(Mis)Information, Fears and Preventative Health Behaviours Related to COVID-19
Abstract
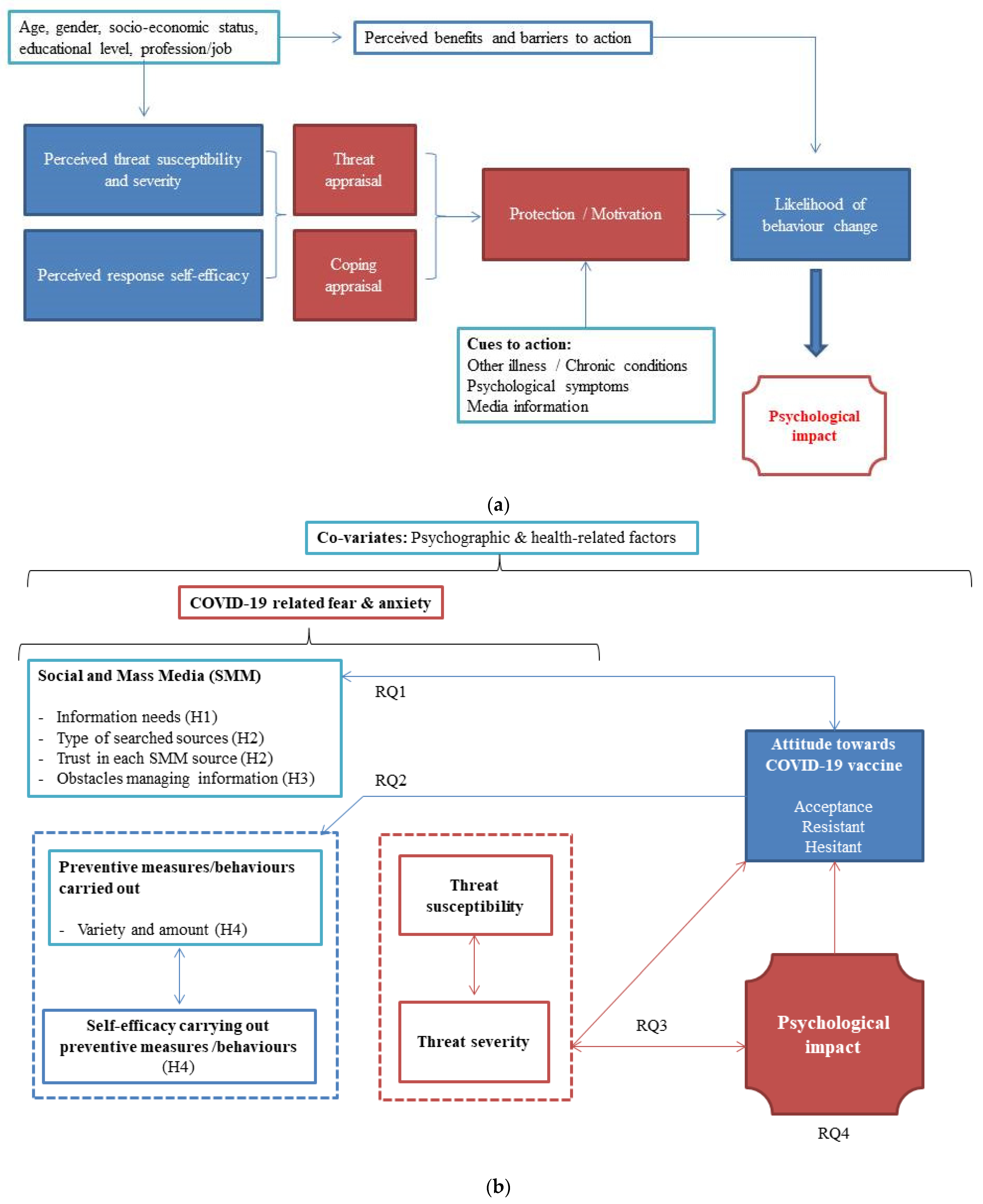
:1. Introduction
2. Materials and Methods
2.1. Design and Recruitment
2.2. Data Collection and Procedures
2.3. Outcomes and Covariates
2.3.1. Primary Outcome Variable
2.3.2. Other Variables
2.4. Ethics
2.5. Statistical Analysis
3. Results
3.1. Demographic Information and Response Rate
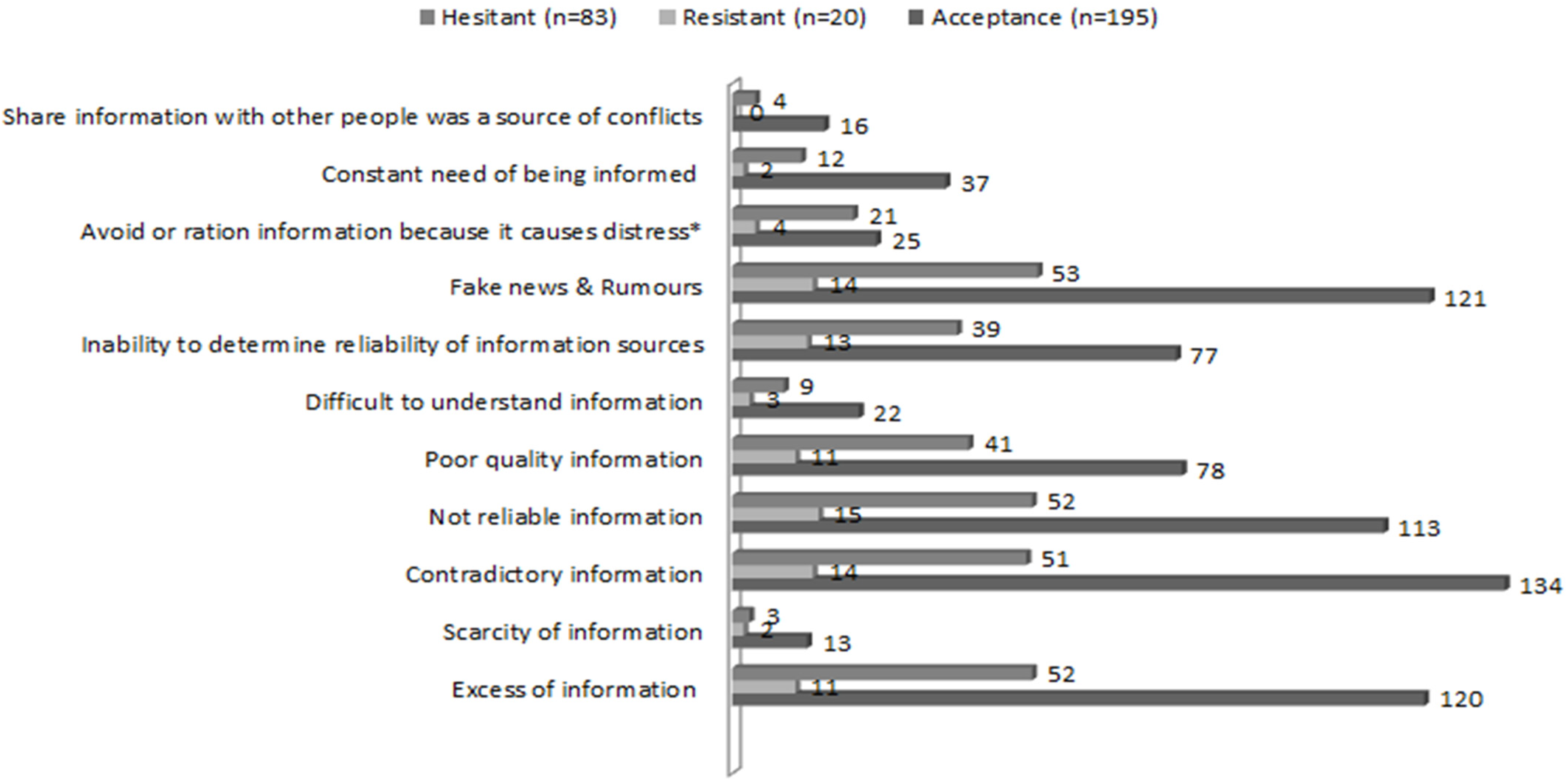
3.2. Results Concerning RQ1: How Do Different Profiles of Individuals Concerning Attitudes towards COVID-19 Vaccination (Accepting, Resistant, Hesitant) Behave in Terms of SMM Use to Seek Trustworthy Information? And What Type of Obstacles Related to COVID-19 Information/Management Experience Each of These Profiles?
3.3. Results Concerning RQ2: How Do Different Profiles of Individuals Concerning Attitudes towards COVID-19 Vaccination (Accepting, Resistant, Hesitant) Behave in Terms of Self-Efficacy and Preventive Behaviours Carried Out?
3.4. Results Concerning RQ3: How Perceived Threat Susceptibility and Severity Relates to Psychological Impact among Different Profiles of Individuals Concerning Attitudes towards COVID-19 Vaccination (Accepting, Resistant, Hesitant)?
3.5. Results Concerning RQ4: How Psychological Impact Relates to SMM Use/Experience, Self-Efficacy and Preventive Behaviours Carried out and Different Demographics and Psychographic Characteristics of the Sample for Each Profile of Individuals (Accepting, Resistant, Hesitant)?
4. Discussion
4.1. Limitations
4.2. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available online: https://coronavirus.jhu.edu/map.html (accessed on 8 June 2020).
- Available online: https://www.census.gov/popclock (accessed on 8 March 2022).
- Wiederhold, B.K. Using Social Media to Our Advantage: Alleviating Anxiety During a Pandemic. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 197–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carroll, J.K.; Moorhead, A.; Bond, R.; LeBlanc, W.G.; Petrella, R.J.; Fiscella, K. Who Uses Mobile Phone Health Apps and Does Use Matter? A Secondary Data Analytics Approach. J. Med Internet Res. 2017, 19, e125. [Google Scholar] [CrossRef] [Green Version]
- Ventola, C.L. Mobile devices and apps for health care professionals: Uses and benefits. Pharm. Ther. 2014, 39, 356–364. [Google Scholar]
- Wijesooriya, N.R.; Mishra, V.; Brand, P.L.P.; Rubin, B.K. COVID-19 and telehealth, education, and research adaptations. Paediatr. Respir. Rev. 2019, 35, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, S.; Howard, P.N. The Global Disinformation Order: 2019 Global Inventory of Organised Social Media Manipulation; Computational Propaganda Research Project: Oxford, UK, 2019. [Google Scholar]
- Fung, I.C.-H.; Duke, C.H.; Finch, K.C.; Snook, K.R.; Tseng, P.-L.; Hernandez, A.C.; Gambhir, M.; Fu, K.-W.; Tse, Z.T.H. Ebola virus disease and social media: A systematic review. Am. J. Infect. Control 2016, 44, 1660–1671. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization [WHO]. Available online: https://www.who.int/immunization/sage/meetings/2014/october/3_SAGE_WG_Strategies_addressing_vaccine_hesitancy_2014.pdf (accessed on 8 March 2022).
- World Health Organization. Coronavirus Disease (COVID-19) Advice for the Public: Myth Busters. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters (accessed on 23 April 2020).
- Lewandowsky, S.; Cook, J.; Schmid, P.; Holford, D.L.; Finn, A.; Leask, J.; Thomson, A.; Lombardi, D.; Al-Rawi, A.K.; Amazeen, M.A.; et al. The COVID-19 Vaccine Communication Handbook. A Practical Guide for Improving Vaccine Communication and Fighting Misinformation. 2021. Available online: https://sks.to/c19vax (accessed on 8 March 2022).
- World Health Organization [WHO]. Available online: https://www.who.int/health-topics/infodemic#tab=tab_1 (accessed on 8 March 2022).
- Ratzan, S.C. “Vaccine Communication in a Pandemic: Improving Vaccine Literacy to Reduce Hesitancy, Restore Trust and Immunize Communities”: Editor’s Introduction. J. Health Commun. 2020, 25, 745–746. [Google Scholar] [CrossRef] [PubMed]
- Garfin, D.R. Technology as a coping tool during the coronavirus disease 2019 (COVID-19) pandemic: Implications and rec-ommendations. Stress Health 2020, 36, 555–559. [Google Scholar] [CrossRef]
- Kalantzi, S.; Kostagiolas, P.; Kechagias, G.; Niakas, D.; Makrilakis, K. Information seeking behavior of patients with diabetes mellitus: A cross-sectional study in an outpatient clinic of a university-affiliated hospital in Athens, Greece. BMC Res. Notes 2015, 8, 48. [Google Scholar] [CrossRef] [Green Version]
- Kostagiolas, P.; Tsiligros, P.; Theodorou, P.; Tentolouris, N.; Niakas, D. A cross-sectional survey interconnecting health information seeking behavior with clinical data of type 2 diabetes mellitus patients. Libr. Hi Tech 2020, 39, 448–461. [Google Scholar] [CrossRef]
- Majid, S.; Rahmat, N.A. Information Needs and Seeking Behavior During the H1N1 Virus Outbreak. J. Inf. Sci. Theory Pract. 2013, 1, 42–53. [Google Scholar] [CrossRef] [Green Version]
- Odlum, M.; Yoon, S. Health Information Needs and Health Seeking Behavior during the 2014-2016 Ebola Outbreak: A Twitter Content Analysis. PLoS Curr. 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Green, E.C.; Murphy, E. Health Belief Model. Wiley Encycl. Health Psychol. 2014, 766–769. [Google Scholar] [CrossRef]
- Rogers, R.W. A Protection Motivation Theory of Fear Appeals and Attitude Change. J. Psychol. 1975, 91, 93–114. [Google Scholar] [CrossRef] [PubMed]
- Hou, Z.; Du, F.; Zhou, X.; Jiang, H.; Martin, S.; Larson, H.; Lin, L. Cross-Country Comparison of Public Awareness, Rumors, and Behavioral Responses to the COVID-19 Epidemic: Infodemiology Study. J. Med. Internet Res. 2020, 22, e21143. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Broström, A.; Griffiths, M.D.; Pakpour, A.H. Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interv. 2020, 21, 100345. [Google Scholar] [CrossRef]
- Austin, E.W.; Austin, B.W.; Willoughby, J.F.; Amram, O.; Domgaard, S. How Media Literacy and Science Media Literacy Predicted the Adoption of Protective Behaviors Amidst the COVID-19 Pandemic. J. Health Commun. 2021, 26, 239–252. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [Green Version]
- Chen, K.; Chen, A.; Zhang, J.; Meng, J.; Shen, C. Conspiracy and debunking narratives about COVID-19 origins on Chinese social media: How it started and who is to blame. Harv. Kennedy Sch. Misinf. Rev. 2020. [Google Scholar] [CrossRef]
- COVID-19-related Misinformation: Fabricated and Unverified Content on Social Media. Anal. Metaphys. 2020, 19, 87. [CrossRef]
- van der Pligt, J.; De Vries, N.K. Expectancy-Value models of health behaviour: The role of salience and anticipated affect. Psychol. Health 1998, 13, 289–305. [Google Scholar] [CrossRef]
- Park, T.; Ju, I.; Ohs, J.E.; Hinsley, A. Optimistic bias and preventive behavioral engagement in the context of COVID-19. Res. Soc. Adm. Pharm. 2020, 17, 1859–1866. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, N. Health Risk Appraisal and Optimistic Bias. In International Encyclopedia of the Social & Behavioral Sciences; Elsevier: Amsterdam, The Netherlands, 2001; pp. 6612–6615. [Google Scholar]
- Du, H.; Yang, J.; King, R.B.; Yang, L.; Chi, P. COVID-19 Increases Online Searches for Emotional and Health-Related Terms. Applied Psychology. Health Well-Being 2020, 12, 1039–1053. [Google Scholar] [CrossRef] [PubMed]
- Castellano-Tejedor, C.; Torres-Serrano, M.; Cencerrado, A. Psychological impact in the time of COVID-19: A cross-sectional population survey study during confinement. J. Health Psychol. 2021, 27, 974–989. [Google Scholar] [CrossRef] [PubMed]
- Kshirsagar, M.M.; Dodamani, A.S.; Dodamani, G.A.; Khobragade, V.R.; Deokar, R.N. Impact of Covid-19 on Mental Health: An Overview. Rev. Recent Clin. Trials 2021, 16, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Rathod, S.; Pallikadavath, S.; Young, A.H.; Graves, L.; Rahman, M.M.; Brooks, A.; Soomro, M.; Rathod, P.; Phiri, P. Psy-chological impact of COVID-19 pandemic: Protocol and results of first three weeks from an international cross-section survey—Focus on health professionals. J. Affect. Disord. Rep. 2020, 1, 100005. [Google Scholar] [CrossRef] [PubMed]
- Rieckert, A.; Schuit, E.; Bleijenberg, N.; Cate, D.T.; De Lange, W.; Ginkel, J.M.D.M.-V.; Mathijssen, E.; Smit, L.C.; Stalpers, D.; Schoonhoven, L.; et al. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open 2021, 11, e043718. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Pakpour, A.H. The Association Between Health Status and Insomnia, Mental Health, and Preventive Behaviors: The Mediating Role of Fear of COVID-19. Gerontol. Geriatr. Med. 2020, 6. [Google Scholar] [CrossRef]
- Pramukti, I.; Strong, C.; Sitthimongkol, Y.; Setiawan, A.; Pandin, M.G.R.; Yen, C.-F.; Lin, C.-Y.; Griffiths, M.D.; Ko, N.-Y. Anxiety and Suicidal Thoughts During the COVID-19 Pandemic: Cross-Country Comparative Study Among Indonesian, Taiwanese, and Thai University Students. J. Med. Internet Res. 2020, 22, e24487. [Google Scholar] [CrossRef]
- Allen, J.D.; Feng, W.; Corlin, L.; Porteny, T.; Acevedo, A.; Schildkraut, D.; King, E.; Ladin, K.; Fu, Q.; Stopka, T.J. Why are some people reluctant to be vaccinated for COVID-19? A cross-sectional survey among U.S. Adults in May–June 2020. Prev. Med. Rep. 2021, 24, 101494. [Google Scholar] [CrossRef]
- Nomura, S.; Eguchi, A.; Yoneoka, D.; Kawashima, T.; Tanoue, Y.; Murakami, M.; Sakamoto, H.; Maruyama-Sakurai, K.; Gilmour, S.; Shi, S.; et al. Reasons for being unsure or unwilling regarding intention to take COVID-19 vaccine among Japanese people: A large cross-sectional national survey. Lancet Reg. Health-West. Pac. 2021, 14, 100223. [Google Scholar] [CrossRef] [PubMed]
- Teasdale, C.A.; Borrell, L.N.; Shen, Y.; Kimball, S.; Rinke, M.L.; Fleary, S.A.; Nash, D. Parental plans to vaccinate children for COVID-19 in New York city. Vaccine 2021, 39, 5082–5086. [Google Scholar] [CrossRef] [PubMed]
- Hafstad, G.S.; Augusti, E.-M. A lost generation? COVID-19 and adolescent mental health [Review of A lost generation? COVID-19 and adolescent mental health]. Lancet. Psychiatry 2021, 8, 640–641. [Google Scholar] [CrossRef]
- Fenollar-Cortés, J.; Jiménez, Ó.; Ruiz-García, A.; Resurrección, D.M. Gender Differences in Psychological Impact of the Confinement During the COVID-19 Outbreak in Spain: A Longitudinal Study. Front. Psychol. 2021, 12, 682860. [Google Scholar] [CrossRef] [PubMed]
- Singer, E.; Van Hoewyk, J.; Maher, M.P. Experiments with Incentives in Telephone Surveys. Public Opin. Q. 2000, 64, 171–188. [Google Scholar] [CrossRef]

| Variables | n (%) |
|---|---|
| Gender (Female) | 227 (75.7%) |
| Country of origin | |
| Spain | 291 (97%) |
| Other a | 9 (3%) |
| Cohabiting | |
| Alone | 32 (10.7%) |
| Couple/Partner | 192 (64%) |
| Mother | 57 (19%) |
| Father | 40 (13.3%) |
| Children | 118 (39.3%) |
| Siblings | 26 (8.7%) |
| Grandmother | 3 (1%) |
| Grandfather | 1 (0.3%) |
| Mother-in-law | 3 (1%) |
| Father-in-law | 1 (0.3%) |
| Caregiver (formal/informal) | 2 (0.7%) |
| Pet(s) | 55 (18.3%) |
| Flat mates | 16 (5.3%) |
| Vulnerable individuals at charge (Yes) b | 65 (21.8%) |
| COVID-19 diagnosis (Yes) | 43 (14.3%) |
| Chronic disease (Yes) | 55 (18.3%) |
| Loss of a relative/family member due to COVID-19 (Yes) | 51 (17%) |
| Age | |
| 18–35 | 114 (38%) |
| 36–59 | 160 (53.3%) |
| >60 | 26 (8.7%) |
| Occupation (Healthcare professionals vs. others) | 131 (43.7%) |
| Education | |
| Primary school | 9 (3%) |
| Secondary school | 21 (7%) |
| Higher education | 52 (17.3%) |
| University degree | 178 (59.3%) |
| PhD | 25 (8.3%) |
| Other degrees | 15 (5%) |
| Employment situation | |
| Working | 243 (81%) |
| Temporary Labor Force adjustment | 5 (7.8%) |
| Dismissal | 2 (3.1%) |
| Unemployed | 9 (14.1%) |
| Self-perceived socio-economic status | |
| Low | 52 (17.3%) |
| Medium | 230 (76.7%) |
| High | 18 (6%) |
| Attitude towards COVID-19 vaccination | |
| Accepting | 195 (65.4%) |
| Resistant | 20 (6.7%) |
| Hesitant | 83 (27.8%) |
| Variables (yes Option Displayed) | Accepting (n = 195) n (%) | Resistant (n = 20) n (%) | Hesitant (n = 83) n (%) |
|---|---|---|---|
| General information | 167 (56%) | 16 (5.4%) | 70 (23.5%) |
| Statistical data * | 126 (42.3%) | 9 (3%) | 43 (14.4%) |
| How to diagnose/identify positive cases | 118 (39.6%) | 11 (3.7%) | 50 (16.8%) |
| Preventive/protective behaviors/measures | 128 (43%) | 9 (3%) | 55 (18.5%) |
| COVID-19 treatment(s) | 86 (28.9%) | 8 (2.7%) | 27 (9.1%) |
| Regulations/restrictions | 165 (55.4%) | 13 (4.4%) | 68 (22.8%) |
| Quarantine/Confinement physical/psychosocial recommendations * | 99 (33.2%) | 5 (1.7%) | 35 (11.7%) |
| Mental health recommendations | 66 (22.1%) | 3 (1%) | 23 (7.7%) |
| Positive family functioning/environment recommendations | 34 (11.4%) | 3 (1%) | 7 (2.3%) |
| Remote work and family life conciliation recommendations | 25 (8.4%) | 3 (1%) | 9 (3%) |
| Other information searched: | |||
| 1 (0.3%) | 0 | 0 |
| 1 (0.3%) | 0 | 0 |
| 2 (0.6%) | 0 | 0 |
| 1 (0.3%) | 0 | 0 |
| 1 (0.3%) | 0 | 1 (0.3%) |
| 1 (0.3%) | 0 | 0 |
| 0 | 0 | 1 (0.3%) |
| 1 (0.3%) | 0 | 0 |
| 1 (0.3%) | 0 | 0 |
| Variables | Accepting (n = 195) M ± SD, Range | Resistant (n = 20) M ± SD, Range | Hesitant (n = 83) M ± SD, Range |
|---|---|---|---|
| TV * | 4.03 ± 1.29, 1–7 | 2.65 ± 1.35, 1–5 | 3.51 ± 1.30, 1–7 |
| Radio * | 3.90 ± 1.24, 1–7 | 2.75 ± 1.25, 1–5 | 3.54 ± 1.23, 1–6 |
| Written press * | 3.81 ± 1.23, 1–6 | 2.55 ± 1.23, 1–4 | 3.39 ± 1.39, 1–6 |
| Web-based press * | 3.79 ± 1.30, 1–7 | 2.55 ± 1.47, 1–5 | 3.43 ± 1.39, 1–6 |
| 2.51 ± 1.37, 1–6 | 2.20 ± 1.44, 1–5 | 2.42 ± 1.05, 1–5 | |
| 1.93 ± 1.11, 1–6 | 2.10 ± 1.29, 1–5 | 2.18 ± 1.15, 1–6 | |
| Telegram | 2.11 ± 1.17, 1–6 | 1.90 ± 1.55, 1–6 | 2.20 ± 1.08, 1–6 |
| 1.92 ± 1.15, 1–7 | 2.05 ± 1.50, 1–7 | 2.14 ± 1.05, 1–5 | |
| Healthcare professionals * | 5.69 ± 1.10, 3–7 | 4.85 ± 1.53, 2–7 | 5.35 ± 1.23, 1–7 |
| Scientific papers & publications * | 5.81 ± 1.18, 1–7 | 4.95 ± 1.57, 2–7 | 5.48 ± 1.06, 3–7 |
| WHO official channels * | 5.24 ± 1.33, 1–7 | 4.10 ± 1.74, 1–7 | 4.71 ± 1.44, 1–7 |
| Health Department official channels (state) * | 4.72 ± 1.34, 1–7 | 3.30 ± 1.78, 1–7 | 4.20 ± 1.47, 1–7 |
| Health Department official channels (regional)* | 4.67 ± 1.36, 1–7 | 3.60 ± 1.60, 1–7 | 4.34 ± 1.36, 2–7 |
| Friends & acquaintances | 3.04 ± 1.22, 1–7 | 2.50 ± 1.43, 1–5 | 3.01 ± 1.43, 1–7 |
| The Internet (in general) | 2.59 ± 1.09, 1–5 | 2.55 ± 1.60, 1–6 | 2.72 ± 1.13, 1–5 |
| Specialized web pages * | 4.41 ± 1.34, 1–7 | 3.65 ± 1.46, 1–6 | 3.95 ± 1.30, 1–7 |
| Accepting (n = 195) * | Resistant (n = 20) | Hesitant (n = 83) | ||||
|---|---|---|---|---|---|---|
| Medium-to-Low Psychological Impact (n = 126) | High Psychological Impact (n = 69) | Medium-to-Low Psychological Impact (n = 14) | High Psychological Impact (n = 6) | Medium-to-Low Psychological Impact (n = 57) | High Psychological Impact (n = 26) | |
| Threat susceptibility M ± SD, 95%CI, range | 7.06 ± 2.20 [6.68–7.45] 0–10 | 7.99 ± 1.55 [7.61–8.36] 2–10 | 6.07 ± 2.40 [4.69–7.46] 2–9 | 7.50 ± 1.97 [5.43–9.57] 4–10 | 6.98 ± 1.67 [6.54–7.43] 2–10 | 7.31 ± 1.62 [6.65–7.96] 5–10 |
| Threat severity, M ± SD, 95%CI, range | 6.98 ± 2.12 [6.61–7.36] 0–10 | 7.41 ± 1.93 [6.99–7.87] 2–10 | 5.79 ± 2.81 [4.17–7.41] 0–10 | 6.83 ± 2.48 [4.23–9.44] 3–10 | 6.65 ± 2.17 [6.07–7.23] 1–10 | 6.42 ± 2.56 [5.39–7.46] 1–10 |
| Accepting (n = 195) | B | t | p | 95% CI |
|---|---|---|---|---|
| (Constant) | 5.868 | <0.001 | 4.125–8.302 | |
| GAD-7 | 0.286 | 4.583 | <0.001 | 0.097–0.243 |
| Age | −0.295 | −4.810 | <0.001 | −0.100–−0.042 |
| Threat susceptibility | 0.171 | 2.796 | 0.006 | 0.074–0.430 |
| Chronic disease | 0.198 | 3.225 | 0.001 | 0.490–2.032 |
| Gender | −0.181 | −2.953 | 0.004 | −2.043–−0.407 |
| Hesitant (n = 83) | B | t | p | 95% CI |
| (Constant) | 0.663 | 0.509 | −2.233–4.462 | |
| Total of psychological symptoms reported | 0.451 | 5.359 | <0.001 | 0.266–0.582 |
| Trust in scientific papers & publication | 0.243 | 2.970 | 0.004 | 0.206–1.043 |
| Trust in Internet in general | −0.195 | −2.462 | 0.016 | −0.852–−0.90 |
| Threat susceptibility | 0.206 | 2.589 | 0.012 | 0.078–0.601 |
| Gender | −0.265 | −3.270 | 0.002 | −2.869–−0.697 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castellano-Tejedor, C.; Torres-Serrano, M.; Cencerrado, A. (Mis)Information, Fears and Preventative Health Behaviours Related to COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 4539. https://doi.org/10.3390/ijerph19084539
Castellano-Tejedor C, Torres-Serrano M, Cencerrado A. (Mis)Information, Fears and Preventative Health Behaviours Related to COVID-19. International Journal of Environmental Research and Public Health. 2022; 19(8):4539. https://doi.org/10.3390/ijerph19084539
Chicago/Turabian StyleCastellano-Tejedor, Carmina, María Torres-Serrano, and Andrés Cencerrado. 2022. "(Mis)Information, Fears and Preventative Health Behaviours Related to COVID-19" International Journal of Environmental Research and Public Health 19, no. 8: 4539. https://doi.org/10.3390/ijerph19084539
APA StyleCastellano-Tejedor, C., Torres-Serrano, M., & Cencerrado, A. (2022). (Mis)Information, Fears and Preventative Health Behaviours Related to COVID-19. International Journal of Environmental Research and Public Health, 19(8), 4539. https://doi.org/10.3390/ijerph19084539







