The Workplace and Psychosocial Experiences of Australian Senior Doctors during the COVID-19 Pandemic: A Qualitative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Australian COVID-19 Frontline Healthcare Workers Study
2.2. Senior Doctors Sub-Study
2.3. Ethics
3. Findings
3.1. Study Participants
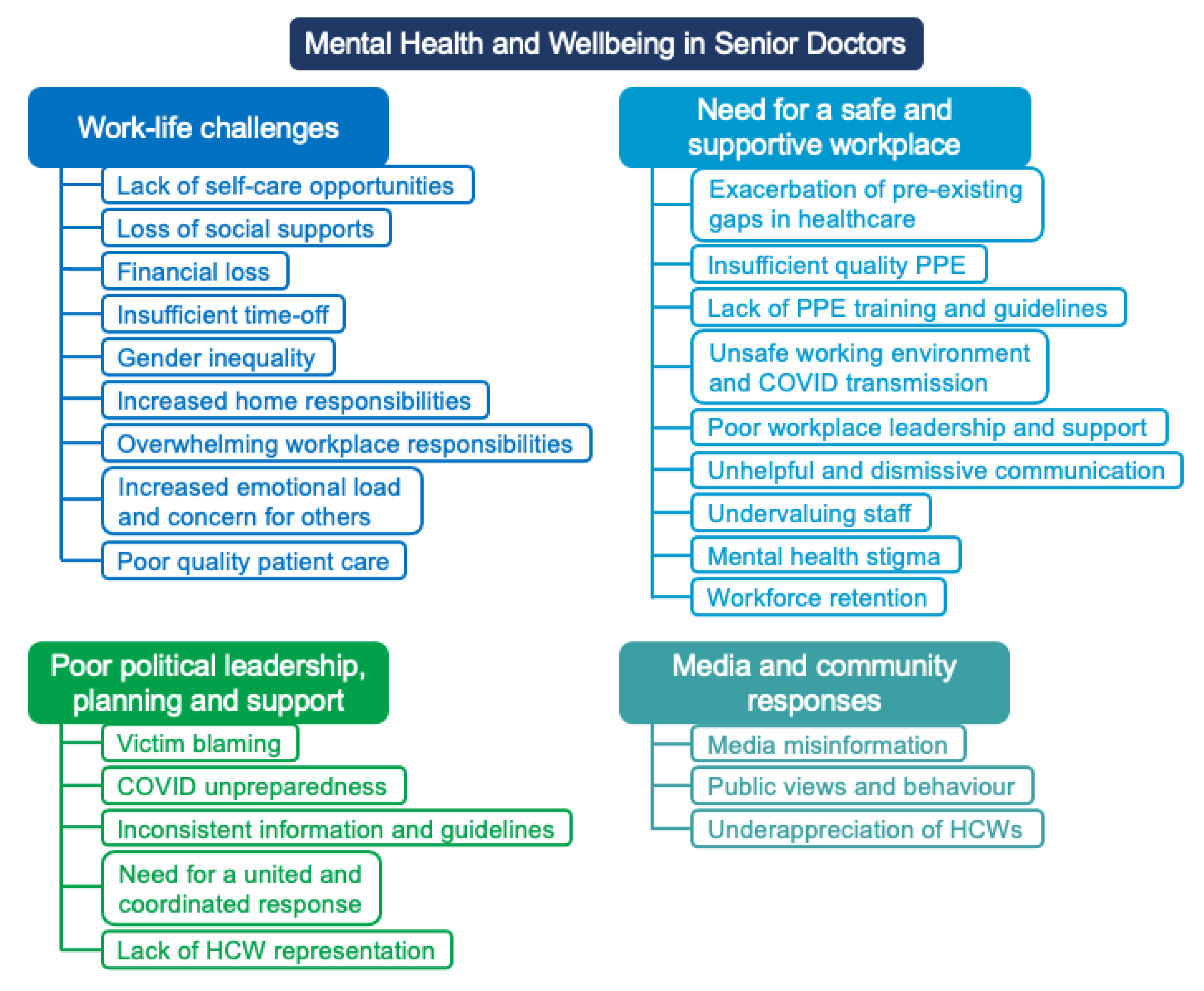
3.2. Overview of Findings
3.3. Theme 1: Work-Life Challenges
3.4. Theme 2: Poor Workplace Safety, Support, and Culture
3.5. Theme 3: Poor Political Leadership, Planning, and Support
3.6. Theme 4: Media and Community Responses
4. Discussion
4.1. Implications and Future Research
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Caplan, R.P. Stress, anxiety, and depression in hospital consultants, general practitioners, and senior health service managers. BMJ 1994, 309, 1261–1263. [Google Scholar] [CrossRef] [Green Version]
- Letvak, S.; Ruhm, C.J.; McCoy, T. Depression in hospital-employed nurses. Clin. Nurse Spec. 2012, 26, 177–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imo, U.O. Burnout and psychiatric morbidity among doctors in the UK: A systematic literature review of prevalence and associated factors. BJPsych Bull. 2017, 41, 197–204. [Google Scholar] [CrossRef] [PubMed]
- De Cieri, H.; Shea, T.; Cooper, B.; Oldenburg, B. Effects of work-related stressors and mindfulness on mental and physical health among Australian nurses and healthcare workers. J. Nurs. Scholarsh. 2019, 51, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Su, J.A.; Weng, H.H.; Tsang, H.Y.; Wu, J.L. Mental health and quality of life among doctors, nurses and other hospital staff. Stress Health J. Int. Soc. Investig. Stress 2009, 25, 423–430. [Google Scholar] [CrossRef]
- Koinis, A.; Giannou, V.; Drantaki, V.; Angelaina, S.; Stratou, E.; Saridi, M. The impact of healthcare workers job environment on their mental-emotional health. Coping strategies: The case of a local general hospital. Health Psychol. Res. 2015, 3, 1984. [Google Scholar] [CrossRef] [Green Version]
- Kumar, S. Burnout and doctors: Prevalence, prevention and intervention. Healthcare 2016, 4, 37. [Google Scholar] [CrossRef] [Green Version]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef] [Green Version]
- McCain, R.S.; McKinley, N.; Dempster, M.; Campbell, W.J.; Kirk, S.J. A study of the relationship between resilience, burnout and coping strategies in doctors. Postgrad. Med. J. 2018, 94, 43–47. [Google Scholar] [CrossRef]
- Wu, F.; Ireland, M.; Hafekost, K.; Lawrence, D. National Mental Health Survey of Doctors and Medical Students; Beyond Blue: Melbourne, Australia, 2013. [Google Scholar]
- Karan, A.; Wadhera, R.K. Healthcare system stress due to COVID-19: Evading an evolving crisis. J. Hosp. Med. 2021, 16, 127. [Google Scholar] [CrossRef]
- Tsamakis, K.; Triantafyllis, A.S.; Tsiptsios, D.; Spartalis, E.; Mueller, C.; Tsamakis, C.; Chaidou, S.; Spandidos, D.A.; Fotis, L.; Economou, M. COVID-19 related stress exacerbates common physical and mental pathologies and affects treatment. Exp. Ther. Med. 2020, 20, 159–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smallwood, N.; Pascoe, A.; Karimi, L.; Bismark, M.; Willis, K. Occupational Disruptions during the COVID-19 Pandemic and Their Association with Healthcare Workers’ Mental Health. Int. J. Environ. Res. Public Health 2021, 18, 9263. [Google Scholar] [CrossRef] [PubMed]
- Ananda-Rajah, M.; Veness, B.; Berkovic, D.; Parker, C.; Kelly, G.; Ayton, D. Hearing the voices of Australian healthcare workers during the COVID-19 pandemic. BMJ Lead. 2021, 5, 31–35. [Google Scholar] [CrossRef]
- Adams, J.G.; Walls, R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA 2020, 323, 1439–1440. [Google Scholar] [CrossRef] [Green Version]
- Digby, R.; Winton-Brown, T.; Finlayson, F.; Dobson, H.; Bucknall, T. Hospital staff well-being during the first wave of COVID-19: Staff perspectives. Int. J. Ment. Health Nurs. 2021, 30, 440–450. [Google Scholar] [CrossRef]
- Ahmad, F. Canadian clinicians adopting virtual health care during COVID-19 pandemic: Salute to our fast learners. J. Concurr. Disord. 2021, 3, 4–7. [Google Scholar]
- Smallwood, N.; Willis, K. Mental health among healthcare workers during the COVID-19 pandemic. Respirology 2021, 26, 1016. [Google Scholar] [CrossRef]
- Kaye, A.D.; Okeagu, C.N.; Pham, A.D.; Silva, R.A.; Hurley, J.J.; Arron, B.L.; Sarfraz, N.; Lee, H.N.; Ghali, G.E.; Gamble, J.W. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best. Pract. Res. Clin. Anaesthesiol. 2021, 35, 293–306. [Google Scholar] [CrossRef]
- Smallwood, N.; Karimi, L.; Bismark, M.; Putland, M.; Johnson, D.; Dharmage, S.C.; Barson, E.; Atkin, N.; Long, C.; Ng, I. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: A cross-sectional survey. Gen. Psychiatr. 2021, 34, e100577. [Google Scholar] [CrossRef]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatr. 2020, 51, 102119. [Google Scholar] [CrossRef]
- Vizheh, M.; Qorbani, M.; Arzaghi, S.M.; Muhidin, S.; Javanmard, Z.; Esmaeili, M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J. Diabetes Metab. Disord. 2020, 19, 1967–1978. [Google Scholar] [CrossRef]
- Smallwood, N.; Pascoe, A.; Karimi, L.; Willis, K. Moral distress and perceived community views are associated with mental health symptoms in frontline health workers during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 8723. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain. Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgan, D.L. Qualitative content analysis: A guide to paths not taken. Qual. Health Res. 1993, 3, 112–121. [Google Scholar] [CrossRef]
- Hsieh, H.-F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef]
- Doherty, A.M.; Colleran, G.C.; Durcan, L.; Irvine, A.D.; Barrett, E. A pilot study of burnout and long covid in senior specialist doctors. Ir. J. Med. Sci. 2021, 191, 133–137. [Google Scholar] [CrossRef]
- Shah, N.; Raheem, A.; Sideris, M.; Velauthar, L.; Saeed, F. Mental health amongst obstetrics and gynaecology doctors during the COVID-19 pandemic: Results of a UK-wide study. Eur. J. Obstet. Gynecol. 2020, 253, 90–94. [Google Scholar] [CrossRef]
- Leigh, J.P.; Kemp, L.G.; de Grood, C.; Brundin-Mather, R.; Stelfox, H.T.; Ng-Kamstra, J.S.; Fiest, K.M. A qualitative study of physician perceptions and experiences of caring for critically ill patients in the context of resource strain during the first wave of the COVID-19 pandemic. BMC Health Serv. Res. 2021, 21, 374. [Google Scholar]
- Aughterson, H.; McKinlay, A.R.; Fancourt, D.; Burton, A. Psychosocial impact on frontline health and social care professionals in the UK during the COVID-19 pandemic: A qualitative interview study. BMJ Open 2021, 11, e047353. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.R.; Tran, T.D.; Hammarberg, K.; Sastry, J.; Nguyen, H.; Rowe, H.; Popplestone, S.; Stocker, R.; Stubber, C.; Kirkman, M. Mental health of people in Australia in the first month of COVID-19 restrictions: A national survey. Med. J. Aust. 2020, 213, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Urooj, U.; Ansari, A.; Siraj, A.; Khan, S.; Tariq, H. Expectations, fears and perceptions of doctors during COVID-19 pandemic. Pak. J. Med. Sci. 2020, 36, S37. [Google Scholar] [CrossRef] [PubMed]
- Litz, B.T.; Stein, N.; Delaney, E.; Lebowitz, L.; Nash, W.P.; Silva, C.; Maguen, S. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clin. Psychol. Rev. 2009, 29, 695–706. [Google Scholar] [CrossRef]
- Litam, S.D.A.; Balkin, R.S. Moral injury in health-care workers during COVID-19 pandemic. Traumatology 2021, 27, 14. [Google Scholar] [CrossRef]
- Hines, S.E.; Chin, K.H.; Glick, D.R.; Wickwire, E.M. Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 488. [Google Scholar] [CrossRef]
- Liberati, E.; Richards, N.; Willars, J.; Scott, D.; Boydell, N.; Parker, J.; Pinfold, V.; Martin, G.; Dixon-Woods, M.; Jones, P.B. A qualitative study of experiences of NHS mental healthcare workers during the COVID-19 pandemic. BMC Psychiatry 2021, 21, 250. [Google Scholar] [CrossRef]
- Williamson, V.; Stevelink, S.A.; Greenberg, N. Occupational moral injury and mental health: Systematic review and meta-analysis. Br. J. Psychiatry 2018, 212, 339–346. [Google Scholar] [CrossRef] [Green Version]
- Vanhaecht, K.; Seys, D.; Bruyneel, L.; Cox, B.; Kaesemans, G.; Cloet, M.; Van Den Broeck, K.; Cools, O.; De Witte, A.; Lowet, K. COVID-19 is having a destructive impact on health-care workers’ mental well-being. Int. J. Qual. Health Care 2021, 33, mzaa158. [Google Scholar] [CrossRef]
- Ahmed, J.; Malik, F.; Arif, T.B.; Majid, Z.; Chaudhary, M.A.; Ahmad, J.; Malik, M.; Khan, T.M.; Khalid, M. Availability of personal protective equipment (PPE) among US and Pakistani doctors in COVID-19 pandemic. Cureus 2020, 12, e8550. [Google Scholar]
- Vindrola-Padros, C.; Andrews, L.; Dowrick, A.; Djellouli, N.; Fillmore, H.; Gonzalez, E.B.; Javadi, D.; Lewis-Jackson, S.; Manby, L.; Mitchinson, L. Perceptions and experiences of healthcare workers during the COVID-19 pandemic in the UK. BMJ Open 2020, 10, e040503. [Google Scholar] [CrossRef] [PubMed]
- Best, J. Undermined and undervalued: How the pandemic exacerbated moral injury and burnout in the NHS. BMJ 2021, 374, n1858. [Google Scholar] [CrossRef] [PubMed]
- RANZCP. PPE Remains a Focus for All Healthcare Professionals; RANZCP: Melbourne, Australia, 2020. [Google Scholar]
- WHPA. World Health Professionals Call on Governments to Prioritise Support for Healthcare Workers in the Frontline against Coronavirus; WHPA: Geneva, Switzerland, 2020. [Google Scholar]
- Kay, M.; Mitchell, G.; Clavarino, A.; Doust, J. Doctors as patients: A systematic review of doctors’ health access and the barriers they experience. Br. J. Gen. Pract. 2008, 58, 501–508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayes, B.; Prihodova, L.; Walsh, G.; Doyle, F.; Doherty, S. What’s up doc? A national cross-sectional study of psychological wellbeing of hospital doctors in Ireland. BMJ Open 2017, 7, e018023. [Google Scholar] [CrossRef] [Green Version]
- Forbes, M.P.; Iyengar, S.; Kay, M. Barriers to the psychological well-being of Australian junior doctors: A qualitative analysis. BMJ Open 2019, 9, e027558. [Google Scholar] [CrossRef] [Green Version]
- Garelick, A.I. Doctors’ health: Stigma and the professional discomfort in seeking help. Psychiatrist 2012, 36, 81–84. [Google Scholar] [CrossRef] [Green Version]
- Bismark, M.M.; Spittal, M.J.; Plueckhahn, T.M.; Studdert, D.M. Mandatory reports of concerns about the health, performance and conduct of health practitioners. Med. J. Aust. 2014, 201, 399–403. [Google Scholar] [CrossRef]
- AMA. Position Statement: Health and Wellbeing of Doctors and Medical Students; AMA: Barton, Australia, 2020. [Google Scholar]
- Bianchi, E.F.; Bhattacharyya, M.R.; Meakin, R. Exploring senior doctors’ beliefs and attitudes regarding mental illness within the medical profession: A qualitative study. BMJ Open 2016, 6, e012598. [Google Scholar] [CrossRef] [Green Version]
- Halley, M.C.; Mathews, K.S.; Diamond, L.C.; Linos, E.; Sarkar, U.; Mangurian, C.; Sabry, H.; Goyal, M.K.; Olazo, K.; Miller, E.G.; et al. The intersection of work and home challenges faced by physician mothers during the coronavirus disease 2019 pandemic: A mixed-methods analysis. J. Women’s Health 2021, 30, 514–524. [Google Scholar] [CrossRef]
- Coronavirus (COVID-19) at a Glance—23 October 2020. Available online: https://www.health.gov.au/resources/publications/coronavirus-covid-19-at-a-glance-23-october-2020 (accessed on 29 September 2021).
- Mahase, E. COVID-19: UK study aims to understand effects on ethnic minority healthcare workers. BMJ 2021, 372, n23. [Google Scholar] [CrossRef]
- Dobson, H.; Malpas, C.B.; Burrell, A.J.; Gurvich, C.; Chen, L.; Kulkarni, J.; Winton-Brown, T. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas. Psychiatry 2021, 29, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Holton, S.; Wynter, K.; Trueman, M.; Bruce, S.; Sweeney, S.; Crowe, S.; Dabscheck, A.; Eleftheriou, P.; Booth, S.; Hitch, D. Psychological well-being of Australian hospital clinical staff during the COVID-19 pandemic. Aust. Health Rev. 2020, 45, 297–305. [Google Scholar] [CrossRef] [PubMed]
| Free-Text Questions | Number of Senior Doctor Responses |
|---|---|
| 869 |
| 1032 |
| 852 |
| 373 |
| Characteristic | Frequency | Percent (%) |
|---|---|---|
| Age (years) | ||
| 20–30 | 4 | 0.3 |
| 31–40 | 349 | 27.3 |
| 41–50 | 497 | 38.9 |
| 50–64 | 383 | 30.0 |
| 65–70 | 34 | 2.7 |
| 71+ | 11 | 0.9 |
| Gender | ||
| Female | 752 | 58.8 |
| Male | 517 | 40.5 |
| Non-Binary | 5 | 0.4 |
| Prefer not to say | 4 | 0.3 |
| State | ||
| Victoria | 973 | 76.1 |
| New South Wales | 126 | 9.6 |
| Queensland | 58 | 4.5 |
| Western Australia | 44 | 3.4 |
| South Australia | 40 | 3.1 |
| Tasmania | 14 | 1.1 |
| Norther Territory | 13 | 1.0 |
| Australian Capital Territory | 10 | 0.8 |
| Work Location | ||
| Metropolitan Area | 1118 | 87.5 |
| Regional Area | 150 | 11.7 |
| Remote Area | 10 | 0.8 |
| Frontline Area | ||
| Medical Specialty 1 | 301 | 23.6 |
| Anaesthetics/Perioperative Care | 197 | 15.4 |
| Emergency Department | 182 | 14.2 |
| General Medicine | 103 | 8.1 |
| Respiratory Medicine | 100 | 7.8 |
| Intensive Care Unit | 98 | 7.7 |
| Surgical Specialty | 73 | 5.7 |
| Aged Care 2 | 64 | 5.0 |
| Infectious Diseases | 58 | 4.5 |
| Palliative Care | 49 | 3.8 |
| Other 3 | 53 | 4.1 |
| Sub-Theme | Quotes |
|---|---|
| Lack of self-care opportunities | “[For mental health I need] time to exercise, meditate, cook etc. rather than being busier by working full time while homeschooling also”. (Female, Age 41–50, Medical Specialty, Q1) “[For mental health I need] better sleep, more exercise, eating better. Developing new interests. Limited by inertia and lack of energy—burnout/anxiety”. (Female, Age 41–50, Aged Care, Q1) |
| Loss of social supports | “Human contact is important and impossible. I haven’t touched a person in over two months without a latex glove, living alone and single, not being able to see friends. That is hard, particularly after a long day in COVID-affected nursing homes with multiple deaths and traumatic scenes”. (Male, Age 31–40, Aged Care, Q1) |
| Financial loss | “Initially the biggest stress was the lack of telehealth item numbers which dropped income to ⅓ of usual values, despite hours tripling”. (Female, Age 50–64, Other Medical Specialty Area, Q1) “Financially, this has been a strain with my private practice income dropping by 60–70%. I am unsure when that is going to return to normal which is quite stressful as we have financial commitments and I do not want to lay off any of my staff”. (Male, Age 41–50, Respiratory Medicine, Q1) |
| Insufficient time-off | “The cumulative stress is more than I think people/systems realise, and that is why I am seeing so many staff leaving or having to take extended leave because they have hit the wall at the 6–9 month mark. This is a marathon—not a sprint, and most of us are not elite athletes with the psychology that goes with it…Maybe in times like these, all frontline workers should be given extra leave, so they are not afraid to use their leave when they need it, rather than “saving it up” for afterwards”. (Female, Age 41–50, Palliative Care, Q3) |
| Gender inequality | “There is a pervading attitude that a) women will deal with all the child rearing aspects and b) this means they are now fairly useless from an employment perspective, and this will hurt their careers in ways that they cannot recover from. This will end up true as a self-fulfilling prophecy without better recognition of the impact of COVID-19 on health workers who are mothers and policy and financial steps taken to change this- otherwise we will see worsening of the current economic and senior leadership inequality between women and men”. (Female, Age 41–50, Medical Specialty, Q4) |
| Increased home responsibilities | “Having a caring role for my young (pre-school) children and also my elderly mother is even more challenging during the pandemic, and I feel that my (older, male) colleagues have little understanding of how challenging this is. The pandemic has amplified sexism in the workplace”. (Female, Age 31–40, Intensive Care Unit, Q4) “The Victorian government have made it difficult to send children to school and childcare. Schools and childcare have then passed this difficulty onto parents…I have been asked to complete homeschooling exercises despite my child being at school. I have been asked to be keeping track of the online learning timetable in order to remind the school supervisors of my child’s classes. I have also been asked to send in a signed form every week indicating my child is attending in the next week. The requirements of school and childcare have been unnecessarily onerous for a frontline health worker”. (Female, Age 41–50, Medical Specialty, Q1) |
| Overwhelming workplace responsibilities | “[Main challenge was] increased workload both clinical and non-clinical. Overtime +++. High rates of sick leave of medical staff with no availability of extra staff. Working with limited staffing on every shift creating fatigue and burnout”. (Female, Age 41–50, Emergency Department, Q2) “[Main challenge was] maintaining momentum and energy to deal with constant changes (e.g., DHHS guidelines, sudden changes in testing requirements overnight) and keeping up with clinical knowledge and data”. (Female, Age 41–50, Infectious Diseases, Q2) |
| Increased emotional load and concern for others | “There’s never been a more challenging time in my experience as a paediatrician. Managing patients, checking in on my staff’s mental health, managing my family with my husband unemployed and one son still in senior school. I feel I’m not looking out for me as there’s nothing left in the tank!” (Female, Age 50–64, Medical Specialty, Q4) “[Main challenge was] holding the fear and anger of all my staff. Managing my own fears for their safety. Fears that we would be unable to provide basic care to people. Fear of finishing it all with PTSD”. (Male, Age 41–50, Emergency Department, Q2) “I am a co-director of training in Victoria and I really worry about the impact of COVID on trainees/registrars. Our registrars are working in our ‘resp zone’ with support/supervision available as needed—but not with constant support…We keep hearing comments from them [the junior doctors]: ‘I’m the lamb to the slaughter tonight am I’ and ‘if a trainee died from COVID would anyone even care?’—which is extremely worrying…” (Female, Age 31–40, Emergency Department, Q4) “I have more concern for junior medical staff. They have borne the brunt of the difficult clinical work, long hours, and roster changes. And they are still expected to study and progress in their career despite enormous uncertainty”. (Female, Age 41–50, Medical Specialty, Q4) |
| Quality of patient care | “The main challenge though was the psychological impact of having so many sick patients simultaneously and trying to communicate remotely with families so that they understood what was happening with their relatives. Rationing of treatment because of a lack of ventilators and ECMO meant that clinicians were forced to make very difficult moral decisions. I have never witnessed so many people dying in such a short space of time and they all died alone”. (Male, Age 31–40, Respiratory Medicine, Q2) “One of the clinics I work at has decided to be completely hidden from patients and do telehealth 100% of the time. My main challenge is to try to justify to my paediatric patients (and my conscience) why providing inferior medical care to children is meant to be in their best interest (given that these medical conditions will affect them more than the COVID)”. (Female, Age 41–50, Medical Specialty, Q2) |
| Sub-Theme | Quotes |
|---|---|
| Exacerbation of pre-existing gaps in healthcare | “I think the pandemic has merely exposed the pre-existing issues we were struggling with. Colleagues who are highly supportive were even more so, those who are often draining or difficult in teams deteriorated. Shortages of staff and resources including PPE worsened. Lack of leave worsened. The drain on limited services to provide education to junior staff and students worsened due to increased clinical load. The only resource we had we could increase was personal sacrifice of our own wellbeing and the systems don’t seem to have acknowledged the pre-existing nature of these issues”. (Female, Age 41–50, Palliative Care, Q4) |
| Insufficient quality PPE | “[Main challenge was] lack of appropriately fitted PPE—not enough N95 masks and no fit testing which should be mandated. I have no confidence that the N95 masks fit me properly. I don’t think my organisation was totally honest regarding PPE…We were told no surgical masks if looking after “low risk patients” on coronary care and surgical mask only for looking after COVID patients who were not coughing and not having an aerosolizing procedure. I gather these guidelines have now been changed due to the high numbers of health care worker infections—this was obvious from the beginning and has made it hard to trust hospital administration. There has been no attempt to get us proper fit testing—this means we are working in an unsafe workplace”. (Female, Age 50–64, Medical Specialty, Q2) |
| Lack of PPE training and guidelines | “I also don’t appreciate the lag in recommending N95 for all workers looking after suspected and confirmed COVID cases. I have had some PPE training but no fit testing. And the training I had was for a duck billed N95 at the start of the pandemic. Now I’m being given rigid 3M masks with no training other than being sent a link to an instructional video. All of this needs to be better!” (Female, Age 41–50, General Medicine, Q3) |
| Unsafe working environment and COVID transmission | “The hospital is very poorly set up for cross contamination prevention especially opening of doors, cleaning of common areas, hot desking. Inability to work from home due to abysmal IT and lack of digital pathology. Staff do not practice social distancing during meal and coffee breaks”. (Male, Age 50–64, Other, Q2) |
| Poor workplace leadership and support | “Executive staff are invisible as mostly working from home. They only look at the numbers, not the complexities of patients”. (Female, Age 50–64, Emergency Department, Q2) “I work in private practice and a public hospital. The hospital asked where I’d work but never how they’d help if I got sick. Feel unsupported and excluded as a contractor. My organisation does not even pay for meetings between departments”. (Female, Age 41–50, Medical Specialty, Q2) “My GP gave me permission to take time off from work after I had recovered from COVID. I did not understand the emotional toll that having COVID would take on me even though I was not unwell. I was very angry and traumatized when I returned to work. A return-to-work plan and emotional support via my public health employer would have been good. Recognition that I did contract the illness at work instead of pretending it didn’t happen. Acknowledgement, support and an apology for not instituting safe COVID practices is what I hoped for and never came”. (Female, Age 41–50, Surgical Speciality, Q1) |
| Unhelpful and dismissive communication | “Managers don’t take doctors’ risks seriously. Too busy managing up to the people above them. They were slow in putting in new policies, ignored doctors’ concerns, minimised the support for those who could work from home, didn’t get fit testing, discouraged the use of PPE in the first wave, stopped people bringing in their own PPE- as it would raise concerns/anxiety in others. So, what would help—serious focus on listening and enacting changes in relation to doctors’ concerns, management accountability in real time, honesty that they don’t have all the answers or protective equipment available if this is the case. Not expecting and demanding business as usual in terms of efficiency and numbers. A caring culture that is inclusive”. (Female, Age 50–64, Medical Specialty, Q1) |
| Undervaluing staff | “[Main challenge was] the lack of care and support the hospital actually showed to the doctors and nurses working on the COVID ward. I was bullied and so were many of the staff on the COVID ward into wearing inappropriate PPE. They only changed practice because the hospital had an outbreak and it made it into the media. They showed little concern when the pandemic started for workers and cared little… Having executives and nurses who had climbed the ladder but are not well educated in getting the latest data was a huge failing and one that impacted on every worker’s mental health in our hospital”. (Male, Age 41–50, General Medicine, Q2) “Support and commiseration from colleagues, knowing we are all equally undervalued and disposable in our health system”. (Female, Age 31–40, Medical Specialty, Q4) |
| Mental health stigma | “The stigma and negative consequences of reaching out for help should be abolished so we do not have to suffer alone and suffer without formal help and support”. (Female, Age 41–50, Community Clinic, Q4) “[Strategies to help] on an individual level—early access to support. Along with this, a more concerted effort from health services to encourage their use and disarm the notion (whether real or not) that accessing mental health services may lead to consequences for future employment”. (Male, Age 41–50, Anaesthetics/Perioperative Care, Q3) |
| Workforce retention | “I am concerned if we don’t have a lot of ongoing genuine professional psychological support, we are going to see a lot of burnout and HCWs leaving the profession”. (Female, Age 41–50, Intensive Care Unit, Q4) |
| Sub-Theme | Quotes |
|---|---|
| Victim blaming | “[We need] the government to stop making off the cuff stupid remarks that throw HCWs under the bus for a positive diagnosis...More thoughtful and considered public statements by CHO [chief health officer], Health Ministers, Premiers, PM [prime minister] etc that have some nuance and don’t blame HCWs immediately for everything will go a long way to minimize stigma and collateral damage of COVID panic in this country”. (Male, Age 41–50, Radiology, Q1) “They [doctors] should not be blamed if they get infected, media is so nasty in this country. They [media] put their camera in front of the hospital for a few days and every one of us going to the hospital felt like criminals because a poor doctor was found positive”. (Male, Age 41–50, Respiratory Medicine, Q3) |
| COVID unpreparedness | “[Main challenges were] a useless CEO [chief executive officer] of our public hospital, a useless department of health in Victoria which is totally dysfunctional, a useless disorganised supply of inadequate PPE, a very delayed response to increasing numbers of community transmission of COVID. Working in a hospital in which 750 staff are furloughed. Dysfunctional work environment at a global hospital level”. (Female, Age 41–50, Anaesthetics/Perioperative Care, Q2) “[We need] a predetermined disaster management plan that is actually communicated and implemented in a timely manner, rather than the reliance on a grass roots movement in local groups to plan and manage both patient and HCW safety. The absolute avoidance of politicisation of a disaster response, and a well communicated public education program to assist in preparation and management”. (Female, Age 31–40, Anaesthetics/Perioperative Care, Q3) |
| Inconsistent information and guidelines | “[Main challenge was] the inconsistent, and at times, lacking communication around healthcare organisation policies; often-lagging DHHS (Vic) guidelines for PPE use (for health care workers) and aged care response to outbreaks; the mixed public health messages; frustration with inconsistent public response to pandemic management strategies; lack of accountability of politicians (in Victoria) for pandemic management failures”. (Male, Age 41–50, Hospital Aged Care, Q2) |
| Need for a united and coordinated response | “[We need] a centralized Department of Health in Victoria—one set of guidelines that everyone has to follow and prioritize staff safety and/or WorkSafe involvement in healthcare. Nimble response and willingness to adapt when healthcare workers are at risk. Priorities that allow training and staff development during usual times not just when in crisis, so we are ready”. (Female, Age 41–50, Anaesthetics/Perioperative Care, Q3) |
| Lack of HCW representation | “[We need] improved lines of communication from the top down. Have frontline HCW appropriately represented in working groups making key decisions that affect us” (Female, Age 41–50, Emergency Department, Q3) |
| Sub-Theme | Quotes |
|---|---|
| Media misinformation | “[We need] sensible government and media reporting and less scaremongering and psychological barrage to get people to do what they want”. (Male, Age 31–40, Anaesthetics/Perioperative Care, Q1) |
| Public views and behaviour | “I wish I could change the behaviour of people who obviously do not care about the effects of their action by not following public health directives, or who are actively protesting against the need to socially distance, wear masks and avoid crowds”. (Female, Age 41–50, Emergency Department, Q4) |
| Underappreciation of HCWs | “I feel that many of my colleagues’ efforts are under appreciated by the general community. They are putting their health at risk while some sectors of the community are debating the need for masks and isolation. It is the health care workers who pay the highest cost when the community fails to control the virus”. (Male, Age 50–64, Radiology, Q4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, J.; Willis, K.; Kay, M.; Hutt, K.; Smallwood, N. The Workplace and Psychosocial Experiences of Australian Senior Doctors during the COVID-19 Pandemic: A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 3079. https://doi.org/10.3390/ijerph19053079
Tran J, Willis K, Kay M, Hutt K, Smallwood N. The Workplace and Psychosocial Experiences of Australian Senior Doctors during the COVID-19 Pandemic: A Qualitative Study. International Journal of Environmental Research and Public Health. 2022; 19(5):3079. https://doi.org/10.3390/ijerph19053079
Chicago/Turabian StyleTran, Jonathan, Karen Willis, Margaret Kay, Kathryn Hutt, and Natasha Smallwood. 2022. "The Workplace and Psychosocial Experiences of Australian Senior Doctors during the COVID-19 Pandemic: A Qualitative Study" International Journal of Environmental Research and Public Health 19, no. 5: 3079. https://doi.org/10.3390/ijerph19053079
APA StyleTran, J., Willis, K., Kay, M., Hutt, K., & Smallwood, N. (2022). The Workplace and Psychosocial Experiences of Australian Senior Doctors during the COVID-19 Pandemic: A Qualitative Study. International Journal of Environmental Research and Public Health, 19(5), 3079. https://doi.org/10.3390/ijerph19053079







