Patients’ Health Literacy in Rehabilitation: Comparison between the Estimation of Patients and Health Care Professionals
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
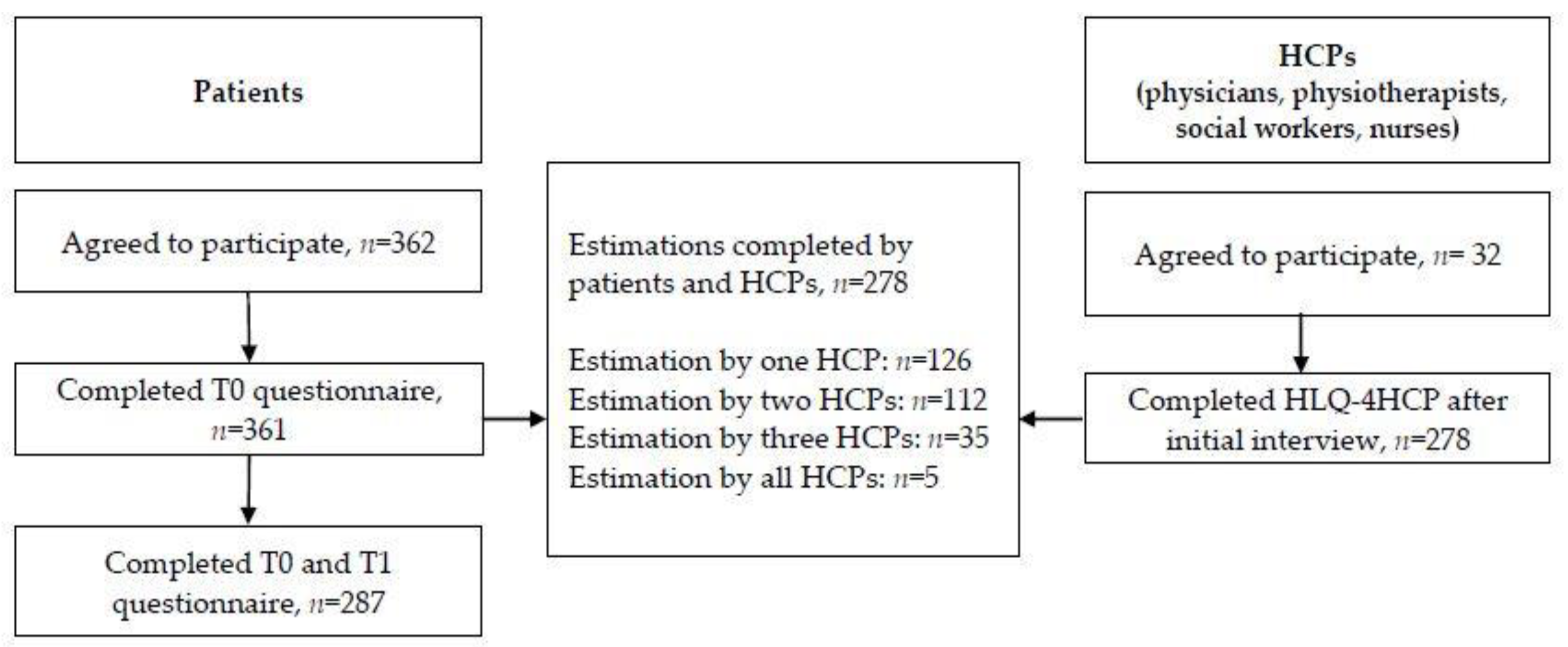
2.2. Sampling and Participants
2.3. Measures
2.3.1. Health Literacy
- Feeling understood and supported by health care providers (four items)
- 2.
- Having sufficient information to manage my health (four items)
- 3.
- Actively managing my health (five items)
- 4.
- Social support for health (five items)
- 5.
- Appraisal of health information (five items)
- 6.
- Ability to actively engage with health care providers (five items)
- 7.
- Navigating the health care system (six items)
- 8.
- Ability to find good health information (five items)
- 9.
- Understanding health information well enough to know what to do (five items)
2.3.2. Patients Survey
2.3.3. HCPs Survey
2.4. Data Collection
2.5. Data Analysis
2.6. Ethical Considerations and Trial Registration
3. Results
3.1. Sample Characteristics
3.2. Estimations by Patients and HCPs
3.3. Self-Assessment of Patients’ HL Level
3.4. HCPs Estimation of Patients’ HL Level
3.5. HL Agreement
4. Discussion
4.1. Implications for Practice and Research
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berkman, N.D.; Davis, T.C.; McCormack, L. Health literacy: What is it? J. Health Commun. 2010, 15, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Baccolini, V.; Rosso, A.; Di Paolo, C.; Isonne, C.; Salerno, C.; Migliara, G.; Prencipe, G.P.; Massimi, A.; Marzuillo, C.; De Vito, C.; et al. What is the Prevalence of Low Health Literacy in European Union Member States? A Systematic Review and Meta-analysis. J. Gen. Intern. Med. 2021, 36, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, D.; Berens, E.M.; Vogt, D. Health Literacy in the German Population. Dtsch. Arztebl. Int. 2017, 114, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, S.L.; Halpern, D.J.; Viera, A.J.; Berkman, N.D.; Donahue, K.E.; Crotty, K. Interventions for individuals with low health literacy: A systematic review. J. Health Commun. 2011, 16 (Suppl. 3), 30–54. [Google Scholar] [CrossRef] [PubMed]
- Brach, C.; Keller, D.; Hernandez, L.M.; Baur, C.; Parker, R.; Dreyer, B.; Schyve, P.; Lemerise, A.J.; Schillinger, D. Ten Attributes of Health Literate Health Care Organizations. NAM Perspect. 2012. [Google Scholar] [CrossRef]
- Schillinger, D.; Grumbach, K.; Piette, J.; Wang, F.; Osmond, D.; Daher, C.; Palacios, J.; Sullivan, G.D.; Bindman, A.B. Association of health literacy with diabetes outcomes. JAMA 2002, 288, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Cajita, M.I.; Cajita, T.R.; Han, H.R. Health Literacy and Heart Failure: A Systematic Review. J. Cardiovasc. Nurs. 2016, 31, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.W.; Parker, R.M.; Clark, W.S. Health literacy and the risk of hospital admission. J. Gen. Intern. Med. 1998, 13, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, D.; Vogt, D.; Berens, E.M.; Hurrelmann, K. Gesundheitskompetenz der Bevölkerung in Deutschland: Ergebnisbericht; Universität Bielefeld: Bielefeld, Germany, 2017. [Google Scholar]
- Hasseler, M. Menschen mit geistigen und mehrfachen Behinderungen als vulnerable Bevölkerungsgruppe in gesundheitlicher Versorgung. Dtsch. Med. Wochenschr. 2014, 139, 2030–2034. [Google Scholar] [CrossRef] [PubMed]
- Bitzer, E.M.; Dierks, M.L.; Heine, W.; Becker, P.; Vogel, H.; Beckmann, U.; Butsch, R.; Dörning, H.; Brüggemann, S. Empowerment and health literacy in medical rehabilitation—recommendations for strengthening patient education. Rehabilitation 2009, 48, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Mittag, O.; Welti, F. Medizinische Rehabilitation im europäischen Vergleich und Auswirkungen des europäischen Rechts auf die deutsche Rehabilitation. Bundesgesundheitsblatt Gesundh. Gesundh. 2017, 60, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Ernstmann, N.; Bauer, U.; Berens, E.-M.; Bitzer, E.M.; Bollweg, T.M.; Danner, M.; Dehn-Hindenberg, A.; Dierks, M.L.; Farin, E.; Grobosch, S.; et al. DNVF Memorandum Gesundheitskompetenz (Teil 1)—Hintergrund, Relevanz, Gegenstand und Fragestellungen in der Versorgungsforschung. Gesundheitswesen 2020, 82, e77–e93. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, E.; Schöpf, A.C.; Farin, E. What is competent communication behaviour of patients in physician consultations?—Chronically-ill patients answer in focus groups. Psychol. Health Med. 2017, 22, 987–1000. [Google Scholar] [CrossRef]
- Schillinger, D.; Bindman, A.; Wang, F.; Stewart, A.; Piette, J. Functional health literacy and the quality of physician–patient communication among diabetes patients. Patient Educ. Couns. 2004, 52, 315–323. [Google Scholar] [CrossRef]
- Allenbaugh, J.; Spagnoletti, C.L.; Rack, L.; Rubio, D.; Corbelli, J. Health Literacy and Clear Bedside Communication: A Curricular Intervention for Internal Medicine Physicians and Medicine Nurses. MedEdPORTAL 2019, 15, 10795. [Google Scholar] [CrossRef]
- Tavakoly Sany, S.B.; Behzhad, F.; Ferns, G.; Peyman, N. Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: A randomized controlled trial. BMC Health Serv. Res. 2020, 20, 60. [Google Scholar] [CrossRef]
- Voigt-Barbarowicz, M.; Brütt, A.L. The Agreement between Patients’ and Healthcare Professionals’ Assessment of Patients’ Health Literacy-A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 2372. [Google Scholar] [CrossRef]
- Nolte, S.; Osborne, R.H.; Dwinger, S.; Elsworth, G.R.; Conrad, M.L.; Rose, M.; Härter, M.; Dirmaier, J.; Zill, J.M. German translation, cultural adaptation, and validation of the Health Literacy Questionnaire (HLQ). PLoS ONE 2017, 12, e0172340. [Google Scholar] [CrossRef]
- Hawkins, M.; Gill, S.D.; Batterham, R.; Elsworth, G.R.; Osborne, R.H. The Health Literacy Questionnaire (HLQ) at the patient-clinician interface: A qualitative study of what patients and clinicians mean by their HLQ scores. BMC Health Serv. Res. 2017, 17, 309. [Google Scholar] [CrossRef]
- Maindal, H.T.; Kayser, L.; Norgaard, O.; Bo, A.; Elsworth, G.R.; Osborne, R.H. Cultural adaptation and validation of the Health Literacy Questionnaire (HLQ): Robust nine-dimension Danish language confirmatory factor model. Springerplus 2016, 5, 1232. [Google Scholar] [CrossRef] [PubMed]
- Osborne, R.H.; Batterham, R.W.; Elsworth, G.R.; Hawkins, M.; Buchbinder, R. The grounded psychometric development and initial validation of HLQ. BMC Public Health 2013, 13, 658. [Google Scholar] [CrossRef] [PubMed]
- Bo, A.; Friis, K.; Osborne, R.H.; Maindal, T.H. National indicators of health literacy: Ability to understand health information and to engage actively with healthcare providers—A population based survey among Danish adults. BMC Public Health 2014, 14, 1095. Available online: http://www.biomedcentral.com/1471-2458/14/1095 (accessed on 17 January 2022). [CrossRef] [PubMed]
- Faruqi, N.; Stocks, N.; Spooner, C.; El Haddad, N.; Harris, M.F. Research protocol: Management of obesity in patients with low health literacy in primary health care. BMC Obes. 2015, 2, 5. [Google Scholar] [CrossRef] [PubMed][Green Version]
- IBM Corp. IBM SPSS Statistics for Windows, Version 27.0; IBM Corp: Armonk, NY, USA, 2020. [Google Scholar]
- Cicchetti, D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 1994, 6, 284–290. [Google Scholar] [CrossRef]
- Lindskrog, S.; Christensen, K.B.; Osborne, R.H.; Vingtoft, S.; Phanareth, K.; Kayser, L. Relationship Between Patient-Reported Outcome Measures and the Severity of Chronic Obstructive Pulmonary Disease in the Context of an Innovative Digitally Supported 24-Hour Service: Longitudinal Study. J. Med. Internet. Res. 2019, 21, e10924. [Google Scholar] [CrossRef]
- Bass, P.F., III.; Wilson, J.F.; Griffith, C.H.; Barnett, D.R. Residents’ Ability to Identifity Patients with Poor literacy Skills. Acad. Med. 2002, 77, 1030–1041. [Google Scholar] [CrossRef]
- Dickens, C.; Lambert, B.L.; Cromwell, T.; Piano, M.R. Nurse overestimation of patients’ health literacy. J. Health Commun. 2013, 18 (Suppl. 1), 62–69. [Google Scholar] [CrossRef]
- Kelly, P.A.; Haidet, P. Physician overestimation of patient literacy: A potential source of health care disparities. Patient Educ. Couns. 2007, 66, 119–122. [Google Scholar] [CrossRef]
- Lindau, S.T.; Basu, A.; Leitsch, S.A. Health Literacy as a Predictor of Follow-Up After an Abnormal Pap Smear. J. Gen. Intern. Med. 2006, 21, 829–834. [Google Scholar] [CrossRef][Green Version]
- Rogers, E.D.; Wallace, L.S.; Weiss, B.D. Misperceptions of Medical Understanding in low. Cancer Control 2006, 13, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Storms, H.; Aertgeerts, B.; Vandenabeele, F.; Claes, N. General practitioners’ predictions of their own patients´ health literacy. BMJ Open 2019, 9, e029357. [Google Scholar] [CrossRef] [PubMed]
- Zawilinski, L.L.; Kirkpatrick, H.; Pawlaczyk, B.; Yarlagadda, H. Actual and perceived patient health literacy: How accurate are residents’ predictions? Int. J. Psychiatry Med. 2019, 54, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Toronto, C.E.; Weatherford, B.J. Health Literacy Education in Health Professions Schools: An Integrative Review. Nurs. Educ. 2015, 54, 669–676. [Google Scholar] [CrossRef]
- Saunders, C.; Palesy, D.; Lewis, J. Systematic Review and Conceptual Framework for Health Literacy Training in Health Professions Education. Health Prof. Edu. 2019, 5, 13–29. [Google Scholar] [CrossRef]
- Sadeghi, S.; Brooks, D.; Goldstein, R.S. Patients’ and providers’ perceptions of the impact of health literacy on communication in pulmonary rehabilitation. Chron. Respir. Dis. 2013, 10, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Levasseur, M.; Carrier, A. Do rehabilitation professionals need to consider their clients’ health literacy for effective practice? Clin. Rehabil. 2010, 24, 756–765. [Google Scholar] [CrossRef]
- Coleman, C. Teaching health care professionals about health literacy: A review of the literature. Nurs. Outlook 2011, 59, 70–78. [Google Scholar] [CrossRef]
- Brega, A.G.; Barnard, J.; Mabachi, N.M.; Weiss, B.D.; DeWalt, D.A.; Brach, C.; Cifuentes, M.; Albright, K.; West, D.R. Use the Teach-Back Method: Tool 5; AHRQ Health Literacy Universal Precautions Toolkit: Rockville, MD, USA, 2015. [Google Scholar]
- Schmidt-Kaehler, S.; Vogt, D.; Berens, E.M.; Horn, A.; Schaeffer, D. Gesundheitskompetenz: Verständlich Informieren und Beraten. Material-und Methodensammlung zur Verbraucher-und Patientenberatung für Zielgruppen mit Geringer Gesundheitskompetenz; Bielefeld University: Bielefeld, Germany, 2017. [Google Scholar]
- Kountz, D.S. Strategies for improving low health literacy. Postgrad. Med. 2009, 121, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Kaper, M.S.; Winter, A.F.; Bevilacqua, R.; Giammarchi, C.; McCusker, A.; Sixsmith, J.; Koot, J.A.R.; Reijneveld, S.A. Positive Outcomes of a Comprehensive Health Literacy Communication Training for Health Professionals in Three European Countries: A Multi-centre Pre-post Intervention Study. Int. J. Environ. Res. Public Health 2019, 16, 20. [Google Scholar] [CrossRef] [PubMed]
- Kaper, M.S.; Reijneveld, S.A.; van Es, F.D.; de Zeeuw, J.; Almansa, J.; Koot, J.A.R.; de Winter, A.F. Effectiveness of a Comprehensive Health Literacy Consultation Skills Training for Undergraduate Medical Students: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 17, 81. [Google Scholar] [CrossRef] [PubMed]
- Kripalani, S.; Weiss, B.D. Teaching about health literacy and clear communication. J. Gen. Intern. Med. 2006, 21, 888–890. [Google Scholar] [CrossRef] [PubMed]
| Demographic and Health Characteristics | Total n = 287 |
|---|---|
| Age, n (%) | |
| Until 29 years | 4 (1.4) |
| 30–39 years | 15 (5.2) |
| 40–49 years | 32 (11.1) |
| 50–59 years | 140 (48.8) |
| 60 years and older | 95 (33.1) |
| Prefer not to answer | 1 (0.3) |
| Gender, n (%) | |
| Women | 178 (62.0) |
| Men | 109 (38.0) |
| Live alone, n (%) | |
| Alone | 55 (19.2) |
| Not alone | 224 (78.0) |
| Prefer not to answer | 8 (2.8) |
| Nationality, n (%) | |
| German | 273 (95.1) |
| Other | 6 (2.1) |
| Prefer not to answer | 8 (2.8) |
| Mother tongue, n (%) | |
| German | 261 (90.9) |
| Other languages | 17 (5.9) |
| Prefer not to answer | 9 (3.1) |
| Language skills in German | |
| very good | 3 (17.6) |
| good | 12 (70.6) |
| medium | 2 (11.8) |
| Education, n (%) | |
| A-level or higher | 120 (41.8) |
| GCSE or equivalent | 153 (53.3) |
| No Qualification | 5 (1.7) |
| Prefer not to answer | 9 (3.1) |
| Reasons for rehabilitation, n (%) | |
| Joint replacement surgery (e.g., hip, knee) | 135 (34.3) |
| Spine surgery (e.g., intervertebral disc) | 70 (17.8) |
| Wear disease (e.g., arthrosis) | 47 (11.9) |
| Functional disorders of the musculoskeletal system | 46 (11.7) |
| Chronic back pain | 38 (9.7) |
| Bone fracture, muscle-tendon rupture, capsular ligament injury | 21 (5.4) |
| Other diseases | 35 (9.0) |
| 1 (chronic) disease | 215 (54.9) |
| ≥2 (chronic) diseases | 177 (45.1) |
| Status of disability | |
| No severe disability | 250 (87.1) |
| Severe disability (≥50%) | 35 (12.2) |
| Not sure | 2 (0.7) |
| HLQ Scale | Mean (SD) (95% CI), Patients T0 (n = 287) a | Mean (SD) (95% CI), Patients T1 (n = 287) b | p-Value * | Cohens d ** | Mean (SD) (95% CI), Physicians (n = 176) | Mean (SD) (95% CI), Physio- Therapists (n = 141) | Mean (SD) (95% CI), Social Workers (n = 113) c | Mean (SD) (95% CI]), Nurses (n = 45) d |
|---|---|---|---|---|---|---|---|---|
| Range 1 (lowest)–4 (highest) | ||||||||
| 1. Feeling understood and supported by health care providers | 3.15 (0.47) (3.09, 3.20) | 3.18 (0.46) (3.12, 3.23) | 0.261 | |||||
| 2. Having sufficient information to manage my health | 2.85 (0.50) (2.80, 2.91) | 3.02 (0.48) (2.96, 3.08) | 0.000 | −0.35 | 2.82 (0.61) (2.73, 2.91) | 2.73 (0.60) (2.63, 2.83) | 2.93 (0.61) (2.82, 3.05) | 3.24 (0.46) (3.09, 3.38) |
| 3. Actively managing my health | 2.95 (0.44) (2.90, 3.00) | 3.07 (0.42) (3.02, 3.12) | 0.000 | −0.28 | 2.73 (0.69) (2.63, 2.83) | 2.90 (0.54) (2.81, 2.99) | 2.76 (0.54) (2.66, 2.86) | 3.18 (0.45) (3.03, 3.32) |
| 4. Social support for health | 3.06 (0.50) (3.00, 3.11) | 3.10 (0.49) (3.04, 3.15) | 0.082 | |||||
| 5. Appraisal of health information | 2.86 (0.48) (2.80, 2.91) | 2.89 (0.50) (2.83, 2.95) | 0.113 | |||||
| Range 1 (lowest)–5 (highest) | ||||||||
| 6. Ability to actively engage with health care providers | 3.84 (0.57) (3.77, 3.90) | 3.92 (0.56) (3.86, 3.99) | 0.003 | −0.14 | 4.04 (0.61) (3.95, 4.13) | 4.05 (0.52) (3.96, 4.13) | 4.18 (0.72) (4.04, 4.31) | 4.46 (0.53) (4.30, 4.62) |
| 7. Navigating the health care system | 3.68 (0.56) (3.62, 3.75) | 3.79 (0.58) (3.72, 3.86) | 0.000 | −0.19 | ||||
| 8. Ability to find good health information | 3.79 (0.56) (3.72, 3.85) | 3.89 (0.55) (3.82, 3.95) | 0.000 | −0.18 | ||||
| 9. Understanding health information well enough to know what to do | 3.83 (0.55) (3.77, 3.89) | 3.89 (0.55) (3.83, 3.96) | 0.011 | 4.04 (0.58) (3.95, 4.13) | 4.30 (0.58) (4.20, 4.40) | 4.01 (0.72) (3.87, 4.14) | 4.37 (0.57) (4.20, 4.54) | |
| ICC * | |||||
|---|---|---|---|---|---|
| Patients | HLQ Scale | Physicians (n = 176) | Physiotherapists (n = 141) | Social Workers (n = 113) | Nurses (n = 45) |
| 2. Having sufficient information to manage my health | 0.21 | 0.20 | 0.47 | 0.10 | |
| 3. Actively managing my health | 0.27 | 0.45 | 0.44 | 0.40 | |
| 6. Ability to actively engage with health care providers | 0.21 | 0.02 | 0.31 | 0.16 | |
| 9. Understanding health information well enough to know what to do | 0.44 | 0.16 | 0.56 | 0.27 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Voigt-Barbarowicz, M.; Dietz, G.; Renken, N.; Schmöger, R.; Brütt, A.L. Patients’ Health Literacy in Rehabilitation: Comparison between the Estimation of Patients and Health Care Professionals. Int. J. Environ. Res. Public Health 2022, 19, 3522. https://doi.org/10.3390/ijerph19063522
Voigt-Barbarowicz M, Dietz G, Renken N, Schmöger R, Brütt AL. Patients’ Health Literacy in Rehabilitation: Comparison between the Estimation of Patients and Health Care Professionals. International Journal of Environmental Research and Public Health. 2022; 19(6):3522. https://doi.org/10.3390/ijerph19063522
Chicago/Turabian StyleVoigt-Barbarowicz, Mona, Günter Dietz, Nicole Renken, Ruben Schmöger, and Anna Levke Brütt. 2022. "Patients’ Health Literacy in Rehabilitation: Comparison between the Estimation of Patients and Health Care Professionals" International Journal of Environmental Research and Public Health 19, no. 6: 3522. https://doi.org/10.3390/ijerph19063522
APA StyleVoigt-Barbarowicz, M., Dietz, G., Renken, N., Schmöger, R., & Brütt, A. L. (2022). Patients’ Health Literacy in Rehabilitation: Comparison between the Estimation of Patients and Health Care Professionals. International Journal of Environmental Research and Public Health, 19(6), 3522. https://doi.org/10.3390/ijerph19063522






