Rasch-Validated Italian Scale for Diagnosing Digital Eye Strain: The Computer Vision Syndrome Questionnaire IT©
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Italian Version of the Computer Vision Syndrome Questionnaire (CVS-Q IT©)
2.2. Design, Target Population, and Ethical Aspects
2.3. Procedure
2.4. Statistical Analysis
2.4.1. Sample Description
2.4.2. Rasch–Andrich Rating Scale Model Analysis
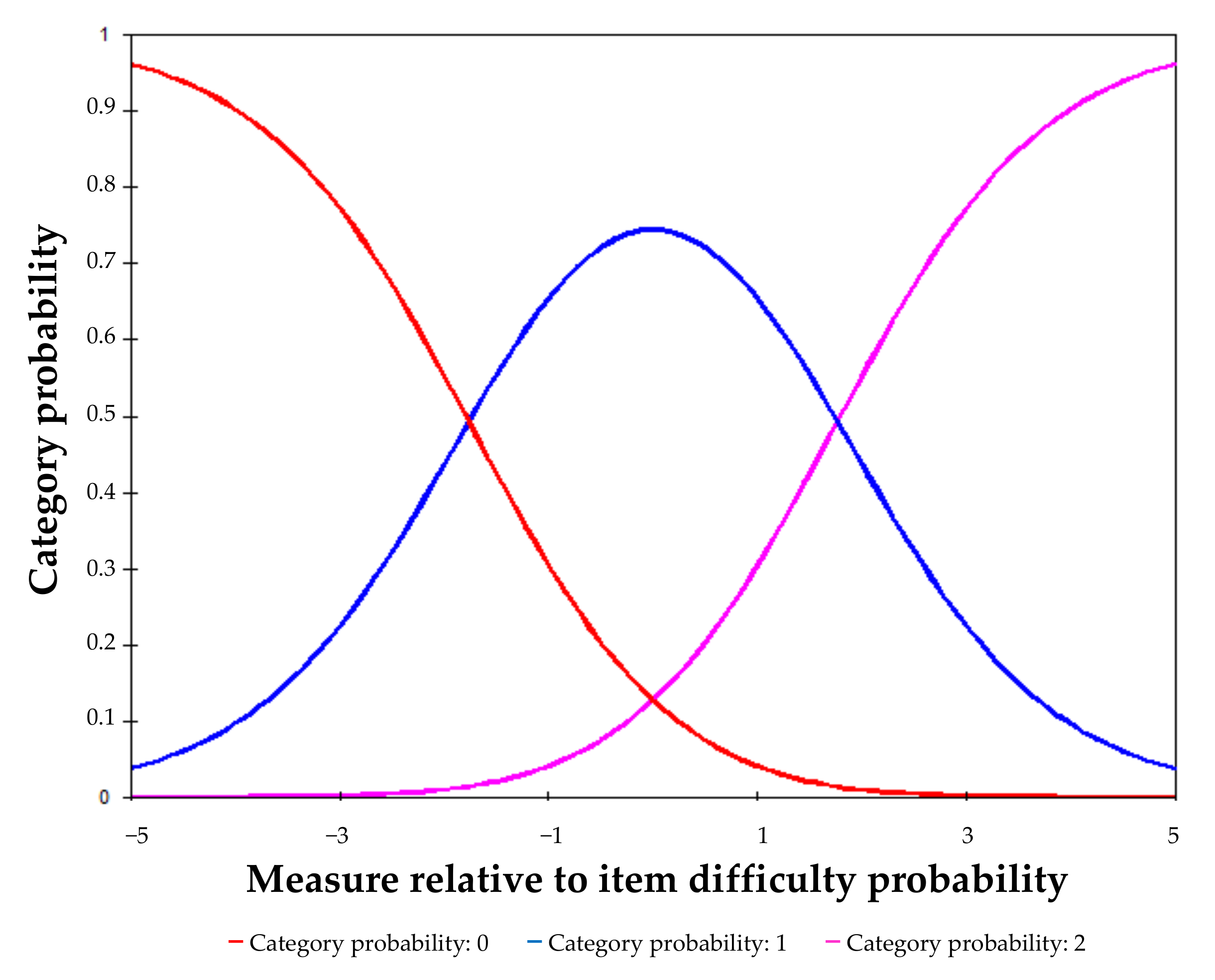
- The performance of the rating scale. The two thresholds of the rating scale (a threshold between categories 0 and 1 and a threshold between categories 1 and 2) should advance monotonically, i.e., they should be ordered, and the separation between them should be at least 1.4 logits. In addition, the average measures of the categories should also advance monotonically;
- The fit of the items and the response structure to the model predictions. For this, infit and outfit mean square error (MNSQ) chi-square statistics were used. Infit MNSQ gives more weight to differences close to the point where item difficulty and subject ability are matched, and outfit MNSQ includes all differences, regardless of the match between difficulty and ability. Ideally, such values should be close to unity, with a critical range of 0.7–1.3, if the fit to the Rasch model is good [33];
- The fit of persons to model predictions, using the MNSQ statistics referring to persons. This analysis focuses on detecting persons with MNSQ values greater than two and examining their influence on the model parameters;
- The assumptions of unidimensionality (only one dimension determines the response to the items) and local independence (the response to one item is not influenced by the responses to the other test items once the level in the trait is controlled). Unidimensionality was assessed using the principal component (PC) analyses of Rasch residuals. The variance explained by the first contrast should be <10%, and the eigenvalue of the first contrast should be <1.9 [34]. In addition, the examination of the patterns of item loadings can give information about the relevance of possible secondary dimensions. Local independence is examined using the residual correlations between items: if they are equal to or less than 0.3, local independence can be assumed [35];
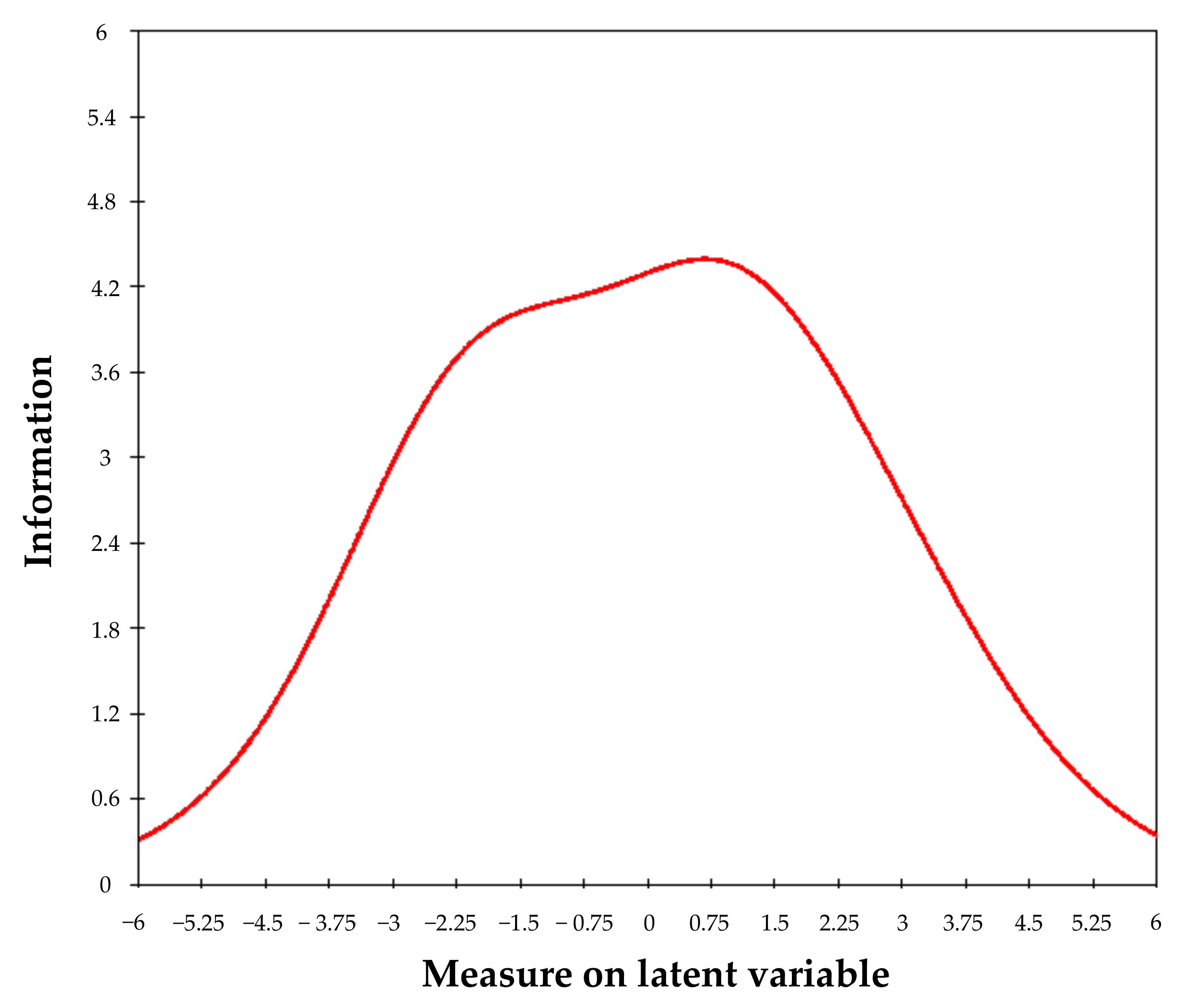
- Measurement error and reliability item–person model. Compared to a global indicator of scale precision, such as the standard error measurement (SEM), IRT models enable us to estimate the information function of the test (and its reciprocal, the standard error function). This function describes the variation of scale precision along with the trait. As a measure of scale reliability in the sample, the Rasch model’s person separation reliability statistic was employed, which is analogous to Cronbach’s alpha (and which we also compute) and uses logits (the linear scores) instead of raw scores. Person separation reliability usually underestimates reliability, whereas Cronbach’s alpha overestimates it. Reliability should be equal to or higher than 0.7 [36];
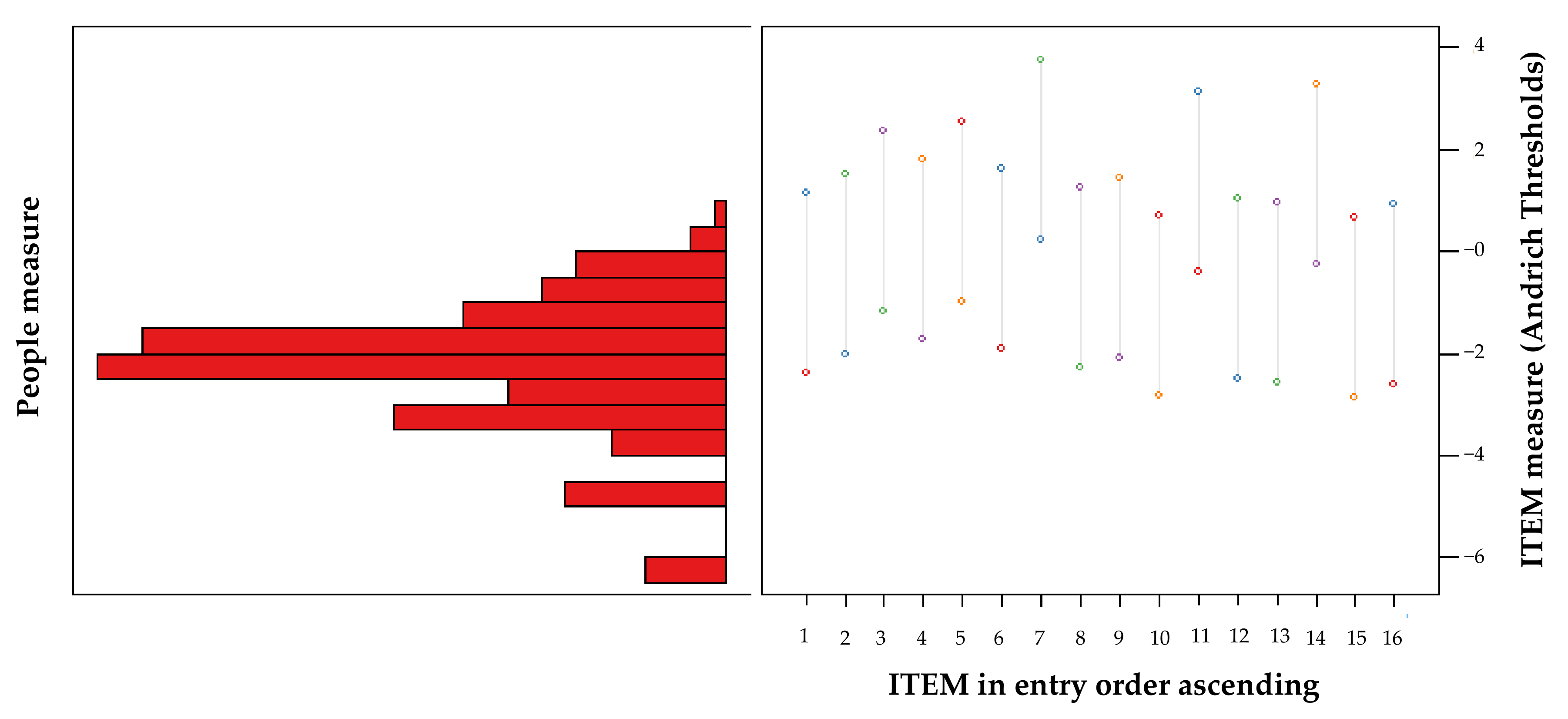
- Targeting the difficulty level of the items to the sample. A good alignment between items and persons occurs when a given person’s mean scores are close to 0 logits, which is the value at which the scale is centred and corresponds to the mean of the items. In addition, a joint mapping of item and person locations allows for a more detailed exploration of the target;
- Analysis of differential item functioning (DIF) and its impact on scale scores. DIF was examined as a function of gender (female vs. male), age (40+ vs. 40−), and version of the questionnaire (Spanish vs. Italian). It was considered an item to have severe DIF if the between-group contrast (DIF size) was >1 and the t-Student value was significant at the 0.05 level, after Bonferroni correction (0.05/16 = 0.003). This was followed by an iterative procedure that eliminated a single item at each step to achieve a purified scale without DIF. To examine the impact of DIF on the scale scores, the procedure developed by Tennant was followed [37]. The proportion of estimates that differed by 0.5 logits or more was calculated as an indicator of the impact of DIF on the non-trivial scores.
2.4.3. Test–Retest Reliability
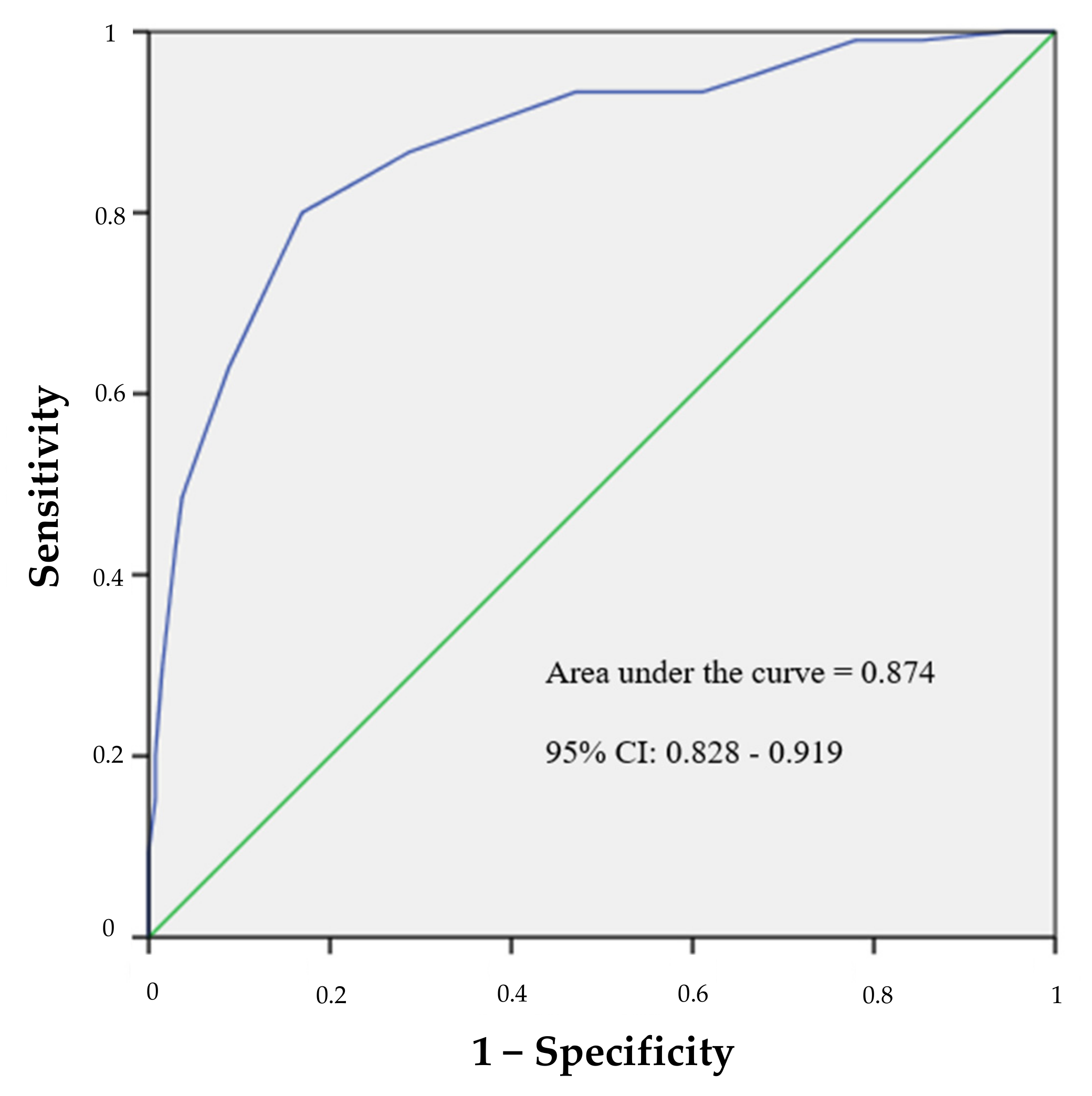
2.4.4. Criterion Validity—Sensitivity, Specificity and ROC Curve
2.4.5. Construct Validity Based on Known Groups
2.5. Prevalence of CVS and Frequency and Intensity of CVS-Q IT© Symptoms
3. Results
3.1. Description of the Study Sample
3.2. Rasch–Andrich Rating Scale Model Analysis
3.3. Test–Retest Reliability
3.4. Criterion Validity—Sensitivity, Specificity and ROC Curves
3.5. Construct Validity Based on Known Groups
3.6. Prevalence of CVS and Frequency and Intensity of Symptoms of CVS-Q IT©
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sheppard, A.L.; Wolffsohn, J.S. Digital eye strain: Prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018, 3, e000146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Munshi, S.; Varghese, A.; Dhar-Munshi, S. Computer vision syndrome—A common cause of unexplained visual symptoms in the modern era. Int. J. Clin. Pract. 2017, 71, e12962. [Google Scholar] [CrossRef] [PubMed]
- American Optometric Association, Computer Vision Syndrome. Available online: https://www.aoa.org/patients-and-public/caring-for-your-vision/protecting-your-vision/computer-vision-syndrome (accessed on 25 November 2021).
- Randolph, S.A. Computer Vision Syndrome. Workplace Health Saf. 2017, 65, 328. [Google Scholar] [CrossRef] [PubMed]
- Bahkir, F.A.; Grandee, S.S. Impact of the COVID-19 lockdown on digital device-related ocular health. Indian J. Ophthalmol. 2020, 68, 2378–2383. [Google Scholar] [CrossRef]
- Salinas-Toro, D.; Cartes, C.; Segovia, C.; Alonso, M.J.; Soberon, B.; Sepulveda, M.; Zapata, C.; Yañez, P.; Traipe, L.; Goya, C.; et al. High frequency of digital eye strain and dry eye disease in teleworkers during the coronavirus disease (2019) pandemic. Int. J. Occup. Saf. Ergon. 2021, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- EUROSTAT. Eurostat Database. Available online: https://ec.europa.eu/eurostat/web/main/data/database (accessed on 30 November 2021).
- Xiao, Y.; Becerik-Gerber, B.; Lucas, G.; Roll, S.C. Impacts of Working from Home during COVID-19 Pandemic on Physical and Mental Well-Being of Office Workstation Users. J. Occup. Environ. Med. 2021, 63, 181–190. [Google Scholar] [CrossRef]
- González-Menéndez, E.; López-González, M.J.; González Menéndez, S.; García González, G.; Álvarez Bayona, T. Major health consequences a rising from the continued use of new electronic devices with visual display units. Rev. Esp. Salud Pública 2019, 93, 201908062. [Google Scholar]
- Ganne, P.; Najeeb, S.; Chaitanya, G.; Sharma, A.; Krishnappa, N.C. Digital Eye Strain Epidemic amid COVID-19 Pandemic—A Cross-sectional Survey. Ophthalmic Epidemiol. 2021, 28, 285–292. [Google Scholar] [CrossRef]
- Ap Vilela, M.; Castagno, V.D.; Meucci, R.D.; Fassa, A.G. Asthenopia in schoolchildren. Clin. Ophthalmol. 2015, 9, 1595–1603. [Google Scholar] [CrossRef] [Green Version]
- Assefa, N.L.; Weldemichael, D.Z.; Alemu, H.W.; Anbesse, D.H. Prevalence and associated factors of computer vision syndrome among bank workers in Gondar City, northwest Ethiopia, 2015. Clin. Optom. 2017, 9, 67–76. [Google Scholar] [CrossRef] [Green Version]
- Dessie, A.; Adane, F.; Nega, A.; Wami, S.D.; Chercos, D.H. Computer Vision Syndrome and Associated Factors among Computer Users in Debre Tabor Town, Northwest Ethiopia. J. Environ. Public Health 2018, 2018, 4107590. [Google Scholar] [CrossRef] [PubMed]
- Coles-Brennan, C.; Sulley, A.; Young, G. Management of digital eye strain. Clin. Exp. Optom. 2019, 102, 18–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajabi-Vardanjani, H.; Habibi, E.; Pourabdian, S.; Dehghan, H.; Maracy, M.R. Designing and Validation a Visual Fatigue Questionnaire for Video Display Terminals Operators. Int. J. Prev. Med. 2014, 5, 841–848. [Google Scholar] [PubMed]
- González-Pérez, M.; Susi, R.; Antona, B.; Barrio, A.; González, E. The Computer-Vision Symptom Scale (CVSS17): Development and Initial Validation. Investig. Opthalmol. Vis. Sci. 2014, 55, 4504–4511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seguí, M.D.M.; Cabrero-García, J.; Crespo, A.; Verdú, J.; Ronda, E. A reliable and valid questionnaire was developed to measure computer vision syndrome at the workplace. J. Clin. Epidemiol. 2015, 68, 662–673. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seguí-Crespo, M.; Cantó Sancho, N.; Ronda, E.; Colombo, R.; Porru, S.; Carta, A. Translation and cultural adaptation of the Computer Vision Syndrome Questionnaire (CVS-Q) into Italian. Med. Lav. 2019, 110, 37–45. [Google Scholar] [CrossRef]
- Mikulášová, E.; Cantó-Sancho, N.; Pérez, P.C.; Ronda-Pérez, E.; Seguí-Crespo, M. Translation and cultural adaptation of the Computer Vision Syndrome Questionnaire (CVS-Q) into Slovak. Hygiena 2020, 65, 84–92. [Google Scholar] [CrossRef]
- Carta, A.; Pasquini, L.; Lucchini, R.; Semeraro, F.; Apostoli, P. Relation of asthenopia and some ophthalmological, neuropsychological, and musculoskeletal parameters in workers assigned to video display terminals. Med. Lav. 2003, 94, 466–479. [Google Scholar]
- Fenga, C.; Cacciola, A.; Anzalone, C.; Trimarchi, G.; Grillo, O.C. Influence of microclimate factors on ocular discomfort in video display terminal workers. G. Ital. Med. Lav. Ergon. 2006, 27, 417–421. [Google Scholar]
- Taino, G.; Ferrari, M.; Mestad, I.J.; Fabris, F.; Imbriani, M. Asthenopia and work at video display terminals: Study of 191 workers exposed to the risk by administration of a standardized questionnaire and ophthalmologic evaluation. G. Ital. Med. Lav. Ergon. 2007, 28, 487–497. [Google Scholar]
- Fenga, C.; Di Pietro, R.; Fenga, P.; Di Nola, C.; Spinella, R.; Cacciola, A.; Germanò, D.; Aragona, P. Asthenopia in VDT users: Our experience. G. Ital. Med. Lav. Ergon. 2008, 29, 500–501. [Google Scholar]
- Fenga, C.; Aragona, P.; Cacciola, A.; Spinella, R.; Di Nola, C.; Ferreri, F.; Rania, L. Meibomian gland dysfunction and ocular discomfort in video display terminal workers. Eye 2007, 22, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Carta, A.; Oppini, M.; Bellina, B.; Crippa, M.; Lucchini, R.; Porru, S.; Alessio, L. VDT use and others visual demanding works: Risks and prevention. G. Ital. Med. Lav. Ergon. 2010, 32 (Suppl. S2), 90–91. [Google Scholar]
- Filon, F.L.; Drusian, A.; Ronchese, F.; Negro, C. Video Display Operator Complaints: A 10-Year Follow-Up of Visual Fatigue and Refractive Disorders. Int. J. Environ. Res. Public Health 2019, 16, 2501. [Google Scholar] [CrossRef] [Green Version]
- Società Italiana di Medicina del Lavoro (SIML). Available online: https://www.siml.it/ (accessed on 30 November 2021).
- Piccoli, B.G.; Colais, L.; Leka, I.; Battevi, N.; Di Bari, A.; Di Bisceglie, M.; Grosso, D.; Muzi, G.; Paraluppi, P.; Santucci, P.; et al. Linee Guida per la Sorveglianza Sanitaria Degli Addetti ad Attività Lavorativa con Videoterminali. (Linee Guida SIMLII); Nuova Editrice Berti S.r.l.: Parma, Italy, 2013; ISBN 9788873646129. [Google Scholar]
- Piccoli, B.; Battevi, N.; Coggiola, M.; Colais, L.; D’orso, M.I.; Di Bari, A.; Di Bisceglie, M.; Grosso, D.; Leka, I.; Muzi, G.; et al. Funzione Visiva ed uso Occupazionale di Videoterminali: Orientamenti ed Indicazioni Pratico-Applicative per l’attività Professionale del Medico del Lavoro e del Medico Competente. Strumenti di Orientamento e Aggiornamento in Medicina del Lavoro; Documento di Orientamento Professionale per i Medici del Lavoro; Società Italiana di Medicina del Lavoro: Vicenza, Italy, 2020. [Google Scholar]
- Andrich, D.; Marais, I. A Course in Rasch Measurement Theory: Measuring in the Educational, Social and Health Sciences; Springer: Singapore, 2019. [Google Scholar]
- Wolffsohn, J.S.; Arita, R.; Chalmers, R.; Djalilian, A.; Dogru, M.; Dumbleton, K.; Gupta, P.K.; Karpecki, P.; Lazreg, S.; Pult, H.; et al. TFOS DEWS II Diagnostic Methodology report. Ocul. Surf. 2017, 15, 539–574. [Google Scholar] [CrossRef]
- Perneger, T.V.; Courvoisier, D.S.; Hudelson, P.M.; Gayet-Ageron, A. Sample size for pre-tests of questionnaires. Qual. Life Res. 2014, 24, 147–151. [Google Scholar] [CrossRef] [Green Version]
- Wright, B.D.; Linacre, J.M. Reasonable mean-square fit values. Rasch Meas. Trans. 1994, 8, 370–371. [Google Scholar]
- Linacre, J.M. A User’s Guide to WINSTEPS/MINISTEP Rasch-Model Computer Programs; Program Manual 4.5.3; John M. Linacre: Chicago, IL, USA, 2020; ISBN 0-941938-03. [Google Scholar]
- Woodburn, J.; Turner, D.E.; Rosenbaum, D.; Balint, G.; Korda, J.; Ormos, G.; Szabo, A.; Vlieland, T.V.; Van Der Leeden, M.; Steultjens, M.P.M. Adaptation and cross-cultural validation of the foot impact scale for rheumatoid arthritis (FIS-RA) using Rasch analysis. Arthritis Care Res. 2012, 64, 986–992. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.M.; de Boer, M.R.; van der Windt, D.A.W.M.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C.W. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [Green Version]
- Tennant, A.; Pallant, J.F. DIF matters: A practical approach to test if differential item functioning makes a difference. Rasch Meas. Trans. 2007, 20, 1082–1084. [Google Scholar]
- Prinsen, C.A.C.; Mokkink, L.B.; Bouter, L.M.; Alonso, J.; Patrick, D.L.; De Vet, H.C.W.; Terwee, C.B. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual. Life Res. 2018, 27, 1147–1157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, W.-H.; Lenderking, W.; Jin, Y.; Wyrwich, K.W.; Gelhorn, H.; Revicki, D.A. Is Rasch model analysis applicable in small sample size pilot studies for assessing item characteristics? An example using PROMIS pain behavior item bank data. Qual. Life Res. 2013, 23, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Andrich, D. Rasch Models for Measurement; SAGE Publications: Newbury Park, CA, USA, 1988. [Google Scholar]
- Doruk, C.; Celik, M.; Kara, H.; Polat, B.; Guldiken, Y.; Orhan, K.S. Turkish Translation and Validation of Chronic Otitis Media Questionnaire-12. Turk. Arch. Otorhinolaryngol. 2019, 57, 24–29. [Google Scholar] [CrossRef] [PubMed]
- McAlinden, C.; Pesudovs, K.; Moore, J.E. The Development of an Instrument to Measure Quality of Vision: The Quality of Vision (QoV) Questionnaire. Investig. Ophthalmol. Vis. Sci. 2010, 51, 5537–5545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reise, S.P.; Waller, N.G. Item Response Theory and Clinical Measurement. Annu. Rev. Clin. Psychol. 2009, 5, 27–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolffsohn, J.S.; Leteneux-Pantais, C.; Chiva-Razavi, S.; Bentley, S.; Johnson, C.; Findley, A.; Tolley, C.; Arbuckle, R.; Kommineni, J.; Tyagi, N. Social Media Listening to Understand the Lived Experience of Presbyopia: Systematic Search and Content Analysis Study. J. Med. Internet Res. 2020, 22, e18306. [Google Scholar] [CrossRef] [PubMed]
- Grzybowski, A.; Markeviciute, A.; Zemaitiene, R. A Review of Pharmacological Presbyopia Treatment. Asia-Pac. J. Ophthalmol. 2020, 9, 226–233. [Google Scholar] [CrossRef]
- Cantó-Cerdán, M.; Cacho-Martínez, P.; Lara-Lacárcel, F.; García-Muñoz, Á. Rasch analysis for development and reduction of Symptom Questionnaire for Visual Dysfunctions (SQVD). Sci. Rep. 2021, 11, 14855. [Google Scholar] [CrossRef]
- Gómez-Benito, J.; Sireci, S.; Padilla, J.-L. Differential Item Functioning: Beyond validity evidence based on internal structure. Psicothema 2018, 30, 104–109. [Google Scholar]
- Raczek, A.E.; Ware, J.E.; Bjorner, J.B.; Gandek, B.; Haley, S.M.; Aaronson, N.K.; Apolone, G.; Bech, P.; Brazier, J.E.; Bullinger, M.; et al. Comparison of Rasch and Summated Rating Scales Constructed from SF-36 Physical Functioning Items in Seven Countries: Results from the IQOLA Project. Int. Qual. Life Assess. J. Clin. Epidemiol. 1998, 51, 1203–1214. [Google Scholar] [CrossRef]

| Reason for Exclusion | N |
|---|---|
| Daily use of contact lenses | 6 |
| Prior refractive surgery | 8 |
| Prior cataract surgery | 4 |
| Ocular pathology at the time of the study | 20 |
| Ocular pharmacological treatment at the time of the study | 8 |
| Failure to perform the battery of clinical tests | 9 |
| Total | 55 |
| N | % | |
|---|---|---|
| Total | 241 | 100 |
| Gender | ||
| Female | 155 | 64.3 |
| Male | 86 | 35.7 |
| Age (years) | ||
| ≤35 | 52 | 21.6 |
| 36–45 | 55 | 22.8 |
| ≥46 | 134 | 55.6 |
| Occupational use of digital devices (hours/week) | ||
| <20 | 17 | 7.0 |
| ≥20 | 224 | 93.0 |
| Years working with digital devices | ||
| ≤10 | 74 | 30.7 |
| 11–20 | 94 | 39.0 |
| ≥21 | 73 | 30.3 |
| Scheduled breaks during work with digital devices | ||
| No | 34 | 14.1 |
| Yes | 207 | 85.9 |
| Use of digital devices to leisure (hours/day) | ||
| <2 | 130 | 53.9 |
| ≥2 | 111 | 46.1 |
| Total use of digital devices (hours/day) | ||
| ≤4 | 9 | 3.7 |
| 5–8 | 156 | 64.7 |
| >8 | 76 | 31.6 |
| Item Description | Severity | SE | Infit MNSQ | Outfit MNSQ | Gender DIF Contrast | Age DIF Contrast | Version DIF Contrast |
|---|---|---|---|---|---|---|---|
| 1. Burning | −0.61 | 0.13 | 0.73 | 0.70 | 0.12 | 0.10 | * 1.30 |
| 2. Itching | −0.24 | 0.14 | 0.93 | 0.94 | 0.76 | 0.00 | * 1.31 |
| 3. Feeling of a foreign body | 0.60 | 0.15 | 0.93 | 0.86 | 0.26 | 0.29 | 0.52 |
| 4. Tearing | 0.06 | 0.14 | 1.10 | 1.10 | 0.29 | 0.16 | 0.25 |
| 5. Excessive blinking | 0.79 | 0.16 | 0.95 | 0.94 | 0.47 | 0.36 | 0.19 |
| 6. Eye redness | −0.15 | 0.14 | 1.00 | 1.06 | 0.90 | 0.29 | 0.67 |
| 7. Eye pain | 1.99 | 0.21 | 1.03 | 0.82 | 0.10 | 0.49 | * 1.35 |
| 8. Heavy eyelids | −0.49 | 0.13 | 0.99 | 1.01 | 0.18 | 0.68 | 0.72 |
| 9. Dryness | −0.33 | 0.13 | 1.14 | 1.05 | 0.73 | 0.15 | 0.08 |
| 10. Blurred vision | −1.07 | 0.13 | 0.87 | 0.87 | 0.03 | 0.18 | 0.31 |
| 11. Double vision | 1.38 | 0.18 | 1.02 | 0.86 | 0.25 | 0.05 | * 1.41 |
| 12. Difficulty focusing for near vision | −0.72 | 0.13 | 1.14 | 1.19 | 0.20 | * 1.58 | 0.19 |
| 13. Increased sensitivity to light | −0.78 | 0.13 | 1.25 | 1.23 | 0.62 | 0.15 | 0.47 |
| 14. Coloured halos around objects | 1.51 | 0.19 | 0.91 | 0.76 | 0.29 | 0.13 | 0.39 |
| 15. Feeling that sight is worsening | −1.09 | 0.13 | 0.84 | 0.81 | 0.36 | 0.51 | 0.20 |
| 16. Headache | −0.85 | 0.13 | 1.18 | 1.23 | 0.32 | 0.61 | 0.45 |
| Raw Score | Rasch Score (Logits) | Raw Score | Rasch Score (Logits) |
|---|---|---|---|
| 0 | −6.05 E | 17 | 0.24 |
| 1 | −4.78 | 18 | 0.47 |
| 2 | −4.00 | 19 | 0.70 |
| 3 | −3.50 | 20 | 0.93 |
| 4 | −3.11 | 21 | 1.16 |
| 5 | −2.78 | 22 | 1.39 |
| 6 | −2.48 | 23 | 1.63 |
| 7 | −2.20 | 24 | 1.88 |
| 8 | −1.94 | 25 | 2.15 |
| 9 | −1.69 | 26 | 2.43 |
| 10 | −1.44 | 27 | 2.75 |
| 11 | −1.19 | 28 | 3.11 |
| 12 | −0.94 | 29 | 3.53 |
| 13 | −0.70 | 30 | 4.07 |
| 14 | −0.46 | 31 | 4.90 |
| 15 | −0.22 | 32 | 6.20 E |
| 16 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cantó-Sancho, N.; Ronda, E.; Cabrero-García, J.; Casati, S.; Carta, A.; Porru, S.; Seguí-Crespo, M. Rasch-Validated Italian Scale for Diagnosing Digital Eye Strain: The Computer Vision Syndrome Questionnaire IT©. Int. J. Environ. Res. Public Health 2022, 19, 4506. https://doi.org/10.3390/ijerph19084506
Cantó-Sancho N, Ronda E, Cabrero-García J, Casati S, Carta A, Porru S, Seguí-Crespo M. Rasch-Validated Italian Scale for Diagnosing Digital Eye Strain: The Computer Vision Syndrome Questionnaire IT©. International Journal of Environmental Research and Public Health. 2022; 19(8):4506. https://doi.org/10.3390/ijerph19084506
Chicago/Turabian StyleCantó-Sancho, Natalia, Elena Ronda, Julio Cabrero-García, Stefano Casati, Angela Carta, Stefano Porru, and Mar Seguí-Crespo. 2022. "Rasch-Validated Italian Scale for Diagnosing Digital Eye Strain: The Computer Vision Syndrome Questionnaire IT©" International Journal of Environmental Research and Public Health 19, no. 8: 4506. https://doi.org/10.3390/ijerph19084506
APA StyleCantó-Sancho, N., Ronda, E., Cabrero-García, J., Casati, S., Carta, A., Porru, S., & Seguí-Crespo, M. (2022). Rasch-Validated Italian Scale for Diagnosing Digital Eye Strain: The Computer Vision Syndrome Questionnaire IT©. International Journal of Environmental Research and Public Health, 19(8), 4506. https://doi.org/10.3390/ijerph19084506








