Effects of Balance Training Using a Virtual Reality Program in Hemiplegic Patients
Abstract
1. Introduction
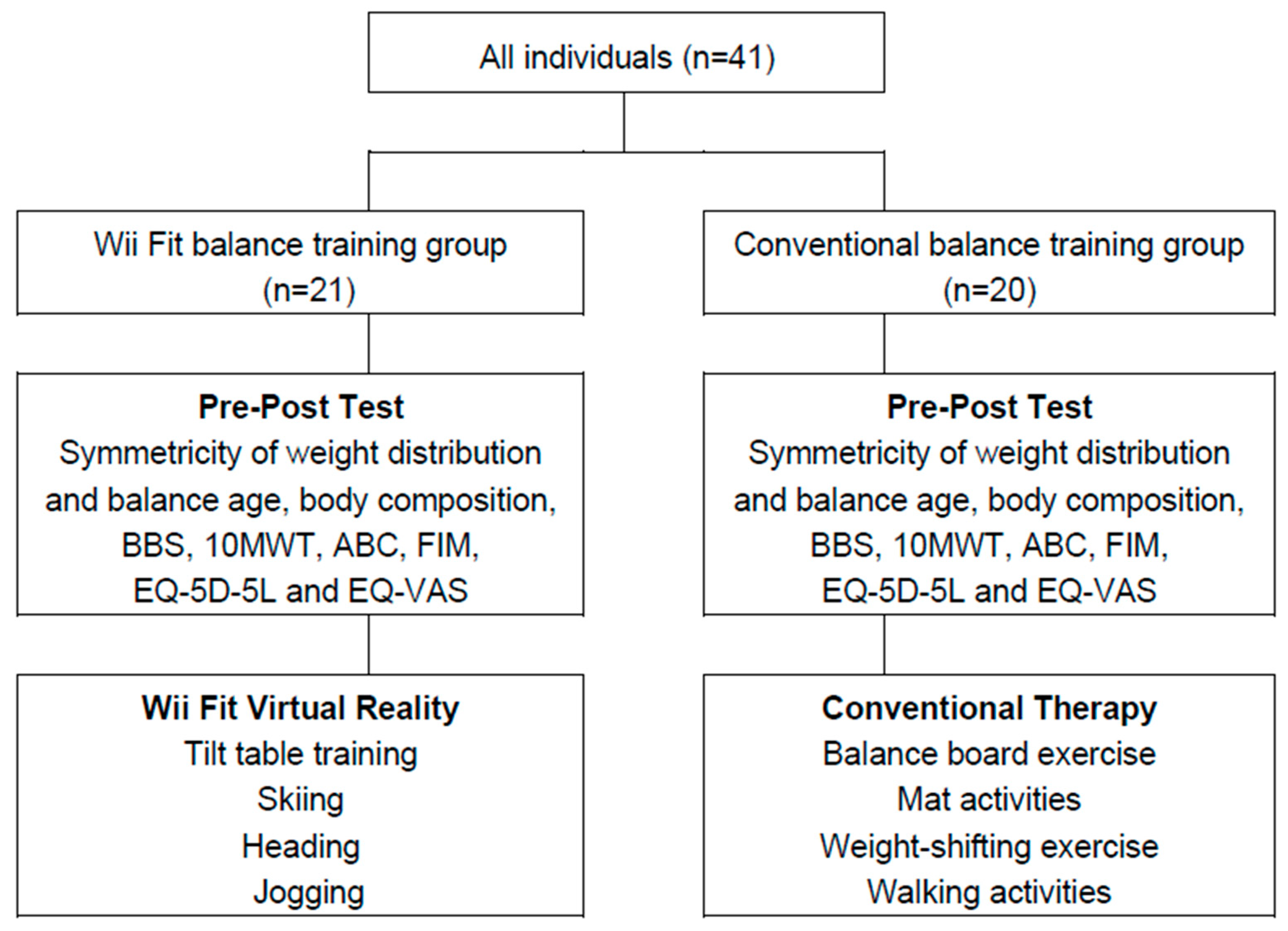
2. Materials and Methods
2.1. Patients
2.2. Procedures
2.3. Outcome Measures
2.3.1. Symmetricity of Weight Distribution and Balance Age
2.3.2. Body Composition
2.3.3. Berg Balance Scale
2.3.4. Walking Speed
2.3.5. Balance Confidence
2.3.6. Activities of Daily Living
2.3.7. Quality of Life
2.4. Statistical Analyses
3. Result
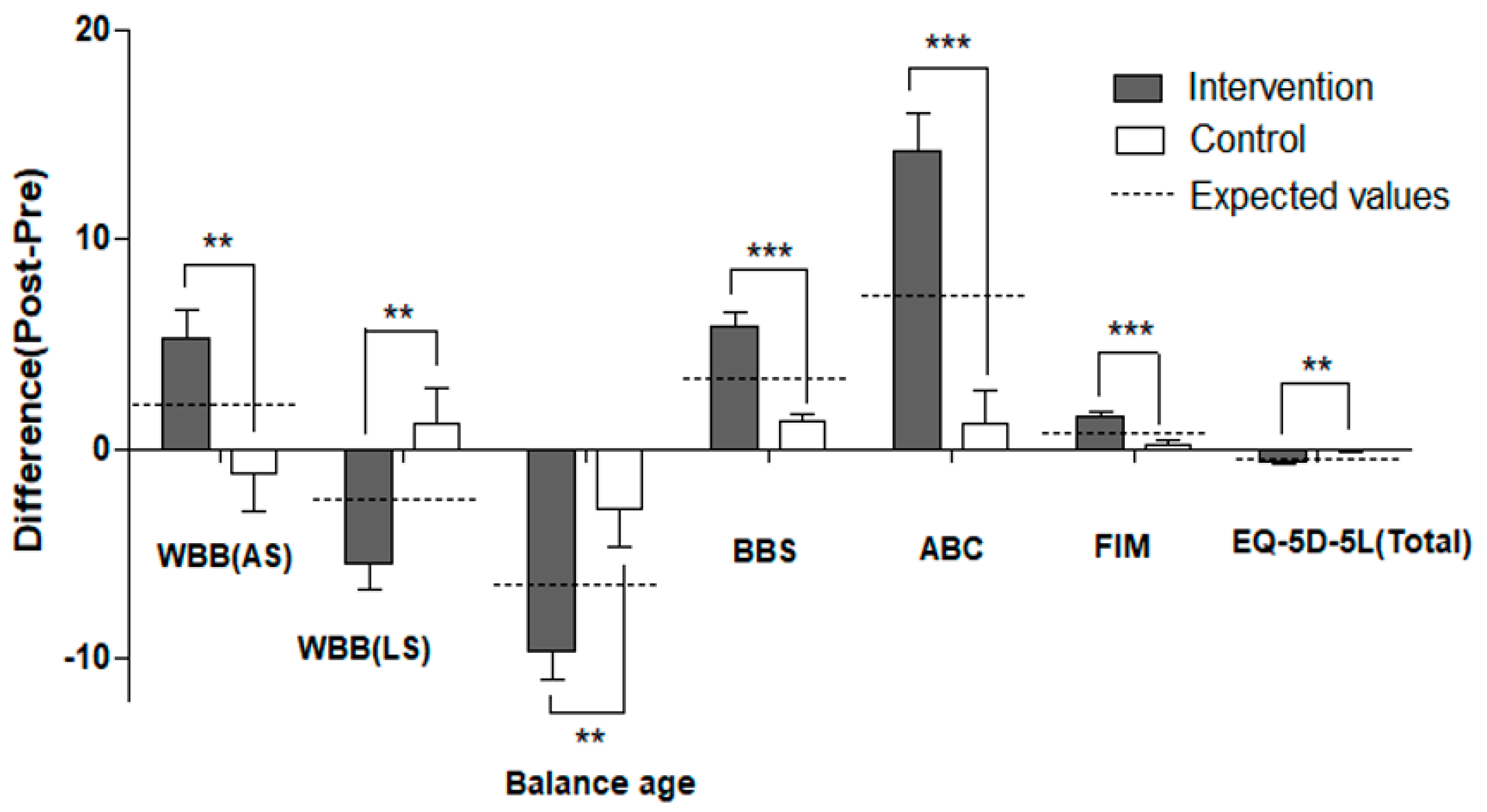
3.1. Symmetricity of Weight Distribution and Balance Age
3.2. Balance and Functional Outcomes
3.3. Body Composition
3.4. Quality of Life
3.5. Factors Affecting Health-Related Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheng, P.T.; Wu, S.H.; Liaw, M.Y.; Wong, A.M.; Tang, F.T. Symmetrical body-weight distribution training in stroke patients and its effect on fall prevention. Arch. Phys. Med. Rehabil. 2001, 82, 1650–1654. [Google Scholar] [CrossRef] [PubMed]
- Gil-Gomez, J.A.; Llorens, R.; Alcaniz, M.; Colomer, C. Effectiveness of a wii balance board-based system (ebavir) for balance rehabilitation: A pilot randomized clinical trial in patients with acquired brain injury. J. Neuroeng. Rehabil. 2011, 8, 30. [Google Scholar] [CrossRef] [PubMed]
- Kushner, D.S.; Amidei, C. Rehabilitation of motor dysfunction in primary brain tumor patients. Neurooncol. Pract. 2015, 2, 185–191. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Salbach, N.M.; Mayo, N.E.; Robichaud-Ekstrand, S.; Hanley, J.A.; Richards, C.L.; Wood-Dauphinee, S. Balance self-efficacy and its relevance to physical function and perceived health status after stroke. Arch. Phys. Med. Rehabil. 2006, 87, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Tanne, D.; Medalie, J.H.; Goldbourt, U. Body fat distribution and long-term risk of stroke mortality. Stroke 2005, 36, 1021–1025. [Google Scholar] [CrossRef]
- Gilliat-Wimberly, M.; Manore, M.M.; Woolf, K.; Swan, P.D.; Carroll, S.S. Effects of habitual physical activity on the resting metabolic rates and body compositions of women aged 35 to 50 years. J. Am. Diet Assoc. 2001, 101, 1181–1188. [Google Scholar] [CrossRef]
- St-Onge, M.P.; Gallagher, D. Body composition changes with aging: The cause or the result of alterations in metabolic rate and macronutrient oxidation? Nutrition 2010, 26, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Serra, M.C.; Hafer-Macko, C.E.; Ryan, A.S. Reduced resting metabolic rate in adults with hemiparetic chronic stroke. J. Neurol. Neurophysiol. 2015, 6, 1000341. [Google Scholar] [CrossRef]
- MacDougall, N.J.; Amarasinghe, S.; Muir, K.W. Secondary prevention of stroke. Expert Rev. Cardiovasc. Ther. 2009, 7, 1103–1115. [Google Scholar] [CrossRef]
- Dean, C.M.; Richards, C.L.; Malouin, F. Task-related circuit training improves performance of locomotor tasks in chronic stroke: A randomized, controlled pilot trial. Arch. Phys. Med. Rehabil. 2000, 81, 409–417. [Google Scholar] [CrossRef]
- Goble, D.J.; Cone, B.L.; Fling, B.W. Using the wii fit as a tool for balance assessment and neurorehabilitation: The first half decade of “wii-search”. J. Neuroeng. Rehabil. 2014, 11, 12. [Google Scholar] [CrossRef] [PubMed]
- Morone, G.; Tramontano, M.; Iosa, M.; Shofany, J.; Iemma, A.; Musicco, M.; Paolucci, S.; Caltagirone, C. The efficacy of balance training with video game-based therapy in subacute stroke patients: A randomized controlled trial. Biomed. Res. Int. 2014, 2014, 580861. [Google Scholar] [CrossRef] [PubMed]
- Saywell, N.; Taylor, N.; Rodgers, E.; Skinner, L.; Boocock, M. Play-based interventions improve physical function for people with adult-acquired brain injury: A systematic review and meta-analysis of randomised controlled trials. Clin. Rehabil. 2017, 31, 145–157. [Google Scholar] [CrossRef]
- Fang, Q.; Ghanouni, P.; Anderson, S.E.; Touchett, H.; Shirley, R.; Fang, F.; Fang, C. Effects of exergaming on balance of healthy older adults: A systematic review and meta-analysis of randomized controlled trials. Games Health J. 2020, 9, 11–23. [Google Scholar] [CrossRef]
- Zhang, B.; Li, D.; Liu, Y.; Wang, J.; Xiao, Q. Virtual reality for limb motor function, balance, gait, cognition and daily function of stroke patients: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 77, 3255–3273. [Google Scholar] [CrossRef] [PubMed]
- de Rooij, I.J.; van de Port, I.G.; Meijer, J.G. Effect of virtual reality training on balance and gait ability in patients with stroke: Systematic review and meta-analysis. Phys. Ther. 2016, 96, 1905–1918. [Google Scholar] [CrossRef]
- Garcia-Munoz, C.; Casuso-Holgado, M.J. Effectiveness of wii fit balance board in comparison with other interventions for post-stroke balance rehabilitation. Systematic review and meta-analysis. Rev. Neurol. 2019, 69, 271–279. [Google Scholar] [PubMed]
- Oliveira, T.D.P.; Miranda, C.S.; Gouvêa, J.X.M.D.; Perez, D.B.; Marques, A.P.; Piemonte, M.E.P. Improvement of balance and gait in patients with stroke after training based on nintendo wii fit™ games: Randomized controlled trial. Physiotherapy 2015, 101, e1207. [Google Scholar] [CrossRef][Green Version]
- da Silva Ribeiro, N.M.; Ferraz, D.D.; Pedreira, E.; Pinheiro, I.; da Silva Pinto, A.C.; Neto, M.G.; Dos Santos, L.R.; Pozzato, M.G.; Pinho, R.S.; Masruha, M.R. Virtual rehabilitation via nintendo wii(r) and conventional physical therapy effectively treat post-stroke hemiparetic patients. Top. Stroke Rehabil. 2015, 22, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Unibaso-Markaida, I.; Iraurgi, I. Effect of the wii sports resort on mobility and health-related quality of life in moderate stroke. Behav. Neurol. 2021, 2021, 6635298. [Google Scholar] [CrossRef] [PubMed]
- Aramaki, A.L.; Sampaio, R.F.; Reis, A.C.S.; Cavalcanti, A.; Dutra, F. Virtual reality in the rehabilitation of patients with stroke: An integrative review. Arq. Neuropsiquiatr. 2019, 77, 268–278. [Google Scholar] [CrossRef]
- Dominguez-Tellez, P.; Moral-Munoz, J.A.; Salazar, A.; Casado-Fernandez, E.; Lucena-Anton, D. Game-based virtual reality interventions to improve upper limb motor function and quality of life after stroke: Systematic review and meta-analysis. Games Health J. 2020, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Cano-Manas, M.J.; Collado-Vazquez, S.; Rodriguez Hernandez, J.; Munoz Villena, A.J.; Cano-de-la-Cuerda, R. Effects of video-game based therapy on balance, postural control, functionality, and quality of life of patients with subacute stroke: A randomized controlled trial. J. Healthc. Eng. 2020, 2020, 5480315. [Google Scholar] [CrossRef] [PubMed]
- Manuli, A.; Maggio, M.G.; Latella, D.; Cannavò, A.; Balletta, T.; De Luca, R.; Naro, A.; Calabrò, R.S. Can robotic gait rehabilitation plus virtual reality affect cognitive and behavioural outcomes in patients with chronic stroke? A randomized controlled trial involving three different protocols. J. Stroke Cerebrovasc. Dis. 2020, 29, 104994. [Google Scholar] [CrossRef] [PubMed]
- Corbetta, D.; Imeri, F.; Gatti, R. Rehabilitation that incorporates virtual reality is more effective than standard rehabilitation for improving walking speed, balance and mobility after stroke: A systematic review. J. Physiother. 2015, 61, 117–124. [Google Scholar] [CrossRef]
- Karasu, A.U.; Batur, E.B.; Karataş, G.K. Effectiveness of wii-based rehabilitation in stroke: A randomized controlled study. J. Rehabil. Med. 2018, 50, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Yatar, G.I.; Yildirim, S.A. Wii fit balance training or progressive balance training in patients with chronic stroke: A randomised controlled trial. J. Phys. Ther. Sci. 2015, 27, 1145–1151. [Google Scholar] [CrossRef] [PubMed]
- Tarakci, D.; Ersoz Huseyinsinoglu, B.; Tarakci, E.; Razak Ozdincler, A. Effects of nintendo wii-fit® video games on balance in children with mild cerebral palsy. Pediatr. Int. 2016, 58, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- Bower, K.J.; McGinley, J.L.; Miller, K.J.; Clark, R.A. Instrumented static and dynamic balance assessment after stroke using wii balance boards: Reliability and association with clinical tests. PLoS ONE 2014, 9, e115282. [Google Scholar] [CrossRef]
- Wang, J.; Thornton, J.C.; Kolesnik, S.; Pierson, R.N., Jr. Anthropometry in body composition. An overview. Ann. N. Y. Acad. Sci. 2000, 904, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.; Wood-Dauphinee, S.; Williams, J.I. The balance scale: Reliability assessment with elderly residents and patients with an acute stroke. Scand. J. Rehabil. Med. 1995, 27, 27–36. [Google Scholar]
- Wirz, M.; Müller, R.; Bastiaenen, C. Falls in persons with spinal cord injury: Validity and reliability of the berg balance scale. Neurorehabil. Neural Repair. 2010, 24, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Andersen, C.W.; Kristensen, M.T. Performance stability and interrater reliability of culturally adapted 10-meter walking test for danes with neurological disorders. J. Stroke Cerebrovasc. Dis. 2019, 28, 2459–2467. [Google Scholar] [CrossRef]
- Cleland, B.T.; Arshad, H.; Madhavan, S. Concurrent validity of the gaitrite electronic walkway and the 10-m walk test for measurement of walking speed after stroke. Gait Posture 2019, 68, 458–460. [Google Scholar] [CrossRef]
- Botner, E.M.; Miller, W.C.; Eng, J.J. Measurement properties of the activities-specific balance confidence scale among individuals with stroke. Disabil. Rehabil. 2005, 27, 156–163. [Google Scholar] [CrossRef]
- Pedersen, A.R.; Stubbs, P.W.; Nielsen, J.F. Reducing redundant testing using the functional independence measure and early functional abilities scale during rehabilitation in patients with brain injury. Brain Inj. 2018, 32, 1090–1095. [Google Scholar] [CrossRef] [PubMed]
- Gosman-Hedström, G.; Svensson, E. Parallel reliability of the functional independence measure and the barthel adl index. Disabil. Rehabil. 2000, 22, 702–715. [Google Scholar] [CrossRef] [PubMed]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of eq-5d (eq-5d-5l). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Golicki, D.; Niewada, M.; Buczek, J.; Karlińska, A.; Kobayashi, A.; Janssen, M.F.; Pickard, A.S. Validity of eq-5d-5l in stroke. Qual. Life Res. 2015, 24, 845–850. [Google Scholar] [CrossRef]
- Omiyale, O.; Crowell, C.R.; Madhavan, S. Effect of wii-based balance training on corticomotor excitability post stroke. J. Mot. Behav. 2015, 47, 190–200. [Google Scholar] [CrossRef]
- Dos Santos, L.R.; Carregosa, A.A.; Masruha, M.R.; Dos Santos, P.A.; Da Silveira Coelho, M.L.; Ferraz, D.D.; Da Silva Ribeiro, N.M. The use of nintendo wii in the rehabilitation of poststroke patients: A systematic review. J. Stroke Cerebrovasc. Dis. 2015, 24, 2298–2305. [Google Scholar] [CrossRef] [PubMed]
- Bacon, N.; Farnworth, L.; Boyd, R. The use of the wii fit in forensic mental health: Exercise for people at risk of obesity. Br. J. Occup. Ther. 2012, 75, 61–68. [Google Scholar] [CrossRef]
| Intervention Group (n = 21) | Control Group (n = 20) | p | |
|---|---|---|---|
| Age, years | 46.52 ± 14.15 † | 47.00 ± 13.82 | 0.252 |
| Gender, n(%) | 0.087 | ||
| Male | 7 (33.3) | 12 (60.0) | |
| Female | 14 (66.7) | 8 (40.0) | |
| Diagnosis, n (%) | 0.511 | ||
| Stroke | 15 (71.4) | 14 (70.0) | |
| Traumatic brain injury | 2 (9.5) | 4 (20.0) | |
| Tumor | 4 (19.1) | 2 (10.0) | |
| Onset duration, years | 9.16 ± 7.92 | 6.11 ± 4.60 | 0.452 |
| Affected side, n (%) | 0.867 | ||
| Rt. side | 11 (52.3) | 11 (55.0) | |
| Lt. side | 10 (47.7) | 9 (45.0) |
| Variables (Unit) Group | Pre | Post | pa | Difference | pb |
|---|---|---|---|---|---|
| Affected side (%) | |||||
| Intervention | 44.83 ± 7.25 † | 50.25 ± 4.36 | 0.001 ** | 5.31 ± 1.33 § | 0.004 ** |
| Control | 51.26 ± 7.67 | 50.05 ± 5.24 | 0.492 | −1.21 ± 1.72 | |
| Less affected side (%) | |||||
| Intervention | 55.17 ± 7.25 | 49.75 ± 4.36 | 0.001 ** | −5.42 ± 1.33 | 0.004 ** |
| Control | 48.75 ± 7.67 | 49.95 ± 5.24 | 0.492 | 1.21 ± 1.72 | |
| Balance age (years) | |||||
| Intervention | 59.14 ± 12.95 | 49.43 ± 11.50 | 0.000 *** | −9.71 ± 1.32 | 0.003 ** |
| Control | 58.20 ± 15.04 | 55.15 ± 16.17 | 0.108 | −2.90 ± 1.75 |
| Variables (Unit) Group | Pre | Post | pa | Difference | pb | |
|---|---|---|---|---|---|---|
| BBS (score) | ||||||
| Intervention | 42.10 ± 9.36 † | 48.10 ± 7.18 | 0.000 *** | 5.90 ± 0.69 § | 0.000 *** | |
| Control | 47.00 ± 8.52 | 48.35 ± 7.71 | 0.001** | 1.30 ± 0.33 | ||
| ABC (score) | ||||||
| Intervention | 55.95 ± 22.74 | 69.76 ± 20.98 | 0.000 *** | 14.19 ± 1.82 | 0.000 *** | |
| Control | 64.99 ± 29.82 | 66.10 ± 27.87 | 0.501 | 1.16 ± 1.64 | ||
| FIM (score) | ||||||
| Intervention | 30.14 ± 2.35 | 31.67 ± 2.80 | 0.000 *** | 1.52 ± 0.26 | 0.000 *** | |
| Control | 30.90 ± 3.34 | 31.15 ± 3.01 | 0.096 | 0.25 ± 0.14 | ||
| Walking speed (m/s) | Regular speed | |||||
| Intervention | 1.54 ± 0.50 | 1.29 ± 0.41 | 0.000 *** | −0.22 ± 0.05 | 0.091 | |
| Control | 1.30 ± 0.51 | 1.25 ± 0.54 | 0.390 | −0.08 ± 0.07 | ||
| Fast speed | ||||||
| Intervention | 1.21 ± 0.50 | 1.06 ± 0.40 | 0.003 ** | −0.14 ± 0.05 | 0.144 | |
| Control | 1.03 ± 0.38 | 0.96 ± 0.32 | 0.219 | 0.05 ± 0.12 | ||
| Variable (Unit) Group | Pre | Post | pa | Difference | pb | |
|---|---|---|---|---|---|---|
| Body composition | BMI (kg/m2) | |||||
| Intervention | 23.32 ± 2.89 † | 23.44 ± 3.29 | 0.666 | 0.12 ± 0.27 § | 0.842 | |
| Control | 24.89 ± 3.39 | 24.83 ± 3.58 | 0.849 | 0.04 ± 0.29 | ||
| Weight (kg) | ||||||
| Intervention | 64.73 ± 11.65 | 64.30 ± 12.41 | 0.473 | −0.42 ± 0.59 | 0.169 | |
| Control | 69.79 ± 14.34 | 70.51 ± 14.95 | 0.213 | 0.72 ± 0.56 | ||
| Body fat rate (%) | ||||||
| Intervention | 33.22 ± 7.60 | 29.98 ± 8.06 | 0.034 * | −3.30 ± 1.41 | 0.109 | |
| Control | 29.99 ± 7.74 | 29.55 ± 7.32 | 0.571 | −0.70 ± 0.71 | ||
| Body fat amount (kg) | ||||||
| Intervention | 21.09 ± 5.39 | 18.40 ± 4.53 | 0.021 * | −2.69 ± 1.08 | 0.021 * | |
| Control | 21.04 ± 6.66 | 21.39 ± 7.11 | 0.600 | 0.35 ± 0.65 | ||
| Muscle mass (kg) | ||||||
| Intervention | 23.37 ± 6.30 | 24.99 ± 8.17 | 0.039 * | 1.61 ± 0.73 | 0.122 | |
| Control | 26.83 ± 6.82 | 27.25 ± 6.76 | 0.133 | 0.37 ± 0.27 | ||
| Basic metabolic rate (%) | ||||||
| Intervention | 1303.29 ± 232.26 | 1374.24 ± 256.43 | 0.017 * | 70.95 ± 27.18 | 0.038 * | |
| Control | 1438.25 ± 268.22 | 1437.50 ± 240.49 | 0.969 | −0.75 ± 18.91 | ||
| Mid-thigh circumference | Affected side (cm) | |||||
| Intervention | 52.64 ± 4.91 † | 54.33 ± 4.41 | 0.027 * | 1.71 ± 0.70 § | 0.658 | |
| Control | 49.95 ± 8.94 | 51.25 ± 9.31 | 0.021 * | 1.33 ± 0.51 | ||
| Less affected side (cm) | ||||||
| Intervention | 54.88 ± 4.34 | 56.48 ± 4.56 | 0.065 | 1.60 ± 0.82 | 0.249 | |
| Control | 52.65 ± 7.82 | 53.18 ± 8.24 | 0.305 | 0.48 ± 0.50 | ||
| Variables (Unit) Group | Pre | Post | pa | Difference | pb | |
|---|---|---|---|---|---|---|
| EQ-5D-5L | Mobility (score) | |||||
| Intervention | 2.33 ± 0.91 † | 1.81 ± 0.87 | 0.001 ** | −0.43 ± 0.18 § | 0.051 | |
| Control | 2.20 ± 0.95 | 2.15 ± 0.93 | 0.330 | −0.05 ± 0.05 | ||
| Self-care (score) | ||||||
| Intervention | 1.95 ± 0.80 | 1.95 ± 0.80 | — | — | — | |
| Control | 1.95 ± 0.69 | 1.95 ± 0.69 | — | — | ||
| Activity (score) | ||||||
| Intervention | 2.33 ± 0.73 | 2.33 ± 0.73 | — | — | — | |
| Control | 2.20 ± 0.62 | 2.20 ± 0.62 | — | — | ||
| Pain (score) | ||||||
| Intervention | 2.10 ± 0.70 | 2.10 ± 0.70 | — | — | — | |
| Control | 2.20 ± 0.70 | 2.20 ± 0.70 | — | — | ||
| Anxiety (score) | ||||||
| Intervention | 1.95 ± 0.67 | 1.90 ± 0.62 | 0.329 | −0.05 ± 0.05 | 0.329 | |
| Control | 1.95 ± 0.76 | 1.95 ± 0.76 | — | — | ||
| Total score | ||||||
| Intervention | 10.67 ± 2.33 | 10.10 ± 2.34 | 0.001 ** | −0.57 ± 0.15 | 0.003 ** | |
| Control | 10.50 ± 2.98 | 10.45 ± 2.96 | 0.330 | −0.05 ± 0.05 | ||
| EQ-VAS (score) | Intervention | 76.24 ± 14.07 † | 80.90 ± 10.30 | 0.003 ** | 2.76 ± 1.62 § | 0.592 |
| Control | 75.45 ± 16.89 | 77.30 ± 14.86 | 0.110 | 1.70 ± 1.08 | ||
| Variable (Reference) | Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| β | p | Odds Ratio | 95% CI | β | p | Odds Ratio | 95% CI | |
| Gender (female) | 0.105 | 0.479 | 2.651 | −4.878–10.180 | 0.202 | 0.203 | 5.078 | −2.885–13.041 |
| Age | −0.030 | 0.870 | −0.027 | −0.364–0.309 | 0.113 | 0.545 | 0.104 | −0.242–0.449 |
| Diagnosis (tumor) | ||||||||
| Stroke | −0.650 | 0.002 ** | −17.927 | −28.828–−7.026 | −0.448 | 0.021 * | −13.457 | −24.775–−2.139 |
| TBI | −0.431 | 0.046 * | −15.281 | −30.251–−0.310 | −0.377 | 0.074 | −13.382 | −28.150–1.387 |
| Onset duration | −0.217 | 0.150 | −0.417 | −0.991–0.158 | −0.185 | 0.202 | −0.355 | −0.910–0.200 |
| BBS | 0.307 | 0.070 | 0.530 | −0.046–1.107 | ||||
| ABC | 0.411 | 0.017 * | 0.214 | 0.040–0.388 | ||||
| FIM | 0.273 | 0.100 | 1.205 | −0.243–2.652 | ||||
| R2 | 0.279 | 0.396 | ||||||
| Adjusted R2 | 0.176 | 0.245 | ||||||
| F(p) | 2.771 (0.036 *) | 2.624 (0.025 *) | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, J.-A.; Shin, Y.-K.; Kim, D.-J.; Cho, S.-R. Effects of Balance Training Using a Virtual Reality Program in Hemiplegic Patients. Int. J. Environ. Res. Public Health 2022, 19, 2805. https://doi.org/10.3390/ijerph19052805
Kwon J-A, Shin Y-K, Kim D-J, Cho S-R. Effects of Balance Training Using a Virtual Reality Program in Hemiplegic Patients. International Journal of Environmental Research and Public Health. 2022; 19(5):2805. https://doi.org/10.3390/ijerph19052805
Chicago/Turabian StyleKwon, Jung-Ah, Yoon-Kyum Shin, Deok-Ju Kim, and Sung-Rae Cho. 2022. "Effects of Balance Training Using a Virtual Reality Program in Hemiplegic Patients" International Journal of Environmental Research and Public Health 19, no. 5: 2805. https://doi.org/10.3390/ijerph19052805
APA StyleKwon, J.-A., Shin, Y.-K., Kim, D.-J., & Cho, S.-R. (2022). Effects of Balance Training Using a Virtual Reality Program in Hemiplegic Patients. International Journal of Environmental Research and Public Health, 19(5), 2805. https://doi.org/10.3390/ijerph19052805







