee osteoarthritis. J. Rehabil. Med. 2013, 45, 192–197. [Google Scholar] [CrossRef]
- Dammerer, D.; Liebensteiner, M.; Kujala, U.; Emmanuel, K.; Kopf, S.; Dirisamer, F.; Giesinger, J. Validation of the German version of the Kujala score in patients with patellofemoral instability: A prospective multi-centre study. Arch. Orthop. Trauma Surg. 2018, 138, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Cerciello, S.; Corona, K.; Morris, B.J.; Visonà, E.; Maccauro, G.; Maffulli, N.; Ronga, M. Cross-cultural adaptation and validation of the Italian versions of the Kujala, Larsen, Lysholm and Fulkerson scores in patients with patellofemoral disorders. J. Orthop. Traumatol. 2018, 19, 18. [Google Scholar] [CrossRef] [PubMed]
- Weitzel, P.P.; Richmond, J.C. Critical evaluation of different scoring systems of the knee. Sports Med. Arthrosc. Rev. 2002, 10, 183–190. [Google Scholar] [CrossRef]
- Siqueira, D.A.; Baraúna, M.A.; Dionísio, V.C. Functional evaluation of the knee in subjects with patellofemoral pain syndrome (PFPS): Comparison between KOS and IKDC scales. Rev. Bras. De Med. Do Esporte 2012, 18, 400–403. [Google Scholar] [CrossRef]
- Becker, B.E. Aquatic therapy: Scientific foundations and clinical rehabilitation applications. PMR 2009, 1, 859–872. [Google Scholar] [CrossRef]
| Variables | AT (n = 27) | BT (n = 27) | t or χ2 | p-Values |
|---|---|---|---|---|
| Age, years | 20.8 ± 1.7 | 20.9 ± 1.9 | 0.031 | 0.976 |
| Height, cm | 179.1 ± 6.0 | 178.9 ± 6.5 | 0.823 | 0.420 |
| Weight, kg | 75.8 ± 5.5 | 76.3 ± 6.7 | −1.027 | 0.316 |
| BMI, kg/m2 | 23.6 ± 1.8 | 23.8 ± 1.9 | −2.239 | 0.210 |
| Left/Right side | 12/15 | 16/11 | 0.667 | 0.587 |
| Dominant/Non-Dominant | 10/17 | 12/15 | 0.307 | 0.782 |
| Variables | Group | Pre-Training | Post-Training | Difference (%) | p-Values | Time × Group p-Values |
|---|---|---|---|---|---|---|
| VO2 peak, mL/kg/min | AT | 43.2 ± 6.3 | 56.1 ± 8.4 | 29.9 | <0.001 | 0.021 |
| BT | 44.7 ± 7.1 | 53.3 ± 8.3 | 19.2 | <0.001 | ||
| p-values | 0.423 | 0.015 | ||||
| Anaerobic threshold, % | AT | 67.2 ± 9.3 | 74.5 ± 6.7 | 10.9 | <0.001 | 0.034 |
| BT | 66.1 ± 8.9 | 70.3 ± 7.1 | 6.4 | 0.005 | ||
| p-values | 0.510 | 0.020 | ||||
| HR recovery 1 min, % | AT | 56.4 ± 6.6 | 69.1 ± 10.7 | 22.5 | <0.001 | 0.011 |
| BT | 56.3 ± 7.9 | 66.3 ± 11.1 | 17.8 | 0.009 | ||
| p-values | 0.399 | 0.010 |
| Variables | Group | Pre-Training | Post-Training | Difference (%) | p-Values | Time × Group p-Values |
|---|---|---|---|---|---|---|
| Extension strength, Nm/kg, % | AT | 255.2 ± 45.1 | 305.6 ± 48.4 | 19.7 | 0.010 | 0.129 |
| BT | 258.9 ± 50.0 | 295.9 ± 52.7 | 14.3 | 0.012 | ||
| p-values | 0.404 | 0.332 | ||||
| Flexion strength, Nm/kg, % | AT | 172.3 ± 21.0 | 182.5 ± 25.6 | 5.9 | 0.106 | 0.230 |
| BT | 170.3 ± 29.1 | 179.8 ± 31.3 | 5.6 | 0.216 | ||
| p-values | 0.215 | 0.320 | ||||
| H:Q ratio | AT | 66.2 ± 16.0 | 59.7 ± 15.6 | −11.5 | 0.004 | 0.210 |
| BT | 65.8 ± 19.1 | 60.8 ± 11.3 | −7.6 | 0.007 | ||
| p-values | 0.469 | 0.221 |
| Variables | Group | Pre-Training | Post-Training | Difference (%) | p-Values | Time × Group p-Values |
|---|---|---|---|---|---|---|
| Single, cm | AT | 146.1 ± 20.3 | 169.3 ± 19.4 | 15.9 | <0.001 | 0.515 |
| BT | 147.4 ± 19.3 | 170.2 ± 23.3 | 15.5 | <0.001 | ||
| p-values | 0.521 | 0.215 | ||||
| Triple, cm | AT | 460.3 ± 41.5 | 493.3 ± 42.9 | 7.2 | <0.001 | 0.611 |
| BT | 454.3 ± 43.1 | 486.4 ± 54.3 | 7.1 | <0.001 | ||
| p-values | 0.419 | 0.318 | ||||
| Crossover, cm | AT | 412.7 ± 35.7 | 444.9 ± 31.4 | 7.8 | <0.001 | 0.318 |
| BT | 416.2 ± 37.3 | 454.4 ± 33.5 | 9.2 | <0.001 | ||
| p-values | 0.514 | 0.325 | ||||
| 6 m, s | AT | 2.19 ± 0.17 | 2.10 ± 0.13 | −4.1 | 0.011 | 0.119 |
| BT | 2.21 ± 0.16 | 2.07 ± 0.11 | −6.3 | 0.018 | ||
| p-values | 0.128 | 0.498 |
| Variables | Group | Pre-Training | Post-Training | Difference (%) | p-Values | Time × Group p-Values |
|---|---|---|---|---|---|---|
| Anterior | AT | 54.3 ± 15.3 | 70.5 ± 17.1 | 29.8 | 0.006 | 0.014 |
| BT | 56.1 ± 17.0 | 63.3 ± 19.4 | 12.8 | 0.012 | ||
| p-values | 0.621 | 0.008 | ||||
| Posteromedial | AT | 66.1 ± 19.6 | 78.7 ± 21.6 | 19.1 | 0.021 | 0.016 |
| BT | 65.3 ± 21.0 | 70.6 ± 23.4 | 8.1 | 0.010 | ||
| p-values | 0.204 | 0.006 | ||||
| Posterolateral | AT | 65.9 ± 25.9 | 79.6 ± 22.7 | 20.8 | <0.001 | 0.011 |
| BT | 62.5 ± 26.1 | 72.4 ± 23.8 | 15.8 | 0.005 | ||
| p-values | 0.634 | 0.012 | ||||
| Total | AT | 73.1 ± 18.3 | 85.4 ± 15.1 | 16.8 | <0.001 | 0.035 |
| BT | 71.7 ± 20.1 | 79.7 ± 17.6 | 11.2 | 0.003 | ||
| p-values | 0.540 | 0.015 |
| Variables | Group | Pre-Training | Post-Training | Difference (%) | p-Values | Time × Group p-Values |
|---|---|---|---|---|---|---|
| IKDC score | AT | 65.2 ± 13.9 | 88.4 ± 13.3 | 35.6 | <0.001 | 0.019 |
| BT | 67.6 ± 15.0 | 85.8 ± 12.1 | 26.9 | 0.004 | ||
| p-values | 0.241 | 0.022 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fang, B.; Kim, Y.-h.; Choi, M.-y. Effects of High-Intensity Aquatic or Bicycling Training in Athletes with Unilateral Patellofemoral Pain Syndrome. Int. J. Environ. Res. Public Health 2022, 19, 4675. https://doi.org/10.3390/ijerph19084675
Fang B, Kim Y-h, Choi M-y. Effects of High-Intensity Aquatic or Bicycling Training in Athletes with Unilateral Patellofemoral Pain Syndrome. International Journal of Environmental Research and Public Health. 2022; 19(8):4675. https://doi.org/10.3390/ijerph19084675
Chicago/Turabian StyleFang, Bin, Yong-hwan Kim, and Moon-young Choi. 2022. "Effects of High-Intensity Aquatic or Bicycling Training in Athletes with Unilateral Patellofemoral Pain Syndrome" International Journal of Environmental Research and Public Health 19, no. 8: 4675. https://doi.org/10.3390/ijerph19084675
APA StyleFang, B., Kim, Y.-h., & Choi, M.-y. (2022). Effects of High-Intensity Aquatic or Bicycling Training in Athletes with Unilateral Patellofemoral Pain Syndrome. International Journal of Environmental Research and Public Health, 19(8), 4675. https://doi.org/10.3390/ijerph19084675







