Appraising Evidence-Based Mental Health and Psychosocial Support (MHPSS) Guidelines—PART I: A Systematic Review on Methodological Quality Using AGREE-HS
Abstract
:1. Introduction
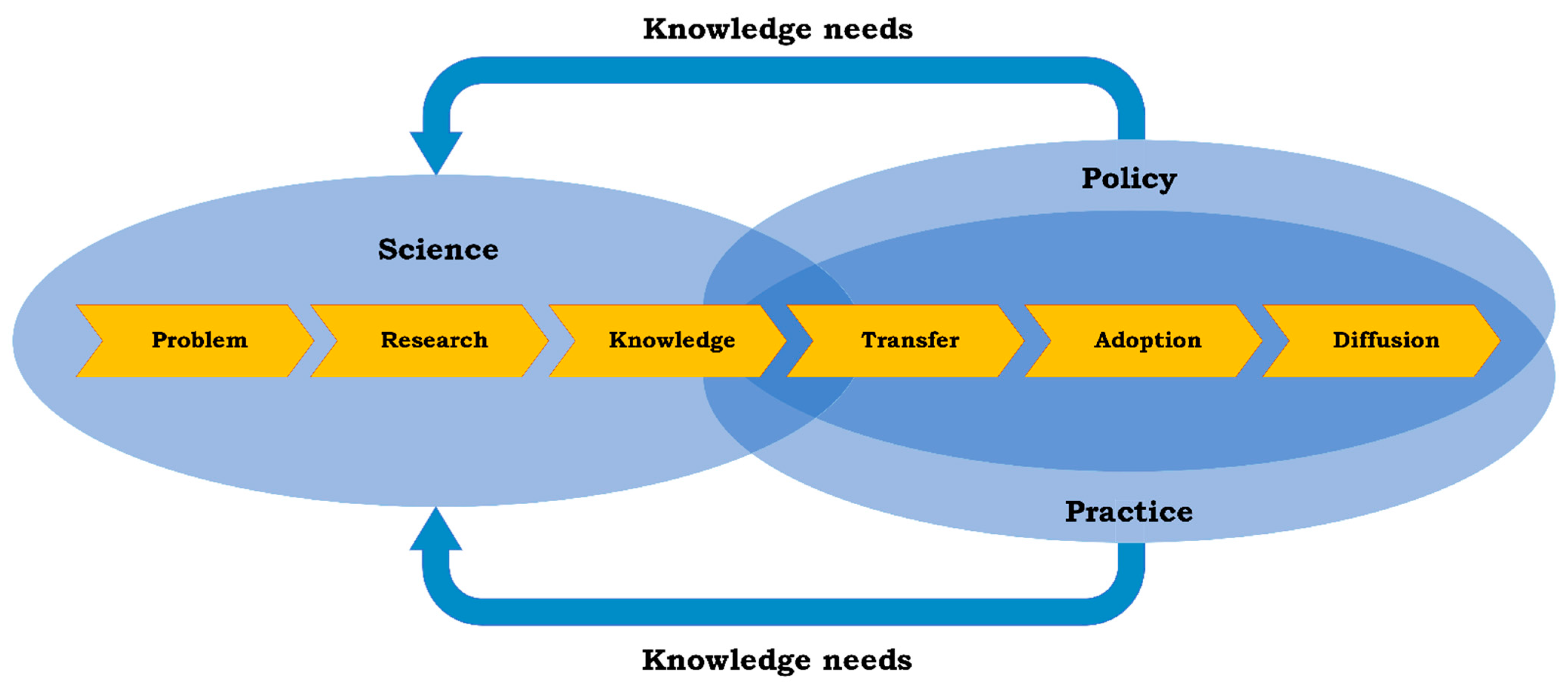
1.1. Merging Disaster Risk Reduction and Mental Health and Psychosocial Support
1.2. Study Focus
2. Materials and Methods
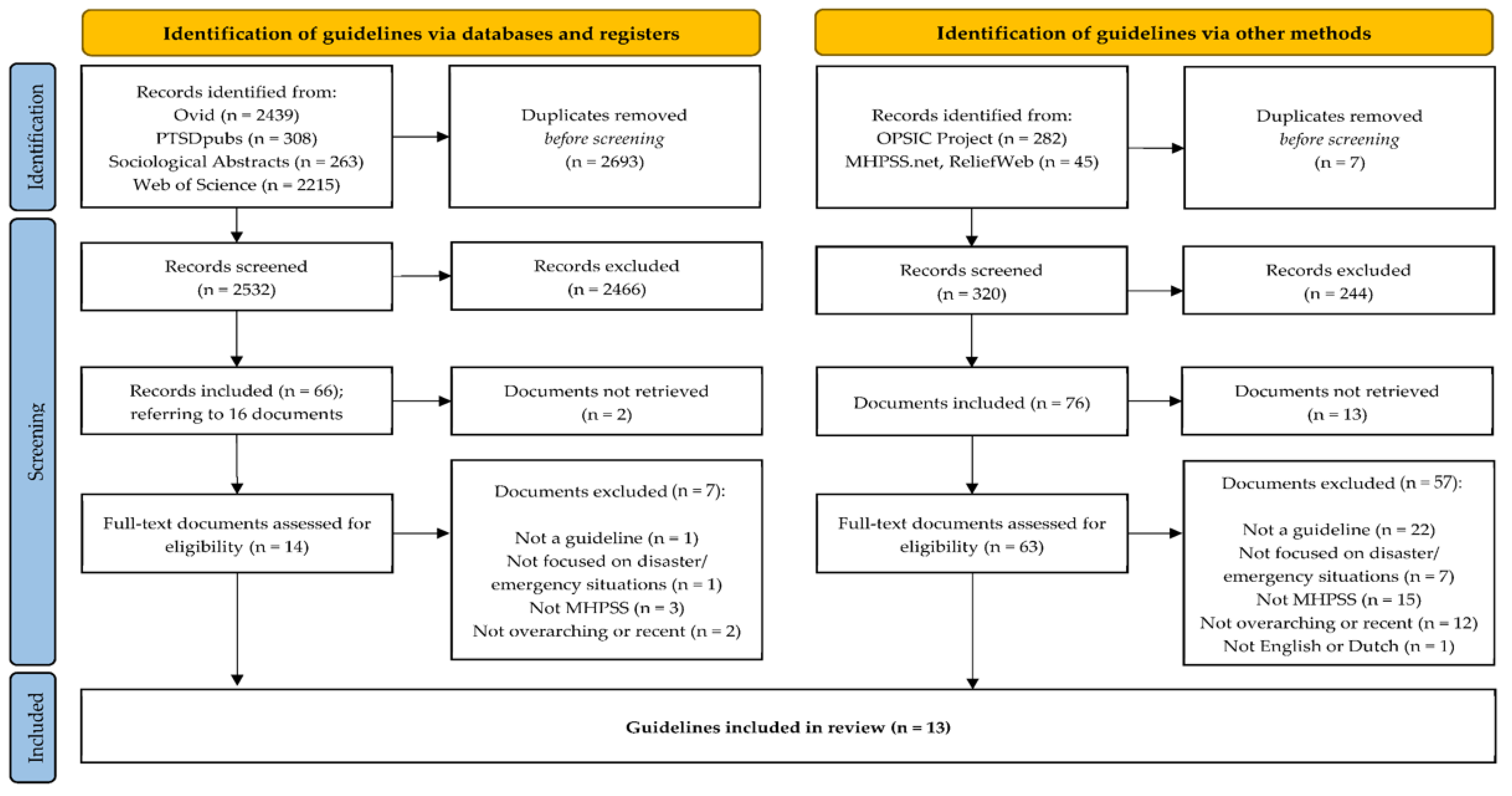
2.1. The Guideline Search
2.2. Guideline Selection (Eligibility Criteria)
- The document is a ‘guideline’ as defined by AGREE-HS (i.e., “Health systems guidance or guideline documents are systematically developed statements to assist with decisions about appropriate options for addressing health system challenges, the implementation of these options, and the monitoring and evaluation of the implementation efforts” [21] (p. iii));
- The document is focused on disaster/emergency situations;
- The core topic of the document concerns the organization of MHPSS, not the use of (one-on-one) interventions, thus the guidance is focused on the organizational or (inter)national level;
- When documents stem from a main ‘overarching guideline’, (i.e., they are spin-offs, such as target group specific translations or practical protocols), only the overarching or most recent version of the document is included;
- The document is available in the English or Dutch language and can be found online.
2.3. Appraisal of Methodological Quality
3. Results
3.1. Guideline Search and Selection
3.2. Appraisal of Methodological Quality
3.2.1. Topic
3.2.2. Participants
3.2.3. Methods
3.2.4. Recommendations
3.2.5. Implementability
4. Discussion
4.1. Retrieving MHPSS Guidelines
4.2. Improving the Methodological Quality of MHPSS Guidelines
4.3. What to Conclude concerning the Implications for Disaster Risk Reduction?
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Literature Search Strategy
| 1 | (((natural or Human-induced or Technological or Societal) adj1 (accident or accidents or hazard*)) or disaster* or epidemic* or pandemic* or “armed conflict*” or war or warfare or crisis or crises or emergencies or “critical incident*”).ti,ab. |
| 2 | (DRM or “disaster risk management” or MHPSS or “Mental health and psychosocial support” or “mental health and psychosocial issue*” or (community adj1 (mobilisation or support or self-help)) or PFA or ((Psychosocial or Psychological or social or “mental health”) adj1 (“first aid” or care or support or assist* or management))).ti,ab. |
| 3 | (guideline or framework or manual or toolkit or “implementation plan” or “systematic review” or “systematic literature” or “integrative review” or “integrative literature” or “evidence-based review” or “evidence-based overview” or meta-analy* or metaanaly* or metanaly*).ti,ab. or “Treatment Guidelines”/or exp “Practice Guidelines as Topic”/or exp “Guidelines as Topic”/ |
| 4 | 1 and 2 and 3 |
| 5 | limit 4 to yr = “2007-Current” [Limit not valid in DARE; records were retained] |
References
- Behlert, B.; Diekjobst, R.; Felgentreff, C.; Manandhar, T.; Mucke, P.; Pries, L.; Radtke, K.; Weller, D. World Risk Report 2020: Forced Displacement and Migration; Bündnis Entwicklung Hilft and Ruhr University Bochum—Institute for International Law of Peace and Armed Conflict (IFHV): Bochum, Germany, 2020; ISBN 978-3-946785-10-1. [Google Scholar]
- International Federation of Red Cross and Red Crescent Societies. World Disasters Report: Come Heat or High Water; International Federation of Red Cross and Red Crescent Societies: Geneva, Switzerland, 2020; ISBN 978-2-9701289-5-3. [Google Scholar]
- United Nations Office for the Coordination of Humanitarian Affairs Global Humanitarian Overview 2021. Available online: https://gho.unocha.org/ (accessed on 20 July 2021).
- Bonde, J.P.; Utzon-Frank, N.; Bertelsen, M.; Borritz, M.; Eller, N.H.; Nordentoft, M.; Olesen, K.; Rod, N.H.; Rugulies, R. Risk of Depressive Disorder Following Disasters and Military Deployment: Systematic Review with Meta-Analysis. Br. J. Psychiatry J. Ment. Sci. 2016, 208, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Brewin, C.R.; Kaniasty, K.; Greca, A.M.L. Weighing the Costs of Disaster: Consequences, Risks, and Resilience in Individuals, Families, and Communities. Psychol. Sci. Public Interest J. Am. Psychol. Soc. 2010, 11, 1–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neria, Y.; Nandi, A.; Galea, S. Post-Traumatic Stress Disorder Following Disasters: A Systematic Review. Psychol. Med. 2008, 38, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Reifels, L.; Mills, K.; Dückers, M.L.A.; O’Donnell, M.L. Psychiatric Epidemiology and Disaster Exposure in Australia. Epidemiol. Psychiatr. Sci. 2017, 28, 310–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Safarpour, H.; Sohrabizadeh, S.; Malekyan, L.; Safi-Keykaleh, M.; Pirani, D.; Daliri, S.; Bazyar, J. Suicide Death Rate after Disasters: A Meta-Analysis Study. Arch. Suicide Res. Off. J. Int. Acad. Suicide Res. 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- United Nations Office for Disaster Risk Reduction (UNDRR) Disaster Risk Reduction. Available online: https://www.undrr.org/terminology/disaster-risk-reduction (accessed on 20 July 2021).
- Gray, B.; Hanna, F.; Reifels, L. The Integration of Mental Health and Psychosocial Support and Disaster Risk Reduction: A Mapping and Review. Int. J. Environ. Res. Public. Health 2020, 17, 1900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inter-Agency Standing Committee (IASC). IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings; IASC: Geneva, Switzerland, 2006. [Google Scholar]
- Bisson, J.; Tavakoly, B. The TENTS Guidelines for Psychosocial Care Following Disasters and Major Incidents; Cardiff University: Cardiff, UK, 2008. [Google Scholar]
- Te Brake, H.; Dückers, M.; De Vries, M.; Van Duin, D.; Rooze, M.; Spreeuwenberg, C. Early Psychosocial Interventions after Disasters, Terrorism, and Other Shocking Events: Guideline Development. Nurs. Health Sci. 2009, 11, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.E.; Jordans, M.J.D.; Tol, W.A.; Galappatti, A. A Call for Greater Conceptual Clarity in the Field of Mental Health and Psychosocial Support in Humanitarian Settings. Epidemiol. Psychiatr. Sci. 2021, 30, e5. [Google Scholar] [CrossRef]
- Tol, W.A.; Purgato, M.; Bass, J.K.; Galappatti, A.; Eaton, W. Mental Health and Psychosocial Support in Humanitarian Settings: A Public Mental Health Perspective. Epidemiol. Psychiatr. Sci. 2015, 24, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Dückers, M. Capturing Intervention in Its Context: The Next Frontier in Disaster Response Evaluation and Scale-Up Planning. Intervention 2021, 19, 4. [Google Scholar] [CrossRef]
- Généreux, M.; Lafontaine, M.; Eykelbosh, A. From Science to Policy and Practice: A Critical Assessment of Knowledge Management before, during, and after Environmental Public Health Disasters. Int. J. Environ. Res. Public. Health 2019, 16, 587. [Google Scholar] [CrossRef] [Green Version]
- Van Hoof, W.; Willems, A.; Te Brake, H.; Dückers, M.L.A. Appraising Evidence-Based Mental Health and Psychosocial Support (MHPSS) Guidelines—PART II: A Qualitative Content Analysis. underreview. 2022. [Google Scholar]
- AGREE Collaboration Development and Validation of an International Appraisal Instrument for Assessing the Quality of Clinical Practice Guidelines: The AGREE Project. Qual. Saf. Health Care 2003, 12, 18–23. [CrossRef] [PubMed]
- Brouwers, M.C.; Ako-Arrey, D.; Spithoff, K.; Vukmirovic, M.; Florez, I.D.; Lavis, J.N.; Cluzeau, F.; Permanand, G.; Bosch-Capblanch, X.; Chen, Y.; et al. Validity and Usability Testing of a Health Systems Guidance Appraisal Tool, the AGREE-HS. Health Res. Policy Syst. 2018, 16, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- AGREE-HS Research Team. The Appraisal of Guidelines Research & Evaluation—Health Systems (AGREE-HS). Available online: https://www.agreetrust.org/wp-content/uploads/2018/03/AGREE-HS-Manual-March-2018.pdf (accessed on 28 September 2021).
- Paez, A. Gray Literature: An Important Resource in Systematic Reviews. J. Evid.-Based Med. 2017, 10, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Juen, B.; Warger, R.; Nindl, S.; Siller, H.; Lindenthal, M.J.; Huttner, E.; Ajdukovic, D.; Bakic, H.; Olff, M.; Thormar, S. The Comprehensive Guideline on Mental Health and Psychosocial Support (MHPSS) in Disaster Settings; OPSIC: Innsbruck, Austria, 2016. [Google Scholar]
- The MHPSS Network Emergency Toolkit. Available online: https://www.mhpss.net/toolkits/emergency (accessed on 28 September 2021).
- Reliefweb about ReliefWeb. Available online: https://reliefweb.int/about (accessed on 28 September 2021).
- The MHPSS Network What We Do. Available online: https://www.mhpss.net (accessed on 28 September 2021).
- AGREE Collaboration AGREE Enterprise Website. Available online: https://www.agreetrust.org/resource-centre/agree-ii/ (accessed on 28 September 2021).
- AGREE-HS Research Team. AGREE-Health Systems (AGREE-HS) Reporting Checklist. Available online: http://www.agreetrust.org (accessed on 28 September 2021).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Lee, H.Y.; Lee, M.K.; Kim, S.; Lee, S.; Lee, H.-W.; Park, E.J.; Sim, M.; Paik, J.-W. Development of Korean Disaster Mental Health Support Guidelines: Results of a Scoping Review and a Delphi Survey. Psychiatry Investig. 2019, 16, 130–138. [Google Scholar] [CrossRef]
- International Committee of the Red Cross. Guidelines on Mental Health and Psychosocial Support; International Committee of the Red Cross: Geneva, Switzerland, 2018. [Google Scholar]
- European Network for Psychosocial Crisis Management (EUNAD). Assisting People with Disabilities in Case of Disaster; Federal Office of Civil Protection and Disaster Assistance: Bonn, Germany, 2017; ISBN 978-3-939347-85-9. [Google Scholar]
- World Health Organization and United Nations High Commissioner for Refugees. MhGAP Humanitarian Intervention Guide (MhGAP-HIG); WHO: Geneva, Switzerland, 2015; ISBN 978 92 4 154892 2. [Google Scholar]
- Werkgroep Multidisciplinaire Richtlijnontwikkeling Psychosociale Hulp Bij Rampen en Crises, Multidisciplinaire Richtlijnontwikkeling Psychosociale Hulp Bij Rampen en Crises; ARQ Kenniscentrum Impact van Rampen en Crises: Diemen, The Netherlands, 2014; ISBN 978-90-78273-22-6.
- World Health Organization, War Trauma Foundation and World Vision International. Psychological First Aid: Guide for Field Workers; WHO: Geneva, Switzerland, 2011; ISBN 978-92-4-154861-8. [Google Scholar]
- DH Emergency Preparedness Division. Psychosocial Care for People Affected by Disasters and Major Incidents; NHS Department of Health: London, UK, 2009.
- NATO Joint Medical Committee. Psychosocial Care for People Affected by Disasters and Major Incidents: A Model for Designing, Delivering and Managing Psychosocial Services for People Involved in Major Incidents, Conflict, Disasters and Terrorism; NATO: Brussels, Belgium, 2008. [Google Scholar]
- Brymer, M.; Jacobs, A.; Layne, C.; Pynoos, R.; Ruzek, J.; Steinberg, A.; Vernberg, E.; Watson, P. Psychological First Aid: Field Operations Guide, 2nd ed.The National Child Traumatic Stress Network and National Center for PTSD; Available online: https://www.nctsn.org/ (accessed on 27 March 2019).
- Psycho-Social Support in Situations of Mass Emergency. A European Policy Paper Concerning Different Aspects of Psychological Support and Social Accompaniment for People Involved in Major Accidents and Disasters; Seynaeve, G.J.R., Ed.; Ministry of Public Health: Brussels, Belgium, 2001; ISBN D/2001/9387/1.
- Brouwers, M.C.; Lavis, J.N.; Spithoff, K.; Vukmirovic, M.; Florez, I.D.; Velez, M.; Kibria, M.; Sekercioglu, N.; Kamler, E.; Halladay, J.; et al. Assessment of Health Systems Guidance Using the Appraisal of Guidelines for Research and Evaluation—Health Systems (AGREE-HS) Instrument. Health Policy 2019, 123, 646–651. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.; Chemaly, W.S.; Hanna, F.; Polutan-Teulières, N.; Ventevogel, P. Engagement of Protection Actors in MHPSS: The Need for Cross-Sectoral Cooperation. Forced Migr. Rev. 2021, 4, 8–11. [Google Scholar]
- Tol, W.A.; Patel, V.; Tomlinson, M.; Baingana, F.; Galappatti, A.; Silove, D.; Sondorp, E.; van Ommeren, M.; Wessells, M.G.; Panter-Brick, C. Relevance or Excellence? Setting Research Priorities for Mental Health and Psychosocial Support in Humanitarian Settings. Harv. Rev. Psychiatry 2012, 20, 25–36. [Google Scholar] [CrossRef] [PubMed]
| Origin | Guideline Author(s) [Reference] | Short Title | |||
|---|---|---|---|---|---|
| A | B | C | D | ||
| 1 | 0 | 0 | 0 | Lee et al. [30] | Korean Guidelines 2019 |
| 0 | 0 | 1 | 0 | The International Committee of the Red Cross [31] | Red Cross Guidelines 2018 |
| 0 | 0 | 0 | 1 | European Network for Psychosocial Crisis Management (EUNAD) [32] | EUNAD Guidelines 2017 |
| 0 | 0 | 0 | 1 | Juen et al. [23] | OPSIC 2016 |
| 4 | 2 | 1 | 1 | World Health Organization & United Nations High Commissioner for Refugees [33] | MhGAP 2015 |
| 2 | 0 | 0 | 1 | Werkgroep multidisciplinaire richtlijnontwikkeling psychosociale hulp bij rampen en crises [34] | Dutch Guidelines 2014 |
| 6 | 1 | 0 | 1 | World Health Organization, War Trauma Foundation & World Vision International [35] | PFA Field Workers 2011 |
| 0 | 0 | 0 | 1 | DH Emergency Preparedness Division [36] | NHS Guidelines 2009 |
| 1 | 0 | 0 | 1 | Bisson & Tavakoly [12] | TENTS Guidelines 2008 |
| 0 | 0 | 0 | 1 | NATO Joint Medical Committee [37] | NATO Guidelines 2008 |
| 33 | 0 | 1 | 1 | Inter-Agency Standing Committee (IASC) [11] | IASC Guidelines 2007 |
| 8 | 0 | 0 | 1 | Brymer et al. [38] | PFA Field Operations 2006 |
| 0 | 0 | 0 | 1 | Seynaeve [39] | European Policy Paper 2001 |
| AGREE (SD) | #Raters | Short Title [Reference] | AGREE Items | ||||
|---|---|---|---|---|---|---|---|
| Topic | Participants | Methods | Recommendations | Implementability | |||
| 67.6 (8.4) | 4 | Dutch Guidelines 2014 [34] | 6.3 | 4.8 | 5.6 | 4.9 | 3.8 |
| 63.6 (11.7) | 4 | IASC Guidelines 2007 [11] | 6.2 | 4.7 | 3.8 | 5.4 | 4.1 |
| 60.8 (9.6) | 4 | Red Cross Guidelines 2018 [31] | 6.6 | 2.7 | 2.8 | 6.3 | 4.9 |
| 56.8 (11.5) | 3 | OPSIC 2016 [23] | 6.3 | 3.6 | 4.5 | 4.8 | 2.9 |
| 48.5 (2.6) | 3 | EUNAD Guidelines 2017 [32] | 5.8 | 3.4 | 4.0 | 4.3 | 2.1 |
| 44.2 (1.8) | 3 | NATO Guidelines 2008 [37] | 5.3 | 3.1 | 3.4 | 3.7 | 2.8 |
| 41.5 (21.4) | 3 | Korean Guidelines 2019 [30] | 4.5 | 3.2 | 4.8 | 3.0 | 1.9 |
| 41.1 (6.9) | 3 | European Policy Paper 2001 [39] | 5.7 | 3.0 | 1.7 | 3.7 | 3.3 |
| 41.0 (9.6) | 3 | PFA Field Workers 2011 [35] | 5.3 | 3.7 | 1.5 | 4.7 | 2.1 |
| 37.3 (16.0) | 4 | MhGAP 2015 [33] | 5.4 | 3.0 | 2.1 | 3.5 | 2.3 |
| 35.4 (13.1) | 3 | NHS Guidelines 2009 [36] | 5.3 | 2.3 | 3.0 | 3.3 | 1.8 |
| 34.1 (11.4) | 5 | TENTS Guidelines 2008 [12] | 3.2 | 2.9 | 3.0 | 3.3 | 2.0 |
| 31.2 (16.8) | 3 | PFA Field Operations 2006 [38] | 3.5 | 1.8 | 1.3 | 3.3 | 1.6 |
| Mean overall score per AGREE-item: | 5.3 | 3.2 | 3.2 | 4.2 | 2.7 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
te Brake, H.; Willems, A.; Steen, C.; Dückers, M. Appraising Evidence-Based Mental Health and Psychosocial Support (MHPSS) Guidelines—PART I: A Systematic Review on Methodological Quality Using AGREE-HS. Int. J. Environ. Res. Public Health 2022, 19, 3107. https://doi.org/10.3390/ijerph19053107
te Brake H, Willems A, Steen C, Dückers M. Appraising Evidence-Based Mental Health and Psychosocial Support (MHPSS) Guidelines—PART I: A Systematic Review on Methodological Quality Using AGREE-HS. International Journal of Environmental Research and Public Health. 2022; 19(5):3107. https://doi.org/10.3390/ijerph19053107
Chicago/Turabian Stylete Brake, Hans, Andrea Willems, Charlie Steen, and Michel Dückers. 2022. "Appraising Evidence-Based Mental Health and Psychosocial Support (MHPSS) Guidelines—PART I: A Systematic Review on Methodological Quality Using AGREE-HS" International Journal of Environmental Research and Public Health 19, no. 5: 3107. https://doi.org/10.3390/ijerph19053107
APA Stylete Brake, H., Willems, A., Steen, C., & Dückers, M. (2022). Appraising Evidence-Based Mental Health and Psychosocial Support (MHPSS) Guidelines—PART I: A Systematic Review on Methodological Quality Using AGREE-HS. International Journal of Environmental Research and Public Health, 19(5), 3107. https://doi.org/10.3390/ijerph19053107






