The Impact of Aquatic Exercise Programs on the Intima-Media thickness of the Carotid Arteries, Hemodynamic Parameters, Lipid Profile and Chemokines of Community-Dwelling Older Persons: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Sample Size
2.3. Outcomes Measurements
2.3.1. Sample Characterization
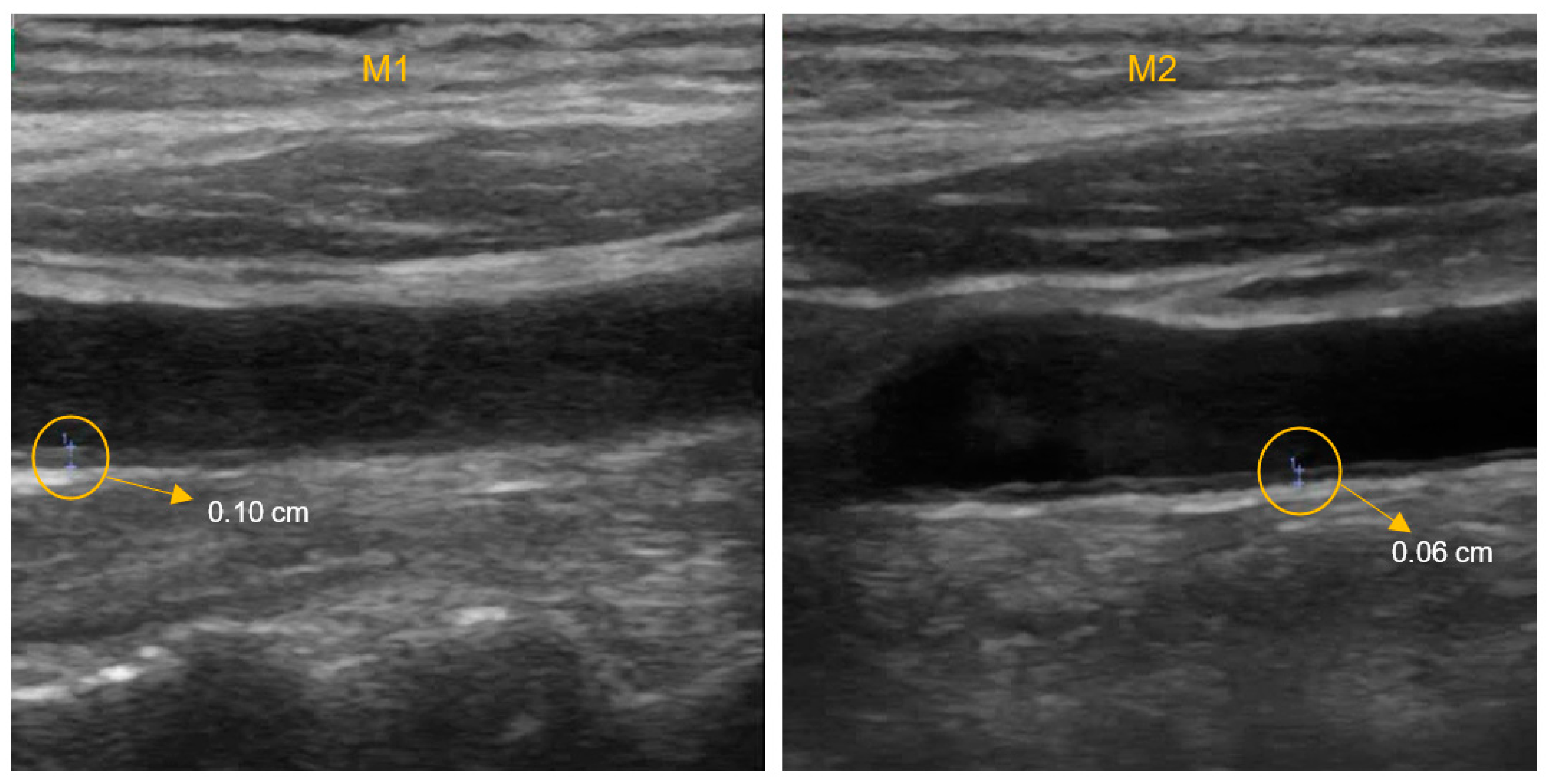
2.3.2. IMT and Hemodynamic Parameters
2.3.3. Biochemical Markers
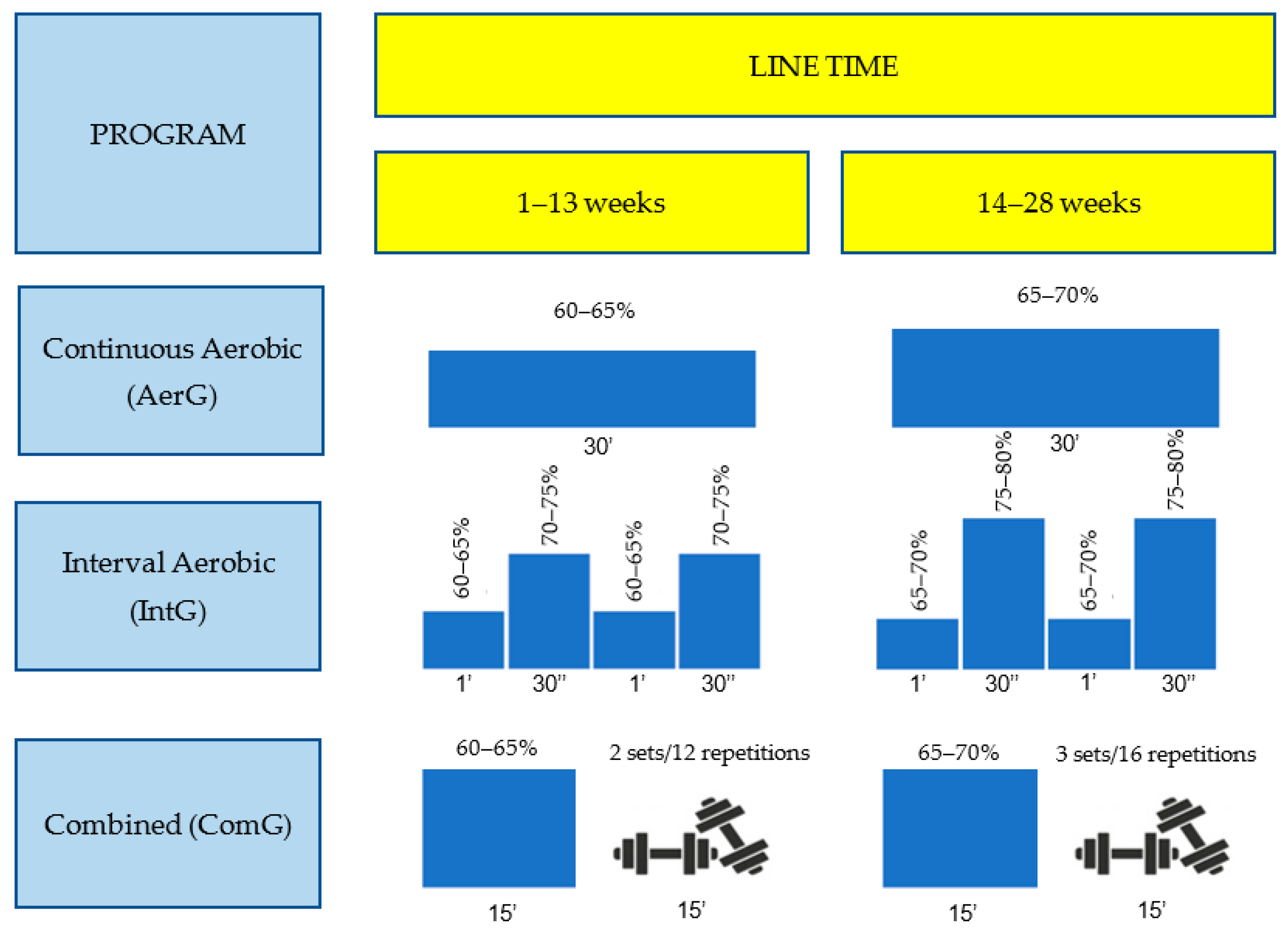
2.4. Intervention Protocol
- -
- Continuous aerobic (AerG): exercise aerobic (weeks 1–13, 60–65% maximum HR; weeks 14–28, 65–70% HR);
- -
- Interval aerobic (IntG): exercise aerobic different intensities (weeks 1–13, 60–65% maximum HR interval to 70–75% maximum HR, weeks 14–28, 65–70% maximum HR interval to 75–80% maximum HR). In IntG, the main part of the sessions consisted of several series (1’ recovery interval with 30’’ with higher intensity);
- -
- Combined (ComG): exercise aerobic (weeks 1–13, 60–65% maximum HR; weeks 14–28, 65–70% maximum HR) and muscle strength (weeks 1–13, 2 sets of 12 repetitions; weeks 14–28, 3 sets of 16 repetitions; 6–7 pois in the Borg Scale).
2.5. Monitoring the Intensity of the Exercise of Programs
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Health Topics. Cardiovascular Diseases. Available online: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1 (accessed on 29 January 2022).
- Jennings, A.; Berendsen, A.M.; De Groot, L.C.P.G.M.; Feskens, E.J.M.; Brzozowska, A.; Sicińska, E.; Pietruszka, B.; Meunier, N.; Caumon, E.; Malpuech-Brugère, C.; et al. Mediterranean-Style Diet Improves Systolic Blood Pressure and Arterial Stiffness in Older Adults. Hypertension 2019, 73, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Kablak-Ziembicka, A.; Przewlocki, T.; Tracz, W.; Pieniazek, P.; Musialek, P.; Sokolowski, A.; Drwila, R.; Rzeznik, D. Carotid intima-media thickness in pre-and postmenopausal women with suspected coronary artery disease. Heart Vessel. 2008, 23, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Munckhof, I.C.V.D.; Jones, H.; Hopman, M.T.; De Graaf, J.; Nyakayiru, J.; Van Dijk, B.; Eijsvogels, T.; Thijssen, D.H. Relation between age and carotid artery intima-medial thickness: A systematic review. Clin. Cardiol. 2018, 41, 698–704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorenz, M.; Von Kegler, S.; Steinmetz, H.; Markus, H.; Sitzer, M. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: Prospective data from the Carotid Atherosclerosis Progression Study (CAPS). Stroke 2006, 37, 87–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Touboul, P.-J.; Hennerici, M.G.; Meairs, S.; Adams, H.; Amarenco, P.; Bornstein, N.; Csiba, L.; Desvarieux, M.; Ebrahim, S.; Hernandez, R.H.; et al. Mannheim Carotid Intima-Media Thickness and Plaque Consensus (2004–2006–2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th european stroke conferences, mannheim, germany, 2004, brussels, belgium, 2006, and hamburg, germany, 2011. Cerebrovasc. Dis. 2012, 34, 290–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, H. Avaliação de Parâmetros Vasculares e Hemodinâmicos Numa População Idosa—Efeito do Exercício Continuado; Coimbra Health School: Coimbra, Portugal, 2020. [Google Scholar]
- Pedralli, M.L.; Marschner, R.; Kollet, D.; Neto, S.; Eibel, B.; Tanaka, H.; Lehnen, A.M. Different exercise training modalities produce similar endothelial function improvements in individuals with prehypertension or hypertension: A randomized clinical trial Exercise, endothelium and blood pressure. Sci. Rep. 2020, 10, 7628. [Google Scholar] [CrossRef] [PubMed]
- Gencer, S.; Evans, B.; van der Vorst, E.; Döring, Y.; Weber, C. Inflammatory Chemokines in Atherosclerosis. Cells 2021, 10, 226. [Google Scholar] [CrossRef] [PubMed]
- Jakubiak, G.K.; Pawlas, N.; Cieślar, G.; Stanek, A. Chronic Lower Extremity Ischemia and Its Association with the Frailty Syndrome in Patients with Diabetes. Int. J. Environ. Res. Public Health 2020, 17, 9339. [Google Scholar] [CrossRef] [PubMed]
- Fittipaldi, E.O.D.S.; De Andrade, A.D.; Santos, A.C.O.; Campos, S.L.; De Souza, H.C.M.; Fernandes, J.; Catanho, M.T.J.D.A. Cardiorespiratory Performance and Acute Effect of High-intensity Exercise on Lipid Profile in Hypertensive Sedentary Older Adults with and without Diabetes Mellitus. Arch. Gerontol. Geriatr. 2020, 89, 104061. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.N.; Siddiqui, S.A.; Ibrahim, M.; Hakim, M.L.; Ahammed, M.S.; Kabir, A.; Sultana, F. Inflammatory cytokines in the pathogenesis of cardiovascular disease and cancer. SAGE Open Med. 2020, 8, 2050312120965752. [Google Scholar] [CrossRef] [PubMed]
- Bianconi, V.; Sahebkar, A.; Atkin, S.L.; Pirro, M. The regulation and importance of monocyte chemoattractant protein-1. Curr. Opin. Hematol. 2018, 25, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Maurer, M.; Von Stebut, E. Macrophage inflammatory protein-1. Int. J. Biochem. Cell Biol. 2004, 36, 1882–1886. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Park, H. Effects of 6 months of aerobic and resistance exercise training on carotid artery intima media thickness in overweight and obese older women. Geriatr. Gerontol. Int. 2017, 17, 2304–2310. [Google Scholar] [CrossRef] [PubMed]
- Venturelli, M.; Cè, E.; Limonta, E.; Schena, F.; Caimi, B.; Carugo, S.; Veicsteinas, A.; Esposito, F. Effects of endurance, circuit, and relaxing training on cardiovascular risk factors in hypertensive elderly patients. AGE 2015, 37, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Son, W.-M.; Sung, K.-D.; Cho, J.-M.; Park, S.-Y. Combined exercise reduces arterial stiffness, blood pressure, and blood markers for cardiovascular risk in postmenopausal women with hypertension. Menopause 2017, 24, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Montero, D.; Vinet, A.; Roberts, C.K. Effect of combined aerobic and resistance training versus aerobic training on arterial stiffness. Int. J. Cardiol. 2015, 178, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Júnior, F.A.; Gomes, S.G.; Da Silva, F.F.; Souza, P.M.; Oliveira, E.C.; Coelho, D.B.; Nascimento-Neto, R.M.; Lima, W.; Becker, L.K. The effects of aquatic and land exercise on resting blood pressure and post-exercise hypotension response in elderly hypertensives. Cardiovasc. J. Afr. 2020, 31, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Martins, R.A.; Veríssimo, M.T.; Coelho e Silva, M.J.; Cumming, S.; Teixeira, A. Effects of aerobic and strength-based training on metabolic health indicators in older adults. Lipids Health Dis. 2010, 9, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Gleeson, M.; Walsh, N.P. The BASES Expert Statement on Exercise, Immunity, and Infection. J. Sports Sci. 2012, 30, 321–324. [Google Scholar] [CrossRef] [Green Version]
- Cugusi, L.; Manca, A.; Bergamin, M.; Di Blasio, A.; Monticone, M.; Deriu, F.; Mercuro, G. Aquatic exercise improves motor impairments in people with Parkinson’s disease, with similar or greater benefits than land-based exercise: A systematic review. J. Physiother. 2019, 5, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.P.; Teixeira, A.; Serrano, J.; Farinha, C.; Santos, H.; Silva, F.M.; Cascante-Rusenhack, M.; Luís, P. Impact of Aquatic-Based Physical Exercise Programs on Risk Markers of Cardiometabolic Diseases in Older People: A Study Protocol for Randomized-Controlled Trials. Int. J. Environ. Res. Public Health 2020, 17, 8678. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Chupel, M.U.; Direito, F.; Furtado, G.E.; Minuzzi, L.G.; Pedrosa, F.M.; Colado, J.C.; Ferreira, J.P.; Filaire, E.; Teixeira, A.M. Strength Training Decreases Inflammation and Increases Cognition and Physical Fitness in Older Women with Cognitive Impairment. Front. Physiol. 2017, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dziubek, W.; Bulińska, K.; Rogowski, Ł.; Gołębiowski, T.; Kusztal, M.; Grochola, M.; Markowska, D.; Zembroń-Łacny, A.; Weyde, W.; Klinger, M.; et al. The Effects of Aquatic Exercises on Physical Fitness and Muscle Function in Dialysis Patients. BioMed Res. Int. 2015, 2015, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moreira, N.B.; da Silva, L.P.; Rodacki, A.L.F. Aquatic exercise improves functional capacity, perceptual aspects, and quality of life in older adults with musculoskeletal disorders and risk of falling: A randomized controlled trial. Exp. Gerontol. 2020, 142, 111135. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.E.; Jones, C.J. Functional Fitness Normative Scores for Community-Residing Older Adults, Ages 60–94. J. Aging Phys. Act. 1999, 7, 162–181. [Google Scholar] [CrossRef]
- Baptista, F.; Sardinha, L. Avaliação da Aptidão Física e do Equilíbrio de Pessoas Idosas. Baterias de Fullerton; Faculty of Human Motricity: Porto, Portugal, 2005. [Google Scholar]
- Mancia, G.; De Backer, G.; Dominiczak, A.; Cifkova, R.; Fagard, R.; Germano, G.; Grassi, G.; Heagerty, A.M.; Kjeldsen, S.E.; Laurent, S.; et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2007, 28, 1462–1536. [Google Scholar] [CrossRef] [PubMed]
- ACSM. Diretrizes do ACSM Para os Testes de Esforço e Sua Prescrição, 10th ed.; Guanabara Koogan LTDA: Philadelphia, PA, USA, 2018. [Google Scholar]
- Karvonen, M.; Kentala, K.; Mustala, O. The effects of training heart rate: A longitudinal study. Ann. Med. Exp. Biol. Fenn. 1957, 35, 307–315. [Google Scholar] [PubMed]
- Franklin, B.; Whaley, M.; Howley, E.; Balady, G. ACSM’s Guidelines for Exercise Testing and Prescription; Williams & Wilkins: Philadelphia, PA, USA, 2000. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Farahati, S.; Hosseini, S.R.A.; Moazzami, M.; Daloee, M.H.; Daloee, S.H. The impact of high-intensity interval training versus moderate-intensity continuous training on carotid intima-media thickness and ankle-brachial index in middle-aged women. Int. J. Prev. Med. 2020, 11, 62. [Google Scholar] [CrossRef] [PubMed]
- Homma, S.; Hirose, N.; Ishida, H.; Ishii, T.; Araki, G. Carotid Plaque and Intima-Media Thickness Assessed by B-Mode Ultrasonography in Subjects Ranging From Young Adults to Centenarians. Stroke 2001, 32, 830–835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.-Y.; Kwak, Y.-S.; Pekas, E.J. Impacts of aquatic walking on arterial stiffness, exercise tolerance, and physical function in patients with peripheral artery disease: A randomized clinical trial. J. Appl. Physiol. 2019, 127, 940–949. [Google Scholar] [CrossRef] [PubMed]
- Park, W.; Jung, W.-S.; Hong, K.; Kim, Y.-Y.; Kim, S.-W.; Park, H.-Y. Effects of Moderate Combined Resistance- and Aerobic-Exercise for 12 Weeks on Body Composition, Cardiometabolic Risk Factors, Blood Pressure, Arterial Stiffness, and Physical Functions, among Obese Older Men: A Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 7233. [Google Scholar] [CrossRef] [PubMed]
- Cugusi, L.; Cadeddu, C.; Nocco, S.; Orrù, F.; Bandino, S.; Deidda, M.; Caria, A.; Bassareo, P.P.; Piras, A.; Cabras, S.; et al. Effects of an Aquatic-Based Exercise Program to Improve Cardiometabolic Profile, Quality of Life, and Physical Activity Levels in Men With Type 2 Diabetes Mellitus. PM&R 2014, 7, 141–148. [Google Scholar] [CrossRef]
- Costa, R.R.; Buttelli, A.C.; Coconcelli, L.; Pereira, L.F.; Vieira, A.; Fagundes, A.D.O.; Farinha, J.B.; Reichert, T.; Stein, R.; Kruel, L.F. Water-Based Aerobic and Resistance Training as a Treatment to Improve the Lipid Profile of Women with Dyslipidemia: A Randomized Controlled Trial. J. Phys. Act. Health 2019, 16, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Keyhani, D.; Tartibian, B.; Dabiri, A.; Teixeira, A. Effect of High-Intensity Interval Training Versus Moderate-Intensity Aerobic Continuous Training on Galectin-3 Gene Expression in Postmenopausal Women: A Randomized Controlled Trial. J. Aging Phys. Act. 2020, 28, 987–995. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, W.J.; Hatfield, D.L.; Comstock, B.A.; Fragala, M.S.; Davitt, P.M.; Cortis, C.; Wilson, J.M.; Lee, E.C.; Newton, R.U.; Dunn-Lewis, C.; et al. Influence of HMB Supplementation and Resistance Training on Cytokine Responses to Resistance Exercise. J. Am. Coll. Nutr. 2014, 33, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Barry, J.C.; Simtchouk, S.; Durrer, C.; Jung, M.E.; Little, J.P. Short-Term Exercise Training Alters Leukocyte Chemokine Receptors in Obese Adults. Med. Sci. Sports Exerc. 2017, 49, 1631–1640. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Lim, S.-T.; Kim, W.-N. Aquatic exercise for improving immune function and mental stress in pre-frailty elderly women. J. Women Aging 2020, 33, 611–619. [Google Scholar] [CrossRef]
- Saleh, M.S.M.; Rehab, N.I.; Aly, S.M.A. Effect of aquatic versus land motor dual task training on balance and gait of patients with chronic stroke: A randomized controlled trial. NeuroRehabilitation 2019, 44, 485–492. [Google Scholar] [CrossRef]
- Avers, D. Exercise and physical activity for older adults. In Guccione’s Geriatric Physical Therapy, 4th ed.; Elsevier: St. Louis, MO, USA, 2020; Chapter 8; pp. 166–200. [Google Scholar]

| Characteristic | AerG (n = 25) | IntG (n = 28) | ComG (n = 29) | CG (n = 20) | p Value |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| AG (years) | 71.44 (4.8) | 72.64 (5.2) | 71.90 (5.7) | 73.60 (5.3) | 0.504 |
| Hgt (m) | 1.58 (0.7) | 1.56 (0.7) | 1.57 (0.7) | 1.60 (0.9) | 0.331 |
| WGT (kg) | 70.5 (8.1) | 71.3 (14.3) | 75.1 (11.0) | 75.5 (13.3) | 0.334 |
| BMI (kg/m2) | 28.20 (3.3) | 29.10 (4.8) | 30.80 (5.3) | 29.50 (5.8) | 0.272 |
| VF (%) | 11.0 (3.0) | 12.0 (3.0) | 13.0 (3.0) | 13.0 (6.0) | 0.128 |
| FM (%) | 38.9 (7.3) | 41.0 (6.7) | 40.3 (9.8) | 34.9 (10.9) | 0.134 |
| LBM (%) | 26.5 (4.3) | 24.5 (3.0) | 25.5 (4.3) | 27.7 (4.7) | 0.079 |
| 2 m-ST (no of steps) | 80.9 (17.4) | 71.5 (16.5) | 81.6 (19.2) | 74.3 (18.9) | 0.069 |
| CSR-R (cm) | −0.5 (6.6) | −3.7 (10.6) | −3.5 (7.8) | −7.6 (9.7) | 0.099 |
| CSR-L (cm) | 0.6 (7.2) | −3.9 (9.9) | −5.8 (9.9) | −3.5 (7.3) | 0.054 |
| BS-R (cm) | −9.9 (10.4) | −11.9 (11.5) | −14.3 (9.7) | −16.6 (9.9) | 0.157 |
| BS-L (cm) | −14.4 (7.2) | −17.4 (8.6) | −21.0 (10.8) | −20.6 (10.7) | 0.056 |
| TUG (s) | 6.1 (1.1) | 7.4 (1.8) | 7.4 (3.0) | 6.8 (1.7) | 0.110 |
| 30 s-CS (reps/30 s) | 15.0 (3.0) | 13.0 (4.0) | 13.0 (3.0) | 15.0 (5.0) | 0.185 |
| 30 s-AC (reps/30 s) | 21.0 (6.0) | 17.0 (7.0) | 20.0 (5.0) | 19.0 (6.0) | 0.119 |
| HG-R (kg) | 22.0 (6.0) | 21.0 (9.0) | 21.0 (9.0) | 24.0 (9.0) | 0.411 |
| HG-L (kg) | 21.0 (6.0) | 20.0 (9.0) | 21.0 (9.0) | 21.0 (10.0) | 0.578 |
| AerG | IntG | ComG | CG | Time × Group (M1) | Time × Group (M2) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 Mean (SD) | M2 Mean (SD) | Time (p) | M1 Mean (SD) | M2 Mean (SD) | Time (p) | M1 Mean (SD) | M2 Mean (SD) | Time (p) | M2 Mean (SD) | M1 Mean (SD) | Time (p) | |||
| IMT-L (cm) | 0.07 (0.02) | 0.07 (0.02) | 0.293 | 0.08 (0.02) | 0.07 (0.02) | 0.376 | 0.07 (0.02) | 0.07 (0.02) | 0.707 | 0.07 (0.01) | 0.07 (0.02) | 0.979 | 0.989 | 0.501 |
| SD-L (cm) | 0.69 (0.12) | 0.67 (0.09) | 0.177 | 0.65 (0.1) | 0.65 (0.09) | 0.539 | 0.66 (0.1) | 0.64 (0.09) | 0.105 | 0.65 (0.06) | 0.66 (0.06) | 0.088 | 0.605 | 0.546 |
| DD-L (cm) | 0.64 (0.12) | 0.62 (0.09) | 0.423 | 0.61 (0.09) | 0.59 (0.09) | 0.105 | 0.63 (0.09) | 0.60 (0.09) | 0.037 ** | 0.61 (0.06) | 0.62 (0.06) | 0.558 | 0.640 | 0.264 |
| PSV-L (cm/s) | 76.79 (21.45) | 80.31 (19.22) | 0.242 | 82.51 (19.78) | 77.21 (16.26) | 0.104 | 79.38 (18.77) | 78.73 (17.06) | 0.315 | 77.28 (15.91) | 80.24 (17.9) | 0.097 | 0.508 | 0.835 |
| EDV-L (cm/s) | 19.28 (6.24) | 19.95 (5.8) | 0.397 | 20.8 (5.43) | 20.26 (4.93) | 0.581 | 22.38 (4.78) | 19.97 (6.56) | 0.027 * | 19.7 (5.32) | 22.41 (5.62) | 0.003 * | 0.090 | 0.443 |
| IMT-R (cm) | 0.08 (0.01) | 0.07 (0.01) | 0.808 | 0.08 (0.02) | 0.07 (0.02) | 0.055 | 0.08 (0.02) | 0.07 (0.01) | 0.205 | 0.08 (0.02) | 0.08 (0.02) | 0.308 | 0.654 | 0.698 |
| SD-R (cm) | 0.70 (0.12) | 0.68 (0.09) | 0.178 | 0.66 (0.09) | 0.65 (0.09) | 0.381 | 0.67 (0.08) | 0.66 (0.09) | 0.249 | 0.68 (0.08) | 0.66 (0.08) | 0.353 | 0.519 | 0.758 |
| DD-R (cm) | 0.66 (0.12) | 0.63 (0.09) | 0.039 * | 0.62 (0.08) | 0.61 (0.09) | 0.282 | 0.63 (0.09) | 0.60 (0.09) | 0.029 * | 0.62 (0.07) | 0.63 (0.07) | 0.813 | 0.316 | 0.543 |
| PSV-R (cm/s) | 74.6 (23.04) | 74.1 (17.56) | 0.904 | 74.63 (18) | 66.23 (17.68) | 0.024 * | 81.23 (15.74) | 77.25 (12.81) | 0.087 | 74.27 (16.9) | 73.11 (16.31) | 0.763 | 0.136 | 0.106 |
| EDV-R (cm/s) | 19.55 (7.29) | 18.89 (5.41) | 0.716 | 19.39 (5.44) | 18.26 (4.8) | 0.186 | 20.74 (5.29) | 19.18 (6.34) | 0.064 | 18.43 (4.63) | 19.27 (5.35) | 0.432 | 0.169 | 0.910 |
| SBP (mmHg) | 134 (13.0) | 128 (16.0) | 0.013 * | 135 (12.0) | 132 (13.0) | 0.184 | 138 (18.0) | 133 (18.0) | 0.018 ** | 137 (15.0) | 132 (18.0) | 0.093 | 0.798 | 0.535 |
| DBP mmHg) | 77 (9.0) | 73 (10.0) | 0.002 * | 76 (7.0) | 73 (7.0) | 0.046 * | 79 (8.0) | 75 (8.0) | 0.004 * | 78 (7.0) | 78 (7.0) | 0.950 | 0.399 | 0.099 |
| HR (bpm) | 71 (11.0) | 69 (12.0) | 0.279 | 69 (9.0) | 67 (11.0) | 0.115 | 74 (12.0) | 70 (10.0) | 0.010 ** | 73 (10.0) | 71 (6.0) | 0.467 | 0.417 | 0.268 |
| AerG | IntG | ComG | CG | Time × Group (M1) | Time × Group (M2) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 Mean (SD) | M2 Mean (SD) | Time (p) | M1 Mean (SD) | M2 Mean (SD) | Time (p) | M1 Mean (SD) | M2 Mean (SD) | Time (p) | M1 Mean (SD) | M2 Mean (SD) | Time (p) | |||
| GLU (mg/dL) | 94 (27) | 89 (22) | 0.006 ** | 95 (18) | 90 (17) | 0.041 ** | 98 (25) | 95 (24) | 0.309 | 97 (20) | 99 (18) | 0.449 | 0.728 | 0.112 |
| TC (mg/dL) | 184 (31) | 185 (24) | 0.935 | 174 (33) | 172 (29) | 0.650 | 182 (26) | 178 (24) | 0.346 | 176 (26) | 177 (27) | 0.757 | 0.512 | 0.381 |
| HDL (mg/dL) | 58 (14) | 59 (12) | 0.586 | 58 (15) | 56 (15) | 0.175 | 58 (11) | 59 (13) | 0.478 | 57 (11) | 55 (11) | 0.111 | 0.907 | 0.582 |
| AI (mg/dL) | 3.29 (0.63) | 3.33 (0.49) | 0.653 | 3.17 (0.54) | 3.25 (0.6) | 0.249 | 3.23 (0.68) | 3.27 (0.71) | 0.566 | 3.21 (0.64) | 3.67 (0.52) | 0.003 * | 0.598 | 0.033 † |
| LDL (mg/dL) | 106 (25) | 108 (20) | 0.712 | 95 (27) | 95 (24) | 0.855 | 103 (25) | 100 (25) | 0.498 | 97 (25) | 97 (25) | 0.989 | 0.338 | 0.226 |
| TG (mg/dL) | 102 (51) | 101 (48) | 0.903 | 105 (36) | 104 (43) | 0.682 | 107 (41) | 104 (46) | 0.503 | 116 (47) | 119 (35) | 0.478 | 0.393 | 0.191 |
| MCP-1 (pg/mL) | 141.74 (82.71) | 82.45 (46.02) | 0.001 ** | 80.43 (37.15) | 63.42 (42.69) | 0.059 | 231.79 (73.36) | 193.44 (94.04) | 0.033 ** | 72.76 (49.30) | 54.34 (31.33) | 0.093 | 0.000 † | 0.000 † |
| MIP-1α (pg/mL) | 93.09 (12.62) | 91.04 (7.39) | 0.009 ** | 96.19 (1.88) | 96.45 (1.29) | 0.179 | 110.49 (9.37) | 110.43 (11.77) | 0.214 | 90.90 (15.12) | 90.96 (15.40) | 0.546 | 0.000 † | 0.000 † |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farinha, C.; Santos, H.; Serrano, J.; Oliveiros, B.; Silva, F.M.; Cascante-Rusenhack, M.; Teixeira, A.M.; Ferreira, J.P. The Impact of Aquatic Exercise Programs on the Intima-Media thickness of the Carotid Arteries, Hemodynamic Parameters, Lipid Profile and Chemokines of Community-Dwelling Older Persons: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 3377. https://doi.org/10.3390/ijerph19063377
Farinha C, Santos H, Serrano J, Oliveiros B, Silva FM, Cascante-Rusenhack M, Teixeira AM, Ferreira JP. The Impact of Aquatic Exercise Programs on the Intima-Media thickness of the Carotid Arteries, Hemodynamic Parameters, Lipid Profile and Chemokines of Community-Dwelling Older Persons: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(6):3377. https://doi.org/10.3390/ijerph19063377
Chicago/Turabian StyleFarinha, Carlos, Hélder Santos, João Serrano, Bárbara Oliveiros, Fernanda M. Silva, Márcio Cascante-Rusenhack, Ana Maria Teixeira, and José Pedro Ferreira. 2022. "The Impact of Aquatic Exercise Programs on the Intima-Media thickness of the Carotid Arteries, Hemodynamic Parameters, Lipid Profile and Chemokines of Community-Dwelling Older Persons: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 6: 3377. https://doi.org/10.3390/ijerph19063377
APA StyleFarinha, C., Santos, H., Serrano, J., Oliveiros, B., Silva, F. M., Cascante-Rusenhack, M., Teixeira, A. M., & Ferreira, J. P. (2022). The Impact of Aquatic Exercise Programs on the Intima-Media thickness of the Carotid Arteries, Hemodynamic Parameters, Lipid Profile and Chemokines of Community-Dwelling Older Persons: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(6), 3377. https://doi.org/10.3390/ijerph19063377








