Prevalence and Risk Factors for Hypertension among Myanmar Migrant Workers in Thailand
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
Population and Study Population
2.2. Research Instruments
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Characteristics of the Study Participants
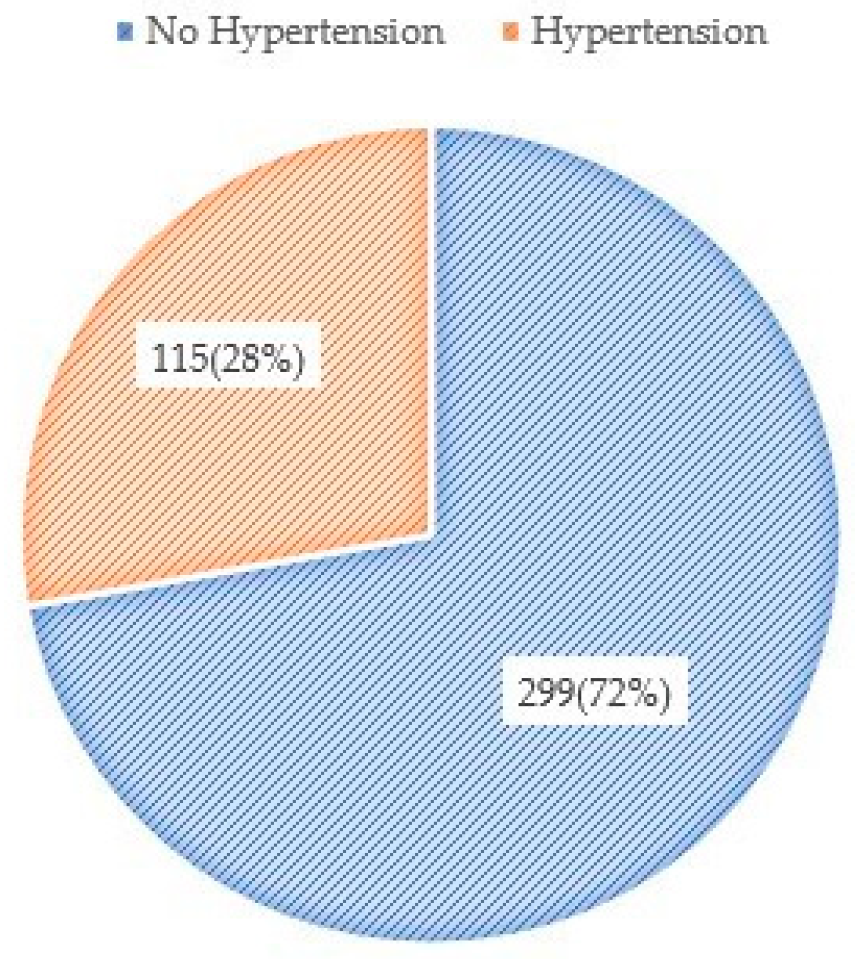
3.2. Prevalence of Hypertension and Associated Factors
4. Discussion
Limitation and Strength of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization (WHO) Thailand. Hypertension Care in Thailand Best Practices and Challenges; WHO: Nonthaburi, Thailand, 2019. [Google Scholar]
- Chalmers, J.; MacMahon, S.; Mancia, G.; Whitworth, J.; Beilin, L.; Hansson, L.; Neal, B.; Rodgers, A.; Ni Mhurchu, C.; Clark, T. 1999 World Health Organization-International Society of Hypertension Guidelines for the management of hypertension. Guidelines sub-committee of the World Health Organization. Clin. Exp. Hypertens. 1999, 21, 1009–1060. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, J.M.A.; Hedt, K.H.; Omar, O.M.; Davies, J.I. Hypertension and diabetes in Zanzibar–prevalence and access to care. BMC Public Health 2020, 20, 1352. [Google Scholar] [CrossRef] [PubMed]
- Thai Hypertension Society. 2019 Thai Guidelines on The Treatment of Hypertension; Thai Hypertension Society: Chiang Mai, Thailand, 2019. [Google Scholar]
- Smith, H.; Lim, R.; Harkins, I.B. 01 Thailand Migration Profile. In Thailand Migration Report 2019; International Organization for Migration: Grand-Saconnex, Switzerland, 2019. [Google Scholar]
- International Organization for Migration. Non-Communicable Diseases and Migration; International Organization for Migration: Grand-Saconnex, Switzerland, 2018. [Google Scholar]
- Agyemang, C.; Born, B.-J.V.D. Non-communicable diseases in migrants: An expert review. J. Travel Med. 2018, 26, tay107. [Google Scholar] [CrossRef] [PubMed]
- United Nations Thematic Working Group on Migration in Thailand. Thailand Migration Report; United Nations Thematic Working Group on Migration in Thailand: Bangkok, Thailand, 2019. [Google Scholar]
- Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study. Lancet 2020, 396, 1204–1222. [Google Scholar]
- The White House. Fact Sheet: President Obama’s Precision Medicine Initiative. Available online: https://www.whitehouse.gov/the-press-office/2015/01/30/fact-sheet-president-obama-s-precision-medicine-initiativeOfficeofScience (accessed on 14 June 2016).
- Jones, N.R.; McCormack, T.; Constanti, M.; McManus, R.J. Diagnosis and management of hypertension in adults: NICE guideline update. Br. J. Gen. Pr. 2020, 70, 90–91. [Google Scholar] [CrossRef] [PubMed]
- WHO. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; Health Communications Australia: Sydney, Australia, 2000. [Google Scholar]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation, Geneva, 8–11 December 2008; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour: Web Annex: Evidence Profiles; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Charoendee, K.; Sriratanaban, J.; Aekplakorn, W.; Hanvoravongchai, P. Assessment of population coverage of hypertension screening in Thailand based on the effective coverage framework. BMC Health Serv. Res. 2018, 18, 208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aung, M.N.; Lorga, T.; Srikrajang, J.; Promtingkran, N.; Kreuangchai, S.; Tonpanya, W.; Vivarakanon, P.; Jaiin, P.; Praipaksin, N.; Payaprom, A. Assessing awareness and knowledge of hypertension in an at-risk population in the Karen ethnic rural community, Thasongyang, Thailand. Int. J. Gen. Med. 2012, 5, 553. [Google Scholar] [CrossRef] [Green Version]
- Verma, N.; Su, C.; Chan, C.; Muennig, P. Between “Voluntary Migrants” and War Refugees: The Health of the Shan Burmese Migrant Workers in Northern Thailand. J. Immigr. Refug. Stud. 2011, 9, 452–459. [Google Scholar] [CrossRef]
- Commodore-Mensah, Y.; Selvin, E.; Aboagye, J.; Turkson-Ocran, R.-A.; Li, X.; Himmelfarb, C.D.; Ahima, R.S.; Cooper, L.A. Hypertension, overweight/obesity, and diabetes among immigrants in the United States: An analysis of the 2010–2016 National Health Interview Survey. BMC Public Health 2018, 18, 773. [Google Scholar] [CrossRef] [Green Version]
- Cohen, L.; Curhan, G.C.; Forman, J.P.; Cohen, L.; Curhan, G.C.; Forman, J.P. Influence of age on the association between lifestyle factors and risk of hypertension. J. Am. Soc. Hypertens. 2012, 6, 284–290. [Google Scholar] [CrossRef]
- McEniery, C.M.; Wilkinson, I.B.; Avolio, A.P. Age, hypertension and arterial function. Clin. Exp. Pharmacol. Physiol. 2007, 34, 665–671. [Google Scholar] [CrossRef] [PubMed]
- Lacruz, M.E.; Kluttig, A.; Hartwig, S.; Löer, M.; Tiller, D.; Greiser, K.H.; Werdan, K.; Haerting, J. Prevalence and incidence of hypertension in the general adult population: Results of the CARLA-cohort study. Medicine 2015, 94, e952. [Google Scholar] [CrossRef]
- Song, J.-J.; Ma, Z.; Wang, J.; Chen, L.-X.; Zhong, J.-C. Gender differences in hypertension. J. Cardiovasc. Transl. Res. 2020, 13, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Liew, S.J.; Lee, J.T.; Tan, C.S.; Koh, C.H.G.; Van Dam, R.; Müller-Riemenschneider, F. Sociodemographic factors in relation to hypertension prevalence, awareness, treatment and control in a multi-ethnic Asian population: A cross-sectional study. BMJ Open 2019, 9, e025869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bjertness, M.B.; Htet, A.S.; Meyer, H.E.; Htike, M.M.T.; Zaw, K.K.; Oo, W.M.; Latt, T.S.; Sherpa, L.Y.; Bjertness, E. Prevalence and determinants of hypertension in Myanmar—A nationwide cross-sectional study. BMC Public Health 2016, 16, 590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aung, T.N.N.; Shirayama, Y.; Moolphate, S.; Aung, M.N.; Lorga, T.; Yuasa, M. Health risk behaviors, musculoskeletal disorders and associated cultural adaptation, depression: A survey among Myanmar migrant workers in Chiangmai, Northern Thailand. Int. J. Gen. Med. 2019, 12, 283–292. [Google Scholar] [CrossRef] [Green Version]
- Aung, T.N.N.; Shirayama, Y.; Moolphate, S.; Lorga, T.; Yuasa, M.; Aung, M.N. Acculturation and Its Effects on Health Risk Behaviors Among Myanmar Migrant Workers: A Cross-Sectional Survey in Chiang Mai, Northern Thailand. Int. J. Environ. Res. Public Health 2020, 17, 5108. [Google Scholar] [CrossRef] [PubMed]
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- WHO. WHO Report on the Global Tobacco Epidemic 2021: Addressing New and Emerging Products; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Leone, A. Smoking and hypertension. J. Cardiol. Curr. Res. 2015, 2, 00057. [Google Scholar]
- Gao, K.; Shi, X.; Wang, W. The life-course impact of smoking on hypertension, myocardial infarction and respiratory diseases. Sci. Rep. 2017, 7, 4330. [Google Scholar] [CrossRef] [Green Version]
- Nawi, A.M.; Mohammad, Z.; Jetly, K.; Razak, M.A.A.; Ramli, N.S.; Ibadullah, W.A.H.W.; Ahmad, N. The Prevalence and Risk Factors of Hypertension among the Urban Population in Southeast Asian Countries: A Systematic Review and Meta-Analysis. Int. J. Hypertens. 2021, 2021, 6657003. [Google Scholar] [CrossRef]
- Neupane, D.; McLachlan, C.S.; Sharma, R.; Gyawali, B.; Khanal, V.; Mishra, S.R.; Christensen, B.; Kallestrup, P. Prevalence of hypertension in member countries of South Asian Association for Regional Cooperation (SAARC): Systematic review and meta-analysis. Medicine 2014, 93, e74. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.B.; Suh, I.L.; Singh, V.P.; Chaithiraphan, S.; Laothavorn, P.; Sy, R.G.; A Babilonia, N.; Rahman, A.; Sheikh, S.; Tomlinson, B.; et al. Hypertension and stroke in Asia: Prevalence, control and strategies in developing countries for prevention. J. Hum. Hypertens. 2000, 14, 749–763. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- San Lau, L.; Samari, G.; Moresky, R.T.; Casey, S.E.; Kachur, S.P.; Roberts, L.F.; Zard, M. COVID-19 in humanitarian settings and lessons learned from past epidemics. Nat. Med. 2020, 26, 647–648. [Google Scholar]
| Hypertension | |||
|---|---|---|---|
| Variables | Yes (n%) | No (n%) | Total (n%) |
| Age | 29.45 ± 9.03 years | ||
| Sex | |||
| Male | 84 (73.0) | 147 (49.2) | 231 (55.8) |
| Female | 31 (27.0) | 152 (50.8) | 183 (44.2) |
| Marital status | |||
| Single | 25 (21.7) | 99 (33.1) | 124 (30.0) |
| Married | 90 (78.3) | 200 (66.9) | 290 (70.0) |
| Education | |||
| No formal education | 61 (53.0) | 142 (47.5) | 203 (49.0) |
| Primary school completed | 32 (19.1) | 81 (27.1) | 113 (27.3) |
| Secondary school and above | 22 (19.1) | 76 (25.4) | 98 (23.7) |
| Years of stay in Thailand | 6.36 ± 5.70 years | ||
| Types of job | |||
| Cleaning/household works | 29 (25.2) | 97 (32.4) | 126 (30.4) |
| Construction | 43 (37.4) | 82 (27.4) | 125 (30.2) |
| Agriculture | 29 (25.2) | 80 (26.8) | 109 (26.3) |
| Factory | 13 (11.3) | 26 (8.7) | 39 (9.4) |
| Currently unemployed | 1 (0.9) | 14 (4.7) | 15 (3.6) |
| Diabetes | |||
| Yes | 2 (1.7) | 2 (0.7) | 4 (1.0) |
| No | 109 (94.8) | 283 (94.6) | 392 (94.7) |
| Never checked | 4 (3.5) | 14 (4.7) | 18 (4.3) |
| Sleeping hours per night | |||
| <8 h | 83 (72.2) | 199 (66.6) | 282 (68.1) |
| >8 h | 32 (27.8) | 100 (33.4) | 132 (31.9) |
| Exercise | |||
| No | 96 (83.5) | 255 (85.3) | 351 (84.8) |
| Yes | 19 (16.5) | 44 (14.7) | 63 (15.2) |
| Current smoking | |||
| No | 69 (60.0) | 36 (78.9) | 305 (73.7) |
| Yes | 46 (40.0) | 63 (21.1) | 109 (26.3) |
| Current alcohol drinking | |||
| No | 46 (40.0) | 199 (66.6) | 245 (59.2) |
| Yes | 69 (60.0) | 100 (33.4) | 169 (40.8) |
| Central obesity | |||
| No | 79 (69.3) | 231 (77.3) | 310 (75.1) |
| Yes | 35 (30.7) | 68 (22.7) | 103 (24.9) |
| Body Mass Index (BMI) | |||
| Normal 18.5–24.9 | 68 (59.1) | 260 (87.0) | 328 (79.2) |
| Overweight 25–29.9 | 37 (32.2) | 31 (10.4) | 68 (16.4) |
| Obese ≥ 30 | 10 (8.7) | 8 (2.7) | 18 (4.3) |
| Hypertension | ||||
|---|---|---|---|---|
| 95% Confidence Interval | ||||
| n (%) | Adjusted OR | Lower | Upper | |
| Age (years) | 1.10 ** | 1.07 | 1.13 | |
| Sex | ||||
| Female | 31 (16.9) | Referent | ||
| Male | 84 (36.4) | 2.42 * | 1.12 | 5.24 |
| Current alcohol drinking | ||||
| No | 46 (18.8) | Referent | ||
| Yes | 69 (40.8) | 2.80 * | 1.41 | 5.57 |
| Current smoking | ||||
| No | 69 (22.6) | Referent | ||
| Yes | 46 (42.2) | 1.21 | 0.64 | 2.29 |
| Exercise | ||||
| Yes | 19 (30.2) | Referent | ||
| No | 96 (27.4) | 1.26 | 0.62 | 2.56 |
| Central obesity | ||||
| No | 79 (25.5) | Referent | ||
| Yes | 35 (34.0) | 1.18 | 0.61 | 2.29 |
| Body Mass Index | ||||
| Normal 18.5–24.9 | 68 (20.7) | Referent | ||
| Overweight 25–29.9 | 37 (54.4) | 5.88 ** | 2.99 | 11.55 |
| Obese ≥ 30 | 10 (55.6) | 6.10 ** | 1.96 | 18.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aung, T.N.N.; Shirayama, Y.; Moolphate, S.; Lorga, T.; Jamnongprasatporn, W.; Yuasa, M.; Aung, M.N. Prevalence and Risk Factors for Hypertension among Myanmar Migrant Workers in Thailand. Int. J. Environ. Res. Public Health 2022, 19, 3511. https://doi.org/10.3390/ijerph19063511
Aung TNN, Shirayama Y, Moolphate S, Lorga T, Jamnongprasatporn W, Yuasa M, Aung MN. Prevalence and Risk Factors for Hypertension among Myanmar Migrant Workers in Thailand. International Journal of Environmental Research and Public Health. 2022; 19(6):3511. https://doi.org/10.3390/ijerph19063511
Chicago/Turabian StyleAung, Thin Nyein Nyein, Yoshihisa Shirayama, Saiyud Moolphate, Thaworn Lorga, Warunyou Jamnongprasatporn, Motoyuki Yuasa, and Myo Nyein Aung. 2022. "Prevalence and Risk Factors for Hypertension among Myanmar Migrant Workers in Thailand" International Journal of Environmental Research and Public Health 19, no. 6: 3511. https://doi.org/10.3390/ijerph19063511
APA StyleAung, T. N. N., Shirayama, Y., Moolphate, S., Lorga, T., Jamnongprasatporn, W., Yuasa, M., & Aung, M. N. (2022). Prevalence and Risk Factors for Hypertension among Myanmar Migrant Workers in Thailand. International Journal of Environmental Research and Public Health, 19(6), 3511. https://doi.org/10.3390/ijerph19063511








