Contextualizing the Chronic Care Model among Non-Hispanic Black and Hispanic Men with Chronic Conditions
Abstract
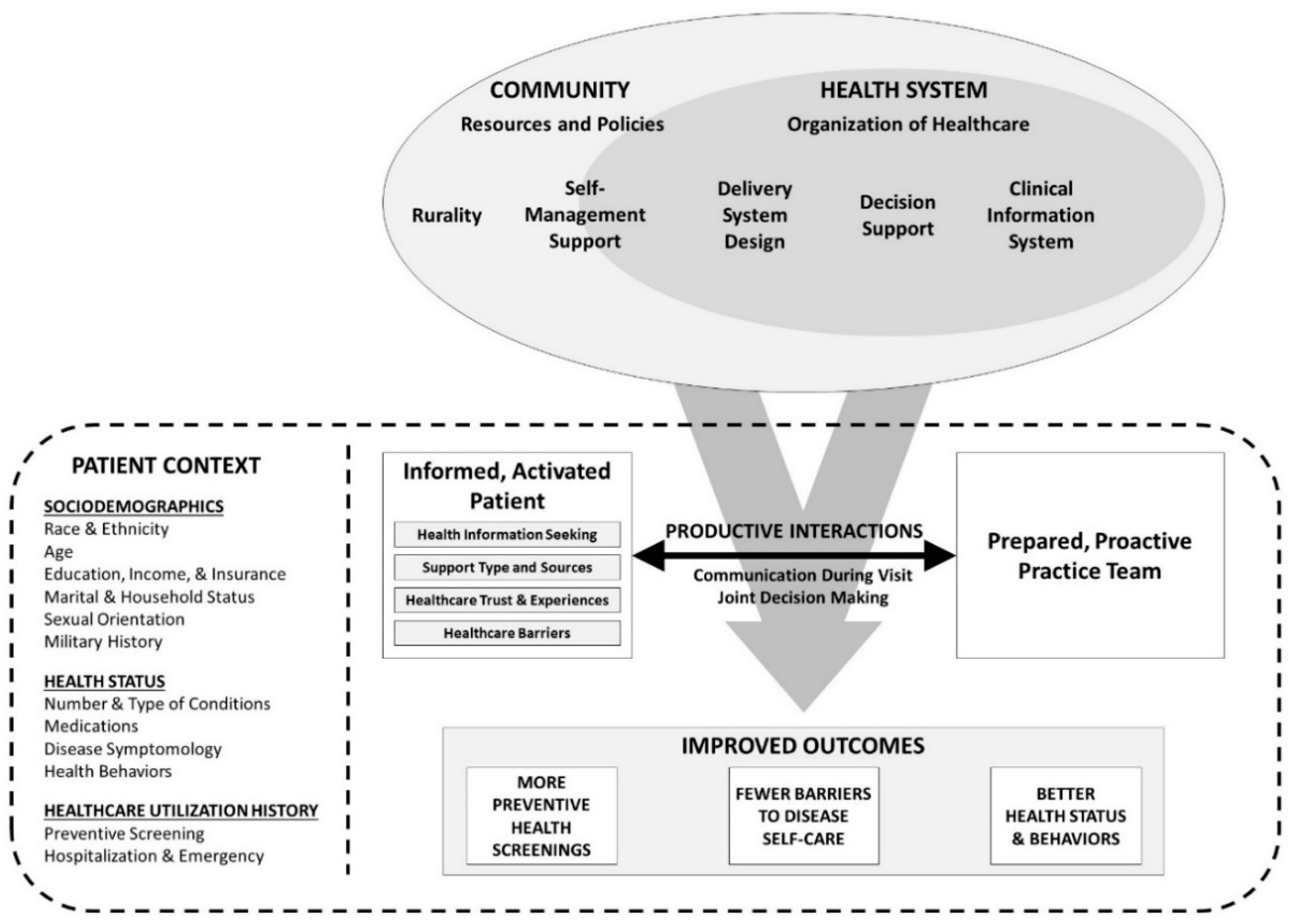
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Measures
2.2.1. Patient Context—Sociodemographics
2.2.2. Patient Context—Health Status
2.2.3. Patient Context—Healthcare Utilization
2.2.4. Informed, Activated Patient
2.2.5. Healthcare Barriers
2.2.6. Productive Interactions
2.3. Statistical Analyses
3. Results
3.1. Patient Context—Sociodemographics
3.2. Patient Context—Health Status
3.3. Patient Context—Healthcare Utilization
3.4. Informed, Activated Patient
3.5. Healthcare Barriers
3.6. Productive Interactions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. About Chronic Diseases. 2019. Available online: https://www.cdc.gov/chronicdisease/about/index.htm#:~:text=Chronic%20diseases%20are%20defined%20broadly,disability%20in%20the%20United%20States (accessed on 3 September 2020).
- Atella, V.; Piano Mortari, A.; Kopinska, J.; Belotti, F.; Lapi, F.; Cricelli, C.; Fontana, L. Trends in age-related disease burden and healthcare utilization. Aging Cell 2019, 18, e12861. [Google Scholar] [CrossRef] [PubMed]
- Furman, D.; Campisi, J.; Verdin, E.; Carrera-Bastos, P.; Targ, S.; Franceschi, C.; Ferrucci, L.; Gilroy, D.W.; Fasano, A.; Miller, G.W.; et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Office of Minority Health, U.S. Department of Health and Human Services. Diabetes and African Americans. 2019. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=18 (accessed on 3 September 2020).
- Office of Minority Health, U.S. Department of Health and Human Services. Chronic Liver Disease and Hispanic Americans. 2020. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=62 (accessed on 3 September 2020).
- Dunlop, D.D.; Manheim, L.M.; Song, J.; Chang, R.W. Gender and ethnic/racial disparities in health care utilization among older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2002, 57, S221–S233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thorpe, J.R.J.; Wilson-Frederick, S.M.; Bowie, J.V.; Coa, K.; Clay, O.; LaVeist, T.A.; Whitfield, K.E. Health behaviors and all-cause mortality in African American men. Am. J. Mens. Health 2013, 7 (Suppl. 4), 8S–18S. [Google Scholar] [CrossRef] [PubMed]
- Laditka, J.N.; Laditka, S.B. Race, ethnicity and hospitalization for six chronic ambulatory care sensitive conditions in the USA. Ethn. Health 2006, 11, 247–263. [Google Scholar] [CrossRef] [PubMed]
- Epping-Jordan, J.E. Improving the quality of health care for chronic conditions. Qual. Saf. Health Care 2004, 13, 299–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Innovative Care for Chronic Conditions: Building Blocks for Action; World Health Organization: Geneva, Switzerland, 2002. Available online: https://www.who.int/chp/knowledge/publications/icccglobalreport.pdf (accessed on 5 March 2022).
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academies Press: Washington, DC, USA, 2001; p. 10027. [Google Scholar] [CrossRef]
- Davy, C.; Bleasel, J.; Liu, H.; Tchan, M.; Ponniah, S.; Brown, A. Effectiveness of chronic care models: Opportunities for improving healthcare practice and health outcomes: A systematic review. BMC Health Serv. Res. 2015, 15, 194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeoh, E.; Wong, M.; Wong, E.L.; Yam, C.; Poon, C.; Chung, R.Y.; Chong, K.C.; Fang, Y.; Wang, H.H.; Liang, M.; et al. Benefits and limitations of implementing Chronic Care Model (CCM) in primary care programs: A systematic review. Int. J. Cardiol. 2018, 258, 279–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bodenheimer, T. Improving primary care for patients with chronic illness. JAMA 2002, 288, 1775. [Google Scholar] [CrossRef] [PubMed]
- Rea, H.; Kenealy, T.; Wellingham, J.; Moffitt, A.; Sinclair, G.; McAuley, S.; Goodman, M.; Arcus, K. Chronic care management evolves towards integrated care in Counties Manukau, New Zealand. N. Z. Med. J. 2007, 120, U2489. [Google Scholar]
- Hutchinson, S.L.; Lauckner, H. Recreation and collaboration within the Expanded Chronic Care Model: Working towards social transformation. Health Promot. Int. 2020, 35, 1531–1542. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.S.; Weaver, K.; Kim, B.; Miller, C.; Lew, R.; Stolzmann, K.; Sullivan, J.L.; Riendeau, R.; Connolly, S.; Pitcock, J.; et al. The collaborative chronic care model for mental health conditions: From evidence synthesis to policy impact to scale-up and spread. Med. Care 2019, 57 (Suppl. 3), S221–S227. [Google Scholar] [CrossRef] [PubMed]
- Garland-Baird, L.; Fraser, K. Conceptualization of the chronic care model: Implications for home care case manager practice. Home Healthc. Now 2018, 36, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Bonevski, B.; Randell, M.; Paul, C.; Chapman, K.; Twyman, L.; Bryant, J.; Brozek, I.; Hughes, C. Reaching the hard-to-reach: A systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med. Res. Methodol. 2014, 14, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lehdonvirta, V.; Oksanen, A.; Räsänen, P.; Blank, G. Social media, web, and panel surveys: Using non-probability samples in social and policy research. Policy Internet 2021, 13, 134–155. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. 2020. Available online: https://www.cdc.gov/brfss/index.html (accessed on 6 September 2020).
- The Atlantic Philanthropies. NCOA Issues Call-to-Action for National Chronic Care Reform Based on Survey of Americans with Chronic Conditions. 2009. Available online: https://www.atlanticphilanthropies.org/news/video-ncoa-issues-call-action-national-chronic-care-reform-based-results-comprehensive-survey-a (accessed on 6 September 2020).
- Smith, M.L.; Ory, M.G.; Ahn, S.; Miles, T.P. Factors associated with women’s chronic disease management: Associations of healthcare frustrations, physician support, and self-care needs. J. Aging Res. 2013, 2013, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ory, M.G.; Ahn, S.; Jiang, L.; Smith, M.L.; Ritter, P.L.; Whitelaw, N.; Lorig, K. Successes of a national study of the chronic disease self-management program: Meeting the triple aim of health care reform. Med. Care 2013, 51, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Ory, M.G.; Ahn, S.; Jiang, L.; Lorig, K.; Ritter, P.; Laurent, D.D.; Whitelaw, N.; Smith, M.L. National study of chronic disease self-management: Six-month outcome findings. J. Aging Health 2013, 25, 1258–1274. [Google Scholar] [CrossRef] [PubMed]
- Center for Community Health Development. Regional Health Partnership 17 Health Assessment: Executive Report; School of Rural Public Health: College Station, TX, USA, 2013. [Google Scholar]
- Centers for Disease Control and Prevention. Measuring Healthy Days; CDC: Atlanta, GA, USA, 2000.
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef]
- Spitzer, R.L. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA 1999, 282, 1737. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, M.L.; Bergeron, C.D.; Adler, C.H.; Patel, A.; Ahn, S.; Towne, S.; Bien, M.; Ory, M.G. Factors associated with healthcare-related frustrations among adults with chronic conditions. Patient Educ. Couns. 2017, 100, 1185–1193. [Google Scholar] [CrossRef] [PubMed]
- Schultz, W.M.; Kelli, H.M.; Lisko, J.C.; Varghese, T.; Shen, J.; Sandesara, P.; Quyyumi, A.A.; Taylor, H.A.; Gulati, M.; Harold, J.G.; et al. Socioeconomic status and cardiovascular outcomes: Challenges and interventions. Circulation 2018, 137, 2166–2178. [Google Scholar] [CrossRef] [PubMed]
- Azap, R.A.; Nolan, T.S.; GrayII, D.M.; Lawson, K.; Gregory, J.; CapersIV, Q.; Odei, J.B.; Joseph, J.J. Association of socioeconomic status with ideal cardiovascular health in Black men. JAHA 2021, 10, e020184. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. How to Pay for Vaccines. 2017. Available online: https://www.cdc.gov/vaccines/adults/pay-for-vaccines.html (accessed on 29 January 2022).
- Kangovi, S.; Barg, F.K.; Carter, T.; Long, J.A.; Shannon, R.; Grande, D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff. 2013, 32, 1196–1203. [Google Scholar] [CrossRef] [PubMed]
- Butkus, R.; Rapp, K.; Cooney, T.G.; Engel, L.S.; Health and Public Policy Committee of the American College of Physicians. Envisioning a better U.S. health care system for all: Reducing barriers to care and addressing social determinants of health. Ann. Intern. Med. 2020, 172 (Suppl. 2), S50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Syed, S.T.; Gerber, B.S.; Sharp, L.K. Traveling towards disease: Transportation barriers to health care access. J. Community Health 2013, 38, 976–993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolfe, M.K.; McDonald, N.C.; Holmes, G.M. Transportation barriers to health care in the United States: Findings from the National Health Interview Survey, 1997–2017. Am. J. Public Health 2020, 110, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Sohn, H. Racial and ethnic disparities in health insurance coverage: Dynamics of gaining and losing coverage over the life-course. Popul. Res. Policy Rev. 2017, 36, 181–201. [Google Scholar] [CrossRef] [Green Version]
- Sherman, L.D.; Goidel, K.; Bergeron, C.D.; Smith, M.L. Web-based health information seeking among African American and Hispanic men living with chronic conditions: Cross-sectional survey study. J. Med. Internet Res. 2021, 23, e26180. [Google Scholar] [CrossRef] [PubMed]
- Madrigal, L.; Escoffery, C. Electronic health behaviors among US adults with chronic disease: Cross-sectional survey. J. Med. Internet Res. 2019, 21, e11240. [Google Scholar] [CrossRef] [PubMed]
- Gordon, N.P.; Crouch, E. Digital information technology use and patient preferences for internet-based health education modalities: Cross-sectional survey study of middle-aged and older adults with chronic health conditions. JMIR Aging 2019, 2, e12243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, M.L.; Bergeron, C.D.; Riggle, S.D.; Meng, L.; Towne, S.; Ahn, S.; Ory, M.G. Self-care difficulties and reliance on support among vulnerable middle-aged and older adults with chronic conditions: A cross-sectional study. Maturitas 2017, 104, 1–10. [Google Scholar] [CrossRef]
- Smith, M.L.; Bergeron, C.D.; Ahn, S.; Towne, S.D.; Mingo, C.A.; Robinson, K.T.; Mathis, J.; Meng, L.; Ory, M.G. Engaging the underrepresented sex: Male participation in chronic disease self-management education (CDSME) programs. Am. J. Mens. Health 2018, 12, 935–943. [Google Scholar] [CrossRef] [PubMed]
- Campione, J.R.; Zebrak, K.A. Predictors of unmet need among informal caregivers. J. Gerontol. Ser. B 2020, 75, 2181–2192. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Caregiving for Family and Friends—A Public Health Issue. 2019. Available online: https://www.cdc.gov/aging/caregiving/caregiver-brief.html#:~:text=Caregivers%20are%20at%20increased%20risk,while%20providing%20care%20to%20others (accessed on 5 September 2020).
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015, 38, 843–844. [Google Scholar] [CrossRef]
- Creamer, M.R.; Wang, T.W.; Babb, S.; Cullen, K.A.; Day, H.; Willis, G.; Jamal, A.; Neff, L. Tobacco product use and cessation indicators among adults—United States, 2018. Morb. Mortal. Wkly. Rep. 2019, 68, 1013–1019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suvarna, B.; Suvarna, A.; Phillips, R.; Juster, R.P.; McDermott, B.; Sarnyai, Z. Health risk behaviours and allostatic load: A systematic review. Neurosci. Biobehav. Rev. 2020, 108, 694–711. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J.L.; Senn, T.E.; Carey, M.P. Longitudinal associations between health behaviors and mental health in low-income adults. Transl. Behav. Med. 2013, 3, 104–113. [Google Scholar] [CrossRef]
- Quinones, A.R.; Liang, J.; Bennett, J.M.; Xu, X.; Ye, W. How does the trajectory of multimorbidity vary across Black, White, and Mexican Americans in middle and old age? J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2011, 66B, 739–749. [Google Scholar] [CrossRef]
- Smith, M.L.; Wilson, M.G.; Robertson, M.M.; Padilla, H.M.; Zuercher, H.; Vandenberg, R.; Corso, P.; Lorig, K.; Laurent, D.D.; DeJoy, D.M. Impact of a translated disease self-management program on employee health and productivity: Six-month findings from a randomized controlled trial. Int. J. Environ. Res. Public Health 2018, 15, 851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, M.G.; DeJoy, D.M.; Vandenberg, R.J.; Padilla, H.M.; Haynes, N.J.; Zuercher, H.; Corso, P.; Lorig, K.; Smith, M.L. Translating CDSMP to the workplace: Results of the Live Healthy Work Healthy Program. Am. J. Health Promot. 2021, 35, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. REACH: CDC’s Racial and Ethnic Approaches to Community Health Program. 2020. Available online: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/reach.htm (accessed on 5 September 2020).
- Garcia, D.O.; Valdez, L.A.; Aceves, B.; Bell, M.; Humphrey, K.; Hingle, M.; McEwen, M.; Hooker, S. A gender- and culturally sensitive weight loss intervention for Hispanic men: Results from the Animo pilot randomized controlled trial. Health Educ. Behav. 2019, 46, 763–772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelly, J.T.; Reidlinger, D.P.; Hoffmann, T.C.; Campbell, K.L. Telehealth methods to deliver dietary interventions in adults with chronic disease: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2016, 104, 1693–1702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sattin, R.W.; Williams, L.B.; Dias, J.K.; Garvin, J.; Marion, L.; Joshua, T.V.; Kriska, A.; Kramer, M.K.; Narayan, K.M.V. Community trial of a faith-based lifestyle intervention to prevent diabetes among African-Americans. J. Community Health 2016, 41, 87–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, M.L.; Towne, S.D.; Herrera-Venson, A.; Cameron, K.; Kulinski, K.P.; Lorig, K.; Horel, S.A.; Ory, M.G. Dissemination of Chronic Disease Self-Management Education (CDSME) programs in the United States: Intervention delivery by rurality. Int. J. Environ. Res. Public Health 2017, 14, 638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitley, M.D.; Payán, D.D.; Flórez, K.; Williams, M.V.; Wong, E.C.; A Branch, C.; Derose, K.P. Feasibility and acceptability of a mobile messaging program within a church-based healthy living intervention for African Americans and Latinos. Health Inform. J. 2020, 26, 880–896. [Google Scholar] [CrossRef] [PubMed]
| Total | Non-Hispanic Black | Hispanic | |||||
|---|---|---|---|---|---|---|---|
| (n = 2028) | Age 40–64 (n = 933) | Age ≥ 65 (n = 267) | Age 40–64 (n = 625) | Age ≥ 65 (n = 203) | V or f | p | |
| Age | 56.54 (±10.03) | 52.98 (±7.23) | 69.90 (±4.36) | 51.60 (±7.24) | 70.26 (±4.71) | 837.80 a | <0.0001 |
| Education | 0.131 | <0.0001 | |||||
| ≤High School Graduate | 20.3% | 23.6% | 18.0% | 19.5% | 10.8% | ||
| Some College or 2-Year Degree | 42.4% | 46.3% | 42.7% | 40.6% | 29.1% | ||
| ≥4-Year Degree | 37.3% | 30.1% | 39.3% | 39.8% | 60.1% | ||
| Marital Status | 0.176 | <0.0001 | |||||
| Married or Partnered | 52.2% | 42.1% | 55.1% | 59.0% | 73.4% | ||
| Never Married | 25.0% | 35.8% | 10.9% | 21.6% | 4.9% | ||
| Divorced or Separated | 18.9% | 19.5% | 23.2% | 17.0% | 16.7% | ||
| Widowed | 3.8% | 2.6% | 10.9% | 2.4% | 4.9% | ||
| Persons Living in Household (including Self) | 2.62 (±1.64) | 2.64 (±1.76) | 2.06 (±1.29) | 2.95 (±1.67) | 2.17 (±0.94) | 24.57 b | <0.0001 |
| Sexual Orientation | 0.069 | 0.001 | |||||
| Straight or Heterosexual | 89.9% | 90.7% | 96.6% | 85.9% | 90.1% | ||
| Gay or Homosexual | 6.2% | 6.3% | 2.2% | 7.8% | 5.9% | ||
| Bisexual | 3.2% | 2.5% | 1.1% | 5.0% | 3.4% | ||
| Identify in Some Other Way | 0.7% | 0.5% | 0.0% | 1.3% | 0.5% | ||
| Annual Household Income | 0.123 | <0.0001 | |||||
| Less than $10,000 | 5.9% | 7.2% | 2.2% | 7.0% | 1.0% | ||
| $10,000 to $19,999 | 10.6% | 12.3% | 11.6% | 7.7% | 9.9% | ||
| $20,000 to $29,999 | 12.9% | 14.0% | 12.7% | 12.0% | 10.3% | ||
| $30,000 to $39,999 | 10.9% | 12.1% | 14.6% | 9.1% | 5.9% | ||
| $40,000 to $49,999 | 9.3% | 9.4% | 9.7% | 9.3% | 8.4% | ||
| $50,000 to $59,999 | 10.7% | 11.5% | 7.5% | 10.9% | 11.3% | ||
| $60,000 to $69,999 | 6.3% | 5.8% | 7.9% | 6.4% | 6.4% | ||
| $70,000 to $79,999 | 7.5% | 7.5% | 8.6% | 6.4% | 9.4% | ||
| $80,000 to $89,999 | 3.6% | 3.1% | 2.6% | 4.5% | 4.4% | ||
| $90,000 to $99,999 | 3.8% | 2.1% | 3.4% | 5.9% | 5.9% | ||
| $100,000 to $149,999 | 11.5% | 9.9% | 12.7% | 13.0% | 12.8% | ||
| $150,000 or More | 7.0% | 5.0% | 6.4% | 7.8% | 14.3% | ||
| Insurance Coverage | 0.132 | <0.0001 | |||||
| No/Don’t Know | 11.0% | 12.6% | 4.1% | 14.2% | 3.0% | ||
| Yes | 89.0% | 87.4% | 95.9% | 85.8% | 97.0% | ||
| Past/Current Service in U.S. Armed Services | 0.185 | <0.0001 | |||||
| No | 70.4% | 71.3% | 53.2% | 79.2% | 61.6% | ||
| Yes | 29.6% | 28.7% | 46.8% | 20.8% | 38.4% | ||
| Rurality | 0.066 | 0.033 | |||||
| Metro | 93.7% | 92.1% | 95.5% | 94.7% | 96.1% | ||
| Non-Metro | 6.3% | 7.9% | 4.5% | 5.3% | 3.9% | ||
| Total | Non-Hispanic Black | Hispanic | |||||
|---|---|---|---|---|---|---|---|
| (n = 2028) | Age 40–64 (n = 933) | Age ≥ 65 (n = 267) | Age 40–64 (n = 625) | Age ≥ 65 (n = 203) | V or f | p | |
| Chronic Conditions | 4.01 (±2.98) | 4.04 (±3.06) | 3.93 (±2.50) | 3.96 (±3.10) | 4.09 (±2.81) | 0.210 | 0.890 |
| Asthma/Emphysema/Chronic Breathing or Lung Problem | 18.8% | 20.5% | 15.0% | 20.3% | 11.8% | 0.076 | 0.009 |
| Arthritis/Rheumatic Disease | 30.0% | 32.2% | 28.1% | 26.6% | 33.0% | 0.058 | 0.074 |
| Cancer or Cancer Survivor | 14.4% | 13.1% | 29.2% | 9.3% | 17.2% | 0.177 | <0.0001 |
| Chronic Pain | 36.8% | 40.0% | 29.6% | 38.1% | 28.1% | 0.092 | 0.001 |
| Depression or Anxiety | 31.9% | 33.8% | 18.0% | 38.4% | 21.7% | 0.153 | <0.0001 |
| Diabetes | 37.9% | 35.3% | 42.3% | 37.1% | 46.8% | 0.077 | 0.008 |
| Heart Disease | 13.0% | 11.1% | 12.0% | 13.4% | 21.2% | 0.087 | 0.002 |
| High Cholesterol | 45.4% | 42.2% | 53.9% | 44.2% | 52.7% | 0.090 | 0.001 |
| Hypertension (High Blood Pressure) | 55.9% | 56.6% | 73.8% | 45.0% | 62.6% | 0.184 | <0.0001 |
| Kidney Disease | 8.1% | 9.0% | 7.1% | 7.0% | 8.4% | 0.034 | 0.506 |
| Memory Problem (e.g., dementia, Alzheimer’s disease) | 5.8% | 5.7% | 4.1% | 6.7% | 5.9% | 0.034 | 0.500 |
| Obesity | 23.5% | 24.5% | 15.0% | 26.4% | 21.2% | 0.086 | 0.002 |
| Osteoporosis (Low Bone Density) | 6.6% | 8.4% | 2.6% | 6.4% | 4.4% | 0.080 | 0.004 |
| Obstructive Sleep Apnea (snoring or trouble breathing when sleeping) | 22.9% | 22.6% | 15.0% | 25.8% | 25.6% | 0.081 | 0.004 |
| Schizophrenia or Other Psychotic Disorder | 6.6% | 8.1% | 4.1% | 6.4% | 3.4% | 0.069 | 0.022 |
| Stroke | 7.1% | 8.0% | 6.0% | 6.9% | 4.9% | 0.040 | 0.356 |
| Thyroid Problem (e.g., Hyperthyroidism, Hypothyroidism) | 8.9% | 6.9% | 8.2% | 10.9% | 12.8% | 0.076 | 0.008 |
| Urinary Incontinence | 9.8% | 9.2% | 13.9% | 8.3% | 11.8% | 0.062 | 0.050 |
| Other Chronic Condition | 17.1% | 17.0% | 15.0% | 18.7% | 15.3% | 0.035 | 0.478 |
| Number of Medications Taken Daily (0 to ≥6) | 3.39 (±2.02) | 3.23 (±2.05) | 4.22 (±1.76) | 3.04 (±1.97) | 4.14 (±1.85) | 34.19 b | <0.0001 |
| General Health Status (1 = poor; 5 = excellent) | 2.84 (±0.89) | 2.80 (±0.90) | 2.88 (±0.79) | 2.82 (0.90±) | 3.02 (±0.89) | 3.75 | 0.011 |
| Disease Symptoms | |||||||
| Fatigue (0 to 10) | 3.59 (±3.29) | 3.71 (±3.30) | 2.51 (±3.02) | 4.21 (±3.32) | 2.51 (±2.85) | 25.70 a | <0.0001 |
| Pain (0 to 10) | 4.10 (±3.33) | 4.24 (±3.35) | 3.18 (±3.23) | 4.62 (±3.33) | 3.00 (±2.89) | 20.55 b | <0.0001 |
| Shortness of Breath (0 to 10) | 2.30 (±2.99) | 2.35 (±3.05) | 2.04 (±2.87) | 2.63 (±3.10) | 1.37 (±2.26) | 9.93 b | <0.0001 |
| Stress (0 to 10) | 3.69 (±3.35) | 4.06 (±3.41) | 1.96 (±2.60) | 4.40 (±3.30) | 2.08 (±2.77) | 56.69 a | <0.0001 |
| Sleep Problem (0 to 10) | 3.95 (±3.36) | 4.13 (±3.34) | 2.52 (±3.01) | 4.69 (±3.34) | 2.73 (±3.01) | 38.13 a | <0.0001 |
| Depressive Symptomatology | 0.212 | <0.0001 | |||||
| No | 68.1% | 66.2% | 82.0% | 61.6% | 78.3% | ||
| Yes | 31.9% | 33.8% | 18.0% | 38.4% | 21.7% | ||
| Behavior | |||||||
| Average Hours of Sleep in 24 Hour Period | 6.62 (±1.73) | 6.49 (±1.85) | 6.97 (±1.86) | 6.48 (±1.57) | 7.18 (±1.27) | 14.25 a | <0.0001 |
| Total Minutes of Physical Activity (past week) | 147.21 (±170.27) | 133.34 (±164.60) | 145.32 (±152.91) | 160.16 (±172.91) | 171.21 (±197.91) | 3.28 | 0.020 |
| Weekly Alcoholic Beverage Consumption | 61.4% | 64.0% | 54.7% | 60.5% | 61.6% | 0.063 | 0.047 |
| Tobacco Use in Past 30 Days | 35.2% | 42.3% | 29.2% | 34.6% | 11.8% | 0.191 | <0.0001 |
| Cannabis Use in Past 30 Days | 21.7% | 26.8% | 13.1% | 21.9% | 9.4% | 0.147 | <0.0001 |
| Total | Non-Hispanic Black | Hispanic | |||||
|---|---|---|---|---|---|---|---|
| (n = 2028) | Age 40–64 (n = 933) | Age ≥ 65 (n = 267) | Age 40–64 (n = 625) | Age ≥ 65 (n = 203) | V or f | p | |
| Preventive Screening | |||||||
| Flu Vaccine in Past Year | 41.4% | 41.3% | 49.4% | 35.8% | 48.8% | 0.098 | 0.0002 |
| Tetanus Shot in Past 10 Years | 58.0% | 54.7% | 64.0% | 58.9% | 63.1% | 0.072 | 0.014 |
| Blood Cholesterol Test Past Year | 75.8% | 74.4% | 83.1% | 70.1% | 90.6% | 0.148 | <0.0001 |
| Blood Pressure Test Past Year | 87.4% | 86.3% | 96.3% | 82.1% | 97.0% | 0.162 | <0.0001 |
| Colon Cancer Test Past Year | 31.0% | 32.7% | 39.0% | 24.6% | 32.5% | 0.102 | <0.0001 |
| Blood Sugar Test Past Year | 71.4% | 70.2% | 77.5% | 66.6% | 84.2% | 0.120 | <0.0001 |
| Eye Exam Past Year | 58.0% | 54.0% | 66.3% | 55.4% | 73.9% | 0.134 | <0.0001 |
| Dental Exam Test Past Year | 54.4% | 50.2% | 59.9% | 54.6% | 66.5% | 0.104 | <0.0001 |
| Prostate-Specific Antigen (PSA) Test in Lifetime | 54.7% | 49.7% | 80.9% | 42.9% | 79.8% | 0.290 | <0.0001 |
| Sigmoidoscopy or Colonoscopy in Lifetime | 56.7% | 52.7% | 81.3% | 44.0% | 81.3% | 0.283 | <0.0001 |
| Routine Check-Up with Physician in Past Year | 84.6% | 84.9% | 92.9% | 78.4% | 91.6% | 0.141 | <0.0001 |
| Ever Attend Program to Prevent or Manage Chronic Illness in Past Year | 17.9% | 20.2% | 15.4% | 17.4% | 12.8% | 0.063 | 0.045 |
| Overnight Hospital Stay in Past Year | 0.092 | 0.0007 | |||||
| No | 72.2% | 69.8% | 77.2% | 70.6% | 82.3% | ||
| Yes | 27.8% | 30.2% | 22.8% | 29.4% | 17.7% | ||
| Emergency Room Visit in Past Year | 0.124 | <0.0001 | |||||
| No | 55.6% | 51.4% | 61.4% | 54.1% | 71.4% | ||
| Yes | 44.4% | 48.6% | 38.6% | 45.9% | 28.6% | ||
| Falls in the Past Year | 0.089 | <0.0001 | |||||
| None | 68.8% | 69.3% | 77.9% | 65.3% | 65.0% | ||
| Once | 11.4% | 9.4% | 12.0% | 12.2% | 17.7% | ||
| Twice or More | 19.8% | 21.2% | 10.1% | 22.6% | 17.2% | ||
| Total | Non-Hispanic Black | Hispanic | |||||
|---|---|---|---|---|---|---|---|
| (n = 2028) | Age 40–64 (n = 933) | Age ≥ 65 (n = 267) | Age 40–64 (n = 625) | Age ≥ 65 (n = 203) | V or f | p | |
| INFORMED, ACTIVATED PATIENT | |||||||
| Preferred Method of Getting Reliable Health/Medical Information | 0.082 | 0.0001 | |||||
| Medical Professional | 70.7% | 71.1% | 80.1% | 64.5% | 75.4% | ||
| The Internet | 27.6% | 26.8% | 18.7% | 33.9% | 23.2% | ||
| Some Other Way | 1.8% | 2.1% | 1.1% | 1.6% | 1.5% | ||
| Get the Help/Support Needed to Improve Health and Manage Health Problems | 0.202 | <0.0001 | |||||
| Never/Rarely/Occasionally | 42.9% | 44.7% | 25.5% | 53.1% | 26.6% | ||
| Frequently/Always | 57.1% | 55.3% | 74.5% | 46.9% | 73.4% | ||
| Reliance for Ongoing Help/Support to Improve Health and Manage Health Problems | |||||||
| Co-Workers | 1.47 (±0.93) | 1.50 (±0.97) | 1.18 (±0.64) | 1.62 (±1.01) | 1.21 (±0.56) | 20.65 b | <0.0001 |
| Community Groups or Clubs | 1.52 (±0.99) | 1.57 (±1.05) | 1.37 (±0.79) | 1.62 (±1.05) | 1.17 (±0.50) | 13.50 a | <0.0001 |
| Church, Synagogue, or Other Faith-Based Organizations | 1.77 (±1.15) | 1.85 (±1.22) | 1.67 (±1.10) | 1.80 (±1.16) | 1.41 (±0.79) | 8.82 a | <0.0001 |
| People with Similar Health Problems | 1.78 (±1.06) | 1.83 (±1.11) | 1.60 (±0.90) | 1.85 (±1.11) | 1.57 (±0.80) | 6.95 a | <0.0001 |
| Friends or Relatives | 2.06 (±1.12) | 2.08 (±1.13) | 1.85 (±0.99) | 2.15 (±1.16) | 2.03 (±1.06) | 4.68 | 0.003 |
| Internet | 2.28 (±1.20) | 2.33 (±1.22) | 1.90 (±0.98) | 2.46 (±1.25) | 2.00 (±1.07) | 18.10 b | <0.0001 |
| Spouse or Partner | 2.61 (±1.50) | 2.41 (±1.46) | 2.43 (±1.46) | 2.84 (±1.54) | 3.05 (±1.47) | 17.98 b | <0.0001 |
| Doctors, Nurses, or Other Healthcare Providers | 3.44 (±1.24) | 3.48 (±1.25) | 3.61 (±1.25) | 3.25 (±1.24) | 3.65 (±1.09) | 9.00 a | <0.0001 |
| Healthcare Frustrations (6 to 18, higher = more frustration) | 9.53 (±3.15) | 9.71 (±3.14) | 8.23 (±2.61) | 10.23 (±3.31) | 8.24 (±2.30) | 40.28a | <0.0001 |
| Disease Self-Management Efficacy (10 to 40, higher = more efficacy) | 28.48 (±2.67) | 28.35 (±2.95) | 28.92 (±1.60) | 28.44 (±2.35) | 28.64 (±3.27) | 3.40 | 0.017 |
| HEALTHCARE BARRIERS | |||||||
| Barriers to Self-Care (5 to 20, higher = more barriers) | 11.53 (±3.65) | 11.77 (±3.62) | 10.23 (±3.42) | 12.25 (±3.62) | 9.92 (±3.22) | 35.77 a | <0.0001 |
| Needed Physician in Past Year but Didn’t Go Because of Cost | 0.199 | <0.0001 | |||||
| No | 80.9% | 78.6% | 93.6% | 74.1% | 96.1% | ||
| Yes | 19.1% | 21.4% | 6.4% | 25.9% | 3.9% | ||
| Needed Medications in Past Year but Didn’t Because of Cost | 0.161 | <0.0001 | |||||
| No | 78.7% | 74.8% | 88.0% | 75.3% | 92.8% | ||
| Yes | 21.3% | 25.2% | 12.0% | 24.7% | 7.2% | ||
| Other Than Cost, Delayed Getting Medical Care Because | |||||||
| Couldn’t get through on the telephone | 19.1% | 18.5% | 16.1% | 19.8% | 23.2% | 0.045 | 0.249 |
| Couldn’t get an appointment soon enough | 49.7% | 49.0% | 43.8% | 52.6% | 51.2% | 0.055 | 0.101 |
| Once there, had to wait too long to see the doctor | 21.6% | 20.3% | 20.6% | 23.2% | 24.6% | 0.040 | 0.363 |
| The clinic or doctor’s office wasn’t open when you got there | 7.3% | 7.3% | 6.7% | 7.5% | 7.4% | 0.009 | 0.982 |
| Didn’t have transportation | 19.4% | 21.7% | 19.9% | 20.6% | 4.9% | 0.123 | <0.0001 |
| PRODUCTIVE INTERACTIONS | |||||||
| Communication During Physician Visit (4 to 20, higher = more engagement) | 14.10 (±3.55) | 14.33 (±3.49) | 14.04 (±3.46) | 13.82 (±3.60) | 13.97 (±3.78) | 2.72 | 0.043 |
| Physician Quality Conversation and Joint Decision Making (6 to 30, higher = more quality conversation) | 18.64 (±5.55) | 18.97 (±5.45) | 19.28 (±5.72) | 17.86 (±5.58) | 18.67 (±5.43) | 6.45 b | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, M.L.; Bergeron, C.D.; Sherman, L.D.; Goidel, K.; Merianos, A.L. Contextualizing the Chronic Care Model among Non-Hispanic Black and Hispanic Men with Chronic Conditions. Int. J. Environ. Res. Public Health 2022, 19, 3655. https://doi.org/10.3390/ijerph19063655
Smith ML, Bergeron CD, Sherman LD, Goidel K, Merianos AL. Contextualizing the Chronic Care Model among Non-Hispanic Black and Hispanic Men with Chronic Conditions. International Journal of Environmental Research and Public Health. 2022; 19(6):3655. https://doi.org/10.3390/ijerph19063655
Chicago/Turabian StyleSmith, Matthew Lee, Caroline D. Bergeron, Ledric D. Sherman, Kirby Goidel, and Ashley L. Merianos. 2022. "Contextualizing the Chronic Care Model among Non-Hispanic Black and Hispanic Men with Chronic Conditions" International Journal of Environmental Research and Public Health 19, no. 6: 3655. https://doi.org/10.3390/ijerph19063655
APA StyleSmith, M. L., Bergeron, C. D., Sherman, L. D., Goidel, K., & Merianos, A. L. (2022). Contextualizing the Chronic Care Model among Non-Hispanic Black and Hispanic Men with Chronic Conditions. International Journal of Environmental Research and Public Health, 19(6), 3655. https://doi.org/10.3390/ijerph19063655








