The Impact of the COVID-19 Pandemic on Rural Food Security in High Income Countries: A Systematic Literature Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Information Sources and Searches
- Food Security: “Food Securit *” OR “Food Insecurit *” OR hunger OR “apparent consumption *” OR “food *”.
- COVID: Coronavirus OR COVID* OR Pandemic * OR SARS-CoV-2.
- Other food security outcomes: access * OR hoarding OR availabil * OR pric * OR income * OR prepar * OR skill * OR suppl * OR environment * OR “panic buy *” OR diet * OR fruit * OR vegetable * OR dairy * OR meat *.
2.4. Study Selection
2.5. Data Collection Process
2.6. Data Synthesis and Analysis
2.7. Quality Assessment
3. Results
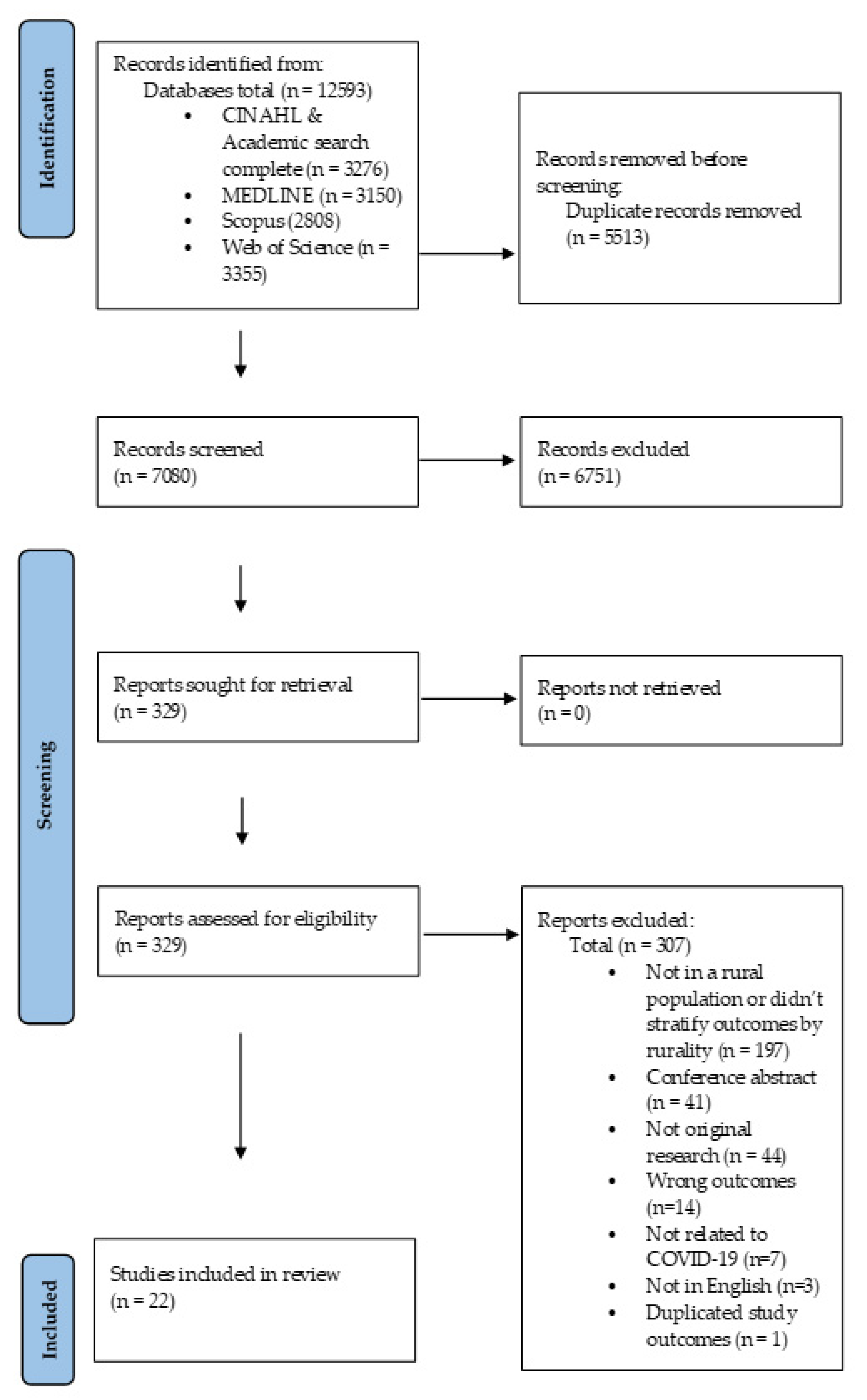
3.1. Study Selection
3.2. Description of Studies
3.3. The Prevalence of Food Insecurity
3.4. Food Availability
3.5. Food Access (Physical and Financial)
3.6. Utilization (e.g., Cooking, Storage)
3.7. Stability of the Food Supply
3.8. Quality Assessment
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- FAO. Declaration of the World Summit on Food Security; FAO: Rome, Italy, 2009. [Google Scholar]
- Alston, L.; Jacobs, J.; Allender, S.; Nichols, M. A comparison of the modelled impacts on CVD mortality if attainment of public health recommendations was achieved in metropolitan and rural Australia. Public Health Nutr. 2020, 23, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Alston, L.; Allender, S.; Peterson, K.; Jacobs, J.; Nichols, M. Rural Inequalities in the Australian Burden of Ischaemic Heart Disease: A Systematic Review. Heart Lung Circ. 2017, 26, 122–133. [Google Scholar] [CrossRef] [Green Version]
- Household Food Security in the United States in 2013. Available online: https://www.ers.usda.gov/webdocs/publications/45265/48787_err173.pdf (accessed on 23 February 2022).
- National Rural Health Alliance. Food Security and Health in Rural and Remote Australia; National Rural Health Alliance: Deakin, ACT, Australia, 2016. [Google Scholar]
- PROOF’s Research Shows that Food Insecurity Is a Policy Decision that Requires Income-Based Interventions to Solve. Available online: http://proof.utoronto.ca (accessed on 23 February 2022).
- Alston, L.; Walker, T.; Kent, K. Characterizing Dietary Intakes in Rural Australian Adults: A Systematic Literature Review. Nutrients 2020, 12, 3515. [Google Scholar] [CrossRef] [PubMed]
- Andress, L.; Fitch, C. Juggling the five dimensions of food access: Perceptions of rural low income residents. Appetite 2016, 105, 151–155. [Google Scholar] [CrossRef]
- Whelan, J.; Millar, L.; Bell, C.; Russell, C.; Grainger, F.; Allender, S.; Love, P. You can’t find healthy food in the bush: Poor accessibility, availability and adequacy of food in rural Australia. Int. J. Environ. Res. Public Health 2018, 15, 2316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, E.A.; Shapiro, M.J.; Welsh, C.; Bleich, S.N.; Cobb, L.K.; Gittelsohn, J. Healthy Food Availability Among Food Sources in Rural Maryland Counties. J. Hunger Environ. Nutr. 2017, 12, 328–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alston, L.; Versace, V.; Brown, E.; Nichols, M.; Whelan, J.; Bolton, K.A.; Sacks, G.; Needham, C.; Orellana, L.; Allender, S. Understanding the healthfulness of outlets providing lunch and dinner meals: A census of a rural food retail environment in Victoria, Australia. Aust. N. Z. J. Public Health 2021, 45, 65–70. [Google Scholar] [CrossRef]
- Cuttler, R.; Evans, R.; McClusky, E.; Purser, L.; Klassen, K.M.; Palermo, C. An investigation of the cost of food in the Geelong region of rural Victoria: Essential data to support planning to improve access to nutritious food. Health Promot. J. Aust. 2019, 30, 124–127. [Google Scholar] [CrossRef] [Green Version]
- Buck-McFadyen, E.V. Rural food insecurity: When cooking skills, homegrown food, and perseverance aren’t enough to feed a family. Can. J. Public Health 2015, 106, e140–e146. [Google Scholar] [CrossRef]
- Lenardson, J.D.; Hansen, A.Y.; Hartley, D. Rural and remote food environments and obesity. Curr. Obes. Rep. 2015, 4, 46–53. [Google Scholar] [CrossRef]
- Pincombe, M.; Reese, V.; Dolan, C.B. The effectiveness of national-level containment and closure policies across income levels during the COVID-19 pandemic: An analysis of 113 countries. Health Policy Plan. 2021, 36, 1152–1162. [Google Scholar] [CrossRef] [PubMed]
- Devereux, S.; Béné, C.; Hoddinott, J. Conceptualising COVID-19’s impacts on household food security. Food Secur. 2020, 12, 769–772. [Google Scholar] [CrossRef] [PubMed]
- Mueller, V.; Grépin, K.A.; Rabbani, A.; Navia, B.; Ngunjiri, A.S.W.; Wu, N. Food insecurity and COVID-19 risk in low- and middle-income countries. Appl. Econ. Perspect. Policy 2022, 44, 92–109. [Google Scholar] [CrossRef]
- Picchioni, F.; Goulao, L.F.; Roberfroid, D. The impact of COVID-19 on diet quality, food security and nutrition in low and middle income countries: A systematic review of the evidence. Clin. Nutr. 2021; Epub ahead of print. [Google Scholar]
- The Coronavirus May Hit Rural America Later—and Harder. Available online: https://www.vox.com/2020/3/28/21197421/usa-coronavirus-covid-19-rural-america (accessed on 23 February 2022).
- Malatzky, D.C.; Gillespie, J.; Couch, D.D.L.; Cosgrave, D.C. Why place matters: A rurally-orientated analysis of COVID-19’s differential impacts. Soc. Sci. Humanit. Open 2020, 2, 100063. [Google Scholar] [CrossRef]
- O’Kane, G. COVID-19 puts the spotlight on food insecurity in rural and remote Australia. Aust. J. Rural Health 2020, 28, 319–320. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Porritt, K.; Gomersall, J.; Lockwood, C. JBI’s systematic reviews: Study selection and critical appraisal. Am. J. Nurs. 2014, 114, 47–52. [Google Scholar] [CrossRef]
- Munn, Z.; Moola, S.; Riitano, D.; Lisy, K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int. J. Health Policy Manag. 2014, 3, 123. [Google Scholar] [CrossRef] [Green Version]
- Kent, K.; Murray, S.; Penrose, B.; Auckland, S.; Godrich, S.; Lester, E.; Visentin, D. Food insecure households faced greater challenges putting healthy food on the table during the COVID-19 pandemic in Australia. Appetite 2022, 169, 105815. [Google Scholar] [CrossRef]
- Parekh, N.; Ali, S.H.; O’Connor, J.; Tozan, Y.; Jones, A.M.; Capasso, A.; Foreman, J.; DiClemente, R.J. Food insecurity among households with children during the COVID-19 pandemic: Results from a study among social media users across the United States. Nutr. J. 2021, 20, 73. [Google Scholar] [CrossRef]
- Jackson, A.M.; Weaver, R.H.; Iniguez, A.; Lanigan, J. A lifespan perspective of structural and perceived social relationships, food insecurity, and dietary behaviors during the COVID-19 pandemic. Appetite 2022, 168, 105717. [Google Scholar] [CrossRef] [PubMed]
- Kar, A.; Motoyama, Y.; Carrel, A.L.; Miller, H.J.; Le, H.T.K. COVID-19 exacerbates unequal food access. Appl. Geogr. 2021, 134, 102517. [Google Scholar] [CrossRef]
- Luckstead, J.; Nayga, R.M., Jr.; Snell, H.A. Labor Issues in the Food Supply Chain Amid the COVID-19 Pandemic. Appl. Econ. Perspect. Policy 2020, 43, 382–400. [Google Scholar] [CrossRef]
- Mui, Y.; Headrick, G.; Raja, S.; Palmer, A.; Ehsani, J.; Pollack Porter, K. Acquisition, mobility and food insecurity: Integrated food systems opportunities across urbanicity levels highlighted by COVID-19. Public Health Nutr. 2021, 25, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Sherbuk, J.E.; Williams, B.; McManus, K.A.; Dillingham, R. Financial, Food, and Housing Insecurity Due to Coronavirus Disease 2019 Among At-Risk People With Human Immunodeficiency Virus in a Nonurban Ryan White HIV/AIDS Program Clinic. Open Forum Infect Dis. 2020, 7, ofaa423. [Google Scholar] [CrossRef]
- Steimle, S.; Gassman-Pines, A.; Johnson, A.D.; Hines, C.T.; Ryan, R.M. Understanding patterns of food insecurity and family well-being amid the COVID-19 pandemic using daily surveys. Child Dev. 2021, 92, e781–e797. [Google Scholar] [CrossRef]
- Taylor, D.E.; Lusuegro, A.; Loong, V.; Cambridge, A.; Nichols, C.; Goode, M.; McCoy, E.; Daupan, S.M.; Bartlett, M.L.; Noel, E.; et al. Racial, Gender, and Age Dynamics in Michigan’s Urban and Rural Farmers Markets: Reducing Food Insecurity, and the Impacts of a Pandemic. Am. Behav. Sci. 2021. [Google Scholar] [CrossRef]
- Barr, M.L.; OoNorasak, K.; Hughes, K.; Batey, L.; Jackson, K.; Marshall, H.; Stephenson, T. Exploring Perceived Importance of a Novel Emergency Food Program during COVID-19 and Program Recipient Characteristics. Int. J. Environ. Res. Public Health 2021, 18, 786. [Google Scholar] [CrossRef]
- Barr, M.L.; Martin, C.; Luecking, C.; Cardarelli, K. Losses, Gains, and Changes to the Food Environment in a Rural Kentucky County during the COVID-19 Pandemic. Nutrients 2021, 13, 3929. [Google Scholar] [CrossRef]
- Pyle, A.; Eichinger, M.; Garst, B.; Mobley, C.; Griffin, S.; Hossfeld, L.; McGirr, M.; Saunders, H. Disease and disaster: Navigating food insecurity in a community affected by crises during COVID-19. J. Agric. Food Syst. Community Dev. 2021, 10, 37–54. [Google Scholar] [CrossRef]
- Niles, M.T.; Wirkkala, K.B.; Belarmino, E.H.; Bertmann, F. Home food procurement impacts food security and diet quality during COVID-19. BMC Public Health 2021, 21, 945. [Google Scholar] [CrossRef] [PubMed]
- Niles, M.T.; Bertmann, F.; Belarmino, E.H.; Wentworth, T.; Biehl, E.; Neff, R. The Early Food Insecurity Impacts of COVID-19. Nutrients 2020, 12, 2096. [Google Scholar] [CrossRef] [PubMed]
- Kent, K.; Murray, S.; Penrose, B.; Auckland, S.; Visentin, D.; Godrich, S.; Lester, E. Prevalence and Socio-Demographic Predictors of Food Insecurity in Australia during the COVID-19 Pandemic. Nutrients 2020, 12, 2682. [Google Scholar] [CrossRef] [PubMed]
- Whelan, J.; Brown, A.D.; Coller, L.; Strugnell, C.; Allender, S.; Alston, L.; Hayward, J.; Brimblecombe, J.; Bell, C. The Impact of COVID-19 on Rural Food Supply and Demand in Australia: Utilising Group Model Building to Identify Retailer and Customer Perspectives. Nutrients 2021, 13, 417. [Google Scholar] [CrossRef]
- Men, F.; Tarasuk, V. Food Insecurity amid the COVID-19 Pandemic: Food Charity, Government Assistance, and Employment. Can. Public Policy 2021, 47, 202–230. [Google Scholar] [CrossRef]
- Snuggs, S.; McGregor, S. Food & meal decision making in lockdown: How and who has Covid-19 affected? Food Qual. Prefer. 2021, 89, 104145. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Cohn-Schwartz, E.; Ayalon, L. COVID-19 Protective Behaviors: The Role of Living Arrangements and Localities. J. Appl. Gerontol. 2021, 40, 799–803. [Google Scholar] [CrossRef]
- Giacoman, C.; Herrera, M.S.; Ayala Arancibia, P. Household food insecurity before and during the COVID-19 pandemic in Chile. Public Health 2021, 198, 332–339. [Google Scholar] [CrossRef]
- Simmet, A.; Stroebele-Benschop, N. Food Bank Operations during the COVID-19 Pandemic in Germany. J. Hunger Environ. Nutr. 2021, 16. [Google Scholar] [CrossRef]
- Jordan, I.; Keding, G.B.; Stosius, L.; Hawrysz, I.; Janiszewska, K.; Heil, E.A. Changes in Vegetable Consumption in Times of COVID-19—First Findings From an International Civil Science Project. Front. Nutr. 2021, 8, 686786. [Google Scholar] [CrossRef] [PubMed]
- Peters, D.J. Community Susceptibility and Resiliency to COVID-19 Across the Rural-Urban Continuum in the United States. J. Rural Health 2020, 36, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Cuadros, D.F.; Branscum, A.J.; Mukandavire, Z.; Miller, F.D.; MacKinnon, N. Dynamics of the COVID-19 epidemic in urban and rural areas in the United States. Ann. Epidemiol. 2021, 59, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Paul, R.; Arif, A.A.; Adeyemi, O.; Ghosh, S.; Han, D. Progression of COVID-19 from urban to rural areas in the United States: A spatiotemporal analysis of prevalence rates. J. Rural Health 2020, 36, 591–601. [Google Scholar] [CrossRef]
- Mueller, J.T.; McConnell, K.; Burow, P.B.; Pofahl, K.; Merdjanoff, A.A.; Farrell, J. Impacts of the COVID-19 pandemic on rural America. Proc. Natl. Acad. Sci. USA 2021, 118, 2019378118. [Google Scholar] [CrossRef]
- Cohen, M.J.; Garrett, J.L. The food price crisis and urban food (in)security. Environ. Urban. 2010, 22, 467–482. [Google Scholar] [CrossRef]
- Deaton, B.J.; Deaton, B.J. Food security and Canada’s agricultural system challenged by COVID-19. Can. J. Agric. Econ./Rev. Can. D’agroeconomie 2020, 68, 143–149. [Google Scholar] [CrossRef]
- Walker, R.E.; Keane, C.R.; Burke, J.G. Disparities and access to healthy food in the United States: A review of food deserts literature. Health Place 2010, 16, 876–884. [Google Scholar] [CrossRef]
- Hobbs, J.E. Food supply chain resilience and the COVID-19 pandemic: What have we learned? Can. J. Agric. Econ./Rev. Can. D’agroeconomie 2021, 69, 189–196. [Google Scholar] [CrossRef]
- Chiwona-Karltun, L.; Amuakwa-Mensah, F.; Wamala-Larsson, C.; Amuakwa-Mensah, S.; Abu Hatab, A.; Made, N.; Taremwa, N.K.; Melyoki, L.; Rutashobya, L.K.; Madonsela, T. COVID-19: From health crises to food security anxiety and policy implications. Ambio 2021, 50, 794–811. [Google Scholar] [CrossRef]
- Killmorgen, A. Coronavirus and Price Gouging—Let’s Put a Stop to It. Available online: https://www.choice.com.au/shopping/online-shopping/selling-online/articles/coronavirus-and-price-gouging (accessed on 28 July 2020).
- Park, M.; Lim, J.T.; Wang, L.; Cook, A.R.; Dickens, B.L. Urban-Rural Disparities for COVID-19: Evidence from 10 Countries and Areas in the Western Pacific. Health Data Sci. 2021, 2021, 9790275. [Google Scholar] [CrossRef]
- Mead, B.R.; Davies, J.A.; Falagán, N.; Kourmpetli, S.; Liu, L.; Hardman, C.A. Growing your own in times of crisis: The role of home food growing in perceived food insecurity and well-being during the early COVID-19 lockdown. Emerald Open Res. 2021, 3, 7. [Google Scholar] [CrossRef]
- Janssen, M.; Chang, B.P.I.; Hristov, H.; Pravst, I.; Profeta, A.; Millard, J. Changes in Food Consumption During the COVID-19 Pandemic: Analysis of Consumer Survey Data From the First Lockdown Period in Denmark, Germany, and Slovenia. Front. Nutr. 2021, 8, 635859. [Google Scholar] [CrossRef] [PubMed]
- Ronto, R.; Nanayakkara, J.; Worsley, A.; Rathi, N. COVID-19 & culinary behaviours of Australian household food gatekeepers: A qualitative study. Appetite 2021, 167, 105598. [Google Scholar] [CrossRef]
- Mullins, L.; Charlebois, S.; Finch, E.; Music, J. Home food gardening in Canada in response to the COVID-19 pandemic. Sustainability 2021, 13, 3056. [Google Scholar] [CrossRef]
- Lehberger, M.; Kleih, A.-K.; Sparke, K. Self-reported well-being and the importance of green spaces–A comparison of garden owners and non-garden owners in times of COVID-19. Landsc. Urban Plan. 2021, 212, 104108. [Google Scholar] [CrossRef]
- Béné, C.; Bakker, D.; Chavarro, M.J.; Even, B.; Melo, J.; Sonneveld, A. Global assessment of the impacts of COVID-19 on food security. Glob. Food Secur. 2021, 31, 100575. [Google Scholar] [CrossRef]
- Mardones, F.O.; Rich, K.M.; Boden, L.A.; Moreno-Switt, A.I.; Caipo, M.L.; Zimin-Veselkoff, N.; Alateeqi, A.M.; Baltenweck, I. The COVID-19 Pandemic and Global Food Security. Front. Vet. Sci. 2020, 7, 578508. [Google Scholar] [CrossRef]
| Section | Criteria | Include If: |
|---|---|---|
| Language | Publication reported in English | Yes |
| Design | Observational studies including prospective and retrospective cohort and cross-sectional studies; or baseline data from intervention studies. | Yes |
| Qualitative research including in-depth interviews, focus groups, ethnographic research, content analysis and case studies. | Yes | |
| Follow-up data from randomised or non-randomised trials, case reports, reviews, editorials, letter to the editor | No | |
| Population | Any age | Yes |
| Those living in rural or remote communities as classified by any regional or remote scales | Yes | |
| Urban dwelling populations, or both urban and rural dwelling populations that have not been stratified by rurality | No | |
| Content | Food security status, including the prevalence of food insecurity, as determined by any valid and reliable screening tool at an individual or population level | Yes |
| The experience of food insecurity or hunger | Yes | |
| Availability of food, including concepts of panic buying, food hoarding and food transport issues | Yes | |
| Physical access to food such as restrictions on shopping, closure of food outlets and loss of public transport. | Yes | |
| Financial access to food such as higher food prices, loss of income and lack of social support during the COVID-19 pandemic | Yes | |
| Utilization of food, including challenges and opportunities around the skills and knowledge surrounding food and food preparation throughout the pandemic | Yes | |
| Stability of the food supply such as disruptions to the labour or transport needed to maintain the food supply, including apparent consumption data. | Yes | |
| Access | Full-text article accessible | Yes |
| Reference | Author and Year | Setting | Rural Sample Size | Key Demographics | Food Security Outcome Assessed | ||||
|---|---|---|---|---|---|---|---|---|---|
| Food Insecurity Prevalence | Access | Availability | Utilization | Stability | |||||
| Quantitative Studies | |||||||||
| [45] | Giacoman et al., 2021 | Adults in rural, regional, and urban Chile | n = 504; 11.4% of sample | Total sample demographics not presented | √ | ||||
| [39] | Kent et al., 2020 | Households in Tasmania, Australia. During lockdown. | n = 305; 28% of sample | 77% female, 68% aged 46+ y; 67% had a university education | √ | ||||
| [38] | Niles et al., 2020 | Households in Vermont, USA | n = 1649; 59% of sample classified as rural dwelling | 79% female; 96% white; 65% had a university education | √ | √ | √ | √ | |
| [26] | Parekh et al., 2021 | Households in rural, suburban and urban USA | n = 1766; 31.5% of total sample rural; n = 439; 30.2% of sample with children | Households with children (62% female; 60% 40–59 years old; 70% employed) and without children (58% female; 44% 40–59 years old; 56% employed); | √ | ||||
| [41] | Men et al., 2021 | Adults in Canada | n = 692; 15.7% of sample rural dwelling | 50.8% were female; 48% household with children, 43% immigrants; 50% not working | √ | ||||
| [32] | Steimle et al., 2021 | Socioeconomically disadvantaged parents and their elementary school-aged children in rural Pennsylvania, USA | n = 272 rural families | Parents (90% mothers; mean age = 35 years) youngest child aged 4–11, 49% female | √ | √ | |||
| [30] | Mui et al., 2021 | Adults in rural and urban USA | n = 385 rural participants; 19% of total sample | Total sample demographics not presented for rural group | √ | √ | √ | ||
| [37] | Niles et al., 2021 | Households in Vermont, USA | n = 600 participants from ‘A rural state’ but rurality of participants not presented | 43.8% were aged 55 y+; 67% female | √ | √ | √ | √ | |
| [28] | Kar et al., 2021 | Store data in Franklin County, OH, USA. During and after the state-wide stay-at-home period | 7 stores in rural areas | Store characteristics included number of employees, sales, volumes. Characteristics of travellers included average trip length, % white and % income <$50 k/year | √ | ||||
| [31] | Sherbuk et al., 2020 | Patients at a HIV/AIDS clinic in the nonurban southern USA who had low income | n = 170 (total sample) | 53.5% were men, 58.8% were black, and 61.2% reported that their income fell below the federal poverty line | √ | ||||
| [46] | Simmet et al., 2021 | Food banks in Germany throughout the pandemic | n = 18 (4.5%) were rural communities (<500 inhabitants) n = 196 were small tows (5000–19,999 inhabitants) | Total sample demographics not presented | √ | ||||
| [33] | Taylor et al., 2021 | Farmers markets in Michigan, USA | n = 19 (20%) of farmers markets were in rural areas | Rural markets had a mean of 189 customers/week and 12.4 years in current location. Mean age of market managers was 55.4 years | √ | ||||
| [44] | Cohn-Schwartz et al., 2021 | Adults in rural and urban Israel | n = 92; 8% of sample were rural | Adults aged 50+, mean age 63 years, 47% women. | √ | ||||
| [47] | Jordan et al., 2021 | Adults; international; 62 different countries | n = 224; 21.4% of respondents were rural | 77% were female, 62% aged between 20 and 39 years. Study also explored influence of perceive price on intake but did not report by rurality. | √ | ||||
| [43] | Sidor and Rzymski | Adults not working regularly in Poland during lockdown (under stay-at-home orders) | n = 216; 19.7% of sample were rural | Of total sample: mean age 27.7 (SD = 9.0), 1043 (95.1%) female. 10% unemployed, 47.2% students and 42.8% full time workers. 51.7% tertiary educated | √ | ||||
| [29] | Luckstead et al., 2021 | Adults, low-skilled domestic workers, USA | Survey 1: n = 612 respondents Survey 2: n = 1036 total respondents; proportion of rural respondents not reported at either timepoint | Not reported; but respondents likely to have income below USD 50,000, without a college degree, and who are below the retirement age of sixty-five | √ | ||||
| Mixed-Methods Studies | |||||||||
| [34] | Barr et al., 2021 | Adults in Kentucky, USA (a largely rural state) | n = 92 emergency food program recipients | 72% female, mean age 43.5 ± 15 years, 37% white | √ | √ | |||
| [27] | Jackson et al., 2022 | Adults in rural and urban USA | n = 71 (19.7%) of sample | Adults aged 18–78, 52% middle aged, 51.1% female | √ | √ | |||
| [42] | Snuggs et al., 2021 | Adults in UK | n = 50; 18.8% of total sample were rural | Of total sample, 208 (86.7%) female; 213 (88.9%) lived in close proximity to a supermarket. n = 215 (89.6%) responsible for food shopping in their household | √ | ||||
| Qualitative Studies | |||||||||
| [35] | Barr et al., 2021 | Laurel County, Kentucky, USA | n = 17 | Mean age 54.9 ± 12.6 years | √ | √ | |||
| [36] | Pyle et al., 2021 | A single neighborhood in Oconee County, South Carolina, USA | n = 14 | 55% female, 65% white, 58% high school graduate | √ | ||||
| [40] | Whelan et al., 2021 | Regional community in Victoria, Australia | n = 3 supermarket managers, n = 33 customers | 55% female, did not report other statistics on participants | √ | √ | √ | ||
| Reference | Method of Data Collection | Food Security Outcome Measures | Analysis Method Used | Interpretation of Results or Key Finding Relating to Rurality Only |
|---|---|---|---|---|
| Prevalence Studies | ||||
| [45] | Telephone survey; country-wide | UN FAO Food Insecurity Experience Scale; eight questions; recall period of 30 days | Weighted descriptive statistics; multinomial logistic regression model | 53.5% of people in rural Chile were food insecure (combining mild (27.2%) and moderate-severe food insecurity (26.3%)), an increase from 29.9% pre-COVID-19 (mild = 15.7%, moderate-severe 14.2%) p < 0001. This was higher compared to 45.9% of people in metropolitan regions (mild = 24.6%, moderate-severe = 21.3%) p = 0.001. |
| [39] | Online survey; state-wide | U.S. Household Food Security Survey Module: Six-Item Short Form with recall period of 30 days | Descriptive statistics; univariate and multivariate binary logistic regression | 33% of rural respondents in Tasmania, Australia were classified into marginal, low and very low food security groups compared to 23% of their urban-dwelling counterparts. After adjusting for other characteristics, authors reported an 82% increase in experiencing food insecurity among respondents in rural areas (AOR: 1.82; SE = 0.34; 95%CI [1.28, 2.62]; p = 0.001) |
| [38] | Online survey; state-wide | U.S. Household Food Security Survey Module: Six-Item Short Form with recall periods “in the year before the coronavirus outbreak” and “since the coronavirus outbreak.” | Kruskal–Wallis tests, Wilcoxon rank sum tests, t-tests, and one-way analysis of variance (ANOVA) tests, logistical regression model | Food insecurity during COVID-19 was 25.1% for rural households, which was higher compared to 21.6% for metropolitan residents (p = 0.035). This consisted of 9.1% of non-metropolitan residents who were newly food insecure during COVID-19 and 16.0% who were food insecure pre-COVID-19. In a multivariate model, when comparing newly food insecure to consistently food-insecure households, urban dwelling respondents did not have significantly different risk compared with rural dwelling respondents (B = 0.134: SE = 0.199; 95%CI [0.523–0.255]; p = 0.499). When comparing newly food-insecure to consistently food-insecure households, urban-dwelling respondents did not have significantly different risk compared with rural dwelling respondents (B = 0.136: SE = 0.177; 95%CI [0.212–0.484]; p = 0.443). |
| [26] | Online survey; country-wide | U.S. Household Food Security Survey Module: Six-Item Short Form with recall period of 90 days | Descriptive statistics; multivariable logistic regression | For rural-dwelling households, 15.3% were food insecure, comprising 8.3% who were food insecure and 7.0% with very low food security. This was compared to urban and suburban households with 14.5% FI who had significantly lower rates of very low food security (5.6%, p = 0.041). In multivariate analysis for the whole study sample and sample “households with children”, a rural dwelling was not significantly different to suburban areas for food insecurity, adjusting for sex, age, race, region, employment, marital status, education, income, number of people in household (whole study sample AOR: 0.91; 95% CI [0.73–1.12]; sample ”households with children” AOR: 0.94; 95%CI [0.64–1.38]) |
| [34] | Online survey; emergency food program recipients | Hager two-item screener | Descriptive statistics | 95% of the sample (participants of a rural emergency food program) were classified as food insecure. |
| [37] | Online survey; convenience sample of Vermont households from August and September 2020 | U.S. Department of Agriculture’s (USDA) Household Food Security Survey Module: Six-Item Short Form, recall periods both “in the year before the coronavirus outbreak” and “since the coronavirus outbreak. | Multivariate logistic regression | 29% (n = 169) of respondents (and their households) were classified as food insecure since the onset of the COVID-19 pandemic. |
| [32] | Daily text-messaged surveys of families in a food assistance program during and after school closures located in rural Pennsylvania | Four daily survey questions assessed families’ levels of FI, all adapted for daily use from the Current Population Survey Food Security Supplement | Multilevel, mixed-effects models | For families with children in rural Pennsylvania, all indicators of daily FI significantly increased when schools closed in their region, and gradually decreased in the months that followed. The mean sum of FI question increased from 0.77 before closures to 0.84 after closures (p < 0.001). Before and after school closures, the food insecurity (%) was reported for
|
| [27] | Online, cross-sectional survey | Food insecurity determined using the Hager 2-item food insecurity screener with a recall period of “since the COVID-19 pandemic” began. | Multivariate analysis of covariance (MANCOVA) followed by pairwise univariate tests | 40% of participants reported food insecurity. Rurality was not significantly associated with food insecurity. |
| [41] | Online survey, Canada wide | Household food insecurity in the past 30 days determined by a six-item questionnaire adapted from the 18-item questionnaire that is routinely used to monitor 12-month food insecurity in Canada | Prevalence of outcomes t-tests, two-part regression | 14.9% of rural dwelling Canadian adults were food insecure, significantly higher than for non-rural adults (11.3%, p = 0.017). Greater food insecurity in urban versus rural respondents (unadjusted). In an adjusted model, households with children rural residents were more likely to be food insecure than urban households without children, compared with urban residents, respectively. |
| [30] | Online survey, USA Country-wide | Food insecurity was determined by adapting the 2-item Hunger Vital Sign screening tool with a recall period of the past 30 days of the COVID-19 pandemic. | Chi-square tests | Food insecurity was significantly higher in rural adults (40.5 %; n = 156) in the USA, at 62.3 % in urban areas and 36.7 % in suburban areas (p < 0.001). A higher proportion of food-insecure adults in rural regions acquired food from supercentres (61.5%; 95% CI [50.4%,72.5%]; p < 0.05), than food-insecure adults in suburban areas. |
| Food Availability | ||||
|---|---|---|---|---|
| Reference | Method of Data Collection | Outcome Measures | Analysis Method Used | Interpretation of Results or Key Finding Relating to Rurality Only |
| [38] | Online survey; state-wide | Close-ended question developed for the study asked respondents if food was unavailable to them. | Kruskal–Wallis tests, Wilcoxon rank sum tests, t-tests, and one-way analysis of ANOVA | Food-insecure respondents were more likely to report that food was unavailable to them during the pandemic than food-secure households, regardless of rurality. |
| [30] | Online survey; USA wide | One question of food availability in food in retailers | Chi square test | 35% of rural participants reported that there was limited availability of food in retailers, compared to urban dwelling (~40%) and suburban (~30%) areas. |
| [46] | Online survey of food banks in one organization | Days of operation during the COVID-19 pandemic | Chi square test | Of the 401 food banks for which data were available, 58.6% were closed at some point from 16 March to 3 May 2020. On average, food banks were closed 48.1 days (SD 28.7). There were no differences between closed and open food banks concerning the size of the municipality the food bank was located in. |
| [33] | Telephone or self-administered surveys of Farmer’s Market managers | Participation in subsidized nutrition programs to reduce FI and Impact of COVID-19 on operations | Descriptive statistics | Rural farmers markets:
|
| [40] | Focus groups and group model building | Group model building was undertaken to map issues impacting on the food supply and consumer behaviour | Thematic analysis and causal loop diagrams to describe the system | Rural supermarket managers described ‘empty shelves’ due to panic buying, product unavailability, and community fear generated from the media/mixed messaging. Customers reported fear of not being able to access the food they needed during lockdowns. |
| Food Access | ||||
|---|---|---|---|---|
| Reference | Method of Data Collection | Outcome Measures | Analysis Method Used | Interpretation of Results or Key Finding Relating to Rurality Only |
| [37] | Online survey; convenience sample of Vermont households from August and September 2020 | Thirteen home food procurement variables developed about home food procurement (local food, gardening, fishing, foraging, hunting, livestock, and canning) examining current practices and changes during the COVID-19 pandemic, | Descriptive statistics | A third of all respondents (34.5%; n = 205) engaged in home food procurement activities during the first 6 months of the COVID-19 pandemic. The activities included gardening (34.7%), followed by canning (23.5%) and fishing (10.2%). Most people who engaged in home food procurement activities, 51.8% (n = 128), performed at least one home food procurement activity more intensely since the COVID-19 pandemic began. |
| [31] | Screening patients during standard care. Developed a database of food bank/home delivered meals services provided by the clinic during April 2020 and the preceding 12 months (March 2019 to February 2020). | The variables used to assess food insecurity included: change in employment among patients at risk based on self-report; food support provided through gift cards or delivery of food boxes. | Descriptive statistics | Support for food services increased 66% during April 2020, from 131 average monthly services to 218 services. Home-delivered meals were the most common source of support for patients. |
| [32] | Daily text messaged surveys of families in a food assistance program during and after school closures located in rural Pennsylvania | Weekly frequency of receiving a “Power Pack” and frequency of use of “Grab and Go” meal options. | Multilevel, mixed-effects models | Families who experienced a greater increase in food insecurity during school closures were more likely to rely upon emergency food relief parcels (“power pack”). Using the power pack services was associated with greater recovery from food insecurity throughout the pandemic. Use of Grab and Go meals was not associated with changes in food insecurity. |
| [38] | Online survey; state-wide | Close-ended questions developed for the study explored food access challenges and concerns; use of food assistance programs | Kruskal–Wallis tests, Wilcoxon rank sum tests, t-tests, and one-way analysis of variance (ANOVA) | Food-insecure households reported more food access challenges compared to food-secure households, including trouble affording food, getting food through a food pantry, and which services were available to help getting food, but this was not affected by rurality. |
| [34] | Online survey; emergency food program recipients | Open-ended response survey data | Thematic analysis | An emergency food program help alleviate issues of food access (physical and financial) during the pandemic, due to reduced income by “keeping food on the table” and “reducing the frequency of leaving the house”. |
| [35] | Focus groups; community residents | Exploring experiences in the changes to the food environment during the pandemic | Grounded theory | Respondents described how COVID-19 increased emergency food assistance while other health resources (such as through a library) were restricted. Positive experiences were found with the expansion and utilization of online food ordering, which increased access to food. |
| [36] | In-depth interviews; community residents | Exploring experiences and the effects of the crises (disasters and pandemics) on community members’ access to food. | A post-positivist theoretical frame | Rural respondents described how food insecurity existed prior to COVID-19, but was exacerbated by the pandemic and disasters in the rural community. Others faced only short-term food insecurity depending on their social networks. A major recurring issue was the scarcity of healthy foods and an increase in food costs during the pandemic. |
| [40] | Focus groups and group model building | Group model building was undertaken to map issues impacting on the food supply and consumer behaviour | Thematic analysis and causal loop diagrams to describe the system | The nearest larger grocery retailers for one rural community were approximately 70 km by road, inaccessible to many residents during ‘lockdown’. Fear of COVID-19 and of not being able to access food drove panic buying in a rural community. |
| [28] | Changes in food access based on observed travel data for all grocery shopping trips during and after the state-wide stay-at-home period. | Data in this study were store locations and characteristics store visits (weekly count of customers) assumed characteristics of incoming shoppers as inferred from their origins, and characteristics of store locations | Variables explored was difference in average weekly store visits to during lockdown and initial reopening phases of the pandemic. | During lockdown, traffic declined 2.5 times more in urban stores than those located in rural areas. Stores in urban area experienced a decline in traffic 7.5 times greater than that of a store located in a rural area during the initial reopening phases. |
| [30] | Online survey | Barriers to food access and transport mode to obtain food | Chi-square tests | Transportation as a barrier did not vary significantly between rural and urban regions. However, food-insecure adults in urban areas faced more barriers to food access and issues obtaining culturally appropriate foods than those in rural areas |
| Utilization of Food | ||||
|---|---|---|---|---|
| Reference | Method of Data Collection | Outcome Measures | Analysis Method Used | Interpretation of Results or Key Finding Relating to Rurality Only |
| [38] | Online survey; state-wide | Close-ended question developed for the study asked respondents about concerns of food safety. | Kruskal–Wallis tests, Wilcoxon rank sum tests, t-tests, and one-way ANOVA | Food-insecure respondents were more concerned about the safety of food during the COVID-19 pandemic than food-secure households, regardless of rurality. |
| [37] | Online survey; convenience sample of Vermont households from August and September 2020 | Authors developed new questions to measure perceived change in fruit/vegetable and red meat/processed meat consumption since the onset of the COVID-19 pandemic. | Descriptive statistics | Of the sample of rural adults, nearly one in four (23.3%) respondents indicated that ate fewer fruits and vegetables during the pandemic as compared to before, most (65.5%) reported eating the same as before COVID-19, and 11.2% reported eating more. A quarter (25.9%) of respondents reported eating less red and/or processed meat since the start of the COVID-19 pandemic, and 7.9% reported eating more. |
| [44] | Telephone surveys; country-wide | A single item-question about stocking up food for emergency. | Descriptive data and bivariate analyses | Rural adults were less likely to report stocking up on food than adults living in urban localities. |
| [35] | Focus groups; community residents | Exploring changes to the food environment during the pandemic | Grounded theory | Rural respondents described how COVID-19 changed the home food environment, including spending more time cooking and eating at home, and increased produce gardening. |
| [43] | Online cross-sectional survey | Change in food concussion during quarantine; Frequency of consumption of selected food products, Frequency of breakfast consumption during quarantine; Level of fear of contracting SARS-CoV-2 during grocery shopping and contact with food products. | Correlation analysis | Changes in food consumption, snacking, and cooking, eating breakfast, during the quarantine were not differentiated by rurality (p > 0.05). Fears regarding contracting COVID-19 from shopping or food sources was not associated with rurality. |
| [42] | Online survey through social media; close and open-ended questions | The Food Choice Questionnaire and The Family Mealtime Goals Questionnaire. Open-ended questions. | Repeated measures ANOVA | There was no significant effect of suburban/rural location on any of the food choices made by participants in the study. |
| [27] | Online survey using open-ended and close-ended questions | Diet quality was measured using the dietary screener questionnaire (DSQ), which was modified to assess intake over the past week. Individual nutrient intakes were then combined into an overall measure of diet quality | Multivariate analysis of covariance (MANCOVA) followed by pairwise univariate tests | Over 60% of participants scored a 2 or lower on the 6-point scale of diet quality. Rurality was not linked to dietary quality. However, social connection and changes in dietary behaviour occurred during the pandemic, with food-insecure adults reporting a reduction in diet quality. |
| [47] | Online survey. | Changes in food quantity, fruit and vegetable consumption as a result of pandemic restrictions. Study also explored the influence of perceive price on intake using open-ended questions but did not report by rurality for this outcome. | Binary logistic regression models and Poisson regression models were calculated to evaluate changes in consumption patterns and to test associations with COVID-19 related factors | The overall effect of living environment was not a significantly influencing vegetable. Regarding consumption, however, among residents of ‘small towns’ (not defined clearly as rural in this study), 20% more (compared to mega cities) reported either an increase/decrease in vegetable intakes. Living in a small town was associated with a reduction in diversity in each of the five vegetable groups reported to be consumed. |
| Stability | ||||
|---|---|---|---|---|
| Reference | Method of Data Collection | Food Security Outcome Measures | Analysis Method Used | Interpretation of Results or Key Finding Relating to Rurality Only |
| [29] | Online survey of a representative sample of low-skilled domestic workers’ attitudes; USA country wide | Perceived importance of agriculture food production and concern about having a food shortage due to the effect of COVID-19 amid the coronavirus crisis. | Descriptive statistics; Logistic and Order Logistic regression | On average, the total sample of respondents perceived that agricultural production was more important than before the crisis and were more concerned about a food shortage than prior to the pandemic. There was no difference between rural and urban respondents regarding the perceived importance of agricultural production and concern for food shortage. |
| [40] | Focus groups and group model building | Group model building was undertaken to map issues impacting on the food supply and consumer behaviour | Thematic analysis and causal loop diagrams to describe the system | Supermarket managers described an unpredictability in consumer behaviour as well as supply chain issues as a result of COVID-19, that led to a lack of stability in the local food supply. The supply chain struggled to re-orient itself in a tight time frame. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kent, K.; Alston, L.; Murray, S.; Honeychurch, B.; Visentin, D. The Impact of the COVID-19 Pandemic on Rural Food Security in High Income Countries: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 3235. https://doi.org/10.3390/ijerph19063235
Kent K, Alston L, Murray S, Honeychurch B, Visentin D. The Impact of the COVID-19 Pandemic on Rural Food Security in High Income Countries: A Systematic Literature Review. International Journal of Environmental Research and Public Health. 2022; 19(6):3235. https://doi.org/10.3390/ijerph19063235
Chicago/Turabian StyleKent, Katherine, Laura Alston, Sandra Murray, Bonnie Honeychurch, and Denis Visentin. 2022. "The Impact of the COVID-19 Pandemic on Rural Food Security in High Income Countries: A Systematic Literature Review" International Journal of Environmental Research and Public Health 19, no. 6: 3235. https://doi.org/10.3390/ijerph19063235
APA StyleKent, K., Alston, L., Murray, S., Honeychurch, B., & Visentin, D. (2022). The Impact of the COVID-19 Pandemic on Rural Food Security in High Income Countries: A Systematic Literature Review. International Journal of Environmental Research and Public Health, 19(6), 3235. https://doi.org/10.3390/ijerph19063235






