The Impact of the COVID-19 Outbreak on Mental Wellbeing in Children with a Chronic Condition Compared to Healthy Peers
Abstract
:1. Introduction
2. Methods
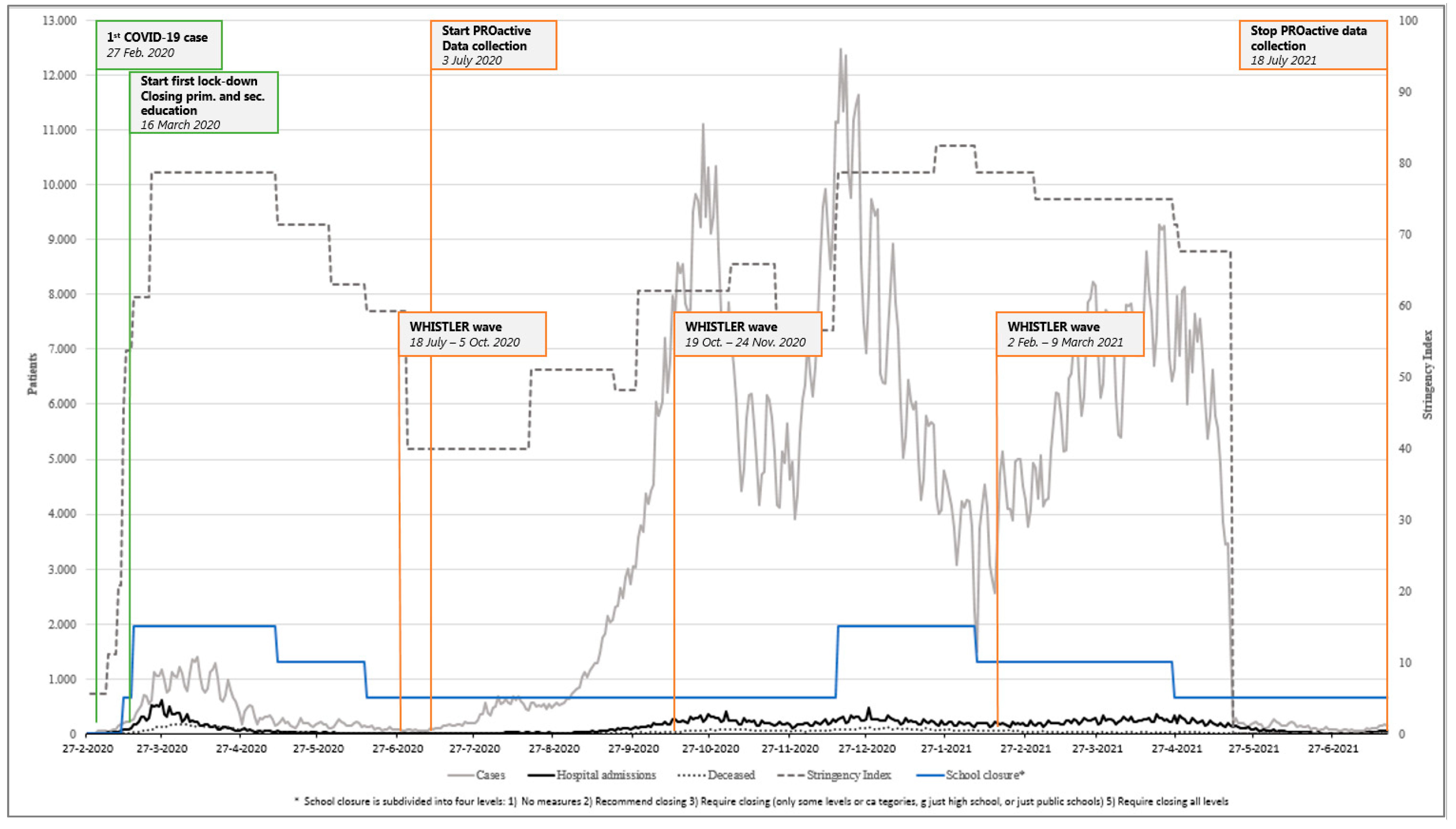
2.1. Research Population and Study Design
2.2. Measurements
2.3. Statistical Analyses
3. Results
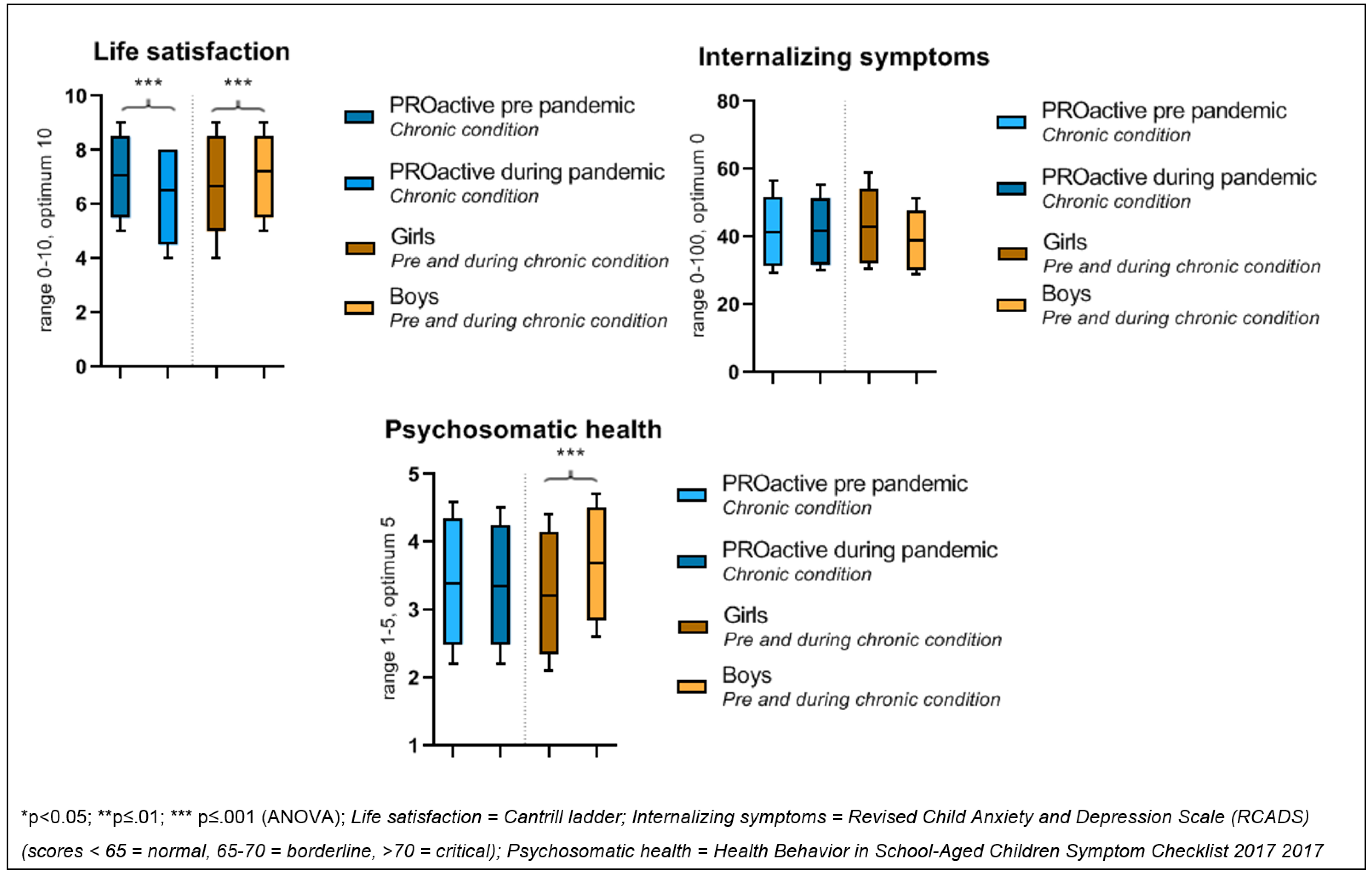
3.1. 1st Aim; Mental Wellbeing in Children with a Chronic Condition before versus during the Pandemic
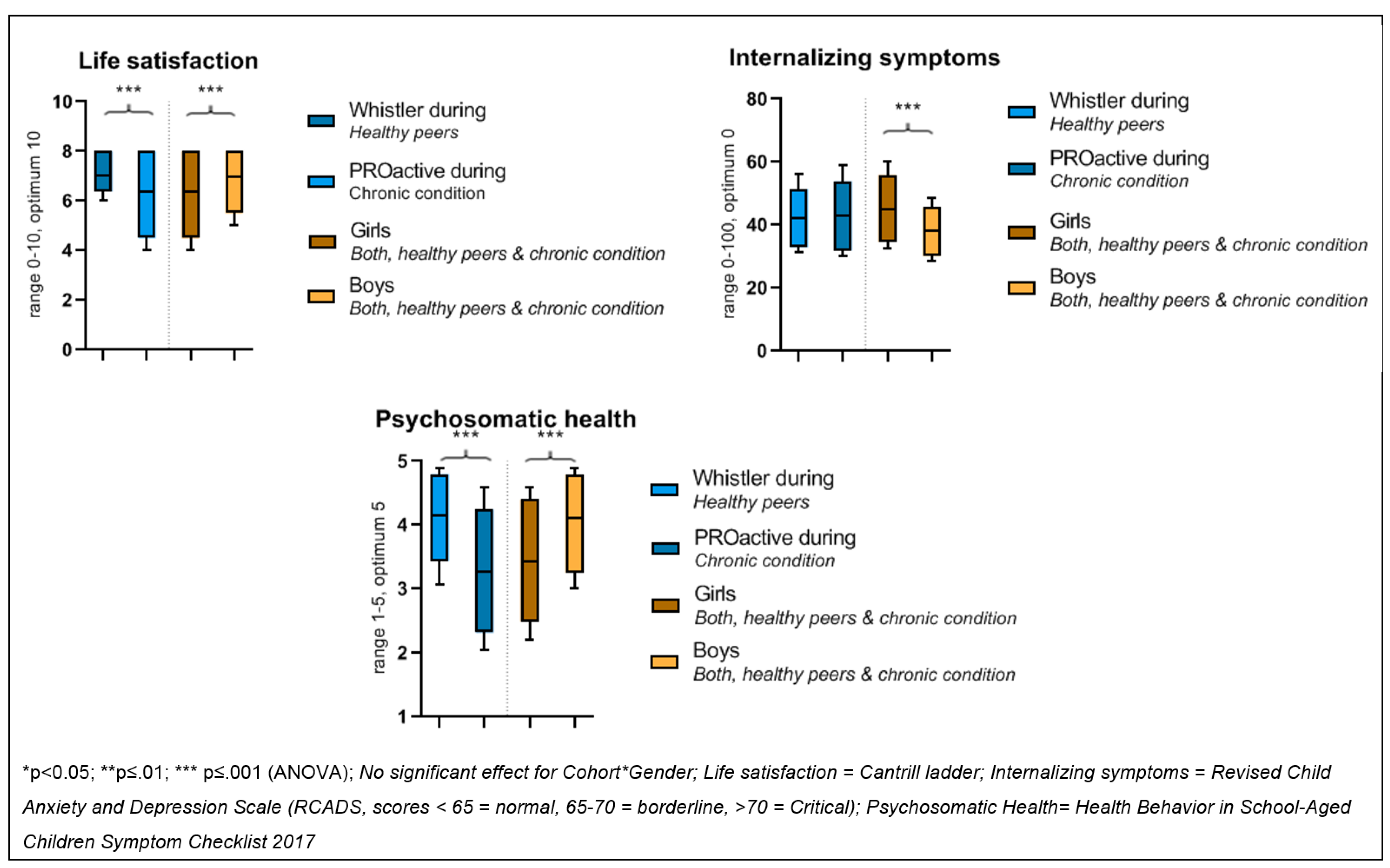
3.2. 2nd Aim: Mental Wellbeing in Children with a Chronic Condition versus Healthy Peers during the Pandemic
3.3. 3rd Aim: Associations between Government Restrictions and the Mental Wellbeing of Children with a Chronic Condition and Healthy Children
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020, 221, 264–266.e1. [Google Scholar] [CrossRef]
- Zhou, S.-J.; Zhang, L.-G.; Wang, L.-L.; Guo, Z.-C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.A.; Faulkner, G.; Rhodes, R.E.; Brussoni, M.; Chulak-Bozzer, T.; Ferguson, L.J.; Mitra, R.; O’Reilly, N.; Spence, J.C.; Vanderloo, L.M.; et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: A national survey. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 85. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, J.A.; Miller, E.A. Addressing the Consequences of School Closure Due to COVID-19 on Children’s Physical and Mental Well-Being. World Med. Health Policy 2020, 12, 300–310. [Google Scholar] [CrossRef]
- Ghosh, R.; Dubey, M.J.; Chatterjee, S.; Dubey, S. Impact of COVID-19 on children: Special focus on the psychosocial aspect. Minerva Pediatr. 2020, 72, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef] [PubMed]
- Almhizai, R.A.; Almogren, S.H.; Altwijery, N.A.; Alanazi, B.A.; Al Dera, N.M.; Alzahrani, S.S.; Alabdulkarim, S.M. Impact of COVID-19 on Children’s and Adolescent’s Mental Health in Saudi Arabia. Cureus 2021, 13, e19786. [Google Scholar] [CrossRef]
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Dattani, S.; Max, R. Coronavirus Pandemic (COVID-19). 2020. Available online: https://ourworldindata.org/covid-stringency-index (accessed on 31 August 2020).
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- van der Laan, S.E.I.; Finkenauer, C.; Lenters, V.C.; van Harmelen, A.-L.; van der Ent, C.K.; Nijhof, S.L. Gender-Specific Changes in Life Satisfaction After the COVID-19–Related Lockdown in Dutch Adolescents: A Longitudinal Study. J. Adolesc. Health 2021, 69, 737–745. [Google Scholar] [CrossRef]
- Marques de Miranda, D.; da Silva Athanasio, B.; Sena Oliveira, A.C.; Simoes-e-Silva, A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster Risk Reduct. 2020, 51, 101845. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239.e3. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect. Disord. 2020, 275, 112–118. [Google Scholar] [CrossRef]
- Berkelbach van der Sprenkel, E.E.; Nijhof, S.L.; Dalmeijer, G.W.; Onland-Moret, N.C.; de Roos, S.A.; Lesscher, H.M.B.; van de Putte, E.M.; van der Ent, C.K.; Finkenauer, C.; Stevens, G.W.J.M. Psychosocial functioning in adolescents growing up with chronic disease: The Dutch HBSC study. Eur. J. Pediatr. 2021, 181, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Varengue, R.; Brochard, S.; Bouvier, S.; Bailly, R.; Houx, L.; Lempereur, M.; Kandalaft, C.; Chatelin, A.; Vagnoni, J.; Vuillerot, C.; et al. Perceived impact of lockdown on daily life in children with physical disabilities and their families during the COVID-19 pandemic. Child Care Health Dev. 2021, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Maurice-Stam, H.; Nijhof, S.L.; Monninkhof, A.S.; Heymans, H.S.A.; Grootenhuis, M.A. Review about the impact of growing up with a chronic disease showed delays achieving psychosocial milestones. Acta Paediatr. Int. J. Paediatr. 2019, 108, 2157–2169. [Google Scholar] [CrossRef]
- Muilekom, M.M.; Luijten, M.A.J.; van Oers, H.A.; Conijn, T.; Maurice-Stam, H.; Goudoever, J.B.; Grootenhuis, M.A.; Haverman, L. Paediatric patients report lower health-related quality of life in daily clinical. Acta Paediatr. 2021, 101, 2264–2276. [Google Scholar]
- Liu, J.J.; Bao, Y.; Huang, X.; Shi, J.; Lin, L. Mental health considerations for children quarantined because of COVID-19. Lancet 2020, 4, 19–21. [Google Scholar] [CrossRef] [Green Version]
- Lee, J. Mental health effects of school closures during COVID-19. Lancet 2020, 4, 19–21. [Google Scholar] [CrossRef]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef]
- Moreno, C.; Wykes, T.; Galderisi, S.; Nordentoft, M.; Crossley, N.; Jones, N.; Cannon, M.; Correll, C.U.; Byrne, L.; Carr, S.; et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 813–824. [Google Scholar] [CrossRef]
- Borel, M.; Xie, L.; Kapera, O.; Mihalcea, A.; Kahn, J.; Messiah, S.E. Long-term physical, mental and social health effects of COVID-19 in the pediatric population: A scoping review. World J. Pediatr. 2022, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Nap-van der Vlist, M.M.; Hoefnagels, J.W.; Dalmeijer, G.W.; Moopen, N.; van der Ent, C.K.; Swart, J.F.; Putte van de, E.M.; Nijhof, S.L. The PROactive Cohort Study: Rationale, Design, and Study Procedures. Res. Sq. 2021, 17, 1–17. [Google Scholar] [CrossRef]
- Katier, N.; Uiterwaal, C.S.P.M.; De Jong, B.M.; Kimpen, J.; Verheij, T.; Grobbee, D.; Brunekreef, B.; Numans, M.; van der Ent, C. The Wheezing Illnesses Study Leidsche Rijn (WHISTLER): Rationale and Design. Eur. J. Epidemiology 2004, 19, 895–903. [Google Scholar] [CrossRef] [PubMed]
- Nap-van der Vlist, M.M.; Dalmeijer, G.W.; Grootenhuis, M.A.; van der Ent, C.K.; van den Heuvel-Eibrink, M.M.; Wulffraat, N.M.; Swart, J.F.; Van Litsenburg, R.R.; Van De Putte, E.M.; Nijhof, S.L. Fatigue in childhood chronic disease. Arch. Dis. Child. 2019, 104, 1090–1095. [Google Scholar] [CrossRef] [PubMed]
- Wiersinga, W.J. SARS-CoV-2 in Nederland: De kliniek van een nieuw virus [Clinical Characteristics of Coronavirus Disease 2019 in The Netherlands]. Ned. Tijdschr. Geneeskd. 2020, 164, 20–22. [Google Scholar]
- Rijksinstituut voor Volksgezondheid en Milieu. Webpage COVID Data on Confirmed Cases, Hospitalization, School Closure and Deceased. 2021. Available online: https://www.rivm.nl/coronavirus-covid-19/grafieken#vanaf-27-februari-2020-462441 (accessed on 31 August 2021).
- Rijksinstituut voor Volksgezondheid en Milieu. Webpage COVID-19 Dutch Stringency Index. 2021. Available online: https://www.rivm.nl/gedragsonderzoek/tijdlijn-maatregelen-covid (accessed on 31 August 2021).
- Levin, K.A.; Currie, C. Reliability and Validity of an Adapted Version of the Cantril Ladder for Use with Adolescent Samples. Soc. Indic. Res. 2014, 119, 1047–1063. [Google Scholar] [CrossRef]
- Mazur, J.; Szkultecka-Dębek, M.; Dzielska, A.; Drozd, M.; Małkowska-Szkutnik, A. What does the Cantril Ladder measure in adolescence? Arch. Med. Sci. 2018, 1, 182–189. [Google Scholar] [CrossRef]
- Kösters, M.P.; Chinapaw, M.J.M.; Zwaanswijk, M.; van der Wal, M.F.; Koot, H.M. Structure, reliability, and validity of the revised child anxiety and depression scale (RCADS) in a multi-ethnic urban sample of Dutch children. BMC Psychiatry 2015, 15, 2–8. [Google Scholar] [CrossRef] [Green Version]
- Chorpita, B.F.; Yim, L.; Moffitt, C.; Umemoto, L.A.; Francis, S.E. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behav. Res. Ther. 2000, 38, 835–855. [Google Scholar] [CrossRef]
- Child Outcomes and Research Consortium. Revised Children’s Anxiety and Depression Scale (and Subscales) (RCADS). Available online: https://www.corc.uk.net/outcome-experience-measures/revised-childrens-anxiety-and-depression-scale-rcads/ (accessed on 20 December 2021).
- Ravens-Sieberer, U.; Erhart, M.; Torsheim, T.; Hetland, J.; Freeman, J.; Danielson, M.; Thomas, C.; The HBSC Positive Health Group. An international scoring system for self-reported health complaints in adolescents. Eur. J. Public Health 2008, 18, 294–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erhart, M.; the HBSC Positive Health Focus Group; Ottova, V.; Gaspar, T.; Jericek, H.; Schnohr, C.; Alikasifoglu, M.; Morgan, A.; Ravens-Sieberer, U. Measuring mental health and well-being of school-children in 15 European countries using the KIDSCREEN-10 Index. Int. J. Public Health 2009, 54 (Suppl. 2), 160–166. [Google Scholar] [CrossRef] [PubMed]
- Greene, J.W.; Walker, L.S. Psychosomatic Problems and Stress in Adolescence. Pediatr. Clin. N. Am. 1997, 44, 1557–1572. [Google Scholar] [CrossRef]
- Zijlmans, J.; Teela, L.; van Ewijk, H.; Klip, H.; van der Mheen, M.; Ruisch, H.; Luijten, M.A.J.; van Muilekom, M.M.; Oostrom, K.J.; Buitelaar, J.; et al. Mental and Social Health of Children and Adolescents with Pre-Existing Mental or Somatic Problems during the COVID-19 Pandemic Lockdown. Front. Psychiatry 2021, 12, 692853. [Google Scholar] [CrossRef]
- Kwok, S.; Engle, J.; Datta, A.N. Resilience of adolescents and teenagers with self-limited and genetic-generalized epilepsy during the COVID-19 pandemic. Epilepsy Behav. Rep. 2022, 17, 100520. [Google Scholar] [CrossRef] [PubMed]
- Samji, H.; Wu, J.; Ladak, A.; Vossen, C.; Stewart, E.; Dove, N.; Long, D.; Snell, G. Review: Mental health impacts of the COVID-19 pandemic on children and youth—A systematic review. Child Adolesc. Ment. Health 2021. Available online: https://acamh-onlinelaibrary-wiley-com.mutex.gmu.edu/doi/full/10.1111/camh.12501 (accessed on 31 August 2020). [CrossRef] [PubMed]
- Viner, R.; Russell, S.; Saulle, R.; Croker, H.; Stansfield, C.; Packer, J.; Nicholls, D.; Goddings, A.-L.; Bonell, C.; Hudson, L.; et al. School Closures during Social Lockdown and Mental Health, Health Behaviors, and Well-Being Among Children and Adolescents during the First COVID-19 Wave: A Systematic Review. JAMA Pediatr. 2022, 18, 1–10. [Google Scholar] [CrossRef]
| 1st Aim (Chronic Condition before vs. during) | 2nd and 3rd Aims (Chronic Condition vs. Healthy Peers during the Pandemic) | |||
|---|---|---|---|---|
| Characteristics | PROactive (Chronic Condition) | PROactive—(Chronic Condition) a | Whistler—(Healthy Peers) | |
| Pre-Pandemic 8–18 yr N = 944 | During Pandemic 8–18 yr N = 545 | During Pandemic 12–18 yr N = 311 | During Pandemic 12–18 yr N = 166 | |
| Age in years, mean ± SD | 14.2 (2.8) | 14.3 (2.9) | 15.7 (1.8) | 16.0 (1.3) |
| Girl, n (%) | 601 (64.2) | 332 (60.9) | 200 (64.3) | 94 (56.6) |
| Disease group | ||||
| 481 (51.0) | 269 (49.4) | 67 (21.5) | n.a. |
| 305 (32.3) | 106 (19.4) | 163 (52.4) | n.a. |
| 72 (7.6) | 26 (4.8) | 17 (5.5) | n.a. |
| 63 (6.7) | 111 (20.4) | 46 (14.8) | n.a. |
| 22 (2.3) | 33 (6.1) | 18 (5.8) | n.a. |
| Education level of the child b, n (%) | ||||
| 219 (24.0) | 105 (25.6) | 14 (5.8) | 3 (1.8) |
| 271 (29.7) | 117 (28.5) | 94 (39.0) | 40 (24.1) |
| 208 (22.8) | 86 (21) | 69 (28.6) | 37 (22.3) |
| 177 (19.4) | 79 (19.3) | 64 (26.6) | 81 (48.8) |
| 37 (4.1) | 23 (5.6) | 0 (0) | 5 (3.0) |
| Life Satisfaction | Internalising Symptoms | Psychosomatic Health | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | 95% Confidence Interval for B | β | Adj. R2 | B | 95% Confidence Interval for B | β | Adj. R2 | B | 95% Confidence Interval for B | β | Adj. R2 | |||||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||||||
| Step 1 | 0.026 *** | 0.029 * | 0.015 * | |||||||||||||
| Stringency | −0.015 | −0.023 | −0.007 | −0.166 *** | 0.107 | 0.043 | 0.171 | 0.183 *** | −0.007 | −0.012 | −0.001 | −0.132 ** | ||||
| Step 2 | 0.064 *** | 0.034 ** | 0.268 *** | |||||||||||||
| Stringency | −0.017 | −0.025 | −0.009 | −0.185 *** | 0.114 | 0.050 | 0.178 | 0.183 *** | −0.009 | −0.014 | −0.005 | −0.182 *** | ||||
| Group | −0.698 | −1.002 | −0.395 | −0.201 *** | 1.683 | −0.718 | 4.08 | 0.072 ns | −0.912 | −1.075 | −0.749 | −0.508 *** | ||||
| Step 3 | 0.062 ns | 0.037 ** | 0.282 ** | |||||||||||||
| Stringency | −0.010 | −0.042 | 0.021 | −0.114 ns | 0.000 | −0.241 | 0.0.241 | 0.001 ns | 0.12 | −0.004 | −0.027 | 0.238 ns | ||||
| Group | −0.693 | −0.998 | 0.389 | −0.200 *** | 1.529 | −0.892 | 3.951 | 0.066 ns | −0.900 | −1.061 | −0.738 | −0.501 *** | ||||
| Interaction | −0.004 | −0.021 | 0.041 | −0.073 ns | 0.068 | −0.071 | 0.206 | 0.188 ns | −0.013 | −0.022 | −0.004 | −0.438 ** | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoefnagels, J.W.; Schoen, A.B.; van der Laan, S.E.I.; Rodijk, L.H.; van der Ent, C.K.; van de Putte, E.M.; Dalmeijer, G.W.; Nijhof, S.L. The Impact of the COVID-19 Outbreak on Mental Wellbeing in Children with a Chronic Condition Compared to Healthy Peers. Int. J. Environ. Res. Public Health 2022, 19, 2953. https://doi.org/10.3390/ijerph19052953
Hoefnagels JW, Schoen AB, van der Laan SEI, Rodijk LH, van der Ent CK, van de Putte EM, Dalmeijer GW, Nijhof SL. The Impact of the COVID-19 Outbreak on Mental Wellbeing in Children with a Chronic Condition Compared to Healthy Peers. International Journal of Environmental Research and Public Health. 2022; 19(5):2953. https://doi.org/10.3390/ijerph19052953
Chicago/Turabian StyleHoefnagels, Johanna W., Annelieke B. Schoen, Sabine E. I. van der Laan, Lyan H. Rodijk, Cornelis K. van der Ent, Elise M. van de Putte, Geertje W. Dalmeijer, and Sanne L. Nijhof. 2022. "The Impact of the COVID-19 Outbreak on Mental Wellbeing in Children with a Chronic Condition Compared to Healthy Peers" International Journal of Environmental Research and Public Health 19, no. 5: 2953. https://doi.org/10.3390/ijerph19052953
APA StyleHoefnagels, J. W., Schoen, A. B., van der Laan, S. E. I., Rodijk, L. H., van der Ent, C. K., van de Putte, E. M., Dalmeijer, G. W., & Nijhof, S. L. (2022). The Impact of the COVID-19 Outbreak on Mental Wellbeing in Children with a Chronic Condition Compared to Healthy Peers. International Journal of Environmental Research and Public Health, 19(5), 2953. https://doi.org/10.3390/ijerph19052953







