Continuity of Nursing Care in Patients with Coronary Artery Disease: A Systematic Review
Abstract
1. Introduction
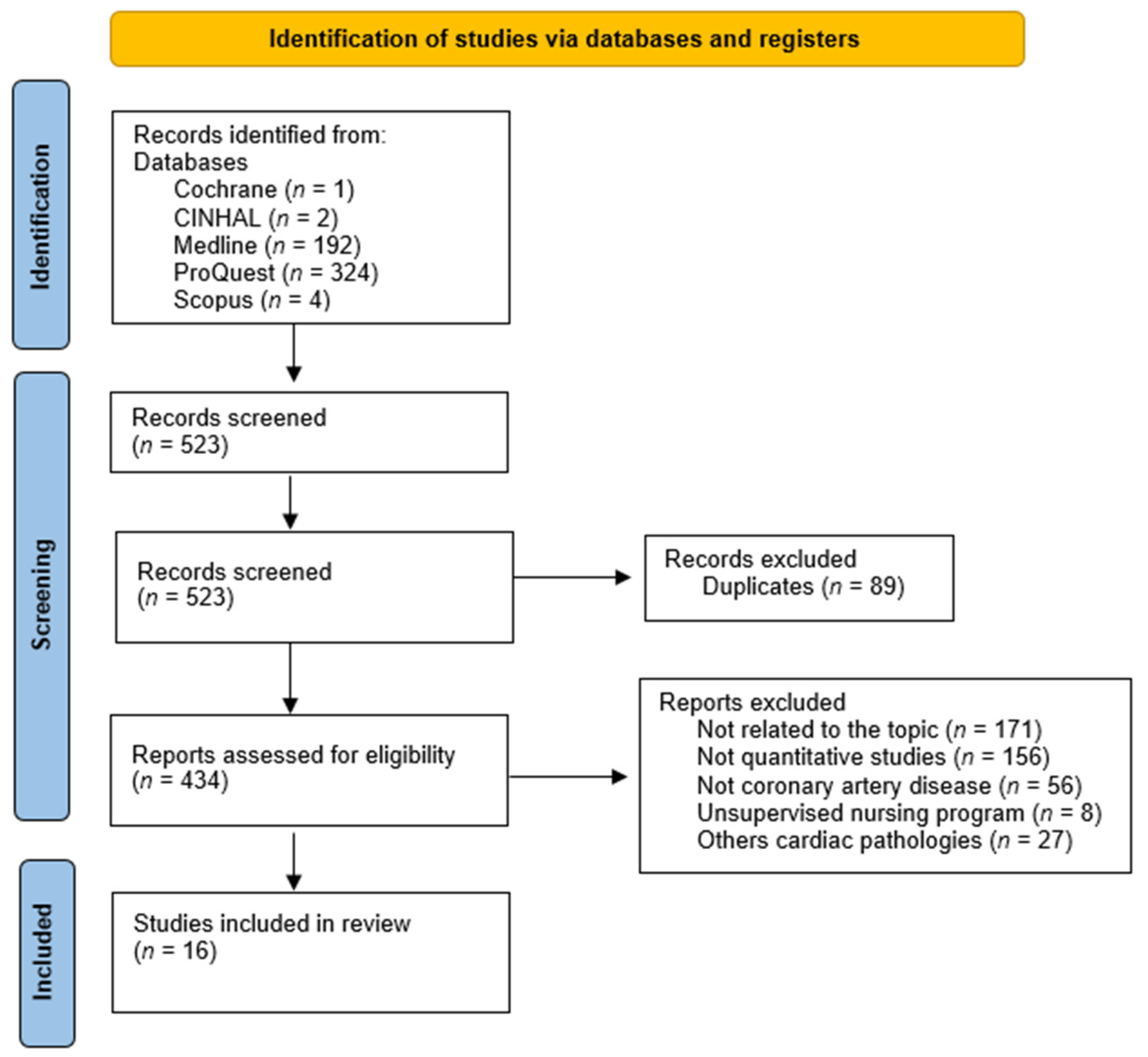
2. Methods
2.1. Design and Search Methods
2.2. Selection Criteria
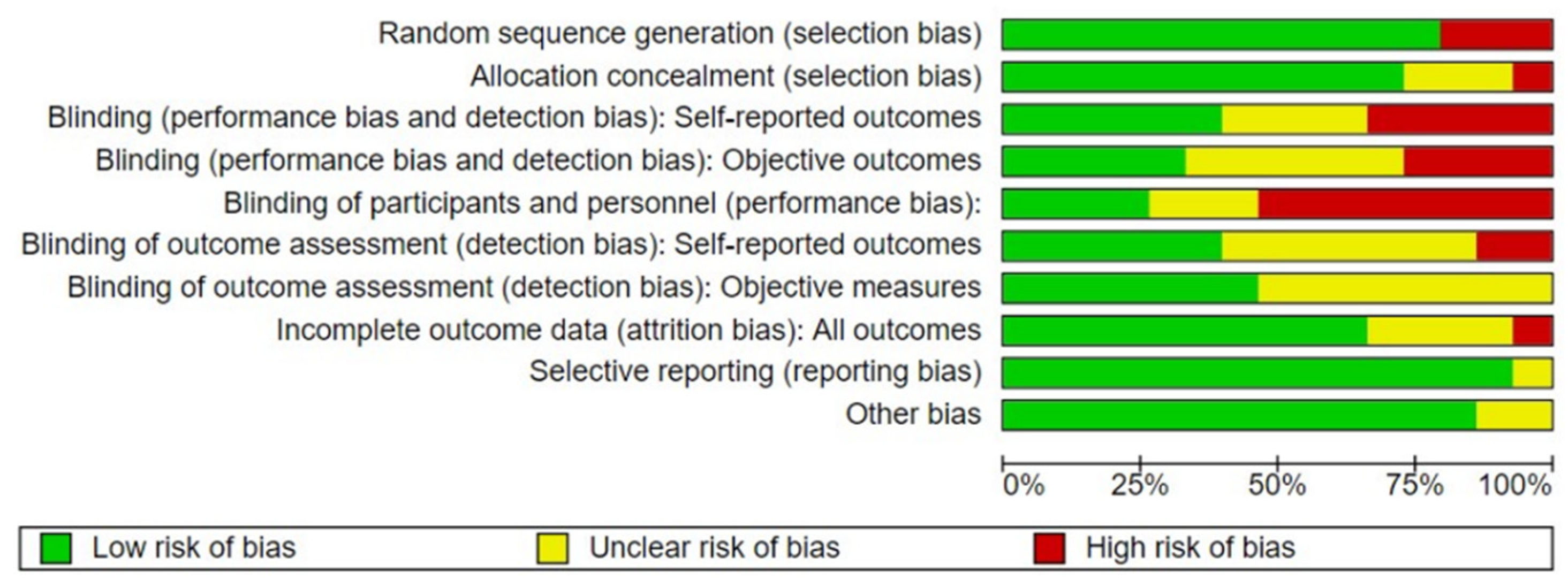
2.3. Quality Appraisal and Risk of Bias
2.4. Data Abstraction and Synthesis
3. Results
3.1. Study Characteristics
3.2. Risk of Bias Assessment
3.3. Effects on Self-Care Capacity, Disease Knowledge, and Self-Efficacy
3.4. Effects on Change of Habits and Prevention of Risk Factors
3.5. Effects on Mental Health and Social Relationships
3.6. Effects on Clinical Parameters
3.7. Effects on Hospital Readmission
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organization Cardiovascular Diseases (CVDs). Available online: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 20 December 2021).
- Reed, G.W.; Rossi, J.E.; Cannon, C.P. Acute myocardial infarction. Lancet 2017, 389, 197–210. [Google Scholar] [CrossRef]
- Bajaj, A.; Sethi, A.; Rathor, P.; Suppogu, N.; Sethi, A. Acute complications of myocardial infarction in the current era: Diagnosis and management. J. Investig. Med. 2015, 63, 844–855. [Google Scholar] [CrossRef] [PubMed]
- Valaker, I.; Norekvål, T.M.; Råholm, M.B.; Nordrehaug, J.E.; Rotevatn, S.; Fridlund, B. Continuity of care after percutaneous coronary intervention: The patient’s perspective across secondary and primary care settings. Eur. J. Cardiovasc. Nurs. 2017, 16, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Riovalle, J.; Ejheisheh, M.A.; Membrive-Jiménez, M.J.; Suleiman-Martos, N.; Albendín-García, L.; Correa-Rodríguez, M.; Gómez-Urquiza, J.L. Quality of life after coronary artery bypass surgery: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 8439. [Google Scholar] [CrossRef]
- Correa-Rodríguez, M.; Abu Ejheisheh, M.; Suleiman-Martos, N.; Membrive-Jiménez, M.J.; Velando-Soriano, A.; Schmidt-RioValle, J.; Gómez-Urquiza, J.L. Prevalence of depression in coronary artery bypass surgery: A systematic review and meta-analysis. J. Clin. Med. 2020, 9, 909. [Google Scholar] [CrossRef]
- Muhammad, I.; He, H.-G.; Kowitlawakul, Y.; Wang, W. Narrative review of health-related quality of life and its predictors among patients with coronary heart disease. Int. J. Nurs. Pract. 2016, 22, 4–14. [Google Scholar] [CrossRef]
- Al-Smadi, A.; Ashour, A.; Hweidi, I.; Gharaibeh, B.; Fitzsimons, D. Illness perception in patients with coronary artery disease: A systematic review. Int. J. Nurs. Pract. 2016, 22, 633–648. [Google Scholar] [CrossRef]
- Schiele, F.; Ecarnot, F.; Chopard, R. Coronary artery disease: Risk stratification and patient selection for more aggressive secondary prevention. Eur. J. Prev. Cardiol. 2017, 24, 88–100. [Google Scholar] [CrossRef]
- Fålun, N.; Fridlund, B.; Schaufel, M.A.; Schei, E.; Norekvål, T.M. Patients’ goals, resources, and barriers to future change: A qualitative study of patient reflections at hospital discharge after myocardial infarction. Eur. J. Cardiovasc. Nurs. 2016, 15, 495–503. [Google Scholar] [CrossRef]
- Stoicea, N.; You, T.; Eiterman, A.; Hartwell, C.; Davila, V.; Marjoribanks, S.; Florescu, C.; Bergese, S.D.; Rogers, B. Perspectives of post-acute transition of care for cardiac surgery patients. Front. Cardiovasc. Med. 2017, 4, 70. [Google Scholar] [CrossRef]
- Rushton, M.; Howarth, M.; Grant, M.J.; Astin, F. Person-centred discharge education following coronary artery bypass graft: A critical review. J. Clin. Nurs. 2017, 26, 5206–5215. [Google Scholar] [CrossRef] [PubMed]
- Stevens, S. Preventing 30-day Readmissions. Nurs. Clin. N. Am. 2015, 50, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Bahr, S.J.; Weiss, M.E. Clarifying model for continuity of care: A concept analysis. Int. J. Nurs. Pract. 2019, 25, e12704. [Google Scholar] [CrossRef] [PubMed]
- Alghanem, F.; Clements, J.M. Narrowing performance gap between rural and urban hospitals for acute myocardial infarction care. Am. J. Emerg. Med. 2020, 38, 89–94. [Google Scholar] [CrossRef]
- Colella, T.J.F.; King-Shier, K. The effect of a peer support intervention on early recovery outcomes in men recovering from coronary bypass surgery: A randomized controlled trial. Eur. J. Cardiovasc. Nurs. 2018, 17, 408–417. [Google Scholar] [CrossRef]
- Giuliano, C.; Parmenter, B.J.; Baker, M.K.; Mitchell, B.L.; Williams, A.D.; Lyndon, K.; Mair, T.; Maiorana, A.; Smart, N.A.; Levinger, I. Cardiac rehabilitation for patients with coronary artery disease: A practical guide to enhance patient outcomes through continuity of care. Clin. Med. Insights Cardiol. 2017, 11, 1179546817710028. [Google Scholar] [CrossRef]
- Mansilla-Chacón, M.; Gómez-Urquiza, J.L.; Begoña Martos-Cabrera, M.; Albendín-García, L.; Romero-Béjar, J.L.; Cañadas-De, G.A.; Fuente, L.; Suleiman-Martos, N.; Pedretti, R.F.E.; Jongbloed, M.R.M. Effects of Supervised Cardiac Rehabilitation Programmes on Quality of Life among Myocardial Infarction Patients: A Systematic Review and Meta-Analysis. J. Cardiovasc. Dev. Dis. 2021, 8, 166. [Google Scholar] [CrossRef]
- Jankowski, P.; Czarnecka, D.; Badacz, L.; Bogacki, P.; Dubiel, J.S.; Grodecki, J.; Grodzicki, T.; Maciejewicz, J.; Mirek-Bryniarska, E.; Nessler, J.; et al. Practice setting and secondary prevention of coronary artery disease. Arch. Med. Sci. 2018, 14, 979–987. [Google Scholar] [CrossRef]
- Wu, Q.; Zhang, D.; Zhao, Q.; Liu, L.; He, Z.; Chen, Y.; Huang, H.; Hou, Y.; Yang, X.; Gu, J. Effects of transitional health management on adherence and prognosis in elderly patients with acute myocardial infarction in percutaneous coronary intervention: A cluster randomized controlled trial. PLoS ONE 2019, 14, e0217535. [Google Scholar] [CrossRef]
- Bikmoradi, A.; Masmouei, B.; Ghomeisi, M.; Roshanaei, G.; Masiello, I. Impact of telephone counseling on the quality of life of patients discharged after coronary artery bypass grafts. Patient Educ. Couns. 2017, 100, 2290–2296. [Google Scholar] [CrossRef]
- Uysal, H.; Özcan, Ş. The effect of individual training and counselling programme for patients with myocardial infarction over patients’ quality of life. Int. J. Nurs. Pract. 2012, 18, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Li, Y.; Meng, Q.; Li, Y.; Tian, X.; Liu, R.; Fang, J. Effects of nurse-led transitional care interventions for patients with heart failure on healthcare utilization: A meta-analysis of randomized controlled trials. PLoS ONE 2021, 16, e0261300. [Google Scholar] [CrossRef] [PubMed]
- Karataş, T.; Bostanoğlu, H. Perceived social support and psychosocial adjustment in patients with coronary heart disease. Int. J. Nurs. Pract. 2017, 23, e12558. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Reid, R.; Haggerty, J.; McKendry, R. Defusing the Confusion: Concepts and Measures of Continuity of Healthcare; Centre for Health Services and Policy Research, University of British Columbia: Vancouver, BC, Canada, 2002. [Google Scholar]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalg, T.; Heneghan, C.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H. The Oxford 2011 Levels of Evidence. Available online: https://www.cebm.net/2016/05/ocebm-levels-of-evidence (accessed on 10 January 2022).
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0; The Cochrane Collaboration: London, UK, 2008; Available online: www.cochrane-handbook.org (accessed on 10 January 2022).
- Bikmoradi, A.; Masmouei, B.; Ghomeisi, M.; Roshanaei, G. Impact of Tele-nursing on adherence to treatment plan in discharged patients after coronary artery bypass graft surgery: A quasi-experimental study in Iran. Int. J. Med. Inform. 2016, 86, 43–48. [Google Scholar] [CrossRef]
- Mohammadpour, A.; Rahmati Sharghi, N.; Khosravan, S.; Alami, A.; Akhond, M. The effect of a supportive educational intervention developed based on the Orem’s self-care theory on the self-care ability of patients with myocardial infarction: A randomised controlled trial. J. Clin. Nurs. 2015, 24, 1686–1692. [Google Scholar] [CrossRef]
- Molazem, Z.; Rezaei, S.; Mohebbi, Z.; Ostovan, M.A.; Keshavarzi, S. Effect of continuous care model on lifestyle of patients with myocardial infarction. ARYA Atheroscler. 2013, 9, 186–191. [Google Scholar]
- Negarandeh, R.; Nayeri, N.D.; Shirani, F.; Janani, L. The impact of discharge plan upon re-admission, satisfaction with nursing care and the ability to self-care for coronary artery bypass graft surgery patients. Eur. J. Cardiovasc. Nurs. 2012, 11, 460–465. [Google Scholar] [CrossRef]
- Cossette, S.; Frasure-Smith, N.; Dupuis, J.; Juneau, M.; Guertin, M.C. Randomized controlled trial of tailored nursing interventions to improve cardiac rehabilitation enrollment. Nurs. Res. 2012, 61, 119–128. [Google Scholar] [CrossRef]
- Fredericks, S. Timing for delivering individualized patient education intervention to coronary artery bypass graft patients: An RCT. Eur. J. Cardiovasc. Nurs. 2009, 8, 144–150. [Google Scholar] [CrossRef]
- Lapointe, F.; Lepage, S.; Larrivée, L.; Maheux, P. Surveillance and treatment of dyslipidemia in the post-infarct patient: Can a nurse-led management approach make a difference. Can. J. Cardiol. 2006, 22, 761–767. [Google Scholar] [CrossRef]
- Zhang, P.; Xing, F.M.; Li, C.Z.; Wang, F.L.; Zhang, X.L. Effects of a nurse-led transitional care programme on readmission, self-efficacy to implement health-promoting behaviours, functional status and life quality among Chinese patients with coronary artery disease: A randomised controlled trial. J. Clin. Nurs. 2018, 27, 969–979. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wong, F.K.Y. Effects of a postdischarge transitional care programme for patients with coronary heart disease in China: A randomised controlled trial. J. Clin. Nurs. 2009, 18, 2444–2455. [Google Scholar] [CrossRef] [PubMed]
- Carroll, D.L.; Rankin, S.H. Comparing interventions in older unpartnered adults after myocardial infarction. Eur. J. Cardiovasc. Nurs. 2006, 5, 83–89. [Google Scholar] [CrossRef]
- Buckley, T.; McKinley, S.; Gallagher, R.; Dracup, K.; Moser, D.K.; Aitken, L.M. The effect of education and counselling on knowledge, attitudes and beliefs about responses to acute myocardial infarction symptoms. Eur. J. Cardiovasc. Nurs. 2007, 6, 105–111. [Google Scholar] [CrossRef]
- Irmak, Z.; Fesci, H. Effects of nurse-managed secondary prevention program on lifestyle and risk factors of patients who had experienced myocardial infarction. Appl. Nurs. Res. 2010, 23, 147–152. [Google Scholar] [CrossRef]
- Furuya, R.K.; Arantes, E.C.; Dessotte, C.A.M.; Ciol, M.A.; Hoffman, J.M.; Schmidt, A.; Dantas, R.A.S.; Rossi, L.A. A randomized controlled trial of an educational programme to improve self-care in Brazilian patients following percutaneous coronary intervention. J. Adv. Nurs. 2015, 71, 895–908. [Google Scholar] [CrossRef]
- Hunger, M.; Kirchberger, I.; Holle, R.; Seidl, H.; Kuch, B.; Wende, R.; Meisinger, C. Does nurse-based case management for aged myocardial infarction patients improve risk factors, physical functioning and mental health? The KORINNA trial. Eur. J. Prev. Cardiol. 2015, 22, 442–450. [Google Scholar] [CrossRef]
- Mols, R.E.; Hald, M.; Vistisen, H.S.; Lomborg, K.; Maeng, M. Nurse-led motivational telephone follow-up after same-day percutaneous coronary intervention reduces readmission and contacts to general practice. J. Cardiovasc. Nurs. 2019, 34, 222–230. [Google Scholar] [CrossRef]
- Minneboo, M.; Lachman, S.; Snaterse, M.; Jørstad, H.T.; Ter Riet, G.; Boekholdt, S.M.; Scholte op Reimer, W.J.M.; Peters, R.J.G.; Riezebos, R.K.; van Liebergen, R.A.M.; et al. Community-based lifestyle intervention in patients with coronary artery disease: The RESPONSE-2 Trial. J. Am. Coll. Cardiol. 2017, 70, 318–327. [Google Scholar] [CrossRef]
- Yuroong, A.; Asdornwised, U.; Pinyopasakul, W.; Wongkornrat, W.; Chansatitporn, N. The effectiveness of the transitional care program among people awaiting coronary artery bypass graft surgery: A randomized control trial. J. Nurs. Scholarsh. 2021, 53, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Dobber, J.; Latour, C.; Snaterse, M.; van Meijel, B.; Ter Riet, G.; Scholte Op Reimer, W.; Peters, R. Developing nurses’ skills in motivational interviewing to promote a healthy lifestyle in patients with coronary artery disease. Eur. J. Cardiovasc. Nurs. 2019, 18, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Corrà, U.; Dendale, P.; Frederix, I.; Prescott, E.; Schmid, J.P.; Cupples, M.; Deaton, C.; Doherty, P.; Giannuzzi, P.; et al. Challenges in secondary prevention after acute myocardial infarction: A call for action. Eur. J. Cardiovasc. Nurs. 2017, 16, 369–380. [Google Scholar] [CrossRef]
- Pereira Sousa, J.; Neves, H.; Pais-Vieira, M. Does symptom recognition improve self-care in patients with heart failure? A pilot study randomised controlled trial. Nurs. Rep. 2021, 11, 418–429. [Google Scholar] [CrossRef] [PubMed]
- Nunes, S.; Rego, G.; Nunes, R. Difficulties of portuguese patients following acute myocardial infarction: Predictors of readmissions and unchanged lifestyles. Asian Nurs. Res. 2016, 10, 150–157. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hydzik, P.; Kolarczyk, E.; Kustrzycki, W.; Kubielas, G.; Kałużna-oleksy, M.; Szczepanowski, R.; Uchmanowicz, B. Readiness for Discharge from Hospital after Myocardial Infarction: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 6937. [Google Scholar] [CrossRef]
- Shin, E.S.; Hwang, S.Y.; Jeong, M.H.; Lee, E.S. Relationships of factors affecting self-care compliance in acute coronary syndrome patients following percutaneous coronary intervention. Asian Nurs. Res. 2013, 7, 205–211. [Google Scholar] [CrossRef]
- Lau-Walker, M.; Landy, A.; Murrells, T. Personalised discharge care planning for postmyocardial infarction patients through the use of the personalised patient education protocol—implementing theory into practice. J. Clin. Nurs. 2016, 25, 1292–1300. [Google Scholar] [CrossRef]
- Alkubati, S.A.; Al-Zaru, I.M.; Khater, W.; Ammouri, A.A. Perceived learning needs of Yemeni patients after coronary artery bypass graft surgery. J. Clin. Nurs. 2013, 22, 930–938. [Google Scholar] [CrossRef]
- Wood, D.A.; Kotseva, K.; Connolly, S.; Jennings, C.; Mead, A.; Jones, J.; Holden, A.; De Bacquer, D.; Collier, T.; De Backer, G.; et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: A paired, cluster-randomised controlled trial. Lancet 2008, 371, 1999–2012. [Google Scholar] [CrossRef]
- Yildiz, F.; Kaşikçi, M. Impact of training based on Orem’s Theory on self-care agency and quality of life in patients with coronary artery disease. J. Nurs. Res. 2020, 28, e125. [Google Scholar] [CrossRef] [PubMed]
- Mosleh, S.M.; Eshah, N.F.; Almalik, M.M.A.M. Perceived learning needs according to patients who have undergone major coronary interventions and their nurses. J. Clin. Nurs. 2017, 26, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Jaspers, N.E.M.; Visseren, F.L.J.; Van der Graaf, Y.; Smulders, Y.M.; Damman, O.C.; Brouwers, C.; Rutten, G.E.; Dorresteijn, J.A. Communicating personalised statin therapy-effects as 10-year CVD-risk or CVD-free life-expectancy: Does it improve decisional conflict? Three-armed, blinded, randomised controlled trial. BMJ Open 2021, 11, e041673. [Google Scholar] [CrossRef] [PubMed]
- Stafford, L.; Berk, M. The use of statins after a cardiac intervention is associated with reduced risk of subsequent depression: Proof of concept for the inflammatory and oxidative hypotheses of depression? J. Clin. Psychiatry 2011, 72, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Thompson, P.D.; Clarkson, P.; Karas, R.H. Statin-associated myopathy. J. Am. Med. Assoc. 2003, 289, 1681–1690. [Google Scholar] [CrossRef]
- Haile, S.; Linné, A.; Johansson, U.B.; Joelsson-Alm, E. Follow-up after surgical treatment for intermittent claudication (FASTIC): A study protocol for a multicentre randomised controlled clinical trial. BMC Nurs. 2020, 19, 45. [Google Scholar] [CrossRef]
- Abaraogu, U.O.; Dall, P.M.; Brittenden, J.; Stuart, W.; Tew, G.A.; Godwin, J.; Seenan, C.A. Efficacy and Feasibility of Pain management and Patient Education for Physical Activity in Intermittent claudication (PrEPAID): Protocol for a randomised controlled trial. Trials 2019, 20, 222. [Google Scholar] [CrossRef]
- Xavier, D.; Gupta, R.; Kamath, D.; Sigamani, A.; Devereaux, P.J.; George, N.; Joshi, R.; Pogue, J.; Pais, P.; Yusuf, S. Community health worker-based intervention for adherence to drugs and lifestyle change after acute coronary syndrome: A multicentre, open, randomised controlled trial. Lancet Diabetes Endocrinol. 2016, 4, 244–253. [Google Scholar] [CrossRef]
- Chudgar, N.; Zhu, R.; Gray, K.; Chiu, K.; Carrera, A.; Lang, S.; Avgerinos, D.; Mack, C. Implementing a high value care discharge protocol in patients undergoing CABG reduces readmission. Ann. Thorac. Surg. 2021; in press. [Google Scholar] [CrossRef]
- Al-Hassan, M.; Sagr, L. Stress and stressors of myocardial infarction patients in the early period after discharge. J. Adv. Nurs. 2002, 40, 181–188. [Google Scholar] [CrossRef]
- Dani, S.; Minhas, A.; Arshad, A.; Krupica, T.; Goel, S.; Virani, S.; Sharma, G.; Blankstein, R.; Blaha, M.; Al-Kindi, S.; et al. Trends in characteristics and outcomes of hospitalized young patients undergoing coronary artery bypass grafting in the United States, 2004 to 2018. J. Am. Heart Assoc. 2021, 10, e021361. [Google Scholar] [CrossRef]
- Ordóñez-Piedra, J.; Ponce-Blandón, J.A.; Robles-Romero, J.M.; Gómez-Salgado, J.; Jiménez-Picón, N.; Romero-Martín, M. Effectiveness of the Advanced Practice Nursing interventions in the patient with heart failure: A systematic review. Nurs. Open 2021, 8, 1879–1891. [Google Scholar] [CrossRef] [PubMed]
| Author, Year, Country | Design | Sample | Intervention | Results (Mean Difference/SD) | EL/RG |
|---|---|---|---|---|---|
| Bikmoradi et al., 2016, Iran [29] | Quasi-experimental | n = 71 CG = 36 Male 62.9% Mean age 64.03 IG = 35 Male 75% Mean age 62 | Education, counselling + tele-nursing follow-up programs (drug use, adherence to physical activity and diet, not smoking, pain management, and taking care of the incision area) | -Medication plan CG: 7.03 (2.05) p < 0.001 IG: 10.8 (1.82) p < 0.01 -Care plan CG: 20.57 (2.14) p < 0.01 IG: 32.11 (2.56) p < 0.01 -Diet plan CG: 7.78 (1.34) p < 0.01 IG: 11.11 (1.08) p < 0.01 -Exercise plan CG: 6.28 (0.95) p < 0.01 IG: 9.22 (0.98) p < 0.01 -Overall adherence CG: 41.66 (4.69) p < 0.01 IG: 62.53 (4.85) p < 0.01 | 2b/B |
| Mohammadpour et al., 2015, Iran [30] | RCT | n = 66 CG = 33 Male 40.9% Mean age 53 IC = 33 Male 40.9% Mean age 52.4 | Three educational sessions (45-min) + phone calls + visit based on support and counselling (45 days) | Before intervention (CG/IG) -Knowledge 1.4 (0.5)/1.4 (0.5) -Motivation 1.6 (0.4)/1.7 (0.4) -Skill 1.5 (0.5)/1.3(0.4) After intervention (CG/IG) -Knowledge 1.5 (0.5)/2 (0.0) p < 0.001 -Motivation 1.6 (0.4)/2 (0.0) p < 0.001 -Skill 1.5 (0.5)/2 (0.0) p < 0.001 | 1b/A |
| Molazem et al., 2013, Iran [31] | RCT | n = 70 CG = 35 Male 60% Age > 50 years 60% IG = 35 Male 65.7% Age > 50 years 57.1% | 1.Orientation (making a relationship) 2.Sensitisation (continuous care and improving lifestyle, 45–60 min sessions) 3.Control (consultations sessions) 4.Evaluation of objectives (3 months) | Baseline (CG/IG) -Health responsibility 17.8 (3.8)/19.2 (4.6) -Physical activity 12.5 (2.8)/13.2 (3.4) -Nutrition 19.9 (3.6)/21.5 (3.4) -Spiritual growth 62.2(5.1)/27.8 (4.8) -Interpersonal relations 24.3 (5.1)/27.8 (4.8) -Stress management 17.7 (4.2)/17.5 (3.6) 3 months later (CG/IG) -Health responsibility 17.2 (4.4)/31.5 (3.6) p < 0.001 -Physical activity 12.5 (4.0)/25.9 (5.3) p < 0.001 -Nutrition 20.2 (4.4)/31.9 (3.4) p < 0.001 -Spiritual growth 25.9 (6.2)/32.2 (3.4) p < 0.001 -Interpersonal relations 24.3 (5.6)/31.3 (3.8) p < 0.001 -Stress management 17.9 (4.4)/27.4 (7.1) p < 0.001 | 1b/A |
| Negarandeh et al., 2012, Iran [32] | Quasi-experimental | n = 83 Age > 50 years CG = 41 Male 80% IG = 42 Male 59.5% | Hospital assessment + call phone to answer questions + 2 home visits (2 weeks) | Significant difference between the mean of two groups in terms of satisfaction with nursing care (p < 0.001) Significant difference between two groups in participants’ ability for self-care 6 weeks and 3 months after leaving the hospital (p < 0.001) | 2b/B |
| Cossette et al., 2012, Canada [33] | RCT | n = 242 Mean age 59.4 CG = 121 Male 90.1% IG = 121 Male 81% | Nurse-patient meeting before discharge + telephone call at 3 days post-discharge + telephone call or hospital meeting at 10 days post-discharge (6 weeks) | Discharge (CG/IG) -IPQ-R Chronic timeline 20.96 (4.80)/20.89(4.70) Negative consequences 19.89 (4.13)/20.08 (3.83) Personal control 24.20 (3.81)/24.07 (3.62) Treatment control 20.32 (2.88)/20.15 (2.71) Illness coherence 20.00 (3.69)/20.08 (3.29) Timeline cyclical 10.70 (3.12)/11.17 (2.65) Negative emotional representation 17.96 (4.98)/17.75 (4.46) -Family support 55.51 (7.92)/56.46 (6.82) -STAI 36.79 (11.31)/39.01 (11.89) -Medication adherence 43.9%/42.9% -Exercise (< 1 once a week) 40.2%/32.4% -Smoking (%) 21.4%/30.8% -BMI (% ≥ 30 kg/m2) 48.1%/37.8% -Healthy diet 62.83 (13.77)/62.30 (14.85) 6 weeks (CG/IG) -IPQ-R Chronic timeline 19.88 (5.81)/62.30 (14.85) p = 0.70 Negative consequences 18.54 (4.45)/18.79 (4.27) p = 0.78 Personal control 23.24 (3.42)/23.96 (2.82) p = 0.04 Treatment control 19.59 (2.42)/23.96 (2.82) p = 0.89 Illness coherence 20.39 (2.86)/20.29 (2.90) p = 0.75 Timeline cyclical 9.95 (2.70)/10.39 (0.32) p = 0.37 Negative emotional representation 15.29 (5.53)/10.39 (0.32) p = 0.96 -Family support 57.25 (5.97)/57.21 (6.49) p = 0.72 -STAI 29.83 (10.66)/57.21 (6.49) p= 0.74 Medication adherence 17.1%/14.3% p = 0.63 Exercise (< 1 once a week) 17.6%/19.4% p = 0.54 Smoking (%) 6.8%/13.1% p = 0.40 BMI (% ≥ 30 kg/m2) 38.3/34.4% p = 0.18 Healthy diet 74.77 (13.25)/75.72 (12.67) p = 0.47 | 1b/A |
| Fredericks, 2009, Canada [34] | RCT | n = 130 Male 52% Mean age 64 CG = 64 IG = 66 | Patient education telephone session + topics and necessities to solve complications + activities, medication, symptom management and psychological symptoms (3 weeks) | Pre-discharge/Post-discharge group -Knowledge 11 (2)/10 (2) p > 0.05 -RSCB 114 (25)/108 (25) p < 0.05 -Symptoms 41 (15)/42 (17) p > 0.05 -Anxiety 69 (15)/32 (15) p < 0.05 | 1b/A |
| Lapointe et al., 2006, Canada [35] | RCT | n = 127 CG = 63 Male 77.8% Mean age 56.9 IG = 64 Male 89.1% Mean age 57.8 | Telephone follow-up (18 months) | Baseline (IG) -LDL cholesterol level (mmol/L) 2.19 (0.65), 87.3% of patients <2.5 After 12 and 18 months (CG/IG): -LDL cholesterol level <2.5 mmol/L: 65%/51.6% p > 0.05 -SF-36 Mental and physical component showed significant improvements across time in the entire group (p < 0.02 to p < 0.04, two-factor ANOVA); no treatment or interaction effect was evident | 1b/A |
| Zhang et al., 2018, China [36] | RCT | n = 199 CG = 99 Male 57.1% Mean age 65.3 IG = 100 Male 50% Mean age 66.6 | Teaching + counselling, treatment + procedures, case management + surveillance (7 months) | Baseline (CG/IG) -SRAHP Exercise 11.1 (3.4)/10.7 (4.0) Psychological well-being 15.7 (4.8)/14.2 (4.2) Nutrition 13.7 (3.3)/14.6 (3.9) Health practices 16.8 (3.8)/17.9 (3.7) -SAQ Physical limitations 71.3 (17.4)/71.3 (20.0) Angina frequency 34.9 (25.4)/35.7 (23.0) Angina stability 59.2 (22.7)/66.2 (23.3) Treatment satisfaction 66.6 (17.6)/67.8 (15.4) Quality of life 42.9 (13.9)/48.1 (16.6) At 7 months (CG/IG) -SRAHP Exercise 15.5 (6.5)/18.8 (3.9) p < 0.001 Psychological well-being 16.6 (4.5)/19.1 (3.4) p < 0.001 Nutrition 16.4 (5.8)/20.2 (2.9) p < 0.001 Health practices18.2 (6.0)/21.7 (3.4) p < 0.001 -SAQ Physical limitations 70.9 (17.2)/75.0 (19.2) p = 0.29 Angina frequency 48.3 (26.1)/61.9 (26.9) Angina stability 62.3 (23.1)/77.2 (19.1) p < 0.001 Treatment satisfaction 67.0 (17.4)/77.0 (12.7) p < 0.001 Quality of life 48.5 (13.4)/58.3 (15.5) p < 0.001 Readmission rates (CG/IG) 17.2%/9.0% | 1b/A |
| Zhao and Wong, 2009 China [37] | RCT | n = 200 CG = 100 Mean age 71.58 Male 47% IG = 100 Mean age 72.86 Male 51% | Educational care programme: Predischarge assessment + structured home visits + telephone follow-up (12 weeks) | Baseline (CG/IG) High adherence -Diet 35%/27% -Medication 54%/58% -Exercise 63%/58% -Health-related lifestyle 40%/34% 12 weeks (CG/IG) High adherence -Diet 33%/50% p = 0.49 -Medication 51%/86% p = 0.34 -Exercise 62%/90% p = 0.06 -Health-related lifestyle 36%/72% p = 0.05 | 1b/A |
| Carroll and Rankin, 2006, USA [38] | RCT | n = 132 Male 32% Mean age 76.3 CG = 43 IG1 (peer advisor, former patient with history of MI) = 46 IG2 (APN with a specialisation in cardiovascular nursing) = 43 | Patient education + shared strategies (12 weeks) | Baseline (CG/IG1/IG2) -Self-efficacy 5.6 (2.4)/5.5 (2.2)/6.5 (6.1) -DASI-SE 17.3 (8.2)/15.6 (6.5)/17.2 (9.9) -SF-36 components Physical health 59 (21)/54 (19)/59 (26) Mental health 61 (20)/58 (21)/67 (21) 12 weeks (CG/IG1/IG2) -Self-efficacy 6.8 (2.3)/7.0 (2.0)/7.1 (2.0) p = 0.41 -DASI-SE 19.5 (8.1)/18.8 (6.6)/19.8 (7.3) p = 0.84 -SF-36 components: Physical health 66 (22)/67 (23)/62 (21) p = 0.20 Mental health 68 (19)/72 (20)/74 (20) p = 0.47 | 1b/A |
| Buckley et al., 2007, Australia [39] | RCT | n = 200 CG = 95 Mean age 65.43 IG = 105 Mean age 64.89 | Individual 40 to 50 min face-to-face education + counselling session phone call reinforcement (4 weeks) | Baseline (CG/IG) -Knowledge 63.67 (11.25)/63.33 (11.93) -Attitudes 14.08 (2.75)/13.89 (2.83) -Beliefs 30.06 (3.17)/29.52 (3.05) 12 months (CG/IG) -Knowledge 67.62 (10.99)/71.62 (11.37) p = 0.02 -Attitudes 14.97 (2.50)/15.48 (2.11) p = 0.20 -Beliefs 32.8 (3.90)/32.85 (3.54) p = 0.17 | 1b/A |
| Irmak and Fesci 2010, Turkey [40] | Quasi-experimental | n = 36 Male 77.8% Mean age 53.7 | Education program: change lifestyle, based on MI and risk factors, hypertension, nutritional habits, smoking cessation, physical activity, and drug treatment. (14 weeks) | Baseline (before discharge)/After 14 weeks -Smoker 61.1%/13.9% p < 0.001 -Caring food habits 5.6%/80.6% p < 0.001 -Regularly exercises 13.9%/86.11% p < 0.001 -Systolic blood pressure (mm Hg) 128.88 (17.44)/121.66 (8.00) p < 0.001 -Diastolic blood pressure (mm Hg) 80.13 (11.05)/76.66 (10.82) p < 0.01 -BMI (kg/m2) 26.93 (2.92)/26.49 (2.83) p = 0.02 -Total cholesterol level (mg/dL) 202.13 (43.50)/175.66 (36.32) p < 0.001 -LDL cholesterol level (mg/dl) 132.61 (40.76)/101.63 (38.31) p < 0.001 -HDL cholesterol level (mg/dL) 43.16 (7.23)/48.05 (8.59) p = 0.001 -Triglyceride’s level (mg/dL) 138.94 (59.04)/137.05 (57.42) p = 0.87 | 2b/B |
| Furuya et al., 2015, Brazil [41] | RCT | n = 60 CG = 30 Male 53.3% Mean age 60.6 IG = 30 Male 60% Mean age 63.3 | Educational programme + telephone follow-up (6 months) | Baseline (CG/IG) -SF-36 components Mental component 49.4 (12.1)/47.6 (9.4) Physical component 37.7 (8.7)/40.5 (10.1) -SF-36 domains Social functioning 71.2 (29.2)/75.4 (25.5) Mental health 68 (20.4)/66.9 (20.8) Physical functioning 57.8 (26.2)/65.5 (24.6) General health 61.9 (19.7)/64 (14.8) Vitality 62.7 (23.8)/61.8 (23) Bodily pain 50.8 (27.9)/57.7 (29.8) Role–emotional 58.9 (41.7)/51.1 (36.9) Role–physical 33.3 (34.9)/30 (34.4) -Self-efficacy 39.6 (7)/40.1 (7.5) -Symptoms of anxiety 7.3 (3.9)/7 (3.9) -Symptoms of depression 5.5 (4.3)/6.6 (3.9) 6 months (CG/IG) -SF-36 component Mental component 48.4 (9.2)/51.7 (9.5) Physical component 41 (11)/43.3 (10.6) p ≤ 0.05 -SF-36 domains Social functioning 64.2 (28.4)/79.2 (25.1) Mental health 70.1 (19.1)/70.9 (22.7) Physical functioning 64.5 (27.8)/72.5 (23.9) p ≤ 0.05 General health 63.9 (20)/66.1 (19.8) Vitality 62.5 (20.7)/69.7 (20.6) Bodily pain 55.7 (24.2)/63.8 (28.5) Role–emotional 64.4 (36)/77.8 (36.4) p ≤ 0.05 Role–physical 50 (44)/52.5 (40.7) p ≤ 0.05 -Self-efficacy 40 (6.6)/41.4 (7.1) -Symptoms of anxiety 7.6 (4.1)/5.1 (4.4) p ≤ 0.05 -Symptoms of depression 4.7 (3.5)/5.4 (4.8) | 1b/A |
| Hunger et al., 2015, Germany [42] | RCT | n = 329 CG = 168 Male 61.3% Mean age 75.6 IG = 161 Male 62.7% Mean age 75.2 | Individualised follow-up programme (home visits and telephone calls) (1 year) | Discharge (CG/IG) Clinical parameters -Systolic BP (mmHg) 124.2 (13.5)/121.6 (13.7) -Diastolic BP (mmHg) 71.3 (8.3)/71.4 (7.8) Physical functioning/mental health -HAQ-DI score 0.752 (0.752)/0.762 (0.808) -Barthel Index 90.8 (17.5)/90.8 (17.1) -Hand grip strength (kg) 28.2 (12.1)/28.6 (12.6) -MMSE 26.4 (3.8)/26.7 (4.1) -GDS-15 3.24 (2.64)/3.25 (3.11) -SCREEN-II 36.4 (6.3)/35.8 (7.2) At 1 year (CG/IG) Clinical parameters -Systolic BP (mmHg) 134.19 (18.91)/133.95 (18.57) p = 0.86 -Diastolic BP (mmHg) 73.85 (10.24)/74.16 (11.33) p = 0.99 Physical functioning/mental health -HAQ-DI score 0.77 (0.81)/0.53 (0.66) p = 0.03 -Barthel Index 93.64 (15.47)/97.63 (8.33) p = 0.01 -Hand grip strength (kg) 26.86 (11.54)/30.98 (11.55) p = 0.0001 -MMSE 27.73 (2.79)/28.10 (2.81) p = 0.65 -GDS 3.15 (2.64)/2.34 (2.31) p = 0.12 -SCREEN-II 36.57 (6.15)/38.93 (6.09) p < 0.01 -LDL cholesterol 100.31 (33.63)/92.03 (30.02) p = 0.04 | 1b/A |
| Mols et al., 2019, Denmark [43] | RCT | n = 294 CG = 147 Male 76% Mean age 65 (9.75) IC = 147 Male 76% Mean age 64 (9.28) | Motivational telephone consultation to support adherence to medical therapy, follow-up activities, emotional well-being, and healthy lifestyle (1 month) | Baseline (CG/IG) Healthy diet 17 (14)/27 (21) Healthy physical activity 44 (35)/53 (41) At 1 month (CG/IG) Healthy diet 18 (14)/23 (18) p= 0.425 Healthy physical activity 51 (41)/68 (53) p = 0.04 | 1b/A |
| Minneboo et al., 2017, Netherlands [44] | RCT | n = 711 Mean age 58.7 Male 79% CG = 351 IG = 360 | Community-based lifestyle programs with a nurse-coordinated referral (12 months) | Clinical parameters (CG/IG) -Systolic BP <140 mm Hg: 62%/70% of patients p = 0.04 -LDL cholesterol level <70 mg/dl 38%/34% of patients p = 0.23 -BMI (≤25 kg/m2) (CG/IG): 11%/15% of patients have a weight reduction p = 0.10 -6MWD (CG/IG): 40%/45% of patients have an improvement p = 0.29 | 1b/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Posadas-Collado, G.; Membrive-Jiménez, M.J.; Romero-Béjar, J.L.; Gómez-Urquiza, J.L.; Albendín-García, L.; Suleiman-Martos, N.; Cañadas-De La Fuente, G.A. Continuity of Nursing Care in Patients with Coronary Artery Disease: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 3000. https://doi.org/10.3390/ijerph19053000
Posadas-Collado G, Membrive-Jiménez MJ, Romero-Béjar JL, Gómez-Urquiza JL, Albendín-García L, Suleiman-Martos N, Cañadas-De La Fuente GA. Continuity of Nursing Care in Patients with Coronary Artery Disease: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(5):3000. https://doi.org/10.3390/ijerph19053000
Chicago/Turabian StylePosadas-Collado, Gloria, María J. Membrive-Jiménez, José L. Romero-Béjar, José L. Gómez-Urquiza, Luis Albendín-García, Nora Suleiman-Martos, and Guillermo A. Cañadas-De La Fuente. 2022. "Continuity of Nursing Care in Patients with Coronary Artery Disease: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 5: 3000. https://doi.org/10.3390/ijerph19053000
APA StylePosadas-Collado, G., Membrive-Jiménez, M. J., Romero-Béjar, J. L., Gómez-Urquiza, J. L., Albendín-García, L., Suleiman-Martos, N., & Cañadas-De La Fuente, G. A. (2022). Continuity of Nursing Care in Patients with Coronary Artery Disease: A Systematic Review. International Journal of Environmental Research and Public Health, 19(5), 3000. https://doi.org/10.3390/ijerph19053000











