Health Literacy-Sensitive Counselling on Early Childhood Allergy Prevention: Results of a Qualitative Study on German Midwives’ Perspectives
Abstract
1. Introduction
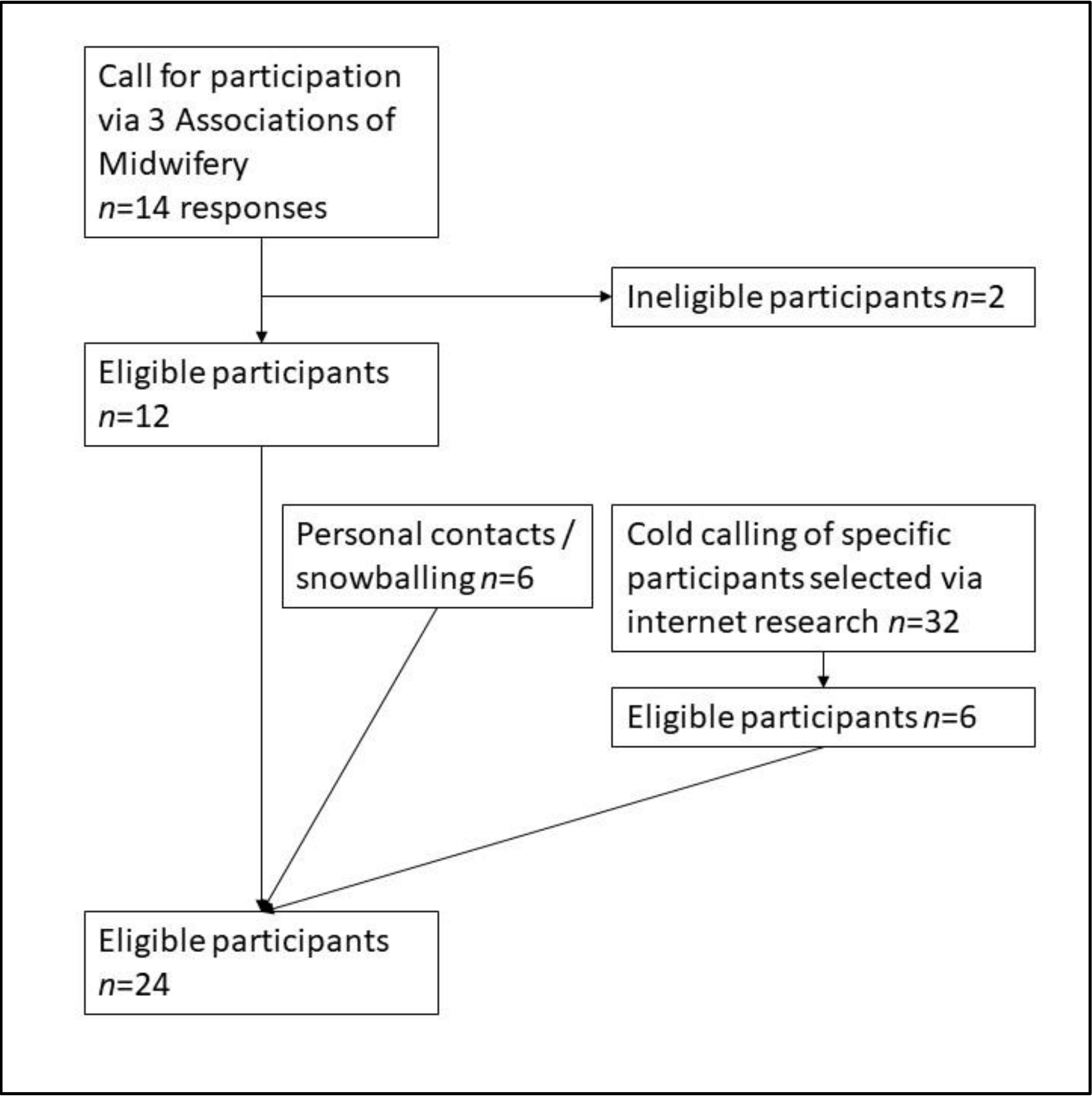
2. Methods
3. Recruitment
4. Sample
5. Analysis
6. Informed Consent and Confidentiality, Ethics Approval
7. Results
7.1. Assessment of Parental HL and Knowledge on ECAP
Some want things explained in simple terms, and to others you have to explain or prove everything down to the last comma. I try to convey information in a way that is understandable to them. In other words, I meet them where they are. I don’t need to come up with any scientific explanations for someone who is rather “simple-minded”.(Int 3)
Sometimes you just have to be a bit more scientific [with academics] and can give them more facts about sudden infant death syndrome and allergy prevention than with a cashier, where you say, “It’s just good if your child gets breast milk”.(Int 12)
This questionnaire stuff… I tend to have the feeling that it would take me away from the women. It would become so scientific. They don’t want that. It’s such a vulnerable time […]. They want to talk a lot. And if you allow that, it’s very easy to understand these women and work with them. You know exactly what you have to say and how you can take good care of them.(Int 2)
So, you quickly realize in a personal conversation, how much information you can give at once. Whether you can do it en bloc or whether you have to convey it in portions. That is individual, always different. Every person is different. And then you always have to see how it is received. Is it understood? How is it implemented? And then you just have to look at it step by step, how is it working? And that’s how it’s passed on.(Int 16)
Of course, there is a pattern. First, when I enter, I observe: Is it clean? Is it tidy or chaotic? What kind of furniture does the person have? How is the person dressed? What kind of food, what kind of creams are standing around? These are all things that are subconsciously absorbed. If the baby only wears cotton clothes, then […] you can start on a different level […]. And if, to put it bluntly, you only see plastic toys with a thousand lights and noises and only potato chips and coke, then you have to start off differently.(Int 21)
7.2. Counselling on ECAP: Evidence-Based Knowledge and Support of Parental HL
It is very, very important that I have these conversations [on ECAP] with them during pregnancy, when the woman is full of anticipation and wants to do everything right anyway. Once the child is born and crying and the mother is going completely crazy, it doesn’t really help anymore. It’s very important to find a good time during pregnancy when the woman is eager to learn and the partner is hopefully also there. Then you can reach them really well.(Int 15)
I think you actually only have a chance to really reach a first-time mother. A second or third-time mother feeds as she sees fit anyway.(Int 21)
I always say, “I explain everything. If there’s anything you don’t understand, please ask.” I also always tell parents, “Better to ask me before you Google anything on the Internet. I’m the expert. I can answer that for you and I’ll try to answer it in a way that you understand”.(Int 10)
There are a lot of allergic people. And of course, all parents want the best for their child. It [ECAP] definitely comes up in conversations, mostly when talking about breastfeeding versus bottle feeding. If formula is used, the question is what kind of formula is considered best and then it [ECAP] comes up again when solid food is introduced.(Int 22)
Allergy counselling plays a very, very minor role, mostly with people who are already allergic themselves. That’s been the case since this allergy guideline changed. I think that the behavior in the case of allergy risk or higher allergy risk is actually identical to the recommendations for people with a low allergy risk, so it’s not such a big issue.(Int 19)
It [ECAP] automatically resonates in our work, because we advise on breastfeeding, for example. That is God-given allergy prevention. That’s why it’s always part of our work. And again, when we advise on weaning, it comes quite automatically that you say, okay, start feeding different solid foods in a short time while maintaining the protection of breast milk.(Int 2)
I try to avoid these blueprints a bit, because I find that most children simply don’t eat according to a blueprint. And then the whole text on allergy prevention doesn’t help if this child decides it doesn’t like vegetables.(Int 9)
I think the most important thing is that they don’t get carried away. Instead, they should take a more nuanced look at what information is available and what is really true. And I try to instill a bit of calmness in the parents when it comes to allergy prevention.(Int 14)
I think it would be much more important to strengthen the women in their skills and abilities, for birth or raising children, because the women simply try too hard to follow blueprints and rules, because they read in a self-help book or because it was done like that in the past.(Int 9)
If a woman decides against breastfeeding, then it doesn’t help if I say, the probability of allergies occurring is much higher. This doesn’t help at all. You can’t convert people.(Int 5)
I emphasize the arguments again, why she should not drink coke. And then I leave it at that. I leave the responsibility to the woman. It is her life, her child, her decision.(Int 20)
And also, when women say they don’t want to breastfeed, I say, “That’s not a problem at all. That’s your decision. But it would be great if we could put the baby to the breast at least once in the delivery room.” And no mommy has turned me down yet.(Int 21)
7.3. HL-Sensitive Counselling Techniques and Materials
I really try to avoid medical terms and speak in simple language. […] When I’m in an academic family, it’s sometimes quicker for me to just blurt out the medical terms. But even then, if you are a parent yourself, you sometimes can’t think straight. No matter what you do for a living. And then it’s important that the person advising you simply takes a moment and sits down again and explains it simply, so that everyone understands it.(Int 18)
I don’t have the impression that parents have any inhibitions about asking me anything.(Int 10)
But then I say, “We’ll make a plan for breastfeeding. Now we have just discussed it, and now I would like to know how you would do it?” In other words, you don’t ask directly, but you do it in a hidden way.(Int 15)
You know whether they understood or not. I’m not testing them. I don’t want to behave toward the women like a schoolteacher.(Int 11)
Now, for example, when it comes to breastfeeding, I have various materials with me. For example, I have little balls that represent the stomach. So I always try to make it very vivid.(Int 15)
A good example is always when the children are crying and I take them in my arms and speak to them in a calm voice. Then you simply practice this with the parents.(Int 8)
I have worksheets and I leave those with the mothers, because I know, when you don’t get enough sleep, all you hear is “bla bla” and you can’t remember what you were told.(Int 2)
The women get a lot of information material. I have been working in postnatal care for many years and I know that all this paper stuff is just lying around at home. During the period immediately after birth women are so preoccupied with themselves and the baby that there is very little time to look at brochures, etc.(Int 10)
8. Discussion
9. Practical Implications
10. Strengths and Limitations
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Interview Guide
- How is early childhood allergy prevention relevant in your routine counselling?
- When and with whom do you address this topic?
- What is the most important message you want to convey to parents concerning allergy prevention? Do you make a difference between low- and high-risk groups?
- Which topics also matter in your counselling on early childhood allergy prevention (prompts: e.g., nutrition, living environment, early exposure to allergens)?
- What are your main sources to keep yourself informed about health topics (especially allergy prevention)?
- Are you satisfied with the available information?
- Do you feel well informed? Why? Why not?
- Is there anything that would help to keep up to date?
- How do you handle inconsistent and changing information? (e.g., avoidance of allergens vs. early confrontation with allergens)
- How did/do you feel about a key message of your consultation changing due to new research findings?
- We have just talked about how you keep yourself up to date on health-related recommendations: What are you doing with this knowledge (in your head) to make it applicable/use it for your practice?
- How do you incorporate this knowledge into your daily work?
- Do you pass on specific scientific information to your patients (on ECAP)?
- If yes, could you give an example of how you pass on this information to your patients?
- What helps you to pass on your knowledge to parents?
- Is there anything that could be improved to facilitate health-related counselling of parents?
- Counselling of parents and health literacy
- How do you deal with different patients (e.g., level of knowledge, education, migration background) in counselling and transfer of knowledge? Do you differentiate? Could you give an example?
- How do you assess the level of knowledge and information demand of parents?
- How do you notice that you have to explain a lot/in a way that is easy to understand?
- Do you consciously use strategies to assess what kind of information and support needs parents have? If yes, which ones do you use?
- Do you think parents are well informed regarding allergy prevention? How do you recognize that?
- What previous knowledge or lay conceptions do parents bring up in counselling?
- What opportunities do you see to support parents regarding the access to information and appraising it? Could you give some examples from your everyday practice?
- Do you provide your patients with information sources so they can inform themselves about health topics (e.g., allergy prevention)? Which sources do you consider (not) helpful?
- Do you use certain strategies during counselling to make sure the parents understand everything? (e.g., simple language, avoidance of special language, drawing pictures, teach-back etc.) Do you encourage parents to ask questions? How?
- How do you ensure that parents apply your health behavior recommendations?
- Attitudes towards and experiences with health literacy/health literacy-sensitive care.
- How well do you feel educated/trained to counsel your patients according to their (information) needs?
- Do you personally see a need of further information/training on the issues we have talked about? If yes, what would be important topics to you?
- How should academic results/recommendations be prepared and made available so that you can use them efficiently in consultations?
- Have you heard of the term “health literacy“ in the context of your work or in advanced training courses?
References
- Sørensen, K.; van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Bitzer, E.M.; Sørensen, K. Gesundheitskompetenz—Health Literacy. Gesundheitswesen 2018, 80, 754–766. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Kickbusch, I.; Pelikan, J.M.; Apfel, F.; Tsouros, A.D. Health Literacy: The Solid Facts; World Health Organization: Copenhagen, Denmark, 2013. [Google Scholar]
- Fernandez, D.M.; Larson, J.L.; Zikmund-Fisher, B.J. Associations between health literacy and preventive health behaviors among older adults: Findings from the health and retirement study. BMC Public Health 2016, 16, 596. [Google Scholar] [CrossRef]
- Shaker, M.S.; Schwartz, J.; Ferguson, M. An update on the impact of food allergy on anxiety and quality of life. Curr. Opin. Pediatr. 2017, 29, 497–502. [Google Scholar] [CrossRef]
- Blaiss, M.S.; Hammerby, E.; Robinson, S.; Kennedy-Martin, T.; Buchs, S. The burden of allergic rhinitis and allergic rhinoconjunctivitis on adolescents: A literature review. Ann. Allergy Asthma Immunol. 2018, 121, 43–52.e3. [Google Scholar] [CrossRef]
- Peters, R.L.; Koplin, J.J.; Gurrin, L.C.; Dharmage, S.C.; Wake, M.; Ponsonby, A.-L.; Tang, M.L.K.; Lowe, A.J.; Matheson, M.C.; Dwyer, T.; et al. The prevalence of food allergy and other allergic diseases in early childhood in a population-based study: HealthNuts age 4-year follow-up. J. Allergy Clin. Immunol. 2017, 140, 145–153.e8. [Google Scholar] [CrossRef]
- Asher, M.I.; Montefort, S.; Björkstén, B.; Lai, C.K.W.; Strachan, D.P.; Weiland, S.K.; Williams, H.; ISAAC Phase Three Study Group. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet 2006, 368, 733–743. [Google Scholar] [CrossRef]
- Jarosz, M.; Syed, S.; Błachut, M.; Badura Brzoza, K. Emotional distress and quality of life in allergic diseases. Wiad Lek 2020, 73, 370–373. [Google Scholar] [CrossRef]
- Caffarelli, C.; Di Mauro, D.; Mastrorilli, C.; Bottau, P.; Cipriani, F.; Ricci, G. Solid Food Introduction and the Development of Food Allergies. Nutrients 2018, 10, 1790. [Google Scholar] [CrossRef]
- Schäfer, T.; Bauer, C.-P.; Beyer, K.; Bufe, A.; Friedrichs, F.; Gieler, U.; Gronke, G.; Hamelmann, E.; Hellermann, M.; Kleinheinz, A.; et al. S3-Guideline on allergy prevention: 2014 update: Guideline of the German Society for Allergology and Clinical Immunology (DGAKI) and the German Society for Pediatric and Adolescent Medicine (DGKJ). Allergo J. Int. 2014, 23, 186–199. [Google Scholar] [CrossRef]
- Waggoner, M.R. Parsing the peanut panic: The social life of a contested food allergy epidemic. Soc. Sci. Med. 2013, 90, 49–55. [Google Scholar] [CrossRef]
- Colver, A. Are the dangers of childhood food allergy exaggerated? BMJ 2006, 333, 494–496. [Google Scholar] [CrossRef][Green Version]
- Shenker, N.S. The resurgent influence of big formula. BMJ 2018, 362, k3577. [Google Scholar] [CrossRef]
- Gharachourlo, M.; Mahmoodi, Z.; Akbari Kamrani, M.; Tehranizadeh, M.; Kabir, K. The effect of a health literacy approach to counselling on the lifestyle of women with gestational diabetes: A clinical trial. F1000Research 2018, 7, 282. [Google Scholar] [CrossRef]
- Nawabi, F.; Krebs, F.; Vennedey, V.; Shukri, A.; Lorenz, L.; Stock, S. Health Literacy in Pregnant Women: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 3847. [Google Scholar] [CrossRef]
- Dennis, S.; Williams, A.; Taggart, J.; Newall, A.; Denney-Wilson, E.; Zwar, N.; Shortus, T.; Harris, M.F. Which providers can bridge the health literacy gap in lifestyle risk factor modification education: A systematic review and narrative synthesis. BMC Fam. Pract. 2012, 13, 44. [Google Scholar] [CrossRef]
- Berni Canani, R.; Leone, L.; D’Auria, E.; Riva, E.; Nocerino, R.; Ruotolo, S.; Terrin, G.; Cosenza, L.; Di Costanzo, M.; Passariello, A.; et al. The effects of dietary counseling on children with food allergy: A prospective, multicenter intervention study. J. Acad. Nutr. Diet 2014, 114, 1432–1439. [Google Scholar] [CrossRef]
- Gagliardi, A.R.; Abdallah, F.; Faulkner, G.; Ciliska, D.; Hicks, A. Factors contributing to the effectiveness of physical activity counselling in primary care: A realist systematic review. Patient Educ. Couns. 2015, 98, 412–419. [Google Scholar] [CrossRef]
- Jenssen, B.P.; Bryant-Stephens, T.; Leone, F.T.; Grundmeier, R.W.; Fiks, A.G. Clinical Decision Support Tool for Parental Tobacco Treatment in Primary Care. Pediatrics 2016, 137, e20154185. [Google Scholar] [CrossRef]
- Stevens, Z.; Barlow, C.; Kendrick, D.; Masud, T.; Skelton, D.A.; Dinan-Young, S.; Iliffe, S. Effectiveness of general practice-based physical activity promotion for older adults: Systematic review. Prim. Health Care Res. Dev. 2014, 15, 190–201. [Google Scholar] [CrossRef]
- Farmanova, E.; Bonneville, L.; Bouchard, L. Organizational Health Literacy: Review of Theories, Frameworks, Guides, and Implementation Issues. Inquiry 2018, 55, 46958018757848. [Google Scholar] [CrossRef]
- Brach, C.; Keller, D.; Hernandez, L.; Baur, C.; Parker, R.; Dreyer, B.; Schyve, P.; Lemerise, A.J.; Schillinger, D. Ten Attributes of Health Literate Health Care Organizations. NAM Perspect. 2012, 2, 1–27. [Google Scholar] [CrossRef]
- Allenbaugh, J.; Spagnoletti, C.L.; Rack, L.; Rubio, D.; Corbelli, J. Health Literacy and Clear Bedside Communication: A Curricular Intervention for Internal Medicine Physicians and Medicine Nurses. MedEdPORTAL 2019, 15, 10795. [Google Scholar] [CrossRef]
- Badaczewski, A.; Bauman, L.J.; Blank, A.E.; Dreyer, B.; Abrams, M.A.; Stein, R.E.K.; Roter, D.L.; Hossain, J.; Byck, H.; Sharif, I. Relationship between Teach-back and patient-centered communication in primary care pediatric encounters. Patient Educ. Couns. 2017, 100, 1345–1352. [Google Scholar] [CrossRef]
- Coleman, C.; Hudson, S.; Pederson, B. Prioritized Health Literacy and Clear Communication Practices For Health Care Professionals. Health Lit. Res. Pract. 2017, 1, e91–e99. [Google Scholar] [CrossRef]
- Vamos, C.A.; Thompson, E.L.; Griner, S.B.; Liggett, L.G.; Daley, E.M. Applying Organizational Health Literacy to Maternal and Child Health. Matern. Child Health J. 2019, 23, 597–602. [Google Scholar] [CrossRef]
- De Walt, D.A.; Hink, A. Health literacy and child health outcomes: A systematic review of the literature. Pediatrics 2009, 124 (Suppl. 3), S265–S274. [Google Scholar] [CrossRef]
- DeWalt, D.A.; Dilling, M.H.; Rosenthal, M.S.; Pignone, M.P. Low parental literacy is associated with worse asthma care measures in children. Ambul. Pediatr. 2007, 7, 25–31. [Google Scholar] [CrossRef]
- Stafford, J.D.; Goggins, E.R.; Lathrop, E.; Haddad, L.B. Health Literacy and Associated Outcomes in the Postpartum Period at Grady Memorial Hospital. Matern. Child Health J. 2021, 25, 599–605. [Google Scholar] [CrossRef]
- Gagnon, A.J.; Sandall, J. Individual or group antenatal education for childbirth or parenthood, or both. Cochrane Database Syst. Rev. 2007, 3, CD002869. [Google Scholar] [CrossRef] [PubMed]
- Venter, C.; Clayton, B.; Dean, T. Infant nutrition part 2: The midwife’s role in allergy prevention. Br. J. Midwifery 2008, 16, 791–803. [Google Scholar] [CrossRef]
- BZgA. Hebammenbetreuung—Ihr Gutes Recht|kindergesundheit-Info.de. 2021. Available online: https://www.kindergesundheit-info.de/themen/ernaehrung/0-12-monate/hebammenbetreuung/ (accessed on 1 October 2021).
- Sander, M.; Albrecht, M.; Loos, S.; Stengel, V. Studie zur Hebammenversorgung im Freistaat Bayern. 2018. Available online: https://www.stmgp.bayern.de/meine-themen/fuer-hebammen-und-entbindungspfleger/ (accessed on 1 March 2022).
- Wilhelmova, R.; Hruba, D.; Vesela, L. Key Determinants Influencing the Health Literacy of Pregnant Women in the Czech Republic. Zdr. Varst. 2015, 54, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Royal, C.; Gray, C. Allergy Prevention: An Overview of Current Evidence. Yale J. Biol. Med. 2020, 93, 689–698. [Google Scholar] [PubMed]
- Ritchie, J. (Ed.) Qualitative Research Practice: A Guide for Social Science Students and Researchers; SAGE: Los Angeles, CA, USA, 2011. [Google Scholar]
- Mays, N.; Pope, C. Rigour and qualitative research. BMJ 1995, 311, 109–112. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef]
- Mayring, P. Qualitative Content Analysis: Theoretical Foundation, Basic Procedures and Software Solution. 2014. Available online: https://nbn-resolving.org/urn:nbn:de:0168-ssoar-395173 (accessed on 31 January 2022).
- Schreier, M. Qualitative Content Analysis in Practice; SAGE: London, UK, 2012. [Google Scholar]
- Kuckartz, U. Qualitative Inhaltsanalyse. Methoden, Praxis, Computerunterstützung, 4th ed.; Beltz Juventa: Weinheim, Germany; Basel, Switzerland, 2018. [Google Scholar]
- Patton, M.Q. Qualitative Research & Evaluation Methods, 3rd ed.; SAGE: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Creedy, D.K.; Gamble, J.; Boorman, R.; Allen, J. Midwives’ self-reported knowledge and skills to assess and promote maternal health literacy: A national cross-sectional survey. Women Birth 2020, 34, e188–e195. [Google Scholar] [CrossRef]
- Bass, P.F.; Wilson, J.F.; Griffith, C.H.; Barnett, D.R. Residents’ ability to identify patients with poor literacy skills. Acad. Med. 2002, 77, 1039–1041. [Google Scholar] [CrossRef]
- Dickens, C.; Lambert, B.L.; Cromwell, T.; Piano, M.R. Nurse overestimation of patients’ health literacy. J. Health Commun. 2013, 18 (Suppl. 1), 62–69. [Google Scholar] [CrossRef]
- Safeer, R.S.; Keenan, J. Health Literacy: The Gap between Physicians and Patients. AFP 2005, 72, 463–468. Available online: https://www.aafp.org/afp/2005/0801/p463.html (accessed on 1 March 2022).
- Rogers, E.S.; Wallace, L.S.; Weiss, B.D. Misperceptions of medical understanding in low-literacy patients: Implications for cancer prevention. Cancer Control 2006, 13, 225–229. [Google Scholar] [CrossRef]
- Katz, M.G.; Jacobson, T.A.; Veledar, E.; Kripalani, S. Patient literacy and question-asking behavior during the medical encounter: A mixed-methods analysis. J. Gen. Intern. Med. 2007, 22, 782–786. [Google Scholar] [CrossRef]
- Wilmore, M.; Rodger, D.; Humphreys, S.; Clifton, V.L.; Dalton, J.; Flabouris, M.; Skuse, A. How midwives tailor health information used in antenatal care. Midwifery 2015, 31, 74–79. [Google Scholar] [CrossRef]
- Phelan, S. Pregnancy: A “teachable moment” for weight control and obesity prevention. Am. J. Obstet. Gynecol. 2010, 202, 135.e1–135.e8. [Google Scholar] [CrossRef]
| Inclusion Criteria | Description |
|---|---|
| Catchment area | Rural vs. urban |
| Education | Professional training vs. bachelor’s/master’s |
| Professional experience | 15 years + vs. less than 15 years |
| Midwives (n = 24) | |
|---|---|
| Catchment area | |
| Village/small town (<20,000 inhabitants (IN)) | 14 |
| Medium-sized/large town (>20,000 IN) | 10 |
| Education | |
| Vocational training | 17 |
| bachelor’s/master’s | 7 |
| Professional experience | |
| <10 years | 12 |
| >10 years | 12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
von Sommoggy, J.; Grepmeier, E.-M.; Curbach, J. Health Literacy-Sensitive Counselling on Early Childhood Allergy Prevention: Results of a Qualitative Study on German Midwives’ Perspectives. Int. J. Environ. Res. Public Health 2022, 19, 4182. https://doi.org/10.3390/ijerph19074182
von Sommoggy J, Grepmeier E-M, Curbach J. Health Literacy-Sensitive Counselling on Early Childhood Allergy Prevention: Results of a Qualitative Study on German Midwives’ Perspectives. International Journal of Environmental Research and Public Health. 2022; 19(7):4182. https://doi.org/10.3390/ijerph19074182
Chicago/Turabian Stylevon Sommoggy, Julia, Eva-Maria Grepmeier, and Janina Curbach. 2022. "Health Literacy-Sensitive Counselling on Early Childhood Allergy Prevention: Results of a Qualitative Study on German Midwives’ Perspectives" International Journal of Environmental Research and Public Health 19, no. 7: 4182. https://doi.org/10.3390/ijerph19074182
APA Stylevon Sommoggy, J., Grepmeier, E.-M., & Curbach, J. (2022). Health Literacy-Sensitive Counselling on Early Childhood Allergy Prevention: Results of a Qualitative Study on German Midwives’ Perspectives. International Journal of Environmental Research and Public Health, 19(7), 4182. https://doi.org/10.3390/ijerph19074182






