“Time Does Not Heal All Wounds”: Sexual Victimisation Is Associated with Depression, Anxiety, and PTSD in Old Age
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Selection
2.2. Definitions and Measures
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Association between Lifetime SV and Depression, Anxiety, and PTSD
4. Discussion
4.1. Mental Health Problems Are Common in Older Adults in Belgium
4.2. Lifetime Sexual Victimisation Is Linked with Depression, Anxiety, and PTSD in Older Adults
4.3. Past 12-Month Sexual Violence, Social Support, and Resilience Do Not Moderate the Relationship between Lifetime Sexual Victimisation and Depression, Anxiety, and PTSD
4.4. Limitations
4.5. Recommendations for Future Research and Clinical Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| α | Cronbach’s alpha |
| BRS | Brief Resilience Scale |
| BSQ | Behavioural Specific Questions |
| CAPS-5 | Clinician-Administered PTSD scale for DSM-5 |
| CI | Confidence Interval |
| CSA | Child Sexual Abuse |
| DSM-IV | Diagnostic and Statistical Manual of Mental Disorders, fourth edition |
| DSM-5 | Diagnostic and Statistical Manual of Mental Disorders, fifth edition |
| GAD-7 | General Anxiety Disorder- 7 |
| PCL-5 | PTSD Checklist for DSM-5 |
| PC-PTSD-5 | Primary Care PTSD Screen for DSM-5 |
| PHQ-9 | Patient Health Questionnaire-9 |
| PTSD | Post-Traumatic Stress Disorder |
| SMI | Severe Mental Illness |
| SV | Sexual Violence |
| VIF | Variance Inflation factor |
| VLESP | Vlaamse Expertisecentrum Suïcidepreventie/Flemish Centre for Suicide Prevention |
| WHO | World Health Organization |
| WPA | World Psychiatric Association |
Appendix A. Detailed Outcome Measurements Sexual Victimization
- Sexual staring: Someone stared at me in a sexual way or looked at my intimate body parts (e.g., breasts, vagina, penis, anus) when I didn’t want it to happen.
- Sexual innuendo: Someone made teasing comments of a sexual nature about my body or appearance even though I didn’t want it to happen.
- Showing sexual images: Someone showed me sexual or obscene materials, such as pictures or videos, directly or over the internet (including email, social networks, and chat platforms), even though I didn’t want to look at them. This does not include mass mailings or spam.
- Sexual calls or texts: Someone made unwelcome sexual or obscene phone calls or texts to me.
- Voyeurism: I caught someone watching me, taking photos, or filming me when I didn’t want it to happen while I was undressing, nude, or having sex.
- Distribution of sexual images: Someone distributed naked pictures or videos of me directly or over the internet (including email, social networks, and chat platforms) when I didn’t want it to happen.
- Exhibitionism: Someone showed their intimate body parts (e.g., breasts, vagina, penis, anus) to me in a sexual way and/or masturbated in front of me when I didn’t want to see it.
- Forcing to show intimate body parts: Someone made me show my intimate body parts (e.g., breasts, vagina, penis, anus) online or face-to-face when I didn’t want to do it.Hands-on sexual victimisationSexual abuse (physical contact but no penetration):
- Kissing: Someone kissed me against my will.
- Touching in care: Someone touched my intimate body parts (e.g., breasts, vagina, penis, anus) during care against my will.
- Fondling/rubbing: Someone fondled or rubbed up against my intimate body parts (e.g., breasts, vagina, penis, anus) against my will.
- Forced undressing: Someone removed (some of) my clothes against my will.Rape and attempted rape (physical contact with attempted or completed penetration):
- Oral penetration: Someone had oral sex with me or made me give oral sex against my will.
- Attempt of oral penetration: Someone tried but did not succeed to have oral sex with me or tried to make me give oral sex against my will.
- Vaginal or anal penetration: Someone put their penis, finger(s), or object(s) into my vagina or anus against my will.
- Attempt of vaginal or anal penetration: Someone tried but did not succeed to put their penis, finger(s), or object(s) into my vagina or anus against my will.
- Forcing to penetrate: Someone made me put my penis, finger(s), or object(s) into their (or someone’s) vagina or anus against my will.
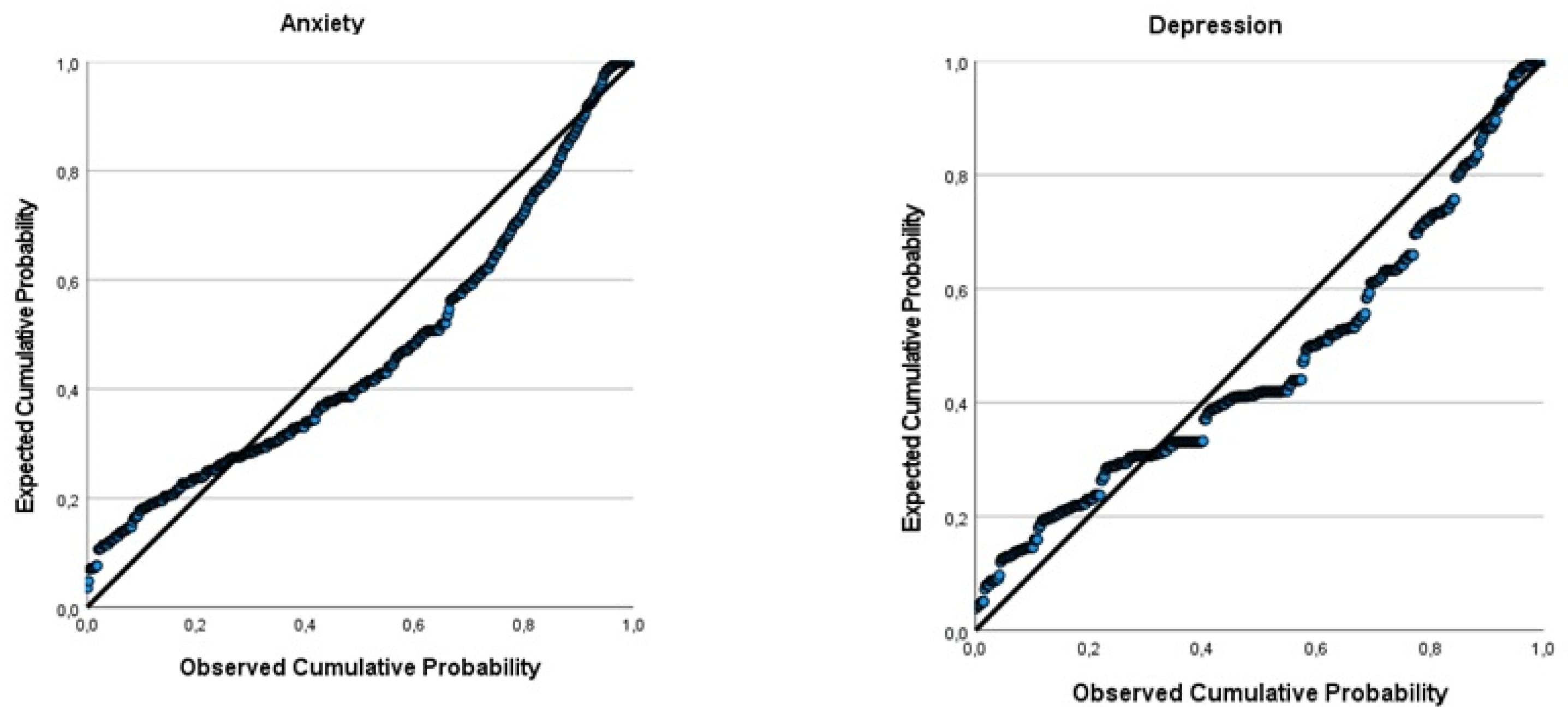
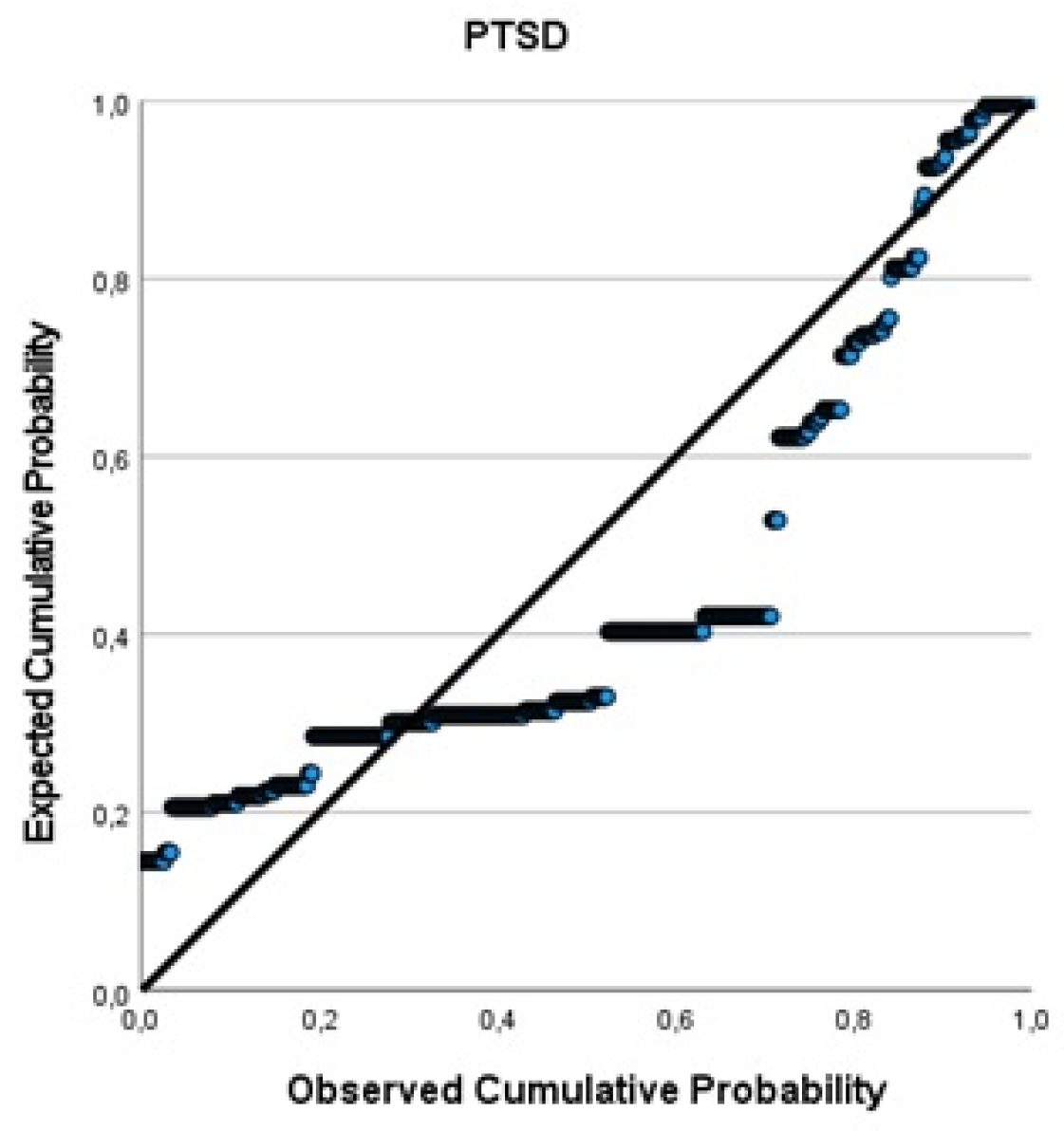
Appendix B. Q-Q Plots of the Outcome Variables of the Linear Regression Model
References
- World Health Organization. Violence Against Women Factsheet No. 239. 2017. Available online: http://www.who.int/mediacentre/factsheets/fs239/en/ (accessed on 4 April 2021).
- World Health Assembly. Prevention of violence: A public health priority. In Proceedings of the Forty-Ninth World Health Assembly, Geneva, Switzerland, 13 November 1996. [Google Scholar]
- Nobels, A.; Vandeviver, C.; Beaulieu, M.; Cismaru-Inescu, A.; Nisen, L.; Van Den Noortgate, N.; Vander Beken, T.; Lemmens, G.; Keygnaert, I. “Too Grey to Be True?” Sexual Violence in Older Adults: A Critical Interpretive Synthesis of Evidence. Int. J. Environ. Res. Public Health 2020, 17, 4117. [Google Scholar] [CrossRef] [PubMed]
- Nobels, A.; Cismaru-Inescu, A.; Nisen, L.; Hahaut, B.; Beaulieu, M.; Lemmens, G.; Adam, S.; Schapanksy, E.; Vandeviver, C.; Keygnaert, I. Sexual Violence in Older Adults: A Belgian Prevalence Study. BMC Geriatr. 2021, 21, 601. [Google Scholar] [CrossRef] [PubMed]
- Mental Health of Older Adults-Factsheet. 2017. Available online: https://www.who.int/newsroom/fact-sheets/detail/mental-health-of-older-adults (accessed on 30 March 2021).
- Meeks, T.W.; Vahia, I.V.; Lavretsky, H.; Kulkarni, G.; Jeste, D.V. A tune in “a minor” can “b major”: A review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J. Affect. Disord. 2011, 129, 126–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolitzky-Taylor, K.B.; Castriotta, N.; Lenze, E.J.; Stanley, M.A.; Craske, M.G. Anxiety disorders in older adults: A comprehensive review. Depress. Anxiety 2010, 27, 190–211. [Google Scholar] [CrossRef]
- Böttche, M.; Kuwert, P.; Knaevelsrud, C. Posttraumatic stress disorder in older adults: An overview of characteristics and treatment approaches. Int. J. Geriatr. Psychiatry 2012, 27, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Rodda, J.; Walker, Z.; Carter, J. Depression in older adults. BMJ 2011, 343, d5219. [Google Scholar] [CrossRef]
- Olofsson, N.; Lindqvist, K.; Danielsson, I. Fear of crime and psychological and physical abuse associated with ill health in a Swedish population aged 65–84 years. Public Health 2012, 126, 358–364. [Google Scholar] [CrossRef] [Green Version]
- Ege, M.A.; Messias, E.; Thapa, P.B.; Krain, L.P. Adverse childhood experiences and geriatric depression: Results from the 2010 BRFSS. Am. J. Geriatr. Psychiatry 2015, 23, 110–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rapsey, C.M.; Scott, K.M.; Patterson, T. Childhood sexual abuse, poly-victimization and internalizing disorders across adulthood and older age: Findings from a 25-year longitudinal study. J. Affect. Disord. 2019, 244, 171–179. [Google Scholar] [CrossRef]
- Naughton, C.; Drennan, J.; Lyons, I.; Lafferty, A.; Treacy, M.; Phelan, A.; O’Loughlin, A.; Delaney, L. Elder abuse and neglect in Ireland: Results from a national prevalence survey. Age Ageing 2012, 41, 98–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luoma, M.; Koivusilta, M.; Lang, G.; Enzenhofer, E.; De Donder, L.; Verté, D.; Reingarde, J.; Tamutiene, I.; Ferreira-Alves, J.; Santos, A.J.; et al. Prevalence Study of Abuse and Violence against Older Women; Results of a Multi-Cultural Survey in Austria, Belgium, Finland, Lithuania, and Portugal (European Report of the AVOW Project); National Institute for Health and Welfare (THL): Helsinki, Finland, 2011. [Google Scholar]
- Declercq, F.; Palmans, V. Two subjective factors as moderators between critical incidents and the occurrence of post-traumatic stress disorders: Adult attachment and perception of social support. Psychol. Psychother. Theory Res. Pract. 2006, 79, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Declercq, F.; Vanheule, S.; Markey, S.; Willemsen, J. Posttraumatic distress in security guards and the various effects of social support. J. Clin. Psychol. 2007, 63, 1239–1246. [Google Scholar] [CrossRef]
- Schulz, A.; Becker, M.; Van der Auwera, S.; Barnow, S.; Appel, K.; Mahler, J.; Schmidt, C.O.; John, U.; Freyberger, H.J.; Grabe, H.J. The impact of childhood trauma on depression: Does resilience matter? Population-based results from the Study of Health in Pomerania. J. Psychosom. Res. 2014, 77, 97–103. [Google Scholar] [CrossRef]
- Fedina, L.; Nam, B.; Jun, H.-J.; Shah, R.; Von Mach, T.; Bright, C.L.; De Vylder, J. Moderating effects of resilience on depression, psychological distress, and suicidal ideation associated with interpersonal violence. J. Interpers. Violence 2021, 36, NP1335–1358NP. [Google Scholar] [CrossRef]
- Yarns, B.C.; Abrams, J.M.; Meeks, T.W.; Sewell, D.D. The Mental Health of Older LGBT Adults. Curr. Psychiatry Rep. 2016, 18, 60. [Google Scholar] [CrossRef] [PubMed]
- Nobels, A.; Keygnaert, I.; Robert, E.; Vandeviver, C.; Haekens, A.; Lemey, L.; Strobbe, M.; Van Den Noortgate, N.; Lemmens, G. ‘Breaking the silence’: Sexual victimisation in an old age psychiatry patient population in Flanders. Int. J. Geriat. Psychiatry. 2021, 36, 1550–1558. [Google Scholar] [CrossRef] [PubMed]
- Steward, E.D.; Chandra, P.S. WPA Position Paper on Intimate Partner Violence and Sexual Violence against Women: Geneva, Switerland. 2017. Available online: https://globalalliancematernalmentalhealth.org/wp-content/uploads/2018/03/WPA_position_Intimate_Partner_Violence_Sexual_Violence_Against_Women29012018.pdf (accessed on 30 June 2021).
- Goldblatt, H.; Band-Winterstein, T.; Lev, S.; Harel, D. “Who Would Sexually Assault an 80-Year-Old Woman?” Barriers to Exploring and Exposing Sexual Assault Against Women in Late Life. J. Interpers. Violence 2020, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Keygnaert, I.; Vandeviver, C.; Nisen, L.; De Schrijver, L.; Depraetere, J.; Nobels, A.; Cismaru-Inescu, A.; Lemonne, A.; Renard, B.; Vander Beken, T. Seksueel geweld in België: Eerste representatieve prevalentiestudie naar de aard, omvang en impact van seksueel geweld in België. Sci. Connect. 2018, 59, 28–31. [Google Scholar]
- Nobels, A.; Cismaru-Inescu, A.; Nisen, L.; Hahaut, B.; Lemmens, G.; Vandeviver, C.; Keygnaert, I. Challenges in conducting sexual health and violence research in older adults beyond the general data protection regulation: A Belgian case study. J. Interpers. Violence 2021, 1–21. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ethical and Safety Recommendations for Intervention Research on Violence against Women: Building on Lessons from the WHO Publication Putting Women First: Ethical and Safety Recommendations for Research on Domestic Violence against Women; WHO: Geneva, Switerland, 2016. [Google Scholar]
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef] [Green Version]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Prins, A.; Bovin, M.J.; Kimerling, R.; Kaloupek, D.G.; Marx, B.P.; Pless Kaiser, A.; Schnurr, P.P. Primary Care PTSD Screen for DSM-5 (PC-PTSD-5); National Centre for PTSD, US Department of Veteran Affairs: Washington, DC, USA, 2015.
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Koss, M.P.; Gidycz, C.A. Sexual experiences survey: Reliability and validity. J. Consult. Clin. Psychol. 1985, 53, 422–423. [Google Scholar] [CrossRef] [PubMed]
- Krahé, B.; Berger, A.; Vanwesenbeeck, I.; Bianchi, G.; Chliaoutakis, J.; Fernández-Fuertes, A.A.; Fuertes, A.; de Matos, M.G.; Hadjigeorgiou, E.; Haller, B. Prevalence and correlates of young people’s sexual aggression perpetration and victimisation in 10 European countries: A multi-level analysis. Cult. Health Sex. 2015, 17, 682–699. [Google Scholar] [CrossRef] [PubMed]
- Keygnaert, I.; Dias, S.F.; Degomme, O.; Deville, W.; Kennedy, P.; Kovats, A.; De Meyer, S.; Vettenburg, N.; Roelens, K.; Temmerman, M. Sexual and gender-based violence in the European asylum and reception sector: A perpetuum mobile? Eur. J. Public Health 2015, 25, 90–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Depraetere, J.; Cismaru-Inscu, A.; De Schrijver, L.; Nobels, A.; Keygnaert, I.; Vandeviver, C. Measuring Sexual Victimisation and Perpetration in Today’s Society: Modifications to the Sexual Experience Survey. SocArXiv 2020. [Google Scholar] [CrossRef]
- Allison, P.D. Logistic Regression Using SAS: Theory and Applications; SAS Institute: Carey, NC, USA, 2012. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 26.0. Armonk; IBM Corp: New York, NY, USA, 2019. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2014; Available online: http://www.R-project.org/ (accessed on 14 February 2022).
- Hair, J.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson Educational International: Bergen County, NJ, USA, 2010. [Google Scholar]
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming; Routledge: New York, NY, USA, 2010. [Google Scholar]
- Kaiser, A.P.; Wachen, J.S.; Potter, C.; Moye, J.; Davison, E. With the Stress, Health, and Aging Research Program (SHARP. Posttraumatic Stress Symptoms among Older Adults: A Review. PTSD: National Centre for PTSD. Available online: https://www.ptsd.va.gov/professional/treat/specific/symptoms_older_adults.asp (accessed on 7 February 2022).
- Rutherford, B.R.; Zilcha-Mano, S.; Chrisanthopolous, M.; Salzman, C.; Zhu, C.; Cimino, N.; Yehuda, R.; Neria, Y.; Roose, S.P. Symptoms profiles and treatment status of older adults with chronic post-traumatic stress disorder. Int. J. Geriatr. Psychiatry 2021, 36, 1216–1222. [Google Scholar] [CrossRef] [PubMed]
- Calhoun, P.S.; Hertzberg, J.S.; Kirby, A.C.; Dennis, M.F.; Hair, L.P.; Dedert, E.A.; Beckham, J.C. The effect of draft DSM-V criteria on posttraumatic stress disorder prevalence. Depress. Anxiety 2012, 29, 1032–1042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kilpatrick, D.G.; Resnick, H.S.; Milanak, M.E.; Miller, M.W.; Keyes, K.M.; Friedman, M.J. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J. Trauma. Stress 2013, 26, 537–547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weathers, F.W.; Blake, D.D.; Schnurr, P.P.; Kaloupek, D.G.; Marx, B.P.; Keane, T.M. Clinician-Administered PTSD Scale for DSM-5 (CAPS-5); National Center for Posttraumatic Stress Disorder, US Department of Veteran Affairs: Washington, DC, USA, 2013.
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. PTSSD Checklist for DSM-5 (PCL-5); National Center for Posttraumatic Stress Disorder, US Department of Veteran Affairs: Washington, DC, USA, 2013.
- Zelfmoord 1813. Zelfmoord Bij Ouderen Factsheet 2018. Available online: https://www.zelfmoord1813.be/sites/default/files/Factsheet%20Ouderen-min.pdf (accessed on 30 June 2021).
- Cole, M.G.; Dendukuri, N. Risk factors for depression among elderly community subjects: A systematic review and meta-analysis. Am. J. Psychiatry 2003, 160, 1147–1156. [Google Scholar] [CrossRef]
- Hardy, S.E.; Concato, J.; Gill, T.M. Resilience of community-Dwelling older persons. J. Am. Geriatr. Soc. 2004, 52, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Leys, C.; Arnal, C.; Wollast, R.; Rolin, H.; Kotsou, I.; Fossion, P. Perspectives on resilience: Personality trait or skill? Eur. J. Trauma Dissociation 2020, 4, 100074. [Google Scholar] [CrossRef]
- Akatsuka, E.; Tadaka, E. Development of a resilience scale for oldest-old age (RSO). BMC Geriatr. 2021, 21, 174. [Google Scholar] [CrossRef] [PubMed]
- Nobels, A.; De Schrijver, L.; Van Landuyt, M.; Vandeviver, C.; Lemmens, G.; Beaulieu, M.; Keygnaert, I. “In the end you keep silent”: Help-seeking behaviour upon sexual victimisation in older adults. Preprint 2022. [Google Scholar]
- Dartnall, E.; Jewkes, R. Sexual violence against women: The scope of the problem. Best Pract. Res. Clin. Obstet. Gynaecol. 2013, 27, 3–13. [Google Scholar] [CrossRef]
- Khalifeh, H.; Moran, P.; Borschmann, R.; Dean, K.; Hart, C.; Hogg, J.; Osborn, D.; Johnson, S.; Howard, L.M. Domestic and sexual violence against patients with severe mental illness. Psychol. Med. 2015, 45, 875–886. [Google Scholar] [CrossRef] [Green Version]
- Scott, K.M.; McLaughlin, K.A.; Smith, D.A.; Ellis, P.M. Childhood maltreatment and DSM-IV adult mental disorders: Comparison of prospective and retrospective findings. Br. J. Psychiatry 2012, 200, 469–475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunn, E.C.; Nishimi, K.; Powers, A.; Bradley, B. Is developmental timing of trauma exposure associated with depressive and post-traumatic stress disorder symptoms in adulthood? J. Psychiatr. Res. 2017, 84, 119–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaplow, J.B.; Widom, C.S. Age of onset of child maltreatment predicts long-term mental health outcomes. J. Abnorm. Psychol. 2007, 116, 176–187. [Google Scholar] [CrossRef] [PubMed]
- Mueller-Pfeiffer, C.; Moergeli, H.; Schumacher, S.; Martin-Soelch, C.; Wirtz, G.; Fuhrhans, C.; Hindermann, E.; Rufer, M. Characteristics of child maltreatment and their relation to dissociation, posttraumatic stress symptoms, and depression in adult psychiatric patients. J. Nerv. Ment. Dis. 2013, 201, 471–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable | n (%) | |
|---|---|---|
| Sex at birth | Female | 299 (58.3) |
| Male | 214 (41.7) | |
| Age a | 70–79 yrs | 283 (55.2) |
| (mean 79 yrs) | 80–89 yrs | 201 (39.2) |
| 90–99 yrs | 29 (5.7) | |
| Sexual orientation | Heterosexual | 475 (92.6) |
| Non-heterosexual b | 38 (7.4) | |
| Living situation | Community-dwelling | 461 (89.8) |
| Assisted-living facility | 25 (4.9) | |
| Nursing home | 27 (5.3) | |
| Education level | No/lower education c | 353 (68.8) |
| Higher education | 160 (31.2) | |
| Financial status d | Easy | 377 (73.5) |
| Difficult | 134 (26.1) | |
| Social support e | Low | 246 (48.3) |
| High | 265 (51.7) | |
| Perceived health status | No disability/chronical illness | 278 (54.2) |
| Disability/chronical illness | 235 (45.8) | |
| Care dependency | Yes | 238 (46.4) |
| No | 275 (53.6) | |
| Resilience f | Low | 136 (26.5) |
| Normal | 319 (62.2) | |
| High | 58 (11.3) | |
| Sexual victimisation | Lifetime | 227 (44.2) |
| Past 12 months | 43 (8.4) | |
| Item | Scale | Outcome | N Total | % Total | % SV | Chi-Square Test |
|---|---|---|---|---|---|---|
| Depression | PHQ-9 | No | 371 | 72.5 | 41.2 | p = 0.047 |
| (n = 512) | (α = 0.737) | Mild | 102 | 19.9 | 47.1 | |
| Moderate | 26 | 5.1 | 65.4 | |||
| Moderately severe/Severe | 13 | 2.5 | 61.5 | |||
| Anxiety | GAD-7 | No | 382 | 74.5 | 40.8 | p = 0.043 |
| (n = 513) | (α = 0.827) | Mild | 90 | 17.5 | 51.1 | |
| Moderate | 23 | 4.5 | 60.9 | |||
| Severe | 18 | 3.5 | 61.1 | |||
| PTSD | PC-PTSD-5 | Yes | 29 | 5.7 | 65.5 | p = 0.018 |
| (n = 512) | (α = 0.572) | |||||
| Suicide attempts | NA | Lifetime | 27 | 5.3 | 51.9 | p = 0.414 |
| (n = 513) | Past 12 months | 8 | 1.6 | 37.5 | p = 1.00 | |
| Self-harm | NA | Lifetime | 11 | 2.1 | 36.4 | p = 0.762 |
| (n = 512) | Past 12 months | 7 | 1.4 | 28.6 | p = 0.471 |
| Depression (PHQ-9) | Anxiety (GAD-7) | PTSD (PC-PTSD-5) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coeff. | 95% CI | p-Value | Coeff. | 95% CI | p-Value | Coeff. | 95% CI | p-Value | |
| Main effects | |||||||||
| Lifetime SV | 1.074 | 0.451, 1.697 | 0.001 | 1.173 | 0.504, 1.841 | 0.001 | 0.284 | 0.129, 0.439 | <0.001 |
| Education level | -- | -- | -- | −0.880 | −1.615, −145 | 0.019 | 0.039 | −0.129, 0.208 | 0.647 |
| Financial status | 1.248 | 0.544, 1.953 | 0.001 | 1.287 | 0.518, 2.056 | 0.001 | 0.211 | 0.034, 0.388 | 0.019 |
| Perceived health status | 1.988 | 1.324, 2.651 | <0.001 | 1.345 | 0.633, 2.057 | <0.001 | 0.225 | 0.069, 0.380 | 0.005 |
| Care dependency | 1.210 | 0.548, 1.872 | <0.001 | 1.259 | 0.544, 1.974 | 0.001 | -- | -- | -- |
| Social support | 0.823 | 0.201, 1.445 | 0.010 | 0.990 | 0.320, 1.659 | 0.004 | -- | -- | -- |
| Resilience | -- | -- | -- | 0.751 | 0.075, 1.426 | 0.029 | -- | -- | -- |
| Cross-product terms | |||||||||
| Lifetime SV × education level | -- | -- | -- | -- | -- | -- | 0.318 | −0.017, 0.652 | 0.062 |
| Lifetime SV × perceived health status | -- | -- | -- | -- | -- | -- | 0.310 | 0.000, 0.620 | 0.050 |
| Interaction effects | |||||||||
| Lifetime SV by education level | -- | -- | -- | -- | -- | -- | |||
| Association in higher education | -- | -- | -- | -- | -- | -- | 0.101 | −0.178, 0.380 | 0.477 |
| Association in no/lower education | -- | -- | -- | -- | -- | -- | 0.356 | 0.165, 0.547 | <0.001 |
| Lifetime SV by perceived health status | -- | -- | -- | -- | -- | -- | |||
| Association in no chronic illness/disability | -- | -- | -- | -- | -- | -- | 0.154 | −0.026, 0.334 | 0.093 |
| Association in chronic illness/disability | -- | -- | -- | -- | -- | -- | 0.422 | 0.155, 0.689 | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nobels, A.; Lemmens, G.; Thibau, L.; Beaulieu, M.; Vandeviver, C.; Keygnaert, I. “Time Does Not Heal All Wounds”: Sexual Victimisation Is Associated with Depression, Anxiety, and PTSD in Old Age. Int. J. Environ. Res. Public Health 2022, 19, 2803. https://doi.org/10.3390/ijerph19052803
Nobels A, Lemmens G, Thibau L, Beaulieu M, Vandeviver C, Keygnaert I. “Time Does Not Heal All Wounds”: Sexual Victimisation Is Associated with Depression, Anxiety, and PTSD in Old Age. International Journal of Environmental Research and Public Health. 2022; 19(5):2803. https://doi.org/10.3390/ijerph19052803
Chicago/Turabian StyleNobels, Anne, Gilbert Lemmens, Lisa Thibau, Marie Beaulieu, Christophe Vandeviver, and Ines Keygnaert. 2022. "“Time Does Not Heal All Wounds”: Sexual Victimisation Is Associated with Depression, Anxiety, and PTSD in Old Age" International Journal of Environmental Research and Public Health 19, no. 5: 2803. https://doi.org/10.3390/ijerph19052803
APA StyleNobels, A., Lemmens, G., Thibau, L., Beaulieu, M., Vandeviver, C., & Keygnaert, I. (2022). “Time Does Not Heal All Wounds”: Sexual Victimisation Is Associated with Depression, Anxiety, and PTSD in Old Age. International Journal of Environmental Research and Public Health, 19(5), 2803. https://doi.org/10.3390/ijerph19052803







