Psychometrics of the Pearlin Mastery Scale among Family Caregivers of Older Adults Who Require Assistance in Activities of Daily Living
Abstract
:1. Introduction
2. Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Mastery
2.2.2. Caregiver Burden
2.2.3. Depression
2.2.4. Health-Related Quality of Life
2.2.5. Demographics Characteristics
2.3. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Confirmatory Factor Analysis Statistics
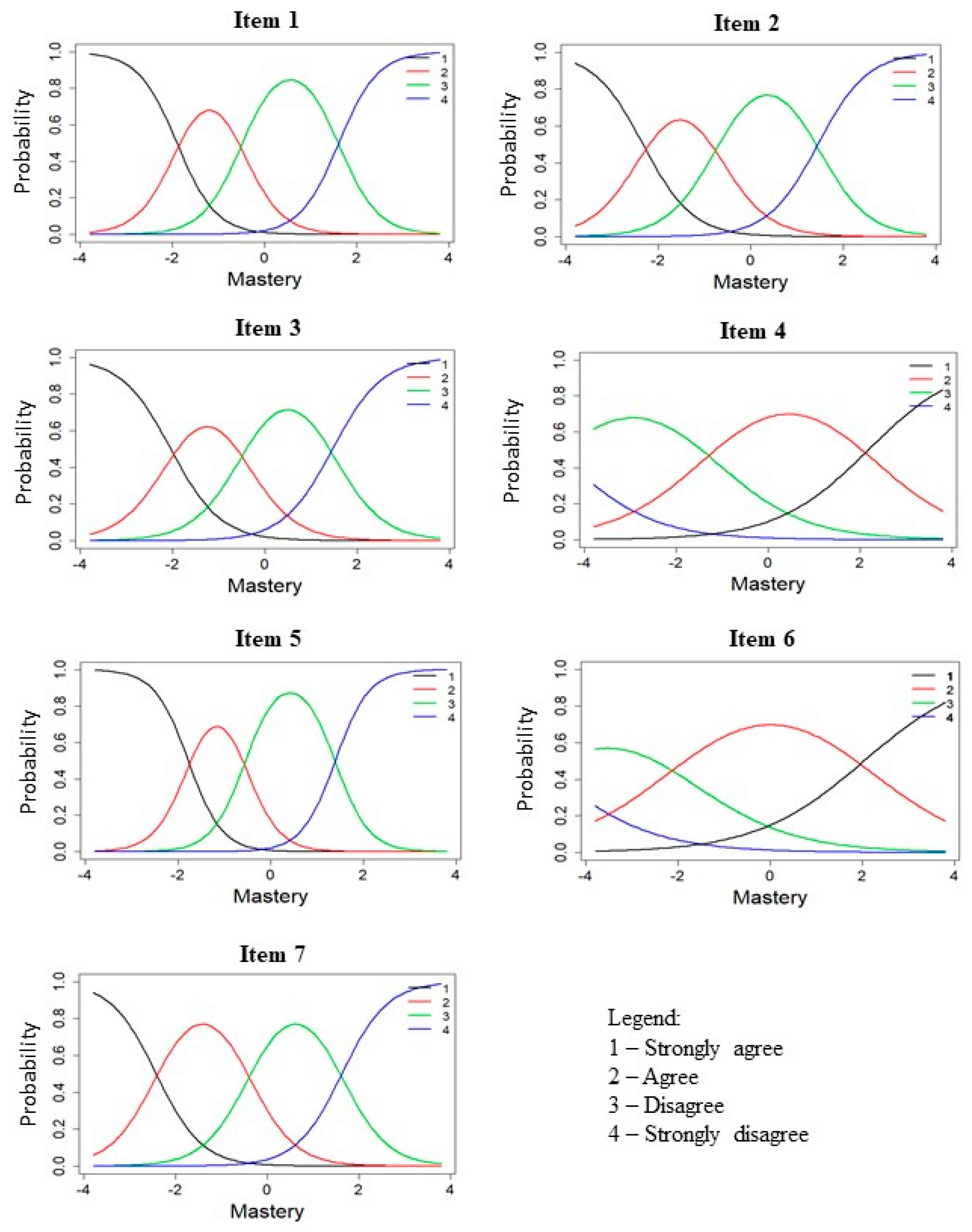
3.3. IRT Parameters and Information
3.4. Validity and Reliability of Mastery Scale
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Item | Statement |
|---|---|
| 1 | There is really no way I can solve some of the problems that I have. |
| 2 | Sometimes I feel like I am being pushed around in life. |
| 3 | I have little control over the things that happen to me. |
| 4 | I can do just about anything I really set my mind to do. * |
| 5 | I often feel helpless in dealing with the problems of life. |
| 6 | What happens to me in the future mostly depends on me. * |
| 7 | There is little I can do to change many of the important things in my life. |
References
- Pearlin, L.I.; Schooler, C. The Structure of Coping. J. Health Soc. Behav. 1978, 19, 2–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pearlin, L.I.; Mullan, J.T.; Semple, S.J.; Skaff, M.M. Caregiving and the Stress Process: An Overview of Concepts and Their Measures. Gerontologist 1990, 30, 583–594. [Google Scholar] [CrossRef] [PubMed]
- Pearlin, L.I.; Menaghan, E.G.; Lieberman, M.A.; Mullan, J.T. The Stress Process. J. Health Soc. Behav. 1981, 22, 337–356. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.; Glass, G.; Chua, K.-C.; Ali, N.; Lim, W.S. Relationship between Mastery and Caregiving Competence in Protecting against Burden, Anxiety and Depression among Caregivers of Frail Older Adults. J. Nutr. Health Aging 2018, 22, 1238–1245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sim, Y.W. Exploring the Relationship between Mastery and Health Outcomes among Caregivers of Older Adults Who Required Assistance with Activities of Daily Living (ADL). Bachelor’s Thesis, National University of Singapore, Singapore, 2020. [Google Scholar]
- Eklund, M.; Backstrom, M. The Role of Perceived Control for the Perception of Health by Patients with Persistent Mental Illness. Scand. J. Occup. Ther. 2006, 13, 249–256. [Google Scholar] [CrossRef]
- Crowe, L.; Butterworth, P. The Role of Financial Hardship, Mastery and Social Support in the Association between Employment Status and Depression: Results from an Australian Longitudinal Cohort Study. BMJ Open 2016, 6, e009834. [Google Scholar] [CrossRef]
- Chiu, M.; Wesson, V.; Sadavoy, J. Improving Caregiving Competence, Stress Coping, and Mental Well-Being in Informal Dementia Carers. World J. Psychiatry 2013, 3, 65–73. [Google Scholar] [CrossRef]
- Togari, T.; Yonekura, Y. A Japanese Version of the Pearlin and Schooler’s Sense of Mastery Scale. Springerplus 2015, 4, 399. [Google Scholar] [CrossRef] [Green Version]
- Eklund, M.; Erlandsson, L.K.; Hagell, P. Psychometric Properties of a Swedish Version of the Pearlin Mastery Scale in People with Mental Illness and Healthy People. Nord. J. Psychiatry 2012, 66, 380–388. [Google Scholar] [CrossRef] [Green Version]
- Gordon, J.R.; Malcarne, V.L.; Roesch, S.C.; Roetzheim, R.G.; Wells, K.J. Structural Validity and Measurement Invariance of the Pearlin Mastery Scale in Spanish-Speaking Primary Care Patients. Eval. Health Prof. 2018, 41, 393–399. [Google Scholar] [CrossRef]
- Chen, Y.-L.; Hsiung, P.-C.; Chung, L.; Chen, S.-C.; Pan, A.-W. Psychometric Properties of the Mastery Scale-Chinese version: Applying Classical Test Theory and Rasch Analysis. Scand. J. Occup. Ther. 2013, 20, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Gadalla, T.M. Sense of Mastery, Social Support, and Health in Elderly Canadians. J. Aging Health 2009, 21, 581–595. [Google Scholar] [CrossRef] [PubMed]
- Gadalla, T.M. The Role of Mastery and Social Support in the Association between Life Stressors and Psychological Distress in Older Canadians. J. Gerontol. Soc. Work 2010, 53, 512–530. [Google Scholar] [CrossRef]
- Chan, E.-Y.; Lim, Z.X.; Ding, Y.Y.; Chan, Y.H.; Lim, W.S. Development of a Brief Caregiver-Centric Screening Tool to Identify Risk of Depression among Caregivers of Hospitalized Older Adults. J. Nutr. Health Aging 2019, 23, 578–585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pioli, M.F. Global and Caregiving Mastery as Moderators in the Caregiving Stress Process. Aging Ment. Health 2010, 14, 603–612. [Google Scholar] [CrossRef] [PubMed]
- Roepke, S.K.; Mausbach, B.T.; Aschbacher, K.; Ziegler, M.G.; Dimsdale, J.E.; Mills, P.J.; von Känel, R.; Ancoli-Israel, S.; Patterson, T.L.; Grant, I. Personal Mastery is Associated with Reduced Sympathetic Arousal in Stressed Alzheimer Caregivers. Am. J. Geriatr. Psychiatry 2008, 16, 310–317. [Google Scholar] [CrossRef] [Green Version]
- Schreiner, A.S.; Morimoto, T. The Relationship between Mastery and Depression among Japanese Family Caregivers. Int. J. Aging Hum. Dev. 2003, 56, 307–321. [Google Scholar] [CrossRef]
- Skaff, M.M.; Pearlin, L.I.; Mullan, J.T. Transitions in the Caregiving Career: Effects on Sense of Mastery. Psychol. Aging 1996, 11, 247–257. [Google Scholar] [CrossRef]
- Sherwood, P.R.; Given, B.A.; Given, C.W.; Schiffman, R.F.; Murman, D.L.; von Eye, A.; Lovely, M.; Rogers, L.R.; Remer, S. The Influence of Caregiver Mastery on Depressive Symptoms. J. Nurs. Scholarsh. 2007, 39, 249–255. [Google Scholar] [CrossRef] [Green Version]
- Yang, F.M.; Kao, S.T. Item Response Theory for Measurement Validity. Shanghai Arch. Psychiatry 2014, 26, 171–177. [Google Scholar]
- Franzen, M.D. Item Response Theory. In Encyclopedia of Clinical Neuropsychology; Kreutzer, J.S., DeLuca, J., Caplan, B., Eds.; Springer: New York, NY, USA, 2011; p. 1362. [Google Scholar]
- Chan, T.S.-F.; Lam, L.C.-W.; Chiu, H.F.-K. Validation of the Chinese version of the Zarit Burden Interview. Hong Kong J. Psychiatry 2005, 15, 9–14. [Google Scholar]
- Leung, C.M.; Ho, S.; Kan, C.S.; Hung, C.H.; Chen, C.N. Evaluation of the Chinese version of the Hospital Anxiety and Depression Scale. A cross-cultural perspective. Int. J. Psychosom. 1993, 40, 29–34. [Google Scholar]
- Zarit, S.H.; Reever, K.E.; Bach-Peterson, J. Relatives of the Impaired Elderly: Correlates of Feelings of Burden. Gerontologist 1980, 20, 649–655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [Green Version]
- IBM Corp. IBM SPSS Statistics for Windows; Version 25.0; IBM Corp.: Armonk, NY, USA, 2017. [Google Scholar]
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Ltm, R.D. An R Package for Latent Variable Modelling and Item Response Theory Analyses. J. Stat. Softw. 2006, 17, 1–25. [Google Scholar]
- Rosseel, Y. Lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef] [Green Version]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting Structural Equation Modeling and Confirmatory Factor Analysis Results: A Review. J. Educ. Res. 2006, 99, 323–338. [Google Scholar] [CrossRef]
- McDonald, R.P.; Ho, M.H. Principles and Practice in Reporting Structural Equation Analyses. Psychol. Methods 2002, 7, 64–82. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance Tests and Goodness of Fit in the Analysis of Covariance Structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Samejima, F. Estimation of Latent Ability Using a Response Pattern of Graded Scores. Psychom. Monogr. Suppl. 1969, 34, 100. [Google Scholar] [CrossRef]
- Chua, K.C.; Bohnke, J.R.; Prince, M.; Banerjee, S. Health-Related Quality-of-Life Assessment in Dementia: Evidence of Cross-Cultural Validity in Latin America. Psychol. Assess. 2019, 31, 1264–1277. [Google Scholar] [CrossRef] [PubMed]
- Reeve, B.B.; Fayers, P. Applying Item Response Theory Modeling for Evaluating Questionnaire Item and Scale Properties. In Assessing Quality of Life in Clinical Trials: Methods and Practice; Fayers, P., Hays, R., Hays, R.D., Eds.; Oxford University Press: Oxford, UK, 2005; pp. 55–73. [Google Scholar]
- Reise, S.P.; Moore, T.M.; Haviland, M.G. Bifactor Models and Rotations: Exploring the Extent to which Multidimensional Data Yield Univocal Scale Scores. J. Personal. Assess. 2010, 92, 544–559. [Google Scholar] [CrossRef] [PubMed]
- Cortina, J.M. What is Coefficient Alpha? An Examination of Theory and Applications. J. Appl. Psychol. 1993, 78, 98–104. [Google Scholar] [CrossRef]
- Pearlin, L.I.; Bierman, A. Current Issues and Future Directions in Research into the Stress Process. In Handbook of the Sociology of Mental Health; Aneshensel, C.S., Phelan, J.C., Bierman, A., Eds.; Springer: Dordrecht, The Netherlands, 2013; pp. 325–340. [Google Scholar]
- Ebesutani, C.; Drescher, C.F.; Reise, S.P.; Heiden, L.; Hight, T.L.; Damon, J.D.; Young, J. The Loneliness Questionnaire-Short Version: An Evaluation of Reverse-Worded and Non-Reverse-Worded Items via Item Response Theory. J. Personal. Assess. 2012, 94, 427–437. [Google Scholar] [CrossRef]
- Lindwall, M.; Barkoukis, V.; Grano, C.; Lucidi, F.; Raudsepp, L.; Liukkonen, J.; Thøgersen-Ntoumani, C. Method Effects: The Problem with Negatively versus Positively Keyed Items. J. Personal. Assess. 2012, 94, 196–204. [Google Scholar] [CrossRef]
- Marsh, H.W. Positive and Negative Global Self-Esteem: A Substantively Meaningful Distinction or Artifactors? J. Personal. Soc. Psychol. 1996, 70, 810–819. [Google Scholar] [CrossRef]
- Menold, N. How Do Reverse-Keyed Items in Inventories Affect Measurement Quality and Information Processing? Field Methods 2020, 32, 140–158. [Google Scholar] [CrossRef]
- Ray, J.V.; Frick, P.J.; Thornton, L.C.; Steinberg, L.; Cauffman, E. Positive and Negative Item Wording and its Influence on the Assessment of Callous-Unemotional Traits. Psychol. Assess. 2016, 28, 394–404. [Google Scholar] [CrossRef]
- van Sonderen, E.; Sanderman, R.; Coyne, J.C. Ineffectiveness of Reverse Wording of Questionnaire Items: Let’s Learn from Cows in the Rain. PLoS ONE 2013, 8, e68967. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aneshensel, C.S.; Pearlin, L.I.; Mullan, J.T.; Zarit, S.H.; Whitlatch, C.J. Profiles in Caregiving: The Unexpected Career, San Diego; Academic Press: Cambridge, CA, USA, 1995. [Google Scholar]

| Demographic Characteristics | n (%)/Mean ± SD |
|---|---|
| Age, year | 57.6 ± 11.5 |
| Female | 260 (66.3) |
| Married | 217 (55.4) |
| Ethnicity | |
| Chinese | 331 (84.4) |
| Malay | 27 (6.9) |
| Indian | 23 (5.9) |
| Others | 11 (2.8) |
| Working (Full/Part-time) | 200 (51) |
| Live-in domestic helper | 194 (49.4) |
| Relationship to care-recipient | |
| Spouse | 61 (15.6) |
| Child | 285 (72.7) |
| Others | 46 (11.7) |
| Living with care-recipient | 307 (78.3) |
| Mastery (range 7 to 28) | 19.5 ± 3.3 |
| ZBI Burden (range 0 to 88) | 28.5 ± 15.1 |
| Depression, HADS subscale (range 0 to 21) | 5.6 ± 4.3 |
| Physical component summary, SF-12 subscale (range 0 to 50) | 47.3 ± 8.1 |
| Mental component summary, SF-12 subscale (range 0 to 50) | 45.4 ± 8.8 |
| Item | Graded Response Model Parameters | |||
|---|---|---|---|---|
| a | b1 | b2 | b3 | |
| 1 | 2.36 | −1.90 | −0.50 | 1.61 |
| 2 | 1.86 | −2.33 | −0.73 | 1.45 |
| 3 | 1.86 | −2.04 | −0.47 | 1.46 |
| 4 | 1.00 | −4.61 | −1.29 | 2.18 |
| 5 | 2.76 | −1.78 | −0.56 | 1.39 |
| 6 | 0.85 | −5.05 | −2.02 | 2.03 |
| 7 | 2.00 | −2.43 | −0.40 | 1.63 |
| Scale | Correlation with Original Scale | McDonald’s ω | Depressive Symptoms | Caregiver Burden | Health Related QoL | |
|---|---|---|---|---|---|---|
| Physical | Mental | |||||
| Mastery 7-item | - | 0.80 | −0.53 * | −0.52 * | 0.32 * | 0.40 * |
| Mastery 5-item | 0.96 * | 0.82 | −0.52 * | −0.54 * | 0.30 * | 0.40 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, Z.X.; Chua, W.L.; Lim, W.S.; Lim, A.Q.; Chua, K.C.; Chan, E.-Y. Psychometrics of the Pearlin Mastery Scale among Family Caregivers of Older Adults Who Require Assistance in Activities of Daily Living. Int. J. Environ. Res. Public Health 2022, 19, 4639. https://doi.org/10.3390/ijerph19084639
Lim ZX, Chua WL, Lim WS, Lim AQ, Chua KC, Chan E-Y. Psychometrics of the Pearlin Mastery Scale among Family Caregivers of Older Adults Who Require Assistance in Activities of Daily Living. International Journal of Environmental Research and Public Health. 2022; 19(8):4639. https://doi.org/10.3390/ijerph19084639
Chicago/Turabian StyleLim, Zhi Xiang, Wei Ling Chua, Wee Shiong Lim, An Qi Lim, Kia Chong Chua, and Ee-Yuee Chan. 2022. "Psychometrics of the Pearlin Mastery Scale among Family Caregivers of Older Adults Who Require Assistance in Activities of Daily Living" International Journal of Environmental Research and Public Health 19, no. 8: 4639. https://doi.org/10.3390/ijerph19084639
APA StyleLim, Z. X., Chua, W. L., Lim, W. S., Lim, A. Q., Chua, K. C., & Chan, E.-Y. (2022). Psychometrics of the Pearlin Mastery Scale among Family Caregivers of Older Adults Who Require Assistance in Activities of Daily Living. International Journal of Environmental Research and Public Health, 19(8), 4639. https://doi.org/10.3390/ijerph19084639






