MicroRNA-21 Expression as a Prognostic Biomarker in Oral Cancer: Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Sources of Information, Research and Selection
2.4. Data Collection Process and Data Characteristics
2.5. Risk of Bias in Individual Studies, Summary Measures, Summary of Results, Risk of Bias between Studies, and Additional Measures
3. Results
3.1. Selection of Studies
3.2. Data Characteristics
- Primary outcome: HR for OS between high and low miR-21 expression.
- Secondary outcome: HR for DFS between high and low miR-21 expression.
- Tertiary outcome: HR for CSS between high and low miR-21 expression.
- Quaternary outcome: HR for RFS between high and low miR-21 expression.
3.3. Risk of Bias in Studies
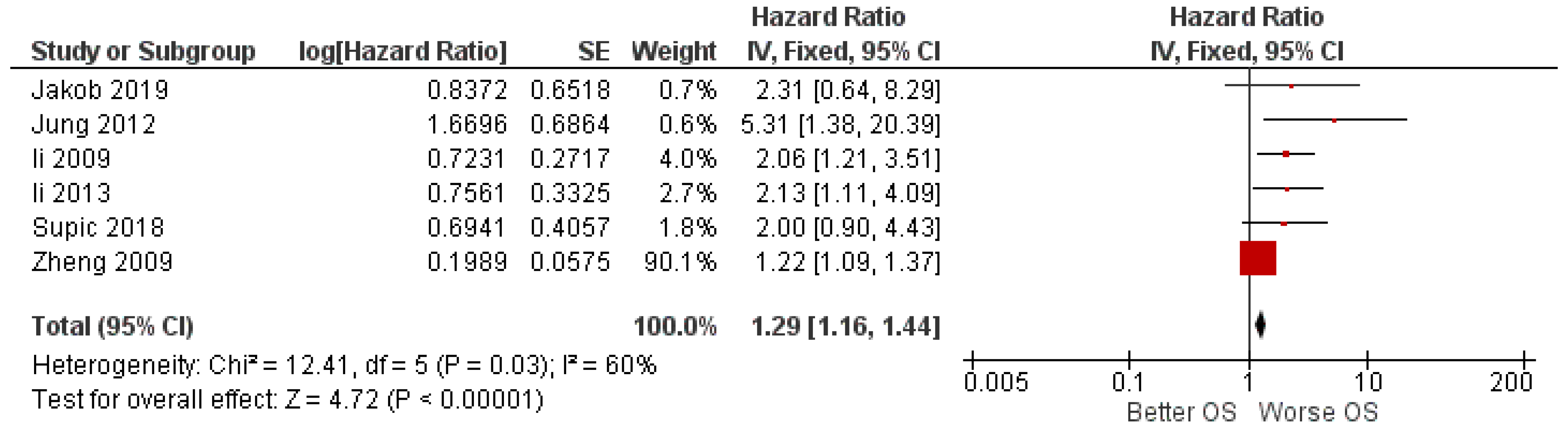
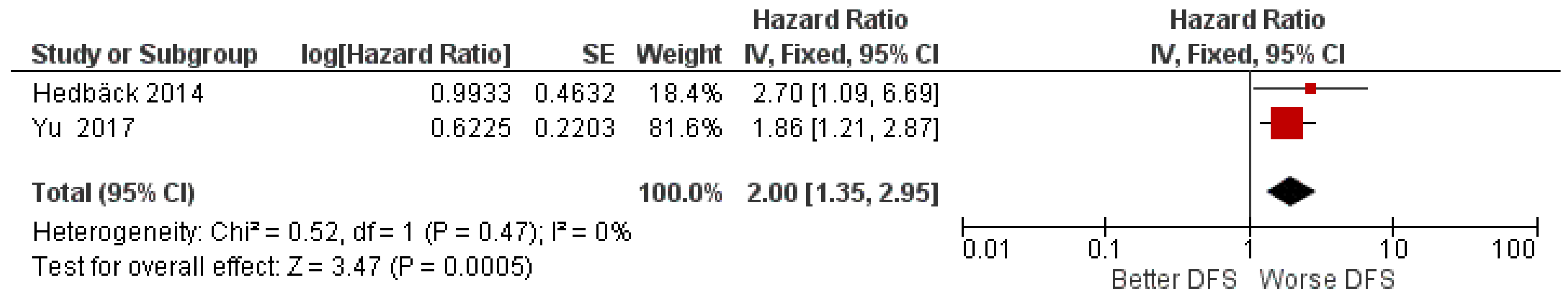
3.4. Primary Outcome and Secondary Outcome
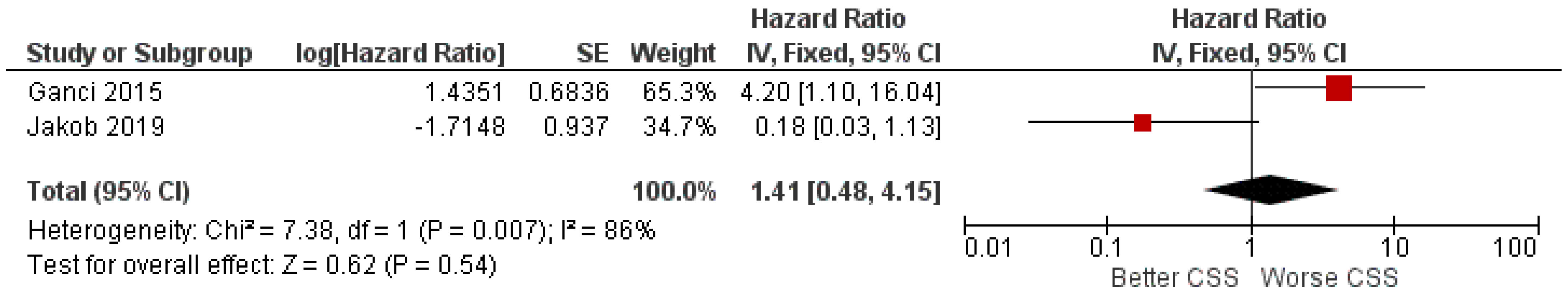
3.5. Tertiary and Quaternary Outcomes
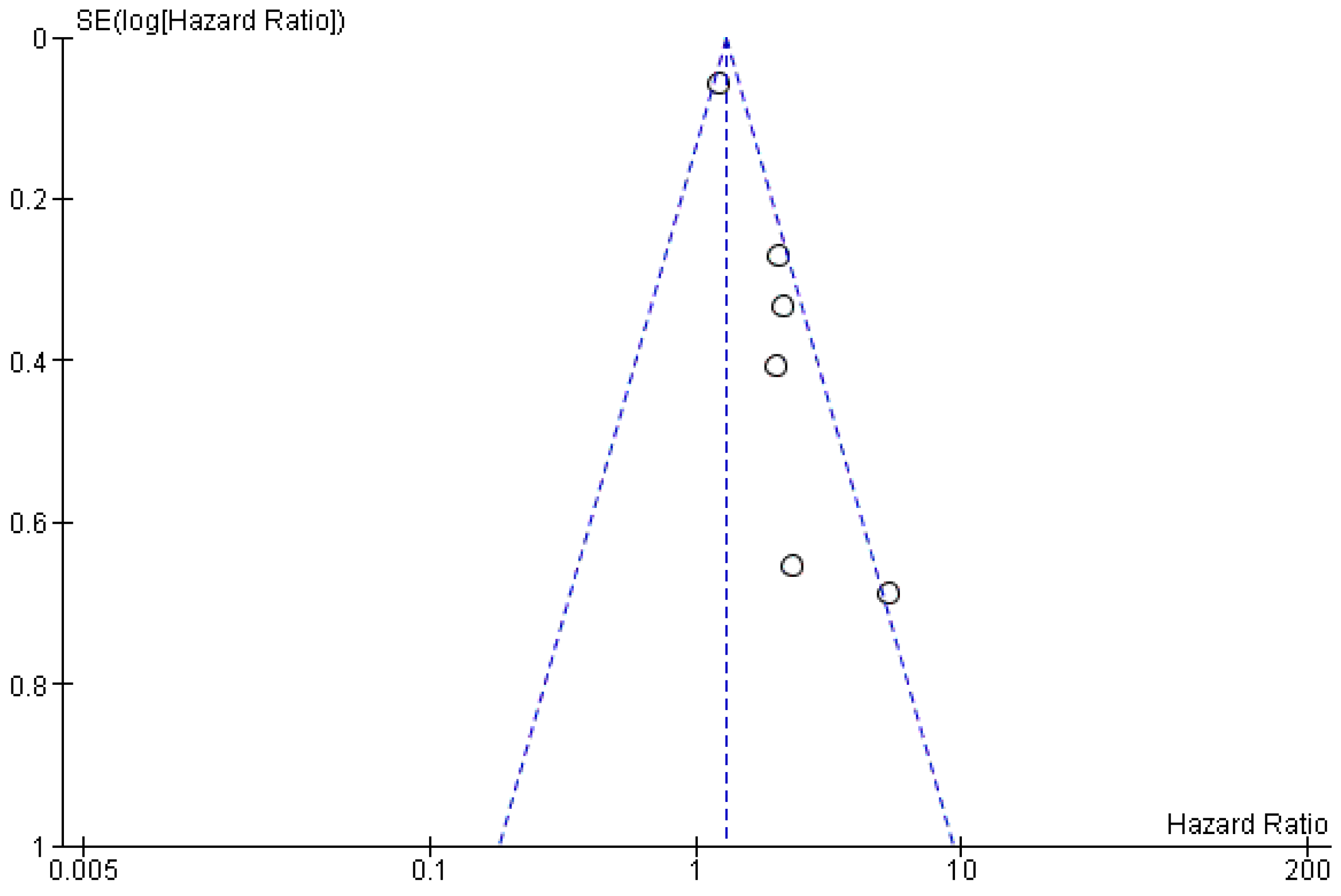
3.6. Risk of Bias across Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Lissoni, A.; Agliardi, E.; Peri, A.; Marchioni, R.; Abati, S. Oral microbiome and mucosal trauma as risk factors for oral cancer: Beyond alcohol and tobacco. A literature review. J. Biol. Regul. Homeost. Agents 2020, 34, 11–18. [Google Scholar] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohideen, K.; Krithika, C.; Jeddy, N.; Balakrishnan, T.; Bharathi, R.; Sankari, S.L. A Meta-analysis of Oral Squamous Cell Carcinoma in Young Adults with a Comparison to the Older Group Patients (2014-2019). Contemp. Clin. Dent. 2021, 12, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Carreras-Torras, C.; Gay-Escoda, C. Techniques for early diagnosis of oral squamous cell carcinoma: Systematic review. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e305–e315. [Google Scholar] [CrossRef] [PubMed]
- Covrig, V.I.; Lazăr, D.E.; Costan, V.V.; Postolică, R.; Ioan, B.G. The Psychosocial Role of Body Image in the Quality of Life of Head and Neck Cancer Patients. What Does the Future Hold?-A Review of the Literature. Medicina 2021, 57, 1078. [Google Scholar] [CrossRef] [PubMed]
- De Cicco, D.; Tartaro, G.; Ciardiello, F.; Fasano, M.; Rauso, R.; Fiore, F.; Spuntarelli, C.; Troiano, A.; Lo Giudice, G.; Colella, G. Health-Related Quality of Life in Oral Cancer Patients: Scoping Review and Critical Appraisal of Investigated Determinants. Cancers 2021, 13, 4398. [Google Scholar] [CrossRef]
- Kowalski, L.P.; Carvalho, A.L. Natural history of untreated head and neck cancer. Eur. J. Cancer 2000, 36, 1032–1037. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2016. CA Cancer J. Clin. 2016, 66, 7–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Núñez-Acurio, D.; Bravo, D.; Aguayo, F. Epstein-Barr Virus-Oral Bacterial Link in the Development of Oral Squamous Cell Carcinoma. Pathogens 2020, 9, 1059. [Google Scholar] [CrossRef] [PubMed]
- Vyhnalova, T.; Danek, Z.; Gachova, D.; Linhartova, P.B. The Role of the Oral Microbiota in the Etiopathogenesis of Oral Squamous Cell Carcinoma. Microorganisms 2021, 9, 1549. [Google Scholar] [CrossRef] [PubMed]
- Borsetto, D.; Fussey, J.; Fabris, L.; Bandolin, L.; Gaudioso, P.; Phillips, V.; Polesel, J.; Boscolo-Rizzo, P. HCV infection and the risk of head and neck cancer: A meta-analysis. Oral Oncol. 2020, 109, 104869. [Google Scholar] [CrossRef]
- Muzio, L.L.; Ballini, A.; Cantore, S.; Bottalico, L.; Charitos, I.A.; Ambrosino, M.; Nocini, R.; Malcangi, A.; Dioguardi, M.; Cazzolla, A.P.; et al. Overview of Candida albicans and Human Papillomavirus (HPV) Infection Agents and their Biomolecular Mechanisms in Promoting Oral Cancer in Pediatric Patients. BioMed Res. Int. 2021, 2021, 7312611. [Google Scholar] [CrossRef] [PubMed]
- Bajbouj, K.; Al-Ali, A.; Ramakrishnan, R.K.; Saber-Ayad, M.; Hamid, Q. Histone Modification in NSCLC: Molecular Mechanisms and Therapeutic Targets. Int. J. Mol. Sci. 2021, 22, 11701. [Google Scholar] [CrossRef] [PubMed]
- Hasbullah, H.H.; Musa, M. Gene Therapy Targeting p53 and KRAS for Colorectal Cancer Treatment: A Myth or the Way Forward? Int. J. Mol. Sci. 2021, 22, 11941. [Google Scholar] [CrossRef]
- Hu, J.; Cao, J.; Topatana, W.; Juengpanich, S.; Li, S.; Zhang, B.; Shen, J.; Cai, L.; Cai, X.; Chen, M. Targeting mutant p53 for cancer therapy: Direct and indirect strategies. J. Hematol. Oncol. 2021, 14, 157. [Google Scholar] [CrossRef] [PubMed]
- Kasikci, Y.; Gronemeyer, H. Complexity against current cancer research—Are we on the wrong track? Int. J. Cancer 2021. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.K.; Sun, X.J.; Gao, X.D.; Qian, Y.; Wang, L.; Zhao, W.L. Methylation alterations and advance of treatment in lymphoma. Front. Biosci. 2021, 26, 602–613. [Google Scholar] [CrossRef]
- Otmani, K.; Lewalle, P. Tumor Suppressor miRNA in Cancer Cells and the Tumor Microenvironment: Mechanism of Deregulation and Clinical Implications. Front. Oncol. 2021, 11, 708765. [Google Scholar] [CrossRef] [PubMed]
- Perri, P.; Ponzoni, M.; Corrias, M.V.; Ceccherini, I.; Candiani, S.; Bachetti, T. A Focus on Regulatory Networks Linking MicroRNAs, Transcription Factors and Target Genes in Neuroblastoma. Cancers 2021, 13, 5528. [Google Scholar] [CrossRef] [PubMed]
- Rozenberg, J.M.; Zvereva, S.; Dalina, A.; Blatov, I.; Zubarev, I.; Luppov, D.; Bessmertnyi, A.; Romanishin, A.; Alsoulaiman, L.; Kumeiko, V.; et al. The p53 family member p73 in the regulation of cell stress response. Biol. Direct 2021, 16, 23. [Google Scholar] [CrossRef]
- Sahin, I.; George, A.; Seyhan, A.A. Therapeutic Targeting of Alternative RNA Splicing in Gastrointestinal Malignancies and Other Cancers. Int. J. Mol. Sci. 2021, 22, 11790. [Google Scholar] [CrossRef]
- Fu, X.; Han, Y.; Wu, Y.; Zhu, X.; Lu, X.; Mao, F.; Wang, X.; He, X.; Zhao, Y.; Zhao, Y. Prognostic role of microRNA-21 in various carcinomas: A systematic review and meta-analysis. Eur. J. Clin. Investig. 2011, 41, 1245–1253. [Google Scholar] [CrossRef] [PubMed]
- Troiano, G.; Boldrup, L.; Ardito, F.; Gu, X.; Lo Muzio, L.; Nylander, K. Circulating miRNAs from blood, plasma or serum as promising clinical biomarkers in oral squamous cell carcinoma: A systematic review of current findings. Oral Oncol. 2016, 63, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Jamali, Z.; Asl Aminabadi, N.; Attaran, R.; Pournagiazar, F.; Ghertasi Oskouei, S.; Ahmadpour, F. MicroRNAs as prognostic molecular signatures in human head and neck squamous cell carcinoma: A systematic review and meta-analysis. Oral Oncol. 2015, 51, 321–331. [Google Scholar] [CrossRef]
- Troiano, G.; Mastrangelo, F.; Caponio, V.C.A.; Laino, L.; Cirillo, N.; Lo Muzio, L. Predictive Prognostic Value of Tissue-Based MicroRNA Expression in Oral Squamous Cell Carcinoma: A Systematic Review and Meta-analysis. J. Dent. Res. 2018, 97, 759–766. [Google Scholar] [CrossRef] [PubMed]
- Dioguardi, M.; Caloro, G.A.; Laino, L.; Alovisi, M.; Sovereto, D.; Crincoli, V.; Aiuto, R.; Coccia, E.; Troiano, G.; Lo Muzio, L. Circulating miR-21 as a Potential Biomarker for the Diagnosis of Oral Cancer: A Systematic Review with Meta-Analysis. Cancers 2020, 12, 936. [Google Scholar] [CrossRef] [Green Version]
- Al Rawi, N.; Elmabrouk, N.; Abu Kou, R.; Mkadmi, S.; Rizvi, Z.; Hamdoon, Z. The role of differentially expressed salivary microRNA in oral squamous cell carcinoma. A systematic review. Arch. Oral Biol. 2021, 125, 105108. [Google Scholar] [CrossRef]
- Sannigrahi, M.K.; Sharma, R.; Panda, N.K.; Khullar, M. Role of non-coding RNAs in head and neck squamous cell carcinoma: A narrative review. Oral Dis. 2018, 24, 1417–1427. [Google Scholar] [CrossRef]
- Ribas, J.; Ni, X.; Castanares, M.; Liu, M.M.; Esopi, D.; Yegnasubramanian, S.; Rodriguez, R.; Mendell, J.T.; Lupold, S.E. A novel source for miR-21 expression through the alternative polyadenylation of VMP1 gene transcripts. Nucleic Acids Res. 2012, 40, 6821–6833. [Google Scholar] [CrossRef] [Green Version]
- Surina, S.; Fontanella, R.A.; Scisciola, L.; Marfella, R.; Paolisso, G.; Barbieri, M. miR-21 in Human Cardiomyopathies. Front. Cardiovasc. Med. 2021, 8, 767064. [Google Scholar] [CrossRef] [PubMed]
- Kumarswamy, R.; Volkmann, I.; Thum, T. Regulation and function of miRNA-21 in health and disease. RNA Biol. 2011, 8, 706–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Supic, G.; Zeljic, K.; Rankov, A.D.; Kozomara, R.; Nikolic, A.; Radojkovic, D.; Magic, Z. miR-183 and miR-21 expression as biomarkers of progression and survival in tongue carcinoma patients. Clin. Oral Investig. 2018, 22, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Jakob, M.; Mattes, L.M.; Küffer, S.; Unger, K.; Hess, J.; Bertlich, M.; Haubner, F.; Ihler, F.; Canis, M.; Weiss, B.G.; et al. MicroRNA expression patterns in oral squamous cell carcinoma: Hsa-mir-99b-3p and hsa-mir-100-5p as novel prognostic markers for oral cancer. Head Neck 2019, 41, 3499–3515. [Google Scholar] [CrossRef]
- Xie, Y.; Wu, J. MicroRNA-21 as prognostic molecular signatures in oral cancer: A meta-analysis. Int. J. Clin. Exp. Med. 2017, 10, 9848–9856. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [Green Version]
- McShane, L.M.; Altman, D.G.; Sauerbrei, W.; Taube, S.E.; Gion, M.; Clark, G.M. REporting recommendations for tumor MARKer prognostic studies (REMARK). Nat. Clin. Pract. Oncol. 2005, 2, 416–422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, H.M.; Phillips, B.L.; Patel, R.S.; Cohen, D.M.; Jakymiw, A.; Kong, W.W.; Cheng, J.Q.; Chan, E.K.L. Keratinization-associated miR-7 and miR-21 regulate tumor suppressor reversion-inducing cysteine-rich protein with kazal motifs (RECK) in oral cancer. J. Biol. Chem. 2012, 287, 29261–29272. [Google Scholar] [CrossRef] [Green Version]
- Kawakita, A.; Yanamoto, S.; Yamada, S.; Naruse, T.; Takahashi, H.; Kawasaki, G.; Umeda, M. MicroRNA-21 promotes oral cancer invasion via the Wnt/beta-catenin pathway by targeting DKK2. Pathol. Oncol. Res. 2014, 20, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Hedbäck, N.; Jensen, D.H.; Specht, L.; Fiehn, A.M.K.; Therkildsen, M.H.; Friis-Hansen, L.; Dabelsteen, E.; Von Buchwald, C. miR-21 expression in the tumor stroma of oral squamous cell carcinoma: An independent biomarker of disease free survival. PLoS ONE 2014, 9, e95193. [Google Scholar] [CrossRef]
- Yu, E.H.; Tu, H.F.; Wu, C.H.; Yang, C.C.; Chang, K.W. MicroRNA-21 promotes perineural invasion and impacts survival in patients with oral carcinoma. J. Chin. Med. Assoc. 2017, 80, 383–388. [Google Scholar] [CrossRef]
- Li, S.; Zhou, X.; Zhang, Q.; Zhang, L. Abnormal expression of STAT3 and miRNA-21 in oral squamous cell carcinoma. Chin. J. Clin. Oncol. 2013, 40, 323–327. [Google Scholar] [CrossRef]
- Zheng, G.; Li, N.; Jia, X.; Peng, C.; Luo, L.; Deng, Y.; Yin, J.; Song, Y.; Liu, H.; Lu, M.; et al. MYCN-mediated miR-21 overexpression enhances chemo-resistance via targeting CADM1 in tongue cancer. J. Mol. Med. 2016, 94, 1129–1141. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Huang, H.; Sun, L.; Yang, M.; Pan, C.; Chen, W.; Wu, D.; Lin, Z.; Zeng, C.; Yao, Y.; et al. MiR-21 indicates poor prognosis in tongue squamous cell carcinomas as an apoptosis inhibitor. Clin. Cancer Res. 2009, 15, 3998–4008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganci, F.; Sacconi, A.; Manciocco, V.; Sperduti, I.; Battaglia, P.; Covello, R.; Muti, P.; Strano, S.; Spriano, G.; Fontemaggi, G.; et al. MicroRNA expression as predictor of local recurrence risk in oral squamous cell carcinoma. Head Neck 2016, 38 (Suppl. 1), E189–E197. [Google Scholar] [CrossRef] [PubMed]
- Tierney, J.F.; Stewart, L.A.; Ghersi, D.; Burdett, S.; Sydes, M.R. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007, 8, 16. [Google Scholar] [CrossRef] [Green Version]
- Ko, Y.H.; Won, H.S.; Sun, D.S.; An, H.J.; Jeon, E.K.; Kim, M.S.; Lee, H.H.; Kang, J.H.; Jung, C.K. Human papillomavirus-stratified analysis of the prognostic role of miR-21 in oral cavity and oropharyngeal squamous cell carcinoma. Pathol. Int. 2014, 64, 499–507. [Google Scholar] [CrossRef]
- Riley, R.D.; Hayden, J.A.; Steyerberg, E.W.; Moons, K.G.; Abrams, K.; Kyzas, P.A.; Malats, N.; Briggs, A.; Schroter, S.; Altman, D.G.; et al. Prognosis Research Strategy (PROGRESS) 2: Prognostic factor research. PLoS Med. 2013, 10, e1001380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voortman, J.; Goto, A.; Mendiboure, J.; Sohn, J.J.; Schetter, A.J.; Saito, M.; Dunant, A.; Pham, T.C.; Petrini, I.; Lee, A.; et al. MicroRNA expression and clinical outcomes in patients treated with adjuvant chemotherapy after complete resection of non-small cell lung carcinoma. Cancer Res. 2010, 70, 8288–8298. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Chen, J.; Chen, X.; Tang, J.; Guo, H.; Wang, X.; Qian, J.; Luo, G.; He, F.; Lu, X.; et al. Serum miRNAs as predictive and preventive biomarker for pre-clinical hepatocellular carcinoma. Cancer Lett. 2016, 373, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Dufour, A.; Palermo, G.; Zellmeier, E.; Mellert, G.; Duchateau-Nguyen, G.; Schneider, S.; Benthaus, T.; Kakadia, P.M.; Spiekermann, K.; Hiddemann, W.; et al. Inactivation of TP53 correlates with disease progression and low miR-34a expression in previously treated chronic lymphocytic leukemia patients. Blood 2013, 121, 3650–3657. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| First Author, Date | Country | Study Design | Number of Patients | Tumor Type/Tumor Site | Cut-Off | miR | HR miR-21 Low and High Expression (OS, CSS, DFS, RFS) |
|---|---|---|---|---|---|---|---|
| Jung (2012) [37] | USA | RT | 17 | OSCC | Median | miR-7, miR-21, miR-424 | OS: HR, 5.31 (C.I.: 1.39–20.38) |
| Kawakita (2014) [38] | Japan | RT | 79 | OTSCC | Score ≥ 1 | miR-21 | CSS: HR, 1.19 (0.71–1.9) |
| Hedbäck (2014) [39] | Denmark | RT | 86 | OSCC (tongue or floor of the mouth) | Tertile | miR-21 | DFS: HR, 2.70 (1.1–6.9) |
| Yu (2017) [40] | Taiwan | RT | 100 | OSCC (buccal mucosa tongue and mouth floor) | Tertile | miR-21 | DFS: HR, 1.87 (1.21–2.87) |
| Supic (2018) [32] | Serbia | RT | 60 | Tongue carcinoma | ROC analysis, cut-off 9.38 | miR-183, miR-21 | OS: HR, 2.002 (0.904–4.434) |
| Jakob (2019) [33] | Germany | RT | 36 | OSCC | Median | miR-21, miR-29, miR-31, miR-99a, miR-99b, miR-100, miR-143, miR-155. | OS: HR, 2.31 (0.62–8.58) RFS: HR, 0.18 (0.02–139) |
| Li (2013) [41] | China | RT | 63 | OSCC | Score > 3 | miR-21 | OS: HR, 2.13 (1.11–4.10) |
| Zheng (2016) [42] | China | RT | 72 | Tongue | Score ≥ 2 | miR-21 | OS: HR, 1.22 (1.09–1.36) |
| Li (2009) [43] | China | RT | 103 | Tongue | Median | miR-21 | OS: HR, 2.06 (1.21–3.51) |
| Ganci (2016) [44] | Italy | RT | 92 | OSCC | Signal score | miR-130b, miR-141, miR-21, miR-96 | RFS: HR, 4.2(1.11–5.98) |
| First Author, Date | Sample | Clinical Data | Marker Quantification | Prognostication | Statistics | Classical Prognostic Factors | |
|---|---|---|---|---|---|---|---|
| Jung (2012) [37] | 1 | 2 | 3 | 2 | 2 | 3 | 13 |
| Kawakita (2014) [38] | 3 | 2 | 2 | 2 | 1 | 3 | 13 |
| Hedbäck (2014) [39] | 3 | 3 | 2 | 3 | 3 | 2 | 16 |
| Yu (2017) [40] | 3 | 3 | 3 | 3 | 3 | 2 | 17 |
| Supic (2018) [32] | 2 | 3 | 3 | 3 | 3 | 3 | 17 |
| Jakob (2019) [33] | 1 | 3 | 3 | 3 | 3 | 3 | 16 |
| Li (2013) [41] | 2 | 2 | 3 | 2 | 2 | 3 | 14 |
| Zheng (2016) [42] | 3 | 2 | 3 | 3 | 2 | 2 | 15 |
| Li (2009) [43] | 3 | 3 | 3 | 3 | 3 | 3 | 18 |
| Ganci (2016) [44] | 3 | 2 | 3 | 3 | 3 | 2 | 16 |
| Certainty Assessment | № of Patients | Effect | Certainty | ||||||
|---|---|---|---|---|---|---|---|---|---|
| № of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Relative (95% CI) | ||
| 6 | Observational studies | Not serious | Not serious 1 | Not serious | Serious | All plausible residual confounding would suggest spurious effect, while no effect was observed Dose–response gradient | 351 | HR: 1.29 (1.16 to 1.44) | ⨁⨁⨁ 2 Moderate |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dioguardi, M.; Spirito, F.; Sovereto, D.; Alovisi, M.; Troiano, G.; Aiuto, R.; Garcovich, D.; Crincoli, V.; Laino, L.; Cazzolla, A.P.; et al. MicroRNA-21 Expression as a Prognostic Biomarker in Oral Cancer: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 3396. https://doi.org/10.3390/ijerph19063396
Dioguardi M, Spirito F, Sovereto D, Alovisi M, Troiano G, Aiuto R, Garcovich D, Crincoli V, Laino L, Cazzolla AP, et al. MicroRNA-21 Expression as a Prognostic Biomarker in Oral Cancer: Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(6):3396. https://doi.org/10.3390/ijerph19063396
Chicago/Turabian StyleDioguardi, Mario, Francesca Spirito, Diego Sovereto, Mario Alovisi, Giuseppe Troiano, Riccardo Aiuto, Daniele Garcovich, Vito Crincoli, Luigi Laino, Angela Pia Cazzolla, and et al. 2022. "MicroRNA-21 Expression as a Prognostic Biomarker in Oral Cancer: Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 6: 3396. https://doi.org/10.3390/ijerph19063396
APA StyleDioguardi, M., Spirito, F., Sovereto, D., Alovisi, M., Troiano, G., Aiuto, R., Garcovich, D., Crincoli, V., Laino, L., Cazzolla, A. P., Caloro, G. A., Di Cosola, M., & Lo Muzio, L. (2022). MicroRNA-21 Expression as a Prognostic Biomarker in Oral Cancer: Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(6), 3396. https://doi.org/10.3390/ijerph19063396













