Effects of Sodium Intake on Health and Performance in Endurance and Ultra-Endurance Sports
Abstract
1. Introduction
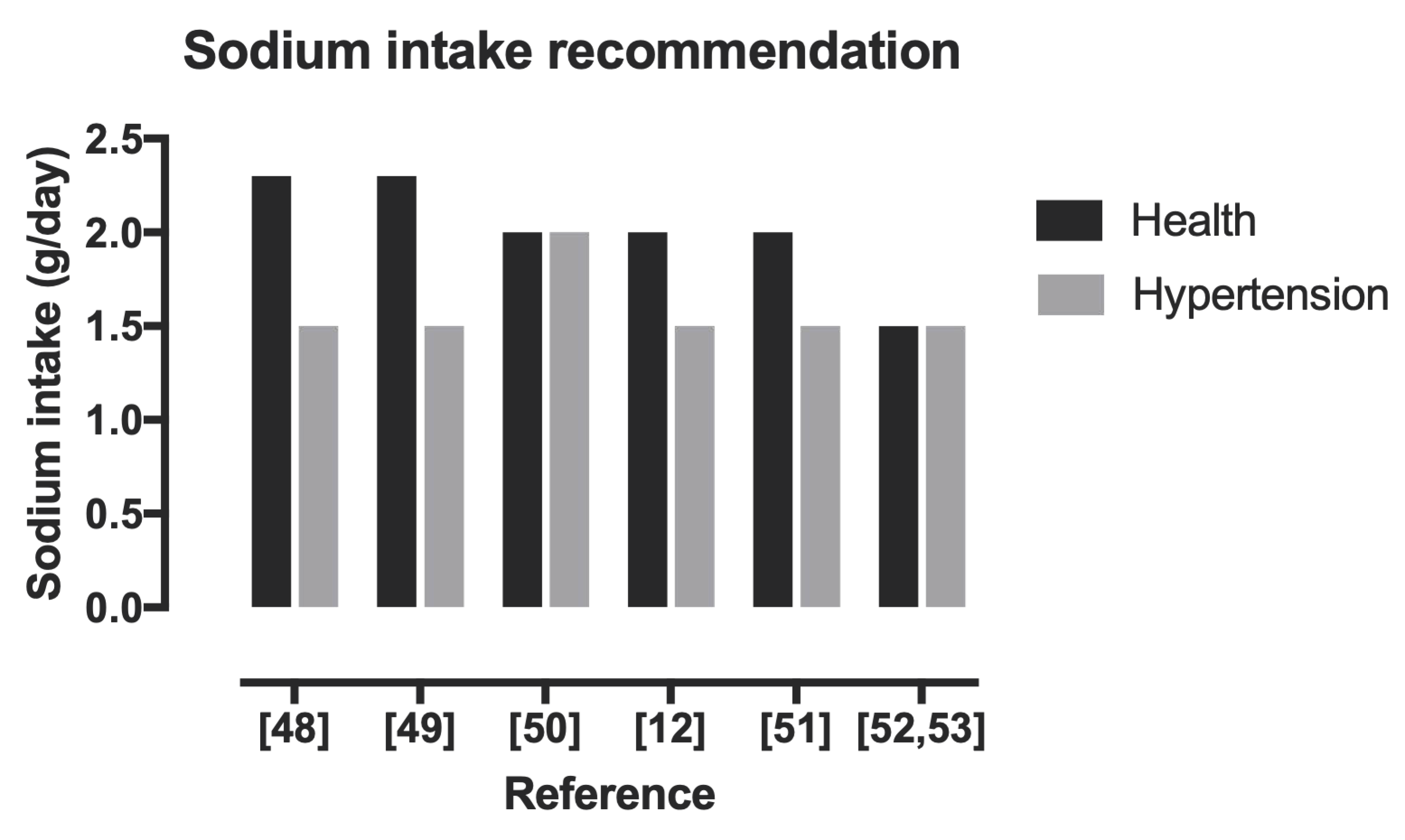
2. Importance of Sodium and Ideal Composition
3. Effects of Sodium Consumption
3.1. Very Low Sodium Consumption
3.2. Very High Sodium Consumption
4. Sodium in Sport
4.1. Exercise-Associated Muscle Cramps
4.2. Exercise-Associated Hyponatremia
Prevention and Treatment
5. Sodium and Hydration
6. Sources and Dosages of Sodium in Endurance–Ultra-Endurance Sports
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stellingwerff, T.; Maughan, R.J.; Burke, L.M. Nutrition for power sports: Middle-distance running, track cycling, rowing, canoeing/kayaking, and swimming. J. Sports Sci. 2011, 29, S79–S89. [Google Scholar] [CrossRef] [PubMed]
- Jeukendrup, A.E. Nutrition for endurance sports: Marathon, triathlon, and road cycling. J. Sports Sci. 2011, 29, 91–99. [Google Scholar] [CrossRef]
- Costa, R.J.S.; Camões-Costa, V.; Snipe, R.M.J.; Dixon, D.; Russo, I.; Huschtscha, Z. The impact of exercise-induced hypohydration on gastrointestinal integrity, function, symptoms, and systemic endotoxin and inflammatory profile. J. Appl. Physiol. 2019, 126, 1281–1291. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B.; Ungaro, C.T.; Barnes, K.A.; Nuccio, R.P.; Reimel, A.J.; Stofan, J.R. Validity and reliability of a field technique for sweat Na+ and K+ analysis during exercise in a hot-humid environment. Physiol. Rep. 2014, 2, e12007. [Google Scholar] [CrossRef] [PubMed]
- Coyle, E.F. Fluid and fuel intake during exercise. J. Sports Sci. 2004, 22, 39–55. [Google Scholar] [CrossRef]
- Shirreffs, S.M.; Sawka, M.N. Fluid and electrolyte needs for training, competition, and recovery. J. Sports Sci. 2011, 29, S39–S46. [Google Scholar] [CrossRef] [PubMed]
- Ganio, M.S.; Armstrong, L.E.; Kavouras, S.A. Hydration. In Sport and Physical Activity in the Heat; Springer: Cham, Switzerland, 2018; pp. 83–100. [Google Scholar]
- Schwellnus, M.P.; Drew, N.; Collins, M. Muscle cramping in athletes—Risk factors, clinical assessment, and management. Clin. Sports Med. 2008, 27, 183–194. [Google Scholar] [CrossRef]
- Knechtle, B.; Chlíbková, D.; Papadopoulou, S.; Mantzorou, M.; Rosemann, T.; Nikolaidis, P.T. Exercise-Associated Hyponatremia in Endurance and Ultra-Endurance Performance–Aspects of Sex, Race Location, Ambient Temperature, Sports Discipline, and Length of Performance: A Narrative Review. Medicina 2019, 55, 537. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Navarro, I.; Montoya-Vieco, A.; Collado-Boira, E.; Hernando, B.; Panizo, N.; Hernando, C. Muscle Cramping in the Marathon: Dehydration and Electrolyte Depletion vs. Muscle Damage. J. Strength Cond. Res. 2020. [Google Scholar] [CrossRef]
- Vitale, K.; Getzin, A. Nutrition and Supplement Update for the Endurance Athlete: Review and Recommendations. Nutrients 2019, 11, 1289. [Google Scholar] [CrossRef] [PubMed]
- Rust, P.; Ekmekcioglu, C. Impact of Salt Intake on the Pathogenesis and Treatment of Hypertension. In Hypertension: From Basic Research to Clinical Practice; Springer: Cham, Switzerland, 2016. [Google Scholar]
- Drüeke, T.B. Salt and health: Time to revisit the recommendations. Kidney Int. 2016, 89, 259–260. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koepsell, H. Glucose transporters in the small intestine in health and disease. Pflüg. Arch. Eur. J. Physiol. 2020, 472, 1207–1248. [Google Scholar] [CrossRef] [PubMed]
- Stolarz-Skrzypek, K.; Bednarski, A.; Czarnecka, D.; Kawecka-Jaszcz, K.; Staessen, J.A. Sodium and Potassium and the Pathogenesis of Hypertension. Curr. Hypertens. Rep. 2013, 15, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Farquhar, W.B.; Edwards, D.G.; Jurkovitz, C.T.; Weintraub, W.S. Dietary Sodium and Health. J. Am. Coll. Cardiol. 2015, 65, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- Mohammadifard, N.; Gotay, C.; Humphries, K.H.; Ignaszewski, A.; Esmaillzadeh, A.; Sarrafzadegan, N. Electrolyte minerals intake and cardiovascular health. Crit. Rev. Food Sci. Nutr. 2018, 59, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Del Coso, J.; González-Millán, C.; Salinero, J.J.; Abián-Vicén, J.; Areces, F.; Lledó, M.; Lara, B.; Gallo-Salazar, C.; Ruiz-Vicente, D. Effects of oral salt supplementation on physical performance during a half-ironman: A randomized controlled trial. Scand. J. Med. Sci. Sports 2015, 26, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Shirreffs, S.M.; Maughan, R.J. Volume repletion following exercise-induced volume depletion in man: Replacement of water and sodium losses. Am. J. Physiol. 1998, 274, F868–F875. [Google Scholar]
- Speedy, D.B.; Thompson, J.; Rodgers, I.; Collins, M.; Sharwood, K. Oral salt supplementation during ultradistance exercise. Clin. J. Sport Med. 2002, 12, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Robinson, A.; Edwards, D.G.; Farquhar, W.B. The Influence of Dietary Salt Beyond Blood Pressure. Curr. Hypertens. Rep. 2019, 21, 42. [Google Scholar] [CrossRef] [PubMed]
- Graudal, N.A.; Hubeck-Graudal, T.; Jurgens, G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst. Rev. 2017, 4, CD004022. [Google Scholar] [CrossRef]
- Mente, A.; O’Donnell, M.; Rangarajan, S.; Dagenais, G.; Lear, S.; McQueen, M.; Diaz, R.; Avezum, A.; Lopez-Jaramillo, P.; Lanas, F.; et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: A pooled analysis of data from four studies. Lancet 2016, 388, 465–475. [Google Scholar] [CrossRef]
- Braam, B.; Huang, X.; Cupples, W.A.; Hamza, S.M. Understanding the Two Faces of Low-Salt Intake. Curr. Hypertens. Rep. 2017, 19, 1777. [Google Scholar] [CrossRef] [PubMed]
- Mente, A.; O’Donnell, M.J.; Rangarajan, S.; McQueen, M.J.; Poirier, P.; Wielgosz, A.; Morrison, H.; Li, W.; Wang, X.; Di, C.; et al. Association of urinary sodium and potassium excretion with blood pressure. N. Engl. J. Med. 2014, 371, 601–611. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.; Lee, H.Y.; Jun, D.W.; Lee, S.M. Low salt diet and insulin resistance. Clin. Nutr. Res. 2016, 5, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Tian, M.; Neal, B. Sodium Reduction: How Big Might the Risks and Benefits Be? Heart Lung Circ. 2020, 30, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Van Horn, L. Dietary sodium and blood pressure: How low should we go? Prog. Cardiovasc. Dis. 2015, 58, 61–68. [Google Scholar] [CrossRef]
- Mente, A.; O’Donnell, M.; Rangarajan, S.; McQueen, M.; Dagenais, G.; Wielgosz, A.; Lear, S.; Ah, S.T.L.; Wei, L.; Diaz, R.; et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: A community-level prospective epidemiological cohort study. Lancet 2018, 392, 496–506. [Google Scholar] [CrossRef]
- O’Donnell, M.; Mente, A.; Rangarajan, S.; McQueen, M.J.; Wang, X.; Liu, L.; Yan, H.; Lee, S.Y.; Mony, P.; Devanatah, A.; et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N. Engl. J. Med. 2014, 371, 612–623. [Google Scholar] [CrossRef] [PubMed]
- Paterna, S.; Fasullo, S.; Cannizzaro, S.; Vitrano, G.; Terrazzino, G.; Maringhini, G.; Ganci, F.; Scalzo, S.; Di Pasquale, P.; Parrinello, G.; et al. Short-term effects of hypertonic saline solution in acute heart failure and long-term effects of a moderate sodium restriction in patients with compensated heart failure with New York heart Association Class III (Class C) (SMAC-HF study). Am. J. Med. Sci. 2011, 342, 27–37. [Google Scholar] [CrossRef]
- Paterna, S.; Gaspare, P.; Fasullo, S.; Sarullo, F.; Di Pasquale, P. Normal-sodium diet compared with low-sodium diet in compensated congestive heart failure: Is sodium an old enemy or a new friend? Clin. Sci. 2008, 114, 221–230. [Google Scholar] [CrossRef]
- Suzuki, H.; Takenaka, T.; Kanno, Y.; Ohno, Y.; Saruta, T. Sodium and Kidney Disease. Nutrition and Kidney Disease: A New Era. In Contribution to Nephrology; Karger: Basel, Switzerland, 2007; Volume 155, pp. 90–101. [Google Scholar] [CrossRef]
- Loh, J.T.; Torres, V.; Cover, T. Regulation of Helicobacter pylori cagA Expression in Response to Salt. Cancer Res. 2007, 67, 4709–4715. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund⁄American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective; American Institute for Cancer Research: Washington, DC, USA, 2007. [Google Scholar]
- Bedford, J.L.; Barr, S.I. Higher urinary sodium, a proxy for intake, is associated with increased calcium excretion and lower hip bone density in healthy young women with lower calcium intakes. Nutrients 2011, 3, 951–961. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Joung, J.Y.; Cho, Y.Y.; Sohn, S.Y.; Hur, K.Y.; Kim, J.H.; Kim, S.W.; Chung, J.H.; Lee, M.K.; Min, Y.K. Effect of high dietary sodium on bone turnover markers and urinary calcium excretion in Korean postmenopausal women with low bone mass. Eur. J. Clin. Nutr. 2015, 69, 361–366. [Google Scholar] [CrossRef]
- Park, Y.; Kwon, S.J.; Ha, Y.C. Association between Urinary Sodium Excretion and Bone Health in Male and Female Adults. Ann. Nutr. Metab. 2016, 68, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-W.; Jeon, J.-H.; Choi, Y.-K.; Lee, W.-K.; Hwang, I.-R.; Kim, J.-G.; Lee, I.-K.; Park, K.-G. Association of urinary sodium/creatinine ratio with bone mineral density in postmenopausal women: KNHANES 2008–2011. Endocrine 2015, 49, 791–799. [Google Scholar] [CrossRef]
- O’Donnell, M.; Mente, A.; Yusuf, S. Sodium intake and cardiovascular health. Circ. Res. 2015, 116, 1046–1057. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Appel, L.J.; Sacco, R.L.; Anderson, C.A.M.; Antmann, E.M.; Campbell, N.; Bunbar, S.B.; Frohlich, E.D.; Hall, J.E.; Jessup, M.; et al. Sodium, blood pressure, and cardiovascular disease: Further evidence supporting the American Heart Association sodium reduction recommendations. Circulation 2012, 126, 2880–2889. [Google Scholar] [CrossRef]
- Irish Heart Foundation. Salt, Blood Pressure and Heart Disease. 2008. Available online: http://www.irishheart.ie/iopen24/pub/healthpromotionreports/ihfstatement_salt (accessed on 3 March 2022).
- Whelton, P.K.; He, J. Health effects of sodium and potassium in humans. Curr. Opin. Lipidol. 2014, 25, 75–79. [Google Scholar] [CrossRef]
- Sugiura, T.; Takase, H.; Ohte, N.; Dohi, Y. Dietary Salt Intake is a Significant Determinant of Impaired Kidney Function in the General Population. Kidney Blood Press. Res. 2018, 43, 1245–1254. [Google Scholar] [CrossRef]
- Peleteiro, B.; Lopes, C.; Figueiredo, C.; Lunet, N. Salt intake and gastric cancer risk aαccording to Helicobacter pylori infection, smoking, tumour site and histological type. Br. J. Cancer 2010, 104, 198–207. [Google Scholar] [CrossRef]
- D’Elia, L.; Galletti, F.; Strazzullo, P. Dietary Salt Intake and Risk of Gastric Cancer. Cancer Treat. Res. 2013, 159, 83–95. [Google Scholar]
- He, F.J.; Li, J.; MacGregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, 1325. [Google Scholar] [CrossRef]
- Institute of Medicine. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. In Panel on Dietary Reference Intakes for Electrolytes, Water; The National Academies of Sciences Engineering Medicine: Washington, DC, USA, 2005. [Google Scholar]
- US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Amercans, 7th ed.; US Government Printing Office: Washington, DC, USA, December 2010.
- WHO. Guideline Sodium Intake for Adults and Children; WHO Press: Geneva, Switzerland, 2012. [Google Scholar]
- Grillo, A.; Salvi, L.; Coruzzi, P.; Salvi, P.; Parati, G. Sodium Intake and Hypertension. Nutrients 2019, 11, 1970. [Google Scholar] [CrossRef] [PubMed]
- Flack, J.M.; Adekola, B. Blood Pressure and the New ACC/AHA Hypertension Guidelines. Trends Cardiovasc. Med. 2019, 30, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Oria, M.; Harrison, M.; Stallings, V.A. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Committee to Review the Dietary Reference Intakes for Sodium and Potassium; National Academies Press (US): Washington, DC, USA, 5 March 2019. [Google Scholar]
- Rehrer, N.J. Fluid and electrolyte balance in the ultra-endurance sport. Sports Med. 2001, 31, 701–715. [Google Scholar] [CrossRef]
- Clapp, A.J.; Bishop, P.A.; Smith, J.F.; Mansfield, E.R. Effects of Carbohydrate-Electrolyte Content of Beverages on Voluntary Hydration in a Simulated Industrial Environment. AIHAJ Am. Ind. Hyg. Assoc. 2000, 61, 692–699. [Google Scholar] [CrossRef]
- Valentine, V. The importance of salt in theathlete’s diet. Curr. Sports Med. Rep. 2007, 6, 237–240. [Google Scholar] [PubMed]
- Maughan, R.J.; Shirreffs, S.M. Muscle Cramping During Exercise: Causes, Solutions, and Questions Remaining. Sports Med. 2019, 49, 115–124. [Google Scholar] [CrossRef]
- Hoffman, M.D.; Stuempfle, K.J. Muscle Cramping During a 161-km Ultramarathon: Comparison of Characteristics of Those with and without Cramping. Sports Med. Open 2015, 1, 24. [Google Scholar] [CrossRef] [PubMed]
- Schwellnus, M.P.; Allie, S.; Derman, W.; Collins, M. Increased running speed and pre-race muscle damage as risk factors for exercise-associated muscle cramps in a 56 km ultra-marathon: A prospective cohort study. Br. J. Sports Med. 2011, 45, 1132–1136. [Google Scholar] [CrossRef] [PubMed]
- Kao, W.F.; Hou, S.K.; Chiu, Y.H.; Chou, S.L.; Kuo, F.C.; Wang, S.H.; Chen, J.J. Effects of 100-km ultra marathon on acute kidney injury. Clin. J. Sport Med. 2015, 25, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, M.; Kreider, R.B.; Greenwood, L.; Byars, A. Cramping and injury incidence in collegiate football players are reduced by creatine supplementation. J. Athl. Train. 2003, 38, 216–219. [Google Scholar] [PubMed]
- Maddali, S.; Rodeo, S.A.; Barnes, R.; Warren, R.F.; Murrell, G.A. Postexercise increase in nitric oxide in football players with muscle cramps. Am. J. Sports Med. 1998, 26, 820–824. [Google Scholar] [CrossRef] [PubMed]
- Bennett, B.L.; Hew-Butler, T.; Rosner, M.H.; Myers, T.; Lipman, G.S. Wilderness Medical Society Clinical Practice Guidelines for the Management of Exercise-Associated Hyponatremia: 2019 Update. Wilderness Environ. Med. 2020, 31, 50–62. [Google Scholar] [CrossRef] [PubMed]
- McGreal, K.; Budhiraja, P.; Jain, N.; Yu, A.S. Current challenges in the evaluation and management of hyponatremia. Kidney Dis. 2016, 2, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Hew-Butler, T.; Almond, C.; Ayus, J.C.; Dugas, J.; Meeuwisse, W.; Noakes, T.; Weschler, L. Consensus Statement of the 1st International Exercise-Associated Hyponatremia Consensus Development Conference, Cape Town, South Africa 2005. Clin. J. Sport Med. 2005, 15, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Hew-Butler, T. Exercise-Associated Hyponatremia. Front. Horm. Res. 2019, 52, 178–189. [Google Scholar]
- Rüst, C.A. Higher prevalence of exercise-associated hyponatremia in triple iron ultra-triathletes than reported for ironman triathletes. Chin. J. Physiol. 2012, 55, 147–155. [Google Scholar] [CrossRef]
- Sharwood, K.A.; Collins, M.; Goedecke, J.H.; Wilson, G.; Noakes, T.D. Weight changes, medical complications, and performance during an Ironman triathlon. Br. J. Sports Med. 2004, 38, 718–724. [Google Scholar] [CrossRef]
- Speedy, D.B.; Faris, J.G.; Hamlin, M.; Gallagher, P.G.; Campbell, R.G. Hyponatremia and weight changes in an ultradistance triathlon. Clin. J. Sport Med. 1997, 7, 180–184. [Google Scholar] [CrossRef]
- Nikolaidis, P.T.; Veniamakis, E.; Rosemann, T.; Knechtle, B. Nutrition in Ultra-Endurance. State of the Art. Nutrients 2018, 10, 1995. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, W.B.; Bennett, W.; Curelop, S.; Bartter, F.C. A Syndrome of Renal Sodium Loss and Hyponatremia Probably Resulting from Inappropriate Secretion of Antidiuretic Hormone. Am. J. Med. 1957, 23, 529–542. [Google Scholar] [CrossRef]
- Buck, E.; Miles, R.; Schroeder, J.D. Exercise-Associated Hyponatremia; StatPearls Publishing, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK572128 (accessed on 3 March 2022).
- Rosner, M.H. Exercise-associated hyponatremia. Physician Sportsmed. 2008, 36, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Twerenbold, R.; Knechtle, B.; Kakebeeke, T.H.; Eser, P.; Müller, G.; Von Arx, P.; Knecht, H.; Rehrer, N.; Speedy, D. Effects of different sodium concentrations in replacement fluids during prolonged exercise in women. Br. J. Sports Med. 2003, 37, 300–303. [Google Scholar] [CrossRef] [PubMed]
- Oh, R.C.; Galer, M.; Bursey, M.M. Found in the Field—A Soldier with Heat Stroke, Exercise-Associated Hyponatremia, and Kidney Injury. Curr. Sports Med. Rep. 2018, 17, 123–125. [Google Scholar] [CrossRef] [PubMed]
- Holtzhausen, L.M.; Noakes, T.D. Collapsed ultraendurance athlete: Proposed mechanisms and an approachto management. Clin. J. Sport Med. 1997, 7, 292–301. [Google Scholar] [CrossRef]
- Hew-Butler, T.; Rosner, M.H.; Fowkes-Godek, S.; Dugas, J.P.; Hoffman, M.; Lewis, D.P.; Maughan, R.J.; Miller, K.C.; Montain, S.J.; Rehrer, N.J.; et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin. J. Sport Med. 2015, 25, 303–320. [Google Scholar] [CrossRef] [PubMed]
- Bailey, E. Electrolytes: Performance Perks and Real Food Sources NASM.org. 2017. Available online: https://blog.nasm.org/fitness/electrolytes-performance-perks-and-real-food-sources (accessed on 3 March 2022).
- Takamata, A.; Mack, G.W.; Stachenfeld, N.S.; Nadel, E.R. Body temperature modification of osmotically induced vasopressin secretion and thirst in humans. Am. J. Physiol. 1995, 269, R874–R880. [Google Scholar] [CrossRef] [PubMed]
- Hew, T.D.; Chorley, J.N.; Cianca, J.C.; Divine, J.G. The Incidence, Risk Factors, and Clinical Manifestations of Hyponatremia in Marathon Runners. Clin. J. Sport Med. 2003, 13, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Spano, S.J.; Reagle, Z.; Evans, T. Symptomatic Hypotonic Hyponatremia Presenting at High Altitude. Wilderness Environ. Med. 2014, 25, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, M.; Roth, R.; Davis, D.L.; Larrabe, E.H.; Callaway, C.W. Hyponatremia in runners requiring on-sitemedical treatment at a single marathon. Med. Sci. Sport Exerc. 2002, 34, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Almond, C.S.; Shin, A.Y.; Fortescue, E.B.; Mannix, R.C.; Wypij, D.; Binstadt, B.A.; Duncan, C.N.; Olson, D.P.; Salerno, A.E.; Newburger, J.W. Hyponatremia among runners in the boston marathon. N. Engl. J. Med. 2005, 352, 1550–1556. [Google Scholar] [CrossRef] [PubMed]
- Chorley, J.; Cianca, J.; Divine, J. Risk Factors for Exercise-Associated Hyponatremia in Non-Elite Marathon Runners. Clin. J. Sport Med. 2007, 17, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Mettler, S.; Rusch, C.; Frey, W.O.; Bestmann, L.; Wenk, C.; Colombani, P.C. Hyponatremia among runners inthe zurich marathon. Clin. J. Sport Med. 2008, 18, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Siegel, A.J.; D’Hemecourt, P.; Adner, M.M.; Shirey, T.; Brown, J.L.; Lewandrowski, K.B. Exertional dysnatremiain collapsed marathon runners: A critical role for point-of-care testing to guide appropriate therapy. Am. J. Clin. Pathol. 2009, 132, 336–340. [Google Scholar] [CrossRef] [PubMed]
- Kipps, C.; Sharma, S.; Pedoe, D.T. The incidence of exercise-associated hyponatraemia in the London marathon. Br. J. Sports Med. 2009, 45, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Nio, A.Q.; Ang, W.H. First reported cases of exercise-associated hyponatremia in Asia. Int. J. Sports Med. 2011, 32, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, M.D.; Hew-Butler, T.; Stuempfle, K.J. Exercise-associated hyponatremia and hydration status in 161-km ultramarathoners. Med. Sci. Sports Exerc. 2013, 45, 784–791. [Google Scholar] [CrossRef]
- Stuempfle, K.J.; Lehmann, D.R.; Case, H.S.; Bailey, S.; Hughes, S.L.; McKenzie, J.; Evans, D. Hyponatremia in a cold weather ultraendurance race. Alsk. Med. 2002, 44, 51–55. [Google Scholar]
- Lebus, D.K.; Casazza, G.A.; Hoffman, M.D.; Van Loan, M.D. Can Changes in Body Mass and Total Body Water Accurately Predict Hyponatremia After a 161-km Running Race? Clin. J. Sport Med. 2010, 20, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Hew-Butler, T. Arginine Vasopressin, Fluid Balance and Exercise. Sports Med. 2010, 40, 459–479. [Google Scholar] [CrossRef] [PubMed]
- Harris, G.; Reid, S.; Sikaris, K.; McCrory, P. Hyponatremia is associated with higher nt-probnp thannormonatremia after prolonged exercise. Clin. J. Sport Med. 2012, 22, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Speedy, D.B.; Noakes, T.D.; Rogers, I.R.; Thompson, J.M.; Campbell, R.G.; Kuttner, J.A.; Boswell, D.R.; Wright, S.; Hamlin, M. Hyponatremia in ultradistance triathletes. Med. Sci. Sports Exerc. 1999, 31, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Wharam, P.C.; Speedy, D.B.; Noakes, T.D.; Thompson, J.M.; Reid, S.A.; Holtzhausen, L.-M. NSAID use increases the risk of developing hyponatremia during an Ironman triathlon. Med. Sci. Sports Exerc. 2006, 38, 618–622. [Google Scholar] [CrossRef] [PubMed]
- Urso, C.; Brucculeri, S.; Caimi, G. Physiopathological, epidemiological, clinical and therapeutic aspects of exercise-associated hyponatremia. J. Clin. Med. 2014, 3, 1258–1275. [Google Scholar] [CrossRef] [PubMed]
- Rosner, M.H. Preventing Deaths Due to Exercise-Associated Hyponatremia: The 2015 Consensus Guidelines. Clin. J. Sport Med. 2015, 25, 301–302. [Google Scholar] [CrossRef] [PubMed]
- Bridges, E.; Altherwi, T.; Correa, J.A.; Hew-Butler, T. Oral Hypertonic Saline Is Effective in Reversing Acute Mild-to-Moderate Symptomatic Exercise-Associated Hyponatremia. Clin. J. Sport Med. 2020, 30, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Hew-Butler, T.; Sharwood, K.; Boulter, J.; Collins, M.; Tucker, R.; Dugas, J.; Noakes, T. Dysnatremia Predicts a Delayed Recovery in Collapsed Ultramarathon Runners. Clin. J. Sport Med. 2007, 17, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Spasovski, G.; Vanholder, R.; Allolio, B.; Annane, D.; Ball, S.; Bichet, D.; Decaux, S.; Fenske, W.; Hoorn, E.J.; Ichai, C.; et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur. J. Endocrinol. 2014, 170, G1–G47. [Google Scholar] [CrossRef] [PubMed]
- Rogers, I.R.; Hook, G.; Stuempfle, K.J.; Hoffman, M.D.; Hew-Butler, T. An intervention study of oralversus intravenous hypertonic saline administration in ultramarathon runners with exercise-associatedhyponatremia: A preliminary randomized trial. Clin. J. Sport Med. 2011, 21, 200–203. [Google Scholar] [CrossRef] [PubMed]
- Sanders, B.; Noakes, T.D.; Dennis, S.C. Sodium replacement and fluid shifts during prolonged exercise in humans. Eur. J. Appl. Physiol. 2001, 84, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Coso, J.D.; Estevez, E.; Baquero, R.A.; Mora-Rodriguez, R. Anaerobic performance when rehydrating with water or commercially available sports drinks during prolonged exercise in the heat. Appl. Physiol. Nutr. Metab. 2008, 33, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Domínguez, R.; Mata-Ordoñez, F.; Sánchez-Oliver, A.J. Nutrición Deportiva Aplicada: Guía para Optimizar el Rendimiento; ICB Editores: Malaga, Spain, 2017. [Google Scholar]
- Zoorob, R.; Parrish, M.-E.E.; O’Hara, H.; Kalliny, M. Sports Nutrition Needs. Primary Care. Clin. Off. Pract. 2013, 40, 475–486. [Google Scholar] [CrossRef]
- Convertino, V.A.; Armstong, L.E.; Coyle, E.F.; Mack, G.W.; Sawka, M.N.; Senay, L.C., Jr.; Sherman, W.M. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 1996, 28, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B.; Jeukendrup, A.E. Optimal Composition of Fluid-Replacement Beverages. Compr. Physiol. 2014, 4, 575–620. [Google Scholar] [PubMed]
- Kenefick, R.W.; Cheuvront, S.N. Hydration for recreational sport and physical activity. Nutr. Rev. 2012, 70, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Parsons, K. The Effects of Hot, Moderate and Cold Environments on Human Health, Comfort and Performance, Human Thermal Environments, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Baker, L.B.; Barnes, K.A.; Anderson, M.L.; Passe, D.H.; Stofan, J.R. Normative data for regional sweat sodiumconcentration and whole-body sweating rate in athletes. J. Sports Sci. 2016, 34, 358–368. [Google Scholar] [CrossRef] [PubMed]
- González-Alonso, J.; Calbet, J.A.L.; Nielsen, B. Muscle blood flow is reduced with dehydration during prolonged exercise in humans. J. Physiol. 1998, 513, 895–905. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.M. Hydration in Sport and Exercise. In Heat Stress in Sport and Exercise; Springer: Cham, Switzerland, 2019; pp. 113–137. [Google Scholar]
- Cheuvront, S.; Carter, R.; Sawka, M.N. Fluid balance and endurance exercise performance. Curr. Sports Med. Rep. 2003, 2, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Maughan, R.J.; Noakes, T.D. Fluid replacement and exercise stress. A brief review of studies on fluid replacement and some guidelines for the athlete. Sports Med. 1991, 12, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Van Rosendal, S.P.; Coombes, J.S. Glycerol Use in Hyperhydration and Rehydration: Scientific Update. Med. Sport Sci. 2012, 59, 104–112. [Google Scholar]
- Cairns, R.S.; Hew-Butler, T. Incidence of Exercise-Associated Hyponatremia and Its Association with Nonosmotic Stimuli of Arginine Vasopressin in the GNW100s Ultra-endurance Marathon. Clin. J. Sport Med. 2015, 25, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. American College of Sports Medicine Joint Position Statement. Nutrition and Athletic Performance. Med. Sci. Sports Exerc. 2016, 48, 543–568. [Google Scholar] [CrossRef] [PubMed]
- Sawka, M.N.; Burke, L.M.; Eichner, E.R.; Maughan, R.J.; Montain, S.J.; Stachenfeld, N.S. American College of Sports Medicine Position Stand. Exercise and Fluid Replacement. Med. Sci. Sports Exerc. 2007, 39, 377–390. [Google Scholar] [PubMed]
- American Dietetic Association; Dietitians of Canada; American College of Sports Medicine; Rodriguez, N.R.; di Marco, N.M.; Langley, S. American College of Sports Medicine position stand. Nutrition and Athletic Performance. Med. Sci. Sports Exerc. 2009, 41, 709–731. [Google Scholar] [CrossRef]
- Kerksick, C.M.; Wilborn, C.D.; Roberts, M.D.; Smith-Ryan, A.; Kleiner, S.M.; Jäger, R.; Collins, R.; Cooke, M.; Davis, J.N.; Galvan, E.; et al. ISSN exercise & sports nutrition review update: Research & recommendations. J. Int. Soc. Sports Nutr. 2018, 15, 38. [Google Scholar] [PubMed]
- Tiller, N.B.; Roberts, J.D.; Beasley, L.; Chapman, S.; Pinto, J.M.; Smith, L.; Wiffin, M.; Russell, M.; Sparks, S.A.; Duckworth, L.; et al. International Society of Sports Nutrition Position Stand: Nutritional considerations for single-stage ultra-marathon training and racing. J. Int. Soc. Sports Nutr. 2019, 16, 1–23. [Google Scholar] [CrossRef]
- Rodriguez, N.R.; DiMarco, N.M.; Langley, S. Position of the American Dietetic Association, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and athletic performance. J. Acad. Nutr. Diet. 2009, 109, 509–527. [Google Scholar]
- Racinais, S.; Alonso, J.M.; Coutts, A.J.; Flouris, A.D.; Girard, O.; González-Alonso, J.; Périard, J.D. Consensus recommendations on training and competing in the heat. Br. J. Sports Med. 2015, 49, 1164–1173. [Google Scholar] [CrossRef]
- Shirreffs, S.M.; Taylor, A.J.; Leiper, J.B.; Maughan, R.J. Post-exercise rehydration in man: Effects of volume consumed and drink sodium content. Med. Sci. Sports Exerc. 1996, 28, 1260–1271. [Google Scholar] [CrossRef]
- Grozenski, A.; Kiel, J. Basic Nutrition for Sports Participation, Part 1: Diet Composition, Macronutrients, and Hydration. Curr. Sports Med. Rep. 2020, 19, 389–391. [Google Scholar] [CrossRef] [PubMed]
- Jeukendrup, A.E.; Currell, K.; Clarke, J.; Cole, J.; Blannin, A.K. Effect of beverage glucose and sodium content on fluid delivery. Nutr. Metab. 2009, 6, 9. [Google Scholar] [CrossRef] [PubMed]
- Ranchordas, M.K.; Tiller, N.B.; Ramchandani, G.; Jutley, R.; Blow, A.; Tye, J.; Drury, B. Normative data on regional sweat-sodium concentrations of professional male team-sport athletes. J. Int. Soc. Sports Nutr. 2017, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Associated Press. Woman Dies after Water Drinking Contest. NBCnews.com. 2007. Available online: http://www.nbcnews.com/id/16614865/ns/us_news-life/t/woman-dies-after-water-drinking-contest (accessed on 3 March 2022).
- Hoffman, M.D.; Myers, T.M. Case Study: Symptomatic Exercise-Associated Hyponatremia in an Endurance Runner Despite Sodium Supplementation. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 603–606. [Google Scholar] [CrossRef] [PubMed]
- Hew-Butler, T.; Loi, V.; Pani, A.; Rosner, M.H. Exercise-Associated Hyponatremia: 2017 Update. Front. Med. 2017, 4, 21. [Google Scholar] [CrossRef] [PubMed]
| Clinical Condition | n | Average Age (Years) | Average Sodium Intake | Τype of Study | Correlation | References |
|---|---|---|---|---|---|---|
| Kidney Disease | 1384 | ≥20 | 11.5 gr | Observational | Positive | [44] |
| Cancer | 2485 | 18–92 | 9 g | Case-control | Positive | [45] |
| Cancer | 634 | 40–49 | 12.8 g | Cross-sectional | Positive | [46] |
| Hypertension | 3230 | 22–73 | 9.4 g | Meta-analysis | Positive | [47] |
| Hypertension | 10,074 | 20–59 | Serum > 100 mmol/L | Cross-sectional | Positive | [12] |
| Osteoporosis | 537 | 58 ± 6 | >2 g/day | Cross-sectional | Positive | [37] |
| Osteoporosis | 102 | 24 ± 3.4 | 2.6 ± 1.1 g/day | Cross checked | Positive | [36] |
| Sports | Prevalence EAMC | References |
|---|---|---|
| Ultra-Marathon 166 km | 14% | [58] |
| Marathon | 18% | [10] |
| Ironman Triathlon | 23% | [59] |
| Ultra-Marathon 100 km | 23% | [60] |
| Ultra-Marathon 56km | 41% | [59] |
| Cycling | 60% | [8] |
| American football | 30–53% | [61,62] |
| Sports | Trial | Prevalence EAH | References |
|---|---|---|---|
| Marathon | Marathon | 15% | [82] |
| Houston Marathon 2000 | <5% | [80] | |
| Boston Marathon | 5% | [83] | |
| Houston Marathon 2000–2004 | >20% | [84] | |
| Zurich Marathon | <5% | [85] | |
| Boston Marathon 2001–2018 | <5% | [86] | |
| London Marathon | Up to 22% | [87] | |
| Ultra-Marathon | Ultra-marathon in Asia | 38% | [88] |
| 161 km in North America | 30–51% | [89] [90] [91] | |
| Cycling | 109 km | 12% | [92] |
| 210–250 km | 4.5% (4 to 90 persons) | [93] | |
| Triathlon | Ironman-Triathlon | 20% | [69] |
| Ironman-Triathlon | 1.8–28% | [94,95] | |
| Triple Ironman | 26% | [67] |
| Mild | Severe | Clinical Appearance |
|---|---|---|
| WearinessDizziness | Mental disorder | Heat stroke |
| Slow urine production | Ictus, collapse | Hypoglycemia |
| Sickness | Oliguria | Stress-related collapse |
| Headache | Coma | Muscle cramps |
| Weakness | Death | Edema |
| Mild Symptoms | Severe (Neurological Symptoms) | In Encephalopathy | Bibliography | |
|---|---|---|---|---|
| Intravenous isotonic fluids of any type or volume are not recommended | recommended | is not recommended | is not recommended | [100] |
| Concentrated oral sodium replacement may be given (with reservation) | recommended | is not recommended | is not recommended | [86] |
| Bolus 100 mL of intravenous hypertonic saline (3% sodium chloride) | is not recommended | recommended | recommended | [63] [75] |
| Should be treated immediately with intravenous IV bolus infusion or HTS infusion for acute reduction of swelling in the brain | is not recommended | is not recommended | recommended | [58] [101] |
| Timing | Dosage | Bibliography |
|---|---|---|
| Before exercise | 5 to 10 mL/kg body weight | [117] |
| Before exercise | 5–7 mL/kg 4 h before exercise and more 3–5 mL/kg, 2 h before competition | [118] |
| 4 h before exercise | 5–7 mL/kg water or sports drink | [119] |
| Before exercise | 400–600 mL cold water or sports drink 20–30 min before exercise | [120] |
| Sports | Timing | Dosage | Bibliography |
|---|---|---|---|
| Ultra-Marathon | During exercise or competition, each 20 min | 150–250 mlliquids | [121] |
| Ultra-Marathon Competition | Each 1 h | 300–600 mL | [70] |
| Marathon | Each 1 h | 400–800 mL | [118] |
| Regardless of sport | During the exercise | 450–675 mL, for every 0.5 kg of body weight lost | [122] |
| Sports | Timing | Dosage | Bibliography |
|---|---|---|---|
| Regardless of sport | After the exercise | 1.25 to 1.5 L liquids for every 1 kg of weight loss | [117] |
| General for athletes in a warm climate | After the exercise | 100–120% body mass losses | [123] |
| Regardless of sport | For fullrestoration | 450–675 mL for every 0.5 kg of weight loss | [119] |
| General for athletes | After the exercise | Liquid with 150% or 200% of weight loss | [124] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veniamakis, E.; Kaplanis, G.; Voulgaris, P.; Nikolaidis, P.T. Effects of Sodium Intake on Health and Performance in Endurance and Ultra-Endurance Sports. Int. J. Environ. Res. Public Health 2022, 19, 3651. https://doi.org/10.3390/ijerph19063651
Veniamakis E, Kaplanis G, Voulgaris P, Nikolaidis PT. Effects of Sodium Intake on Health and Performance in Endurance and Ultra-Endurance Sports. International Journal of Environmental Research and Public Health. 2022; 19(6):3651. https://doi.org/10.3390/ijerph19063651
Chicago/Turabian StyleVeniamakis, Eleftherios, Georgios Kaplanis, Panagiotis Voulgaris, and Pantelis T. Nikolaidis. 2022. "Effects of Sodium Intake on Health and Performance in Endurance and Ultra-Endurance Sports" International Journal of Environmental Research and Public Health 19, no. 6: 3651. https://doi.org/10.3390/ijerph19063651
APA StyleVeniamakis, E., Kaplanis, G., Voulgaris, P., & Nikolaidis, P. T. (2022). Effects of Sodium Intake on Health and Performance in Endurance and Ultra-Endurance Sports. International Journal of Environmental Research and Public Health, 19(6), 3651. https://doi.org/10.3390/ijerph19063651