Prevention of Non-Contact Anterior Cruciate Ligament Injuries among Youth Female Athletes: An Umbrella Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Types
2.2. Participants
2.3. Interventions
2.4. Outcome Measures
2.5. Exclusion Criteria
2.6. Sources of Information
2.7. Selection of Studies
2.8. Data Extraction and Management
2.9. Risk of Bias Assessment in Included Studies
2.10. Data Synthesis
3. Results
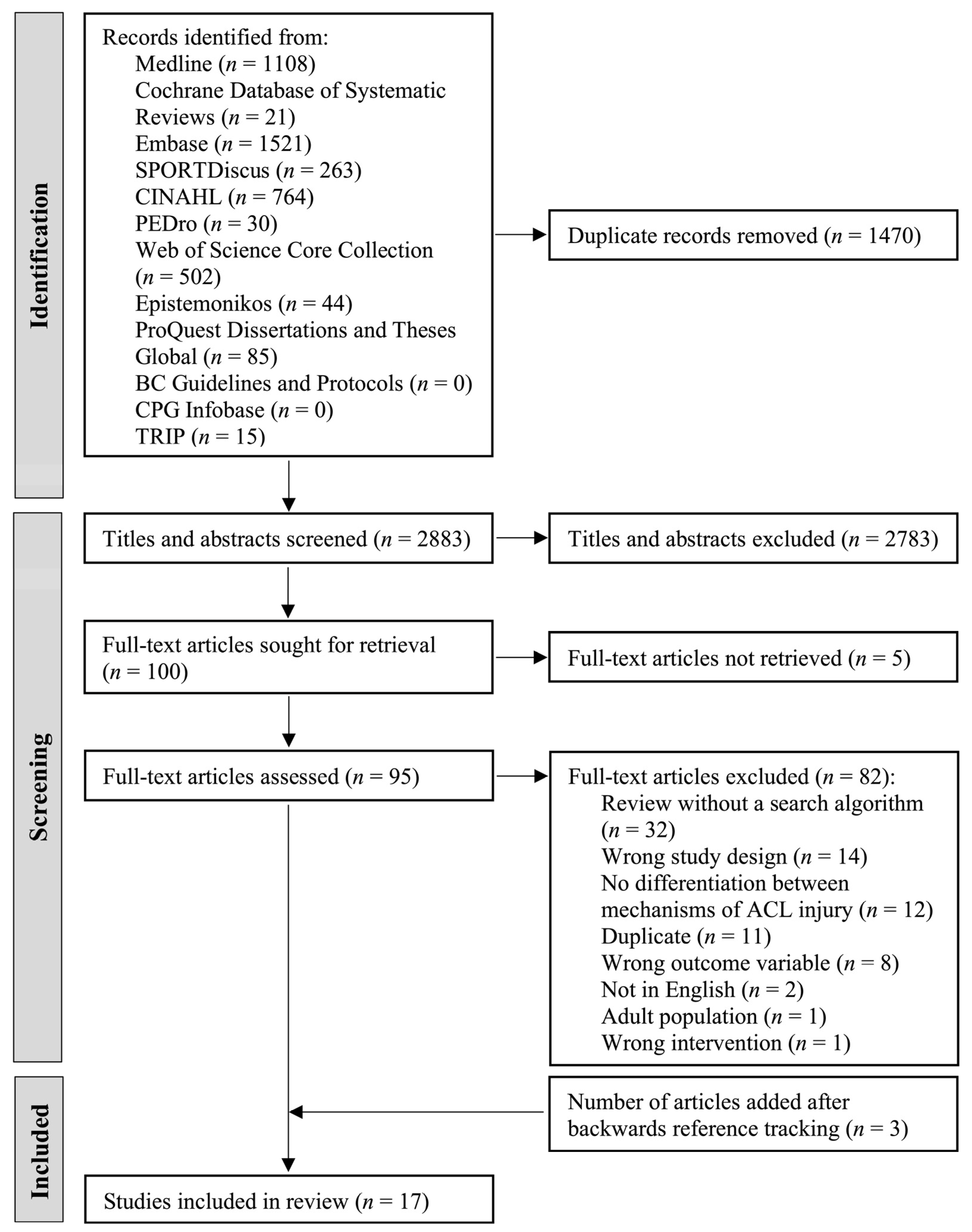
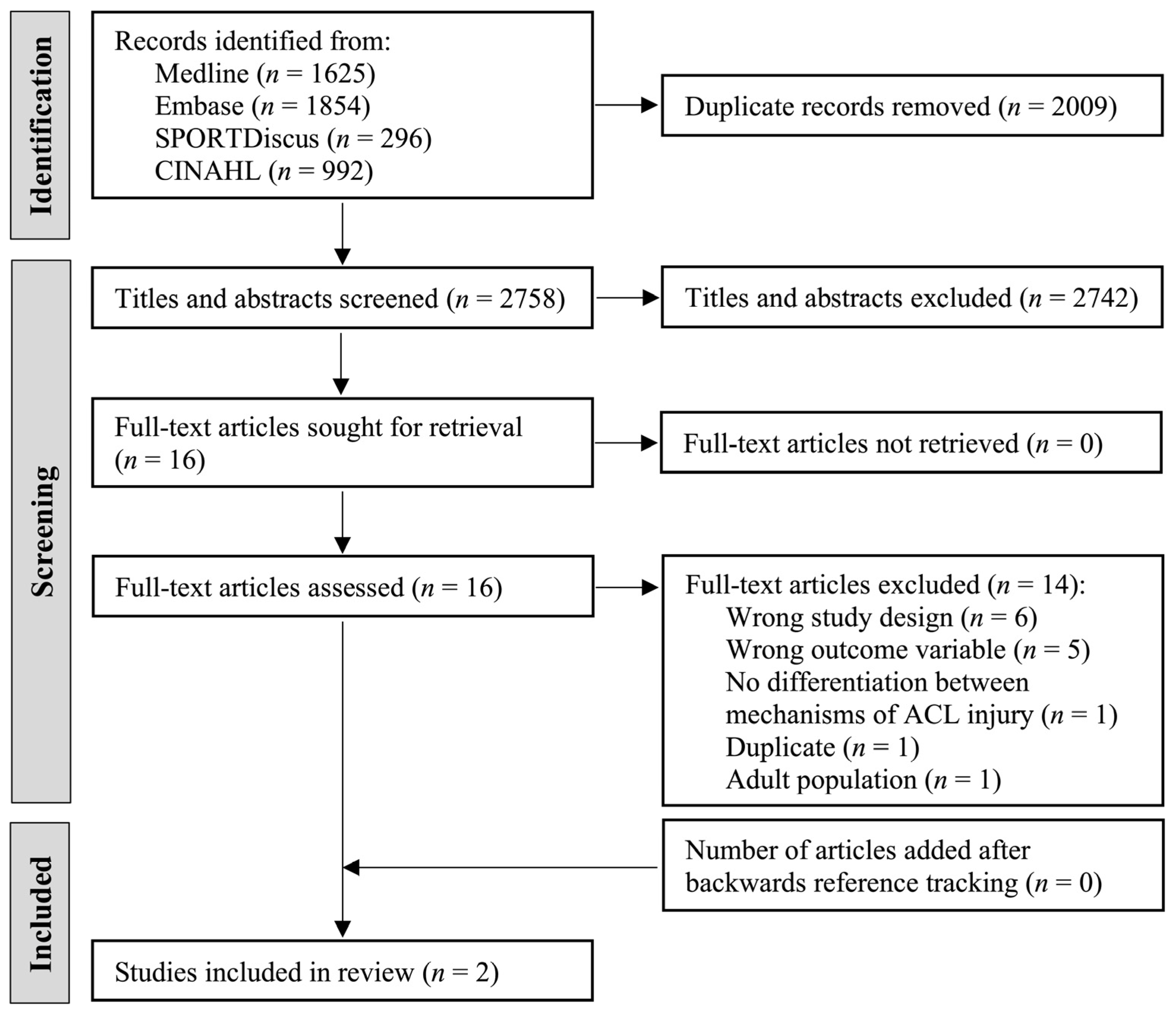
3.1. Literature Search Results
3.1.1. Reviews
3.1.2. Primary Literature
3.2. Study Characteristics
3.2.1. Reviews
3.2.2. Primary Literature
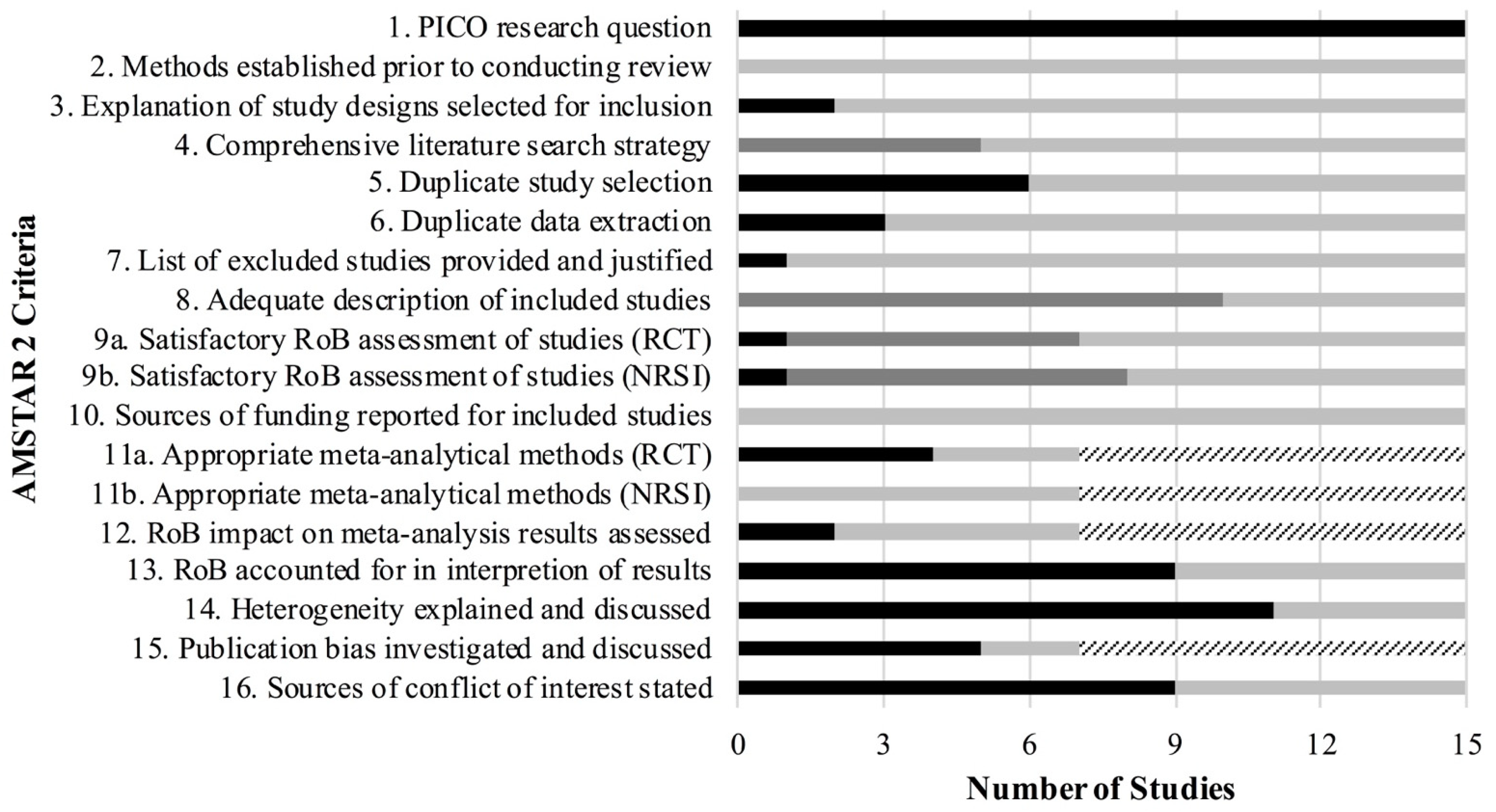
3.3. Risk of Bias in Included Studies
3.3.1. Reviews
3.3.2. Primary Literature
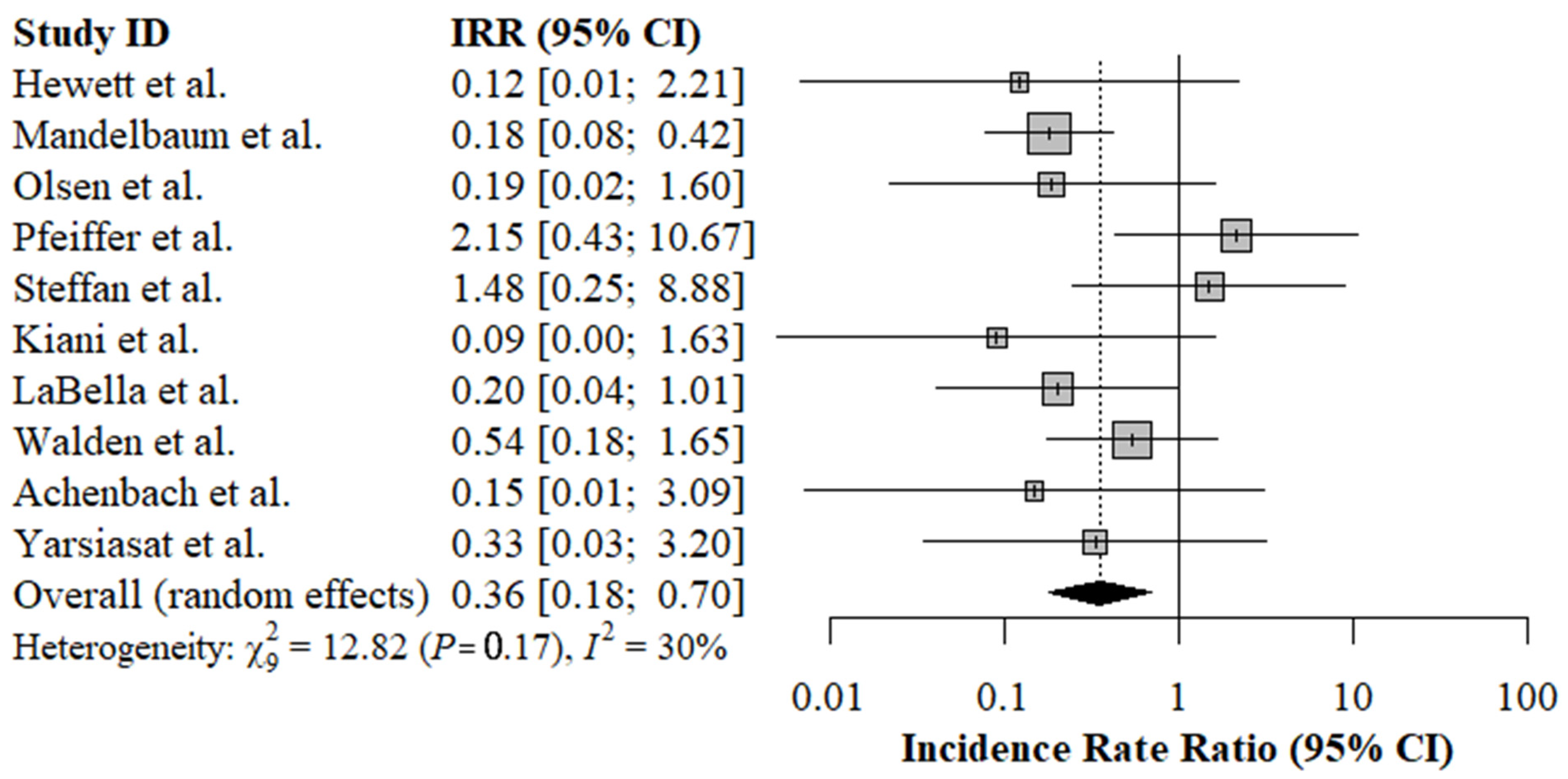
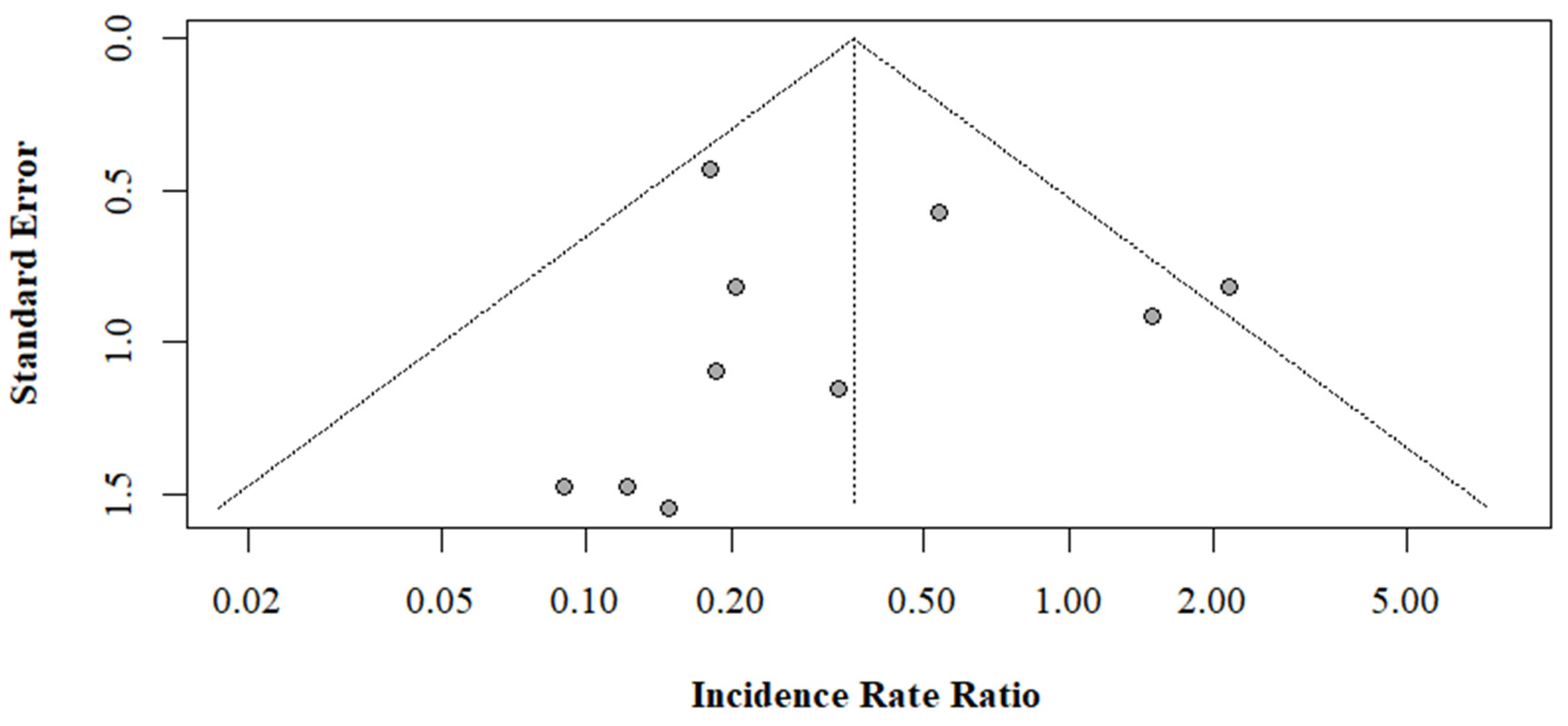
3.4. Effectiveness of ACL Injury Prevention Programs
3.5. Specific Training Components
3.6. Duration, Frequency, and Timing of Interventions
4. Discussion
4.1. Effectiveness of ACL Injury Prevention Programs
4.2. Intervention Components
4.3. Quality Assessment
4.4. Strengths and Limitations
4.5. Recommendations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. Medline Search Terms
- Anterior Cruciate Ligament Injuries/
- (Anterior Cruciate Ligament adj (Injur* or tear or rupture)).mp.
- (ACL adj (Injur* or tear or rupture)).mp.
- Knee Injuries/
- Knee Injur*.mp.
- 1 or 2 or 3 or 4 or 5
- Athletic Injuries/pc [prevention & control]
- (Prevent* or Intervention*).mp.
- (Program* or Programme*).mp.
- Exercise Therapy/or “Physical Education and Training”/or Physical Conditioning, Human/
- Plyometric Exercise/or Muscle Stretching Exercises/or Resistance Training/or Warm-Up Exercise/
- Training*.mp.
- (Propriocept* or Plyometric* or Stretch* or Resistance* or Warm-up* or Neuromuscular* or Strength* or Condition* or Agility*).mp.
- Education/
- Educat*.mp.
- Braces/
- Brac*.mp.
- 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17
- Adolescent/
- (Adolesc* or Teen* or Youth* or Young*).mp.
- Child/
- Child*.mp.
- Pediatrics/
- P?ediatric*.mp.
- 19 or 20 or 21 or 22 or 23 or 24
- Female/
- Female*.mp.
- Athlete/
- (Athlete* or Female Athlete*).mp.
- 26 or 27 or 28 or 29
- (meta or synthesis or literature).ab. or randomized.hw. or published.ab. or meta-analysis.pt. or systematic review.pt. or extraction.ab. or trials.hw. or controlled.hw. or search.ab. or MEDLINE.ab. or selection.ab. or sources.ab. or trials.ab. or review.ab. or review.pt. or articles.ab. or reviewed.ab. or english.ab. or language.ab.
- 6 and 18 and 25 and 30
- 31 and 32
Appendix A.2. Embase Search Terms
- anterior cruciate ligament injury/or anterior cruciate ligament rupture/
- (Anterior Cruciate Ligament adj (Injur* or tear or rupture)).mp.
- (ACL adj (Injur* or tear or rupture)).mp.
- knee injury/
- Knee Injur*.mp.
- 1 or 2 or 3 or 4 or 5
- sport injury/pc [prevention & control]
- (Prevent* or Intervention*).mp.
- (Program* or Programme*).mp.
- kinesiotherapy/or leg exercise/or muscle training/or neuromuscular facilitation/or plyometrics/or stretching exercise/or muscle exercise/or resistance training/or “squatting (exercise)”/or warm up/or training/
- Training*.mp.
- (Propriocept* or Plyometric* or Stretch* or Resistance* or Warm-up* or Neuromuscular* or Strength* or Condition* or Agility*).mp.
- education/
- Educat*.mp.
- brace/
- Brac*.mp.
- 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16
- adolescent/
- (Adolesc* or Teen* or Youth* or Young*).mp.
- child/
- Child*.mp.
- pediatrics/
- P?ediatric*.mp.
- 18 or 19 or 20 or 21 or 22 or 23
- female/
- Female*.mp.
- athlete/
- (Athlete* or Female Athlete*).mp.
- 25 or 26 or 27 or 28
- (meta or synthesis or literature).ab. or randomized.hw. or published.ab. or meta analysis/or “systematic review”/or extraction.ab. or trials.hw. or controlled.hw. or search.ab. or MEDLINE.ab. or selection.ab. or sources.ab. or trials.ab. or review.ab. or review.pt. or articles.ab. or reviewed.ab. or english.ab. or language.ab.
- 6 and 17 and 24 and 29
- 30 and 31
Appendix A.3. Cochrane Database of Systematic Reviews Search Terms
- (Anterior Cruciate Ligament adj (Injur* or tear or rupture)).mp.
- (ACL adj (Injur* or tear or rupture)).mp.
- Knee Injur*.mp.
- 1 or 2 or 3
- (Prevent* or Intervention*).mp.
- (Program* or Programme*).mp.
- Training*.mp.
- (Propriocept* or Plyometric* or Stretch* or Resistance* or Warm-up* or Neuromuscular* or Strength* or Condition* or Agility*).mp.
- Educat*.mp.
- Brac*.mp.
- 5 or 6 or 7 or 8 or 9 or 10
- (Adolesc* or Teen* or Youth* or Young*).mp.
- Child*.mp.
- P?ediatric*.mp.
- 12 or 13 or 14
- Female*.mp.
- (Athlete* or Female Athlete*).mp.
- 16 or 17
- 4 and 11 and 15 and 18
Appendix A.4. SPORTDiscus Search Terms
- S1.
- DE “ANTERIOR cruciate ligament injuries”
- S2.
- (Anterior Cruciate Ligament N1 (Injur* or tear or rupture))
- S3.
- (ACL N1 (Injur* or tear or rupture))
- S4.
- DE “KNEE injuries”
- S5.
- Knee Injur*
- S6.
- S1 OR S2 OR S3 OR S4 OR S5
- S7.
- DE “SPORTS injury prevention”
- S8.
- Prevent* or Intervention*
- S9.
- Program* or Programme*
- S10.
- (DE “EXERCISE therapy” OR DE “EXERCISE therapy for children”) OR DE “PHYSICAL training & conditioning”
- S11.
- DE “PLYOMETRICS” OR DE “STRETCH (Physiology)” OR DE “RESISTANCE training” OR DE “WARMUP” OR DE “STRENGTH training”
- S12.
- Training*
- S13.
- Propriocept* or Plyometric* or Stretch* or Resistance* or Warm-up* or Neuromuscular* or Strength* or Condition* or Agility*
- S14.
- DE “EDUCATION”
- S15.
- Educat*
- S16.
- DE “SPORTS injury prevention equipment”
- S17.
- Brac*
- S18.
- S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17
- S19.
- DE “TEENAGERS” OR DE “YOUTH” OR DE “CHILDREN” OR DE “PEDIATRICS”
- S20.
- Adolesc* or Teen* or Youth* or Young*
- S21.
- Child* OR P#ediatric*
- S22.
- S19 OR S20 OR S21
- S23.
- DE “WOMEN” OR DE “WOMEN & sports” OR DE “ATHLETES” OR DE “WOMEN athletes”
- S24.
- Female* OR Athlete* OR Female Athlete*
- S25.
- S23 OR S24
- S26.
- AB ((meta or synthesis or literature)) OR SU randomized OR AB published OR (meta-analysis or systematic review or review) OR AB extraction OR SU trials OR SU controlled OR AB ((search or MEDLINE or selection or sources or trials or review)) OR AB ((articles or reviewed)) OR AB ((english or language))
- S27.
- S6 AND S18 AND S22 AND S25
- S28.
- S26 AND S27
Appendix A.5. CINAHL Search Terms
- S1.
- (MH “Anterior Cruciate Ligament Injuries”)
- S2.
- (Anterior Cruciate Ligament N1 (Injur* or tear or rupture))
- S3.
- (ACL N1 (Injur* or tear or rupture))
- S4.
- (MH “Knee Injuries”)
- S5.
- Knee Injur*
- S6.
- S1 OR S2 OR S3 OR S4 OR S5
- S7.
- Injury prevent*
- S8.
- Prevent* OR Intervention*
- S9.
- Program* or Programme*
- S10.
- (MH “Therapeutic Exercise”) OR ((MH “Physical Education and Training”)) OR (MH “Athletic Training Programs”)
- S11.
- (MH “Plyometrics”) OR (MH “Balance Training, Physical”) OR (MH “Resistance Training”) OR (MH “Stretching”) OR (MH “Warm-Up Exercise”)
- S12.
- Training*
- S13.
- Propriocept* or Plyometric* or Stretch* or Resistance* or Warm-up* or Neuromuscular* or Strength* or Condition* or Agility*
- S14.
- (MH “Education”)
- S15.
- Educat*
- S16.
- (MH “Orthoses”)
- S17.
- Brac*
- S18.
- S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17
- S19.
- (MH “Adolescence”) OR (MH “Child”)
- S20.
- Adolesc* OR Teen* OR Youth* OR Young* OR Child* OR P?ediatric*
- S21.
- S19 OR S20
- S22.
- (MH “Female”)
- S23.
- (MH “Athletes”)
- S24.
- Female* OR Athlete* OR Female Athlete*
- S25.
- S22 OR S23 OR S24
- S26.
- AB (meta or synthesis or literature) OR MW randomized OR AB published OR PT (meta-analysis or systematic review) OR AB extraction OR MW (trials or controlled) OR AB (search or MEDLINE or selection or sources or trials or review) OR PT review OR AB (articles or reviewed) OR AB (english or language)
- S27.
- S6 AND S18 AND S21 AND S25
- S28.
- S26 AND S27
Appendix A.6. PEDro Search Terms
Appendix A.7. Web of Science Core Collection Search Terms
- TS = (Anterior Cruciate Ligament NEAR (Injur* or tear or rupture))
- TS = (ACL NEAR (Injur* or tear or rupture))
- TS = Knee Injur*
- #3 OR #2 OR #1
- TS = (Prevent* or Intervention*)
- TS = (Program* or Programme*)
- TS = Training*
- TS = (Propriocept* or Plyometric* or Stretch* or Resistance* or Warm-up* or Neuromuscular* or Strength* or Condition* or Agility*)
- TS = Educat*
- TS = Brac*
- #10 OR #9 OR #8 OR #7 OR #6 OR #5
- TS = (Adolesc* or Teen* or Youth* or Young*)
- TS = Child*
- TS = P$ediatric*
- #14 OR #13 OR #12
- TS = Female*
- TS = (Athlete* or Female Athlete*)
- #17 OR #16
- #18 AND #15 AND #11 AND #4
- AB = (meta OR synthesis OR literature)
- KP = randomized
- AB = published
- TS = (meta-analysis OR systematic review)
- AB = extraction
- KP = (trials OR controlled)
- AB = (search OR MEDLINE OR selection OR sources OR trials OR review)
- TS = review
- AB = (articles OR reviewed) OR AB = (english OR language)
- #28 OR #27 OR #26 OR #25 OR #24 OR #23 OR #22 OR #21 OR #20
- #29 AND #19
Appendix A.8. Epistemonikos Search Terms
Appendix A.9. ProQuest Dissertations and Theses Global Search Terms
Appendix A.10. TRIP Database Search Terms
Appendix B
| Study | Main Reason for Exclusion |
|---|---|
| Chiaro [56] | Adult population |
| Albaugh et al. [57] No author [58] Halvorson [59] May et al. [60] Della Villa et al. [61] | Could not find full-text |
| Herman et al. [62] Dompier [63] Hespanhol Junior et al. [64] No author [65] Meyer et al. [66] Elliot et al. [67] Myer et al. [18] Hewett et al. [68] Silvers et al. [69] Sugimoto et al. [54] Sugimoto et al. [17] | Duplicate |
| Rishiraj et al. [70] Elliot et al. [67] Gokeler et al. [71] Hewett et al. [72] Myer et al. [73] Laible et al. [74] Myer et al. [75] Dai et al. [76] Zakieh et al. [77] Paulson et al. [78] LaBella et al. [79] Arabia et al. [80] Myer et al. [81] Padua et al. [53] Bonnette et al. [82] Nessler et al. [83] Kiefer et al. [84] Hewett et al. [68] Myer et al. [85] Silvers et al. [69] Dharamsi et al. [86] Labella et al. [87] Myer et al. [88] Bencke et al. [89] Myer et al. [90] Mehl et al. [91] Ladenhauf et al. [92] Graziano et al. [93] Kelly [94] Acevedo et al. [95] Brophy et al. [96] Bisciotti et al. [97] | Narrative review without a search algorithm |
| Taylor et al. [98] Chang et al. [99] Sugimoto et al. [54] Assaly et al. [100] Myer et al. [18] Sugimoto et al. [101] Ramirez et al. [102] Crossley et al. [103] Sugimoto et al. [55] Petushek et al. [104] Grimm et al. [105] Huang et al. [106] | No differentiation between mechanisms of ACL injury in results and/or analyses |
| Zheng et al. [107] Romero-Moraleda et al. [108] | Not in English |
| Herzberg et al. [109] | Wrong intervention |
| Willadsen et al. [110] Weber et al. [111] Trojian et al. [112] Emery et al. [113] Lim et al. [114] Ter Stege et al. [115] Barber-Westin et al. [116] Monajati et al. [117] | Wrong outcomes |
| Paszkewicz et al. [118] Prather [119] Barber-Westin et al. [120] No author [121] Bottino [122] Moksnes et al. [123] Hornbeck et al. [124] Halvorson [125] Powers et al. [126] Howe [127] Brunner et al. [24] Garcia [128] Nagano et al. [129] Queen [130] | Wrong study design |
| Study | Main Reason for Exclusion |
|---|---|
| Lewis et al. [131] Jari et al. [132] Sibbala et al. [133] Owoeye et al. [134] Richmond et al. [135] | Wrong outcomes |
| Paulson et al. [79] Halvorson [126] Potera [136] No author [122] Murray et al. [137] Decker et al. [138] | Wrong study design |
| Foss et al. [139] | No differentiation between mechanisms of ACL injury |
| Omi et al. [140] | Adult population |
| Achenbach et al. [31] | Duplicate |
References
- Joseph, A.M.; Collins, C.L.; Henke, N.M.; Yard, E.E.; Fields, S.K.; Comstock, R.D. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J. Athl. Train. 2013, 48, 810–817. [Google Scholar] [CrossRef] [PubMed]
- Mather, R.C., 3rd; Koenig, L.; Kocher, M.S.; Dall, T.M.; Gallo, P.; Scott, D.J.; Bach, B.R.J.; Spindler, K.P. Societal and economic impact of anterior cruciate ligament tears. J. Bone Jt. Surg. Am. 2013, 95, 1751–1759. [Google Scholar] [CrossRef]
- Filbay, S.R.; Ackerman, I.N.; Russell, T.G.; Crossley, K.M. Return to sport matters-longer-term quality of life after ACL reconstruction in people with knee difficulties. Scand. J. Med. Sci. Sports 2017, 27, 514–524. [Google Scholar] [CrossRef] [PubMed]
- Toomey, C.M.; Whittaker, J.L.; Nettel-Aguirre, A.; Reimer, R.A.; Woodhouse, L.J.; Ghali, B.; Doyle-Baker, P.K.; Emery, C.A. Higher Fat Mass Is Associated with a History of Knee Injury in Youth Sport. J. Orthop. Sports Phys. Ther. 2017, 47, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Wyatt, R.W.; Inacio, M.C.; Liddle, K.D.; Maletis, G.B. Prevalence and Incidence of Cartilage Injuries and Meniscus Tears in Patients Who Underwent Both Primary and Revision Anterior Cruciate Ligament Reconstructions. Am. J. Sports Med. 2014, 42, 1841–1846. [Google Scholar] [CrossRef]
- Whittaker, J.L.; Woodhouse, L.J.; Nettel-Aguirre, A.; Emery, C.A. Outcomes associated with early post-traumatic osteoarthritis and other negative health consequences 3–10 years following knee joint injury in youth sport. Osteoarthr. Cartil. 2015, 23, 1122–1129. [Google Scholar] [CrossRef]
- Lohmander, L.S.; Ostenberg, A.; Englund, M.; Roos, H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004, 50, 3145–3152. [Google Scholar] [CrossRef]
- Swart, E.; Redler, L.; Fabricant, P.D.; Mandelbaum, B.R.; Ahmad, C.S.; Wang, Y.C. Prevention and Screening Programs for Anterior Cruciate Ligament Injuries in Young Athletes. J. Bone Jt. Surg. Am. 2014, 96, 705–711. [Google Scholar] [CrossRef]
- Boden, B.P.; Sheehan, F.T.; Torg, J.S.; Hewett, T.E. Noncontact anterior cruciate ligament injuries: Mechanisms and risk factors. J. Am. Acad. Orthop. Surg. 2010, 18, 520–527. [Google Scholar] [CrossRef]
- Agel, J.; Olson, D.E.; Dick, R.; Arendt, E.A.; Marshall, S.W.; Sikka, R.S. Descriptive epidemiology of collegiate women’s basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J. Athl. Train. 2007, 42, 202–210. [Google Scholar]
- Webster, K.E.; Hewett, T.E. Meta-analysis of meta-analyses of anterior cruciate ligament injury reduction training programs. J. Orthop. Res. 2018, 36, 2696–2708. [Google Scholar] [CrossRef] [PubMed]
- Gornitzky, A.L.; Lott, A.; Yellin, J.L.; Fabricant, P.D.; Lawrence, J.T.; Ganley, T.J. Sport-Specific Yearly Risk and Incidence of Anterior Cruciate Ligament Tears in High School Athletes: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2016, 44, 2716–2723. [Google Scholar] [CrossRef] [PubMed]
- Arendt, E.; Dick, R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am. J. Sports Med. 1995, 23, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Rauh, M.J.; Macera, C.A.; Ji, M.; Wiksten, D.L. Subsequent injury patterns in girls’ high school sports. J. Athl. Train. 2007, 42, 486–494. [Google Scholar]
- Alentorn-Geli, E.; Myer, G.D.; Silvers, H.J.; Samitier, G.; Romero, D.; Lázaro-Haro, C.; Cugat, R. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: Mechanisms of injury and underlying risk factors. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 705–729. [Google Scholar] [CrossRef]
- Renstrom, P.; Ljungqvist, A.; Arendt, E.; Beynnon, B.; Fukubayashi, T.; Garrett, W.; Georgoulis, T.; Hewett, T.E.; Johnson, H.; Krosshaug, T.; et al. Non-contact ACL injuries in female athletes: An International Olympic Committee current concepts statement. Br. J. Sports Med. 2008, 42, 394–412. [Google Scholar] [CrossRef]
- Sugimoto, D.; Myer, G.D.; McKeon, J.M.; Hewett, T.E. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: A critical review of relative risk reduction and numbers-needed-to-treat analyses. Br. J. Sports Med. 2012, 46, 979–988. [Google Scholar] [CrossRef]
- Myer, G.D.; Sugimoto, D.; Thomas, S.; Hewett, T.E. The Influence of Age on the Effectiveness of Neuromuscular Training to Reduce Anterior Cruciate Ligament Injury in Female Athletes: A Meta-Analysis. Am. J. Sports Med. 2013, 41, 203–215. [Google Scholar] [CrossRef]
- Hartling, L.; Chisholm, A.; Thomson, D.; Dryden, D.M. A descriptive analysis of overviews of reviews published between 2000 and 2011. PLoS ONE 2012, 7, e49667. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Boynton, J.; Glanville, J.; McDaid, D.; Lefebvre, C. Identifying systematic reviews in MEDLINE: Developing an objective approach to search strategy design. J. Inf. Sci. 1998, 24, 137–154. [Google Scholar] [CrossRef]
- Lee, E.; Dobbins, M.; DeCorby, K.; McRae, L.; Tirilis, D.; Husson, H. An optimal search filter for retrieving systematic reviews and meta-analyses. BMC Med. Res. Methodol. 2012, 12, 51. [Google Scholar] [CrossRef] [PubMed]
- Donnell-Fink, L.A.; Klara, K.; Collins, J.E.; Yang, H.Y.; Goczalk, M.G.; Katz, J.N.; Losina, E. Effectiveness of knee injury and anterior cruciate ligament tear prevention programs: A meta-analysis. PLoS ONE 2015, 10, e0144063. [Google Scholar] [CrossRef] [PubMed]
- Brunner, R.; Friesenbichler, B.; Casartelli, N.C.; Bizzini, M.; Maffiuletti, N.A.; Niedermann, K. Effectiveness of multicomponent lower extremity injury prevention programmes in team-sport athletes: An umbrella review. Br. J. Sports Med. 2019, 53, 282–288. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Olsen, O.E.; Myklebust, G.; Engebretsen, L.; Holme, I.; Bahr, R. Exercises to prevent lower limb injuries in youth sports: Cluster randomised controlled trial. BMJ 2005, 330, 449. [Google Scholar] [CrossRef]
- Steffen, K.; Myklebust, G.; Olsen, O.E.; Holme, I.; Bahr, R. Preventing injuries in female youth football—A cluster-randomized controlled trial. Scand. J. Med. Sci. Sports 2008, 18, 605–614. [Google Scholar] [CrossRef]
- Kiani, A.; Hellquist, E.; Ahlqvist, K.; Gedeborg, R.; Michaelsson, K.; Byberg, L. Prevention of Soccer-Related Knee Injuries in Teenaged Girls. Arch. Intern. Med. 2010, 170, 43–49. [Google Scholar] [CrossRef]
- Walden, M.; Atroshi, I.; Magnusson, H.; Wagner, P.; Hagglund, M. Prevention of acute knee injuries in adolescent female football players: Cluster randomised controlled trial. BMJ 2012, 344, e3042. [Google Scholar] [CrossRef]
- Achenbach, L.; Krutsch, V.; Weber, J.; Nerlich, M.; Luig, P.; Loose, O.; Angele, P.; Krutsch, W. Neuromuscular exercises prevent severe knee injury in adolescent team handball players. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1901–1908. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.B.; Waxman, J.P.; Richter, S.J.; Shultz, S.J. Evaluation of the effectiveness of anterior cruciate ligament injury prevention programme training components: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Ford, K.R.; Myer, G.D. Anterior Cruciate Ligament Injuries in Female Athletes Part 2, A Meta-analysis of Neuromuscular Interventions Aimed at Injury Prevention. Am. J. Sports Med. 2006, 34, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Alentorn-Geli, E.; Myer, G.D.; Silvers, H.J.; Samitier, G.; Romero, D.; Lázaro-Haro, C.; Cugat, R. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 2: A review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 859–879. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R. Reducing knee and anterior cruciate ligament injuries among female athletes: A systematic review of neuromuscular training interventions. J. Knee Surg. 2005, 18, 82–88. [Google Scholar] [CrossRef]
- Padua, D.A.; Marshall, S.W. Evidence Supporting ACL-Injury-Prevention Exercise Programs: A Review of the Literature. Int. J. Athl. Ther. Train. 2006, 11, 11–23. [Google Scholar] [CrossRef]
- Noyes, F.R.; Barber Westin, S.D. Anterior cruciate ligament injury prevention training in female athletes: A systematic review of injury reduction and results of athletic performance tests. Sports Health 2012, 4, 36–46. [Google Scholar] [CrossRef]
- Stojanovic, M.; Ostojic, S.M. Preventing ACL injuries in team-sport athletes: A systematic review of training interventions. Res. Sports Med. 2012, 20, 223–238. [Google Scholar] [CrossRef]
- Herman, K.; Barton, C.; Malliaras, P.; Morrissey, D. The effectiveness of neuromuscular warm-up strategies, that require no additional equipment, for preventing lower limb injuries during sports participation: A systematic review. BMC Med. 2012, 10, 75. [Google Scholar] [CrossRef]
- Noyes, F.R.; Barber-Westin, S.D. Neuromuscular retraining intervention programs: Do they reduce noncontact anterior cruciate ligament injury rates in adolescent female athletes? Arthroscopy 2014, 30, 245–255. [Google Scholar] [CrossRef]
- Michaelidis, M.; Koumantakis, G.A. Effects of knee injury primary prevention programs on anterior cruciate ligament injury rates in female athletes in different sports: A systematic review. Phys. Ther. Sport 2014, 15, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, J.H.; Beattie, C.S.; Schwartz, J.B.; Busconi, B.D. Assessing the Effectiveness of Neuromuscular Training Programs in Reducing the Incidence of Anterior Cruciate Ligament Injuries in Female Athletes: A Systematic Review. Am. J. Sports Med. 2015, 43, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.H.; Lim, B.O.; Ha, M.; Lee, S.W.; Oh, S.J.; Lee, Y.S.; Kim, J.G. A meta-analysis of the effect of neuromuscular training on the prevention of the anterior cruciate ligament injury in female athletes. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Grindstaff, T.L.; Hammill, R.R.; Tuzson, A.E.; Hertel, J. Neuromuscular control training programs and noncontact anterior cruciate ligament injury rates in female athletes: A numbers-needed-to-treat analysis. J. Athl. Train. 2006, 41, 450–456. [Google Scholar]
- Sadoghi, P.; von Keudell, A.; Vavken, P. Effectiveness of Anterior Cruciate Ligament Injury Prevention Training Programs. J. Bone Jt. Surg. Am. 2012, 94, 769–776. [Google Scholar] [CrossRef]
- Gagnier, J.J.; Morgenstern, H.; Chess, L. Interventions Designed to Prevent Anterior Cruciate Ligament Injuries in Adolescents and Adults: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2013, 41, 1952–1962. [Google Scholar] [CrossRef]
- LaBella, C.R.; Huxford, M.R.; Grissom, J.; Kim, K.Y.; Peng, J.; Christoffel, K.K. Effect of Neuromuscular Warm-up on Injuries in Female Soccer and Basketball Athletes in Urban Public High Schools: Cluster Randomized Controlled Trial. Arch. Pediatr. Adolesc. Med. 2011, 165, 1033–1040. [Google Scholar] [CrossRef]
- Yarsiasat, J.; Sumannont, S.; Manimmanakorn, N.; Srilamarth, S. Effectiveness of the Prevent Injury Enhance Performance (PEP) training program in reducing injury incidence rates among adolescent female SEPAK takraw players: A randomised controlled trial. J. Med. Assoc. Thai. 2019, 102, 98–105. [Google Scholar]
- Hewett, T.E.; Lindenfeld, T.N.; Riccobene, J.V.; Noyes, F.R. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am. J. Sports Med. 1999, 27, 699–706. [Google Scholar] [CrossRef]
- Mandelbaum, B.R.; Silvers, H.J.; Watanabe, D.S.; Knarr, J.F.; Thomas, S.D.; Griffin, L.Y.; Kirkendall, D.T.; Garrett, W., Jr. Effectiveness of a Neuromuscular and Proprioceptive Training Program in Preventing Anterior Cruciate Ligament Injuries in Female Athletes 2-Year Follow-up. Am. J. Sports Med. 2005, 33, 1003–1010. [Google Scholar] [CrossRef]
- Pfeiffer, R.P.; Shea, K.G.; Roberts, D.; Grandstrand, S.; Bond, L. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J. Bone Jt. Surg. Am. 2006, 88, 1769–1774. [Google Scholar] [CrossRef] [PubMed]
- Griffin, L.Y.; Agel, J.; Albohm, M.J.; Arendt, E.A.; Dick, R.W.; Garrett, W.E.; Garrick, J.G.; Hewett, T.E.; Huston, L.; Ireland, M.L.; et al. Noncontact anterior cruciate ligament injuries: Risk factors and prevention strategies. J. Am. Acad. Orthop. Surg. 2000, 8, 141–150. [Google Scholar] [CrossRef]
- Padua, D.A.; DiStefano, L.J.; Hewett, T.E.; Garrett, W.E.; Marshall, S.W.; Golden, G.M.; Shultz, S.J.; Sigward, S.M. National Athletic Trainers’ Association Position Statement: Prevention of Anterior Cruciate Ligament Injury. J. Athl. Train. 2018, 53, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, D.; Myer, G.D.; Bush, H.M.; Klugman, M.F.; Medina McKeon, J.M.; Hewett, T.E. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: A meta-analysis. J. Athl. Train. 2012, 47, 714–723. [Google Scholar] [CrossRef]
- Sugimoto, D.; Myer, G.D.; Foss, K.D.; Hewett, T.E. Dosage effects of neuromuscular training intervention to reduce anterior cruciate ligament injuries in female athletes: Meta- and sub-group analyses. Sports Med. 2014, 44, 551–562. [Google Scholar] [CrossRef] [PubMed]
- Chiaro, M. Extrinsic Versus Intrinsic Feedback for Movement Coordination in 15-Year-Old ACL Female Athletes. Ph.D. Thesis, Azusa Pacific University, Azusa, CA, USA, 2016. [Google Scholar]
- Albaugh, J.; Friedman, J.; Cody, S.; Ganley, T. Joint Efforts. Train. Cond. 2010, 20, 42–49. [Google Scholar]
- Protecting athletic girl’s knees. J. Gend. Specif. Med. 2001, 4, 5.
- Halvorson, R. Neuromuscular Warm-Ups Reduce Knee Injuries. IDEA Fit. J. 2012, 9, 16. [Google Scholar]
- May, J.H.; Dahm, D.L. Anterior cruciate ligament injury in the skeletally immature patient. Minerva Ortop. Traumatol. 2010, 61, 415–423. [Google Scholar]
- Della Villa, S.; Bizzini, M.; Junge, A.; Dvorak, J. Injury prevention initiative—FIFA 11+. In Proceedings of the 9th World Congress of the International Cartilage Repair Society, Barcelona, Spain, 26–29 September 2010. [Google Scholar]
- Herman, K.; Barton, C.; Malliaras, D.; Morrissey, D. The effectiveness of functional neuromuscular warm-up strategies for preventing lower limb Injuries during sports participation: A systematic review. Muscles Ligaments Tendons J. 2012, 26–27. [Google Scholar]
- Dompier, T. Free Communications, Oral Presentations: Injury Epidemiology. J. Athl. Train. 2006, 41, S54–S56. [Google Scholar]
- Hespanhol Junior, L.C.; Kamper, S.J. Prevention of non-contact anterior cruciate ligament injuries: PEDro synthesis. Br. J. Sports Med. 2015, 49, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Evidence-Based best-practice guidelines for preventing anterior cruciate ligament injuries in young female athletes. Co-Kinet. J. 2018, 6.
- Meyer, S.E.; Yamato, T.P.; Saragiotto, B.T. Knee injury and ACL tear prevention programmes (PEDro synthesis). Br. J. Sports Med. 2017, 51, 1161–1162. [Google Scholar] [CrossRef] [PubMed]
- Elliot, D.L.; Goldberg, L.; Kuehl, K.S. Young Women’s Anterior Cruciate Ligament Injuries. Sports Med. 2010, 40, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Paterno, M.V.; Quatman, C.E. The 2012 ABJS Nicolas Andry Award: The sequence of prevention: A systematic approach to prevent anterior cruciate ligament injury. Clin. Orthop. Relat. Res. 2012, 470, 2930–2940. [Google Scholar] [CrossRef] [PubMed]
- Silvers, H.J.; Mandelbaum, B.R. Prevention of anterior cruciate ligament injury in the female athlete. Br. J. Sports Med. 2007, 41, i52–i59. [Google Scholar] [CrossRef]
- Rishiraj, N.; Taunton, J.E.; Lloyd-Smith, R.; Woollard, R.; Regan, W.; Clement, D.B. The potential role of prophylactic/functional knee bracing in preventing knee ligament injury. Sports Med. 2009, 39, 937–960. [Google Scholar] [CrossRef]
- Gokeler, A.; Benjaminse, A.; Seil, R.; Kerkhoffs, G.; Verhagen, E. Using principles of motor learning to enhance ACL injury prevention programs. Sports Orthop. Traumatol. 2018, 34, 23–30. [Google Scholar] [CrossRef]
- Hewett, T.E.; Ford, K.R.; Hoogenboom, B.J.; Myer, G.D. Understanding and preventing acl injuries: Current biomechanical and epidemiologic considerations-update 2010. N. Am. J. Sports Phys. Ther. 2010, 5, 234–251. [Google Scholar]
- Myer, G.D.; Chu, D.A.; Brent, J.L.; Hewett, T.E. Trunk and Hip Control Neuromuscular Training for the Prevention of Knee Joint Injury. Clin. Sports Med. 2008, 27, 425–448. [Google Scholar] [CrossRef] [PubMed]
- Laible, C.; Sherman, O.H. Risk factors and prevention strategies of non-contact anterior cruciate ligament injuries. Bull. Hosp. Jt. Dis. 2014, 72, 70–75. [Google Scholar]
- Myer, G.D.; Brent, J.L.; Ford, K.R.; Hewett, T.E. Real-Time Assessment and Neuromuscular Training Feedback Techniques to Prevent Anterior Cruciate Ligament Injury in Female Athletes. Strength Cond. J. 2011, 33, 21–35. [Google Scholar] [CrossRef]
- Dai, B.; Herman, D.; Liu, H.; Garrett, W.E.; Yu, B. Prevention of ACL Injury, Part II: Effects of ACL Injury Prevention Programs on Neuromuscular Risk Factors and Injury Rate. Res. Sports Med. 2012, 20, 198–222. [Google Scholar] [CrossRef] [PubMed]
- Zakieh, O.; Park, C.; Hornby, K.; Gupte, C.; Sarraf, K.M. Paediatric anterior cruciate ligament injury. Br. J. Hosp. Med. 2021, 82, 1–9. [Google Scholar] [CrossRef]
- Paulson, W.; Slattengren, A.H. Effectiveness of ACL Injury Prevention Programs. Am. Fam. Physician 2018, 97, 192A. [Google Scholar]
- LaBella, C.R.; Hennrikus, W.; Hewett, T.E. Anterior Cruciate Ligament Injuries: Diagnosis, Treatment, and Prevention. Pediatrics 2014, 133, e1437–e1450. [Google Scholar] [CrossRef]
- Arabia, J.J.M.; Arabia, W.H.M. Anterior cruciate ligament injuries. Iatreia 2009, 22, 256–271. [Google Scholar]
- Myer, G.D.; Ford, K.R.; Brent, J.L.; Hewett, T.E. An integrated approach to change the outcome part II: Targeted neuromuscular training techniques to reduce identified ACL injury risk factors. J. Strength Cond. Res. 2012, 26, 2272–2292. [Google Scholar] [CrossRef]
- Bonnette, S.; DiCesare, C.A.; Diekfuss, J.A.; Grooms, D.R.; MacPherson, R.P.; Riley, M.A.; Myer, G.D. Advancing Anterior Cruciate Ligament Injury Prevention Using Real-Time Biofeedback for Amplified Sensorimotor Integration. J. Athl. Train. 2019, 54, 985–986. [Google Scholar] [CrossRef]
- Nessler, T.; Denney, L.; Sampley, J. ACL Injury Prevention: What Does Research Tell Us? Curr. Rev. Musculoskelet. Med. 2017, 10, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Kiefer, A.W.; Kushner, A.M.; Groene, J.; Williams, C.; Riley, M.A.; Myer, G.D. A Commentary on Real-Time Biofeedback to Augment Neuromuscular Training for ACL Injury Prevention in Adolescent Athletes. J. Sports Sci. Med. 2015, 14, 1–8. [Google Scholar]
- Myer, G.D.; Ford, K.R.; Hewettt, T.E. Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J. Athl. Train. 2004, 39, 352–364. [Google Scholar] [PubMed]
- Dharamsi, A.; LaBella, C.R. Prevention of ACL injuries in adolescent female athletes. Contemp. Pediatr. 2013, 30, 12–20. [Google Scholar]
- LaBella, C.R.; Carl, R. Preventing knee ligament injuries in young athletes. Pediatr. Ann. 2010, 39, 714–720. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; Hewett, T.E. Preventing ACL injuries in women: Testing for neuromuscular deficits helps physicians determine interventions. J. Musculoskelet. Med. 2006, 23, 12–27. [Google Scholar]
- Bencke, J.; Aagaard, P.; Zebis, M.K. Muscle Activation during ACL Injury Risk Movements in Young Female Athletes: A Narrative Review. Front. Physiol. 2018, 9, 445. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; Hewett, T.E. Methodological approaches and rationale for training to prevent anterior cruciate ligament injuries in female athletes. Scand. J. Med. Sci. Sports 2004, 14, 275–285. [Google Scholar] [CrossRef]
- Mehl, J.; Diermeier, T.; Herbst, E.; Imhoff, A.B.; Stoffels, T.; Zantop, T.; Petersen, W.; Achtnich, A. Evidence-Based concepts for prevention of knee and ACL injuries. 2017 guidelines of the ligament committee of the German Knee Society (DKG). Arch. Orthop. Trauma Surg. 2018, 138, 51–61. [Google Scholar] [CrossRef]
- Ladenhauf, H.N.; Graziano, J.; Marx, R.G. Anterior cruciate ligament prevention strategies: Are they effective in young athletes—Current concepts and review of literature. Curr. Opin. Pediatr. 2013, 25, 64–71. [Google Scholar] [CrossRef]
- Graziano, J.; Green, D.W.; Cordasco, F.A. Anterior Cruciate Ligament Injury Prevention the Young Athlete: Evidence-Based Application. Strength Cond. J. 2013, 35, 89–97. [Google Scholar] [CrossRef]
- Kelly, A.K.W. Anterior Cruciate Ligament Injury Prevention. Curr. Sports Med. Rep. 2008, 7, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Acevedo, R.J.; Rivera-Vega, A.; Miranda, G.; Micheo, W. Anterior cruciate ligament injury: Identification of risk factors and prevention strategies. Curr. Sports Med. Rep. 2014, 13, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Brophy, R.H.; Silvers, H.J.; Mandelbaum, B.R. Anterior cruciate ligament injuries: Etiology and prevention. Sports Med. Arthrosc. Rev. 2010, 18, 2–11. [Google Scholar] [CrossRef]
- Bisciotti, G.N.; Chamari, K.; Cena, E.; Carimati, G.; Volpi, P. ACL injury in football: A literature overview of the prevention programs. Muscles Ligaments Tendons J. 2016, 6, 473–479. [Google Scholar] [CrossRef]
- Taylor, J.B.; Ford, K.R.; Nguyen, A.D.; Terry, L.N.; Hegedus, E.J. Prevention of lower extremity injuries in basketball: A systematic review and meta-analysis. Sports Health 2015, 7, 392–398. [Google Scholar] [CrossRef]
- Chang, W.D.; Lai, P.T. Neuromuscular training for prevention of anterior cruciate ligament injury in female athletes. Int. J. Athl. Ther. Train. 2014, 19, 17–21. [Google Scholar] [CrossRef][Green Version]
- Assaly, S.G.; Davenport, T.E.; Mattern-Baxter, K. Effectiveness of neuromuscular conditioning to prevent anterior cruciate ligament injuries in female athletes: A critical synthesis of literature. Orthop. Phys. Ther. Pract. 2011, 23, 140–146. [Google Scholar]
- Sugimoto, D.; Myer, G.D.; Foss, K.D.; Hewett, T.E. Specific exercise effects of preventive neuromuscular training intervention on anterior cruciate ligament injury risk reduction in young females: Meta-analysis and subgroup analysis. Br. J. Sports Med. 2015, 49, 282–289. [Google Scholar] [CrossRef]
- Ramirez, R.N.; Baldwin, K.; Franklin, C.C.D. Prevention of Anterior Cruciate Ligament Rupture in Female Athletes: A Systematic Review. JBJS Rev. 2014, 2, e3. [Google Scholar] [CrossRef]
- Crossley, K.M.; Patterson, B.E.; Culvenor, A.G.; Bruder, A.M.; Mosler, A.B.; Mentiplay, B.F. Making football safer for women: A systematic review and meta-analysis of injury prevention programmes in 11,773 female football (soccer) players. Br. J. Sports Med. 2020, 54, 1089–1098. [Google Scholar] [CrossRef] [PubMed]
- Petushek, E.J.; Sugimoto, D.; Stoolmiller, M.; Smith, G.; Myer, G.D. Evidence-Based Best-Practice Guidelines for Preventing Anterior Cruciate Ligament Injuries in Young Female Athletes: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2019, 47, 1744–1753. [Google Scholar] [CrossRef] [PubMed]
- Grimm, N.L.; Jacobs, J.C.; Kim, J.; Denney, B.S.; Shea, K.G. Anterior Cruciate Ligament and Knee Injury Prevention Programs for Soccer Players: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2015, 43, 2049–2056. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.L.; Jung, J.; Mulligan, C.M.S.; Oh, J.; Norcross, M.F. A majority of anterior cruciate ligament injuries can be prevented by injury prevention programs: A systematic review of randomized controlled trials and cluster-randomized controlled trials with meta-analysis. Am. J. Sports Med. 2020, 48, 1505–1515. [Google Scholar] [CrossRef]
- Zheng, R.; Zhou, J. Biomechanical risk factors and prevention of non-contact anterior cruciate ligament injury. Chin. J. Tissue Eng. Res. 2014, 18, 3919–3924. [Google Scholar]
- Romero-Moraleda, B.; Cuellar, A.; Gonzalez, J.; Bastida, N.; Echarri, E.; Gallardo, J.; Paredes, V. Review risk factors and prevention programs of the anterior cruciate ligament injury in female football: Prevention proposal. Rev. Int. Cienc. Deporte 2017, 13, 117–138. [Google Scholar] [CrossRef]
- Herzberg, S.D.; Motu’apuaka, M.L.; Lambert, W.; Fu, R.; Brady, J.; Guise, J.M. The Effect of Menstrual Cycle and Contraceptives on ACL Injuries and Laxity: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2017, 5, 2325967117718781. [Google Scholar] [CrossRef]
- Willadsen, E.M.; Zahn, A.B.; Durall, C.J. What Is the Most Effective Training Approach for Preventing Noncontact ACL Injuries in High School–Aged Female Athletes? J. Sport Rehabil. 2019, 28, 94–98. [Google Scholar] [CrossRef]
- Weber, M.L.; Lam, K.C.; Valovich McLeod, T.C. The Effectiveness of Injury Prevention Programs for Youth and Adolescent Athletes. Int. J. Athl. Ther. Train. 2016, 21, 25–31. [Google Scholar] [CrossRef]
- Trojian, T.; Driban, J.; Nuti, R.; Distefano, L.; Root, H.; Nistler, C.; LaBella, C.R. Osteoarthritis action alliance consensus opinion—Best practice features of anterior cruciate ligament and lower limb injury prevention programs. World J. Orthop. 2017, 8, 726–734. [Google Scholar] [CrossRef]
- Emery, C.A.; Roy, T.O.; Whittaker, J.L.; Nettel-Aguirre, A.; van Mechelen, W. Neuromuscular training injury prevention strategies in youth sport: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 865–870. [Google Scholar] [CrossRef] [PubMed]
- Lim, B.O.; Lee, Y.S.; Kim, J.G.; An, K.O.; Yoo, J.; Kwon, Y.H. Effects of sports injury prevention training on the biomechanical risk factors of anterior cruciate ligament injury in high school female basketball players. Am. J. Sports Med. 2009, 37, 1728–1734. [Google Scholar] [CrossRef] [PubMed]
- Ter Stege, M.H.; Dallinga, J.M.; Benjaminse, A.; Lemmink, K.A. Effect of interventions on potential, modifiable risk factors for knee injury in team ball sports: A systematic review. Sports Med. 2014, 44, 1403–1426. [Google Scholar] [CrossRef] [PubMed]
- Barber-Westin, S.D.; Noyes, F.R. Effect of Fatigue Protocols on Lower Limb Neuromuscular Function and Implications for Anterior Cruciate Ligament Injury Prevention Training: A Systematic Review. Am. J. Sports Med. 2017, 45, 3388–3396. [Google Scholar] [CrossRef]
- Monajati, A.; Larumbe-Zabala, E.; Goss-Sampson, M.; Naclerio, F. The effectiveness of injury prevention programs to modify risk factors for non-contact anterior cruciate ligament and hamstring injuries in uninjured team sports athletes: A systematic review. PLoS ONE 2016, 11, e0155272. [Google Scholar] [CrossRef]
- Paszkewicz, J.; Webb, T.; Waters, B.; McCarty, C.W.; Van Lunen, B. The Effectiveness of Injury-Prevention Programs in Reducing the Incidence of Anterior Cruciate Ligament Sprains in Adolescent Athletes. J. Sport Rehabil. 2012, 21, 371–377. [Google Scholar] [CrossRef]
- Prather, B.S. The Effect of Improved Strength and Conditioning on Resisting Fatigue and Preventing Anterior Cruciate Ligament Tears in Young Athletes. Master’s Thesis, Weill Medical College of Cornell University, New York, NY, USA, 2015. [Google Scholar]
- Barber-Westin, S.D.; Noyes, F.R.; Smith, S.T.; Campbell, T.M. Reducing the risk of noncontact anterior cruciate ligament injuries in the female athlete. Phys. Sportsmed. 2009, 37, 49–61. [Google Scholar] [CrossRef]
- Universal Neuromuscular Training Reduces ACL Injury Risk in Young Athletes. School Nurse News 2014, 31, 8.
- Bottino, N. Uncharted Waters. Train. Cond. 2014, 24, 41–45. [Google Scholar]
- Moksnes, H.; Grindem, H. Prevention and rehabilitation of paediatric anterior cruciate ligament injuries. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 730–736. [Google Scholar] [CrossRef]
- Hornbeck, K.; Peterson, A. Neuromuscular training program reduces knee injuries among adolescent female soccer players. J. Pediatr. 2012, 161, 970–971. [Google Scholar] [CrossRef] [PubMed]
- Halvorson, R. Neuromuscular Training and ACL Injury. IDEA Fit. J. 2014, 11, 11. [Google Scholar]
- Powers, C.M.; Fisher, B. Mechanisms underlying ACL injury-prevention training: The brain-behavior relationship. J. Athl. Train. 2010, 45, 513–515. [Google Scholar] [CrossRef]
- Howe, D.K. Inury Prevention. Am. Fit. 2006, 24, 19. [Google Scholar]
- Garcia, A. Designing an ACL Injury Prevention Program. Rehab Manag. Interdiscip. J. Rehabil. 2011, 24, 24–26. [Google Scholar]
- Nagano, Y.; Suzukawa, M.; Tamaki, T.; Mochida, T.; Yoshihisa, T.; Yano, S.; Fukubayashi, T.; Nakajima, H. A report on the incidence of injuries for junior high school basketball teams in Yokohama: Introduction of an injury prevention programme. Br. J. Sports Med. 2008, 42, 535. [Google Scholar]
- Queen, R. Adolescents and ACL Injuries: Current Research and Future Challenges. ACSM Fit. Soc. Page 2015, 17, 4. [Google Scholar]
- Lewis, D.A.; Kirkbride, B.; Vertullo, C.J.; Gordon, L.; Comans, T.A. Comparison of four alternative national universal anterior cruciate ligament injury prevention programme implementation strategies to reduce secondary future medical costs. Br. J. Sports Med. 2018, 52, 277–282. [Google Scholar] [CrossRef]
- Jari, E.D.; Salih, H.A.J.; Jawad, A.H. The effect of both (Ballistic and plyometric) methods of exercises in protecting from knee joint injury in terms of the most important muscles working on it for the handball center player. Indian J. Forensic Med. Toxicol. 2020, 14, 2649–2655. [Google Scholar]
- Sibbala, N.; Vamshi, R. Effectiveness of five phase balance training program on the risk of knee injuries in adolescent athletes. Rom. J. Phys. Ther. 2017, 23, 24–32. [Google Scholar]
- Owoeye, O.B.A.; Befus, K.; Raisenen, A.; Palacios-Derflingher, L.; Emery, C.A.; Pasanen, K. Is neuromuscular training effective in reducing specific lower extremity injuries in youth basketball? Clin. J. Sport Med. 2020, 30, e94–e95. [Google Scholar]
- Richmond, S.A.; Kang, J.; Doyle-Baker, P.K.; Nettel-Aguirre, A.; Emery, C.A. A School-Based Injury Prevention Program to Reduce Sport Injury Risk and Improve Healthy Outcomes in Youth: A Pilot Cluster-Randomized Controlled Trial. Clin. J. Sport Med. 2016, 26, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Potera, C. Pediatric ACL Injuries. Am. J. Nurs. 2014, 114, 18. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.J.; Renier, C.M.; Ahern, J.J.; Elliott, B.A. Neuromuscular training availability and efficacy in preventing anterior cruciate ligament injury in high school sports: A retrospective cohort study. Clin. J. Sport Med. 2017, 27, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Decker, M.J.; Shaw, M.; Maddan, C.; Campbell, J.; Davidson, B. A wearable neuromuscular device reduces ACL injury risk in female soccer athletes. Orthop. J. Sports Med. 2016, 4. [Google Scholar] [CrossRef]
- Foss, K.D.; Thomas, S.; Khoury, J.C.; Myer, G.D.; Hewett, T.E. A School-Based Neuromuscular Training Program and Sport-Related Injury Incidence: A Prospective Randomized Controlled Clinical Trial. J. Athl. Train. 2018, 53, 20–28. [Google Scholar] [CrossRef]
- Omi, Y.; Sugimoto, D.; Kuriyama, S.; Kurihara, T.; Miyamoto, K.; Yun, S.; Kawashima, T.; Hirose, N. Effect of Hip-Focused Injury Prevention Training for Anterior Cruciate Ligament Injury Reduction in Female Basketball Players: A 12-Year Prospective Intervention Study. Am. J. Sports Med. 2018, 46, 852–861. [Google Scholar] [CrossRef]
| Study ID | Databases Searched | Date of Last Search | Total Number of Studies * (Non-Contact) | Total Number of Participants * (Non-Contact) | Study Funding |
|---|---|---|---|---|---|
| Hewett et al. [35] | Medline, CINAHL | NR | 5 (3) | 8764 (8324) | NIH |
| Padua et al. [36] | PubMed | NR | 5 (2) | 8850 (6532) | NR |
| Noyes et al. [37] | PubMed, CINAHL, Science Direct | August 2011 | 6 (4) | 13,067 (8400) | NR |
| Stojanovic et al. [38] | Medline | June 2011 | 9 (5) | 13,884 † (NR) | NR |
| Herman et al. [39] | PubMed, Embase, SPORTDiscus, PEDro, Google Scholar, ISI Web of Knowledge, Scirus | January 2012 | 6 (3) | 8999 (4034) | NR |
| Noyes et al. [40] | Medline, CCRCT | May 2013 | 9 # (9) | 19,493 | NR |
| Michaelidis et al. [41] | PubMed, CINAHL, CCRCT, Science Direct, SPORTDiscus, PEDro, SCOPUS | September 2012 | 13 (11) | 22,052 (21,612) | None |
| Stevenson et al. [42] | Medline, CINAHL, CCRCT | 2011 | 10 (5) | 15,512 (5771) | NR |
| Study ID | Databases Searched | Date of Last Search | Total Number of Primary Studies * (Non-Contact) | Total Number of Participants (Non-Contact) | Meta-Analysis Results † | Reduction in Non-Contact ACL Risk | Study Funding Sources |
|---|---|---|---|---|---|---|---|
| Hewett et al. [33] | Medline, CINAHL | 2004 | 6 (3) | 9040 (8324) | Not conducted | - | NIH |
| Grindstaff et al. [44] | PubMed, Medline, CINAHL, SPORTDiscus, Web of Science | October 2005 | 5 (5) | 11,026 | Not conducted | - | NR |
| Yoo et al. [43] * | Medline, CCRCT | June 2007 | 7 (4) | 10,618 (8247) | OR = 0.36 (0.23–0.54) | 64% | NR |
| Sadoghi et al. [45] | PubMed, Medline, CINAHL, CCRCT, Embase | December 2010 | 8 (6) | 10,618 (9982) | RR = 0.48 (0.26–0.89) | 62% | None |
| Sugimoto et al. [17] | PubMed, Medline, CINAHL, SPORTDiscus | January 2012 | 12 (10) | 18,523 (18,083) | RRR = 73.4% (63–81) | 73.4% | NIH |
| NNT = 108 (86–150) | |||||||
| Gagnier et al. [46] ^ | Medline, CINAHL, CCRCT, Embase, SPORTDiscus, HTA | July 2011 | 14 (NR) | ~27,136 (NR) | Not conducted | - | U of M Bone & Joint Injury Prevention & Rehabilitation Center |
| Taylor et al. [32] | PubMed, Medline, CINAHL, CCRCT, SPORTDiscus | July 2012 | 13 (9) | 24,188 (19,891) | OR = 0.38 (0.22–0.64) | 62% | None |
| Donnell-Fink et al. [23] * | PubMed, Medline, CINAHL, CCRCT, Embase, Web of Science | December 2014 | 14 (9) | 20,132 (15,235) # | IRR = 0.51 (0.30–0.88) | 48.7% | NIH, NIAMSD |
| Systematic Review and/or Meta-Analysis | Primary Study | |||||||
|---|---|---|---|---|---|---|---|---|
| Hewett et al. [49] | Mandelbaum et al. [50] | Olsen et al. [27] | Pfeiffer et al. [51] | Steffen et al. [28] | Kiani et al. [29] | LaBella et al. [47] | Walden et al. [30] | |
| Hewett et al. [35] * | X | X | ||||||
| Padua et al. [36] * | X | X | X | |||||
| Hewett et al. [33] | X | X | ||||||
| Grindstaff et al. [44] | X | X | X | |||||
| Yoo et al. [43] # | X | X | X | |||||
| Noyes et al. [37] * | X | X | X | X | ||||
| Sadoghi et al. [45] | X | X | X | |||||
| Stojanovic et al. [38] * | X | X | X | |||||
| Herman et al. [39] * | X | X | X | X | X | |||
| Sugimoto et al. [17] | X | X | X | X | X | X | X | |
| Noyes et al. [40] * | X | X | X | X | X | X | X | X |
| Michaelidis et al. [41] * | X | X | X | X | X | X | X | |
| Taylor et al. [32] | X | X | X | X | X | X | X | X |
| Stevenson et al. [42] * | X | X | X | X | X | |||
| Donnell-Fink et al. [23] # | X | X | X | X | X | X | X | X |
| Study ID | Study Design | Number of Participants | Age (Years) | Sports | Number of Injuries | ACL Injury Incidence * |
|---|---|---|---|---|---|---|
| Hewett et al. [49] | Prospective cohort study | C: 463 | 14–18 | Soccer, basketball, volleyball | C: 5 | 0.22 |
| I: 366 | I: 0 | 0.00 | ||||
| Mandelbaum et al. [50] | Prospective cohort study | C: 3818 | 14–18 | Soccer | C: 67 | 0.49 |
| I: 1885 | I: 6 | 0.09 | ||||
| Olsen et al. [27] | Randomized controlled trial | C: 778 | 15–17 | Handball | C: 5 | 0.11 |
| I: 808 | I: 1 | 0.02 | ||||
| Pfeiffer et al. [51] | Prospective cohort study | C: 862 | 14–18 | Soccer, basketball, volleyball | C: 3 | 0.08 |
| I: 577 | I: 3 | 0.17 | ||||
| Steffen et al. [28] | Randomized controlled trial | C: 947 | 13–17 | Soccer | C: 2 | 0.06 |
| I: 1073 | I: 3 | 0.09 | ||||
| Kiani et al. [29] | Prospective cohort study | C: 729 | 13–19 | Soccer | C: 5 | 0.15 |
| I: 777 | I: 0 | 0.00 | ||||
| LaBella et al. [47] | Randomized controlled trial | C: 755 | 16.2 ± 1.1 | Soccer, basketball | C: 6 | 0.48 |
| I: 737 | 16.2 ± 1.5 | I: 2 | 0.10 | |||
| Walden et al. [30] | Randomized controlled trial | C: 2085 | 12–17 | Soccer | C: 8 | 0.12 |
| I: 2479 | I: 5 | 0.07 | ||||
| Achenbach et al. [31] | Randomized controlled trial | C: 215 | 15.1 ± 1.0 | Handball | C: 2 | 0.32 |
| I: 259 | 14.9 ± 0.9 | I: 0 | 0.00 | |||
| Yarsiasat et al. [48] | Randomized controlled trial | C: 26 | 14–19 | Sepak takraw | C: 3 | 0.05 |
| I: 26 | I: 1 | 0.02 |
| Study ID | Program Name | Exercise Types Included | Feedback | Duration (min.) | Frequency (d/wk.) | Length of Program | Training Season | Equipment | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Warm-Up | Plyometrics | Strength | Agility | Balance | Stretching | ||||||||
| Hewett et al. [49] | Sportsmetrics | X * | X | X | 60–90 | 3 | 6 weeks | PS | Gymnastic mat, cones | ||||
| Mandelbaum et al. [50] | PEP | X | X * | X | X | X | 20 | 2–3 | 12 weeks for 3 seasons | S | Cones | ||
| Olsen et al. [27] | OLSEN | X | X * | X | X | X | X | 15–20 | 15 sessions then 1 | 8 months | S | Wobble board, balance mat | |
| Pfeiffer et al. [51] | KLIPP | X | X * | 20 | 2 | 2 seasons | S | None | |||||
| Steffen et al. [28] | The “11” | X | X | X | X | X | X | 20 | 15 sessions then 1 | 8 months | PS, S | Balance mat | |
| Kiani et al. [29] | HPT | X | X * | X | X | 20–25 | 2 (PS), 1 (S) | 9 months | PS, S | None | |||
| LaBella et al. [47] | KIPP | X | X | X | X | X | X | 20 | 2–5 # | 13 ± 2.5 weeks | S | None | |
| Walden et al. [30] | Walden | X | X | X | X | 15 | 2 | 7 months | S | None | |||
| Achenbach et al. [31] | HSIPP | X | X | X | 15 | 2–3 (PS), 1 (S) | 10–12 weeks + season | PS, S | None | ||||
| Yarsiasat et al. [48] | PEP | X | X | X | X | X | 20 | 3 | 8 weeks | Unsure | Cones | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mattu, A.T.; Ghali, B.; Linton, V.; Zheng, A.; Pike, I. Prevention of Non-Contact Anterior Cruciate Ligament Injuries among Youth Female Athletes: An Umbrella Review. Int. J. Environ. Res. Public Health 2022, 19, 4648. https://doi.org/10.3390/ijerph19084648
Mattu AT, Ghali B, Linton V, Zheng A, Pike I. Prevention of Non-Contact Anterior Cruciate Ligament Injuries among Youth Female Athletes: An Umbrella Review. International Journal of Environmental Research and Public Health. 2022; 19(8):4648. https://doi.org/10.3390/ijerph19084648
Chicago/Turabian StyleMattu, Anmol T., Brianna Ghali, Vanessa Linton, Alex Zheng, and Ian Pike. 2022. "Prevention of Non-Contact Anterior Cruciate Ligament Injuries among Youth Female Athletes: An Umbrella Review" International Journal of Environmental Research and Public Health 19, no. 8: 4648. https://doi.org/10.3390/ijerph19084648
APA StyleMattu, A. T., Ghali, B., Linton, V., Zheng, A., & Pike, I. (2022). Prevention of Non-Contact Anterior Cruciate Ligament Injuries among Youth Female Athletes: An Umbrella Review. International Journal of Environmental Research and Public Health, 19(8), 4648. https://doi.org/10.3390/ijerph19084648






