Abstract
To determine the effectiveness of pelvic floor muscle training (PFMT) with or without biofeedback or electrostimulation in reducing urinary incontinence and pelvic floor muscle con-traction in non-pregnant women with urinary incontinence. Methods: The following electronic databases were searched: PubMed, Cochrane Central, ClinicalTrials.gov, EU Clinical Trials Register, and sources from NICE, FDA, EMA, and SMC (articles only in English, 2000–2021). Search terms were: urinary incontinence, pelvic floor muscle training or exercises, biofeedback, electrostimulation. We used the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) for this systematic review. Relevant articles were selected, data were extracted, and quality was assessed. Data were extracted in predesigned form, followed by narrative synthesis. Results: Following the search, 15 RCTs were retrieved using the strict inclusion and exclusion criteria, assessing 2441 non-pregnant women with urinary incontinence. Of the 15 studies, 7 were low risk, 5 were medium risk, and 3 were high-risk studies. Of the 2441 patients, 970 were in PFMT, 69 were in extracorporeal magnetic innervation (ExMi) or with PFMT + BF, 30 were in electrostimulation (ES), 21 were in whole body vibration training (WBVT), 23 were in pelvic floor muscle + abdominal muscle therapy (PFM + AMT), 326 were in PFMT + biofeedback, 93 were in vaginal cones (VC), 362 were in PFMT + education, 318 were in education, and 229 were in control groups. The most often measures employed were pad tests, bladder diary, and questionnaire on the quality of life. Stress, urge and mixed urinary incontinence were studied. In all RCT, PFMT significantly reduced urinary incontinence, essentially SIU and MUI, when compared with the control group before and after treatment. Overall, out of 997 PFMT or PFMT + education patients, 504 patients (50.5%) showed improvement in urinary incontinence, and 218 became continent (21.8%) (negative pad test). In total, 62% of patients significantly reduced their urinary incontinence or cured it and improved their pelvic floor muscle contraction. All other physiotherapist techniques also significantly reduced urinary leakages, e.g., vaginal cones, biofeedback, ExMI, and WBVT when compared with the control group. There were no significant differences between these methods in reducing the severity of urinary incontinence. Conclusion: PFMT alone or with bio-feedback or electrostimulation was effective in reducing urinary incontinence and improving pelvic floor muscle contraction. PFMT when compared with other interventions such as bio-feedback, VC, and WBVT did not show significant differences but was superior to the control group. RCT studies with similar parameters used for measuring the outcomes need to be included.
1. Introduction
Urinary incontinence (UI) is defined as involuntary leakage of urine through the urethra by the International Continence Society (ICS) [1]. It is considered to be a health, social, and hygienic concern. UI affects 6–10% of the population [1]. UI maybe divided into three subtypes: stress urinary incontinence (SUI), urge urinary incontinence (UUI), and mixed urinary incontinence (MUI) based on behavioral symptoms and pathophysiology [1,2]. Stress urinary incontinence (SIU) is the common type of UI among women. SUI occurs during efforts such as sneezing, coughing, or exertion. It is found in either pure or mixed form in one-third of women [3]. SUI is caused due to a lack of strength in the urethral sphincter muscles, pelvic floor muscles, connective tissues, and fasciae [4].
Urge incontinence is defined by urinary leakage following a sudden and strong desire to urinate [3]. The combination of SIU and UUI is referred to as mixed urinary incontinence. Around 25–45% of all women suffer from involuntary urine loss at some stage in their lives, thus making UI one of the most frequent complaints in this population [5]. Non-pregnant or prepartum women were less likely to suffer from UI compared with postpartum women. However, in the last few decades, there has been an increase in the number of women experiencing incontinence among non-pregnant or prepartum women. Currently, the importance of prevention and treatment of UI has grown. Hence, increased attention has been given to conservative treatments for UI.
Conservative management of UI has been recognized as the first-line management, which includes physical therapies, behavior modification, and pharmacological intervention, specifically for SUI [2]. Some examples of conservative treatments that are used in the management of UI are physical therapies and pelvic floor muscle training (PFMT) alone or combined with other treatments—for example, electrical stimulation, biofeedback, and vaginal cones. These are the standard management procedures [3]. Pelvic floor muscle training (PFMT) is considered as the first-line treatment, as suggested by the International Continence Society (ICS), and it has been proven to guarantee results for UI. Guided PFMT also improves adherence positively and promotes self-efficacy behavior among the participants [4]. PFMT provides support to the pelvic organs and helps in the closure of the urethral sphincter muscles, thus resulting in improvement in incontinence. Hence, it is prescribed for increasing strength, endurance, and muscle coordination [6,7]. Previously, many authors have performed various reviews regarding the implications, causes, and treatments for UI, but no systematic review has been performed in measuring the efficacy of PFMT among non-pregnant women.
This review focused on analyzing the efficacy of pelvic floor muscle training in the treatment of UI and its effect on the improvement in muscle strength and endurance among non-pregnant women.
2. Material and Method
This systematic review was carried out according to the pre-specified PRISMA protocol that was implemented before initiation of the study. The protocol was followed throughout the process of study selection, data extraction, quality assessment, and data synthesis.
2.1. Search Strategy
The following databases (PubMed, Cochrane Central, ClinicalTrials.gov, EU Clinical Trials Register), grey literature sources (NICE, FDA, EMA, SMC), and snowballing search were conducted by using Boolean operators and limiting the search strategy to only articles published in English from the 1 January 2000 to the 1 March 2021. The search strategy used was as follows: (pelvic floor muscle therapy) OR (pelvic floor muscle physiotherapy) OR (pelvic floor muscle exercise) OR (pelvic muscle physiotherapy) OR (pelvic muscle therapy) OR (pelvic muscle exercise) OR (pelvic muscle physical therapy) OR (pelvic floor muscle physical therapy) OR (pelvic floor muscle training) OR (PFMT) OR (pelvic muscle training) OR (pelvic floor muscle electrostimulation) OR (pelvic muscle electrostimulation) OR (pelvic floor muscle electrical stimulation) OR (pelvic muscle electrical stimulation) OR (pelvic floor muscle training) OR (PFMT) OR (pelvic muscle training) OR (pelvic floor muscle electrostimulation) OR (pelvic muscle electrostimulation) OR (pelvic floor muscle electrical stimulation) OR (“pelvic floor training” OR “pelvic floor muscle therapy” OR “PFMT”) AND (urinary incontinence) OR AND (women OR female). The equivalent search keywords or the syntonic terms were used in other databases.
2.2. Study Selection and Criteria
Selection of studies was based on predesigned inclusion and exclusion criteria following the searches in relevant databases. Initially studies were identified based on screening of title and abstract, followed by full-text screening and including the final studies. Screening of the articles was conducted by two reviewers. The inclusion and exclusion criteria were based on the PICOS format (Table 1). The population criteria included only non-pregnant women patients suffering from UI. Post-surgical patients were excluded from the study. Intervention criteria included pelvic floor muscle training with or without biofeedback therapy with the exclusion of pharmacological interventions. The outcome of our interest included muscle strength, the endurance of PFM, UI and urinary leakage, and exclusion of another outcome. RCT studies were included, while the rest of all other types of experimental or analytical studies were excluded. A limitation was placed by including only English language studies published from the 1 January 2000 to 31 March 2021.

Table 1.
Inclusion and exclusion criteria of the study.
2.3. Data Extraction, Quality Assessment, Data Synthesis
Data extraction was performed in Microsoft Excel after reviewing all the final included studies. The data that were extracted from all the studies were the studies’ first author, year of publication, study design, inclusion criteria, intervention groups sample size, drop out, study duration, study outcome. During data extraction, no authors were contacted. Quality assessment of the studies was carried out using, “The Cochrane risk of bias 2 tool”. The quality of the studies was based on the following questions: randomization, deviation from interventions, missing outcome reporting, measuring the outcomes, and selective reporting of outcomes. Based on the following questions, studies were marked as low, medium, or high risk of bias. Following the data extraction, narrative synthesis was performed. Heterogeneity tests and meta-analysis of the studies were not performed.
3. Results
Study Selection
After systematic retrieval, 264 articles were selected from 4411 citations after duplication removal, proper title, and abstract screening. Following this, full-text screening of 264 articles was performed, out of which 15 were finally included, as shown in Figure 1. Finally, 15 articles consisting of 2441 non-pregnant women who had UI were selected for analysis.
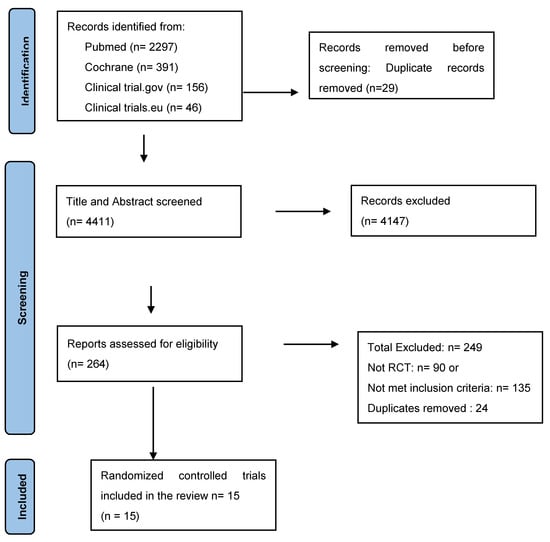
Figure 1.
Study selection, flow diagram.
4. Narrative Synthesis
4.1. Study and Population Characteristics
In terms of study and participants characteristics, there was a lot of homogeneity across all the studies [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16], as shown in Table 2. Among the 15 RCTs selected, 3 were performed in Brazil [3,5,8], 3 were performed in Canada [10,13,15], and 2 in Iran [7,9] while the rest were performed in Poland [1], UK [11], Sweden [4], Bangladesh [14], Norway [12], Hong Kong [2], and Turkey [16].

Table 2.
Study and population characteristic.
Patients randomized across all the studies were 2441, of which dropout was 227, and 2214 patients completed the studies. The lowest drop-out rate was 2 in Dumoulin et al. [10], and the highest was in Wagg et al. [14]
Intervention groups across all the studies were PFMT, extracorporeal magnetic innervation (ExMi), whole body vibration training (WBVT), pelvic floor muscle + abdominal muscle therapy (PFM + AMT), PFMT + biofeedback, pelvic floor muscle therapy + electrical stimulation (PFMT + ES), vaginal cones (VC), PFMT + education, education, and control. Out of the 15 studies, 11 studies [2,4,7,9,10,11,13,15,16] comprised two intervention groups, while 3 studies [1,5,10] comprised three interventions groups, and 1 study [3] comprised 4 intervention groups. The total number of patients in the PFMT group was 970 [1,2,5,7,13,17,18], ExMi was 69 [1,16], WBVT was 21, PFM + AMT was 23, PFMT + biofeedback was 326 [11,18], VC was 93 [3,8], PFMT+ education was 318 [14], education was 290 [14], and control was 229 [1,3,4,5,7,10,12,13].
The most important inclusion criterion across all the studies was aged above 18 years suffering from UI. Pregnant women or women in the early postpartum period (before 10 weeks after delivery) were excluded from the study. Study duration among all the studies ranged from 4 weeks to 104 weeks. A total of 3 studies [3,4,12] had a study duration of 26 weeks, 4 studies [2,8,13,17] had a duration of 12 weeks, and 3 studies lasted 8 weeks [7,10,18]. The remaining 5 studies had a duration of 52 weeks [5], 24 weeks [14], 104 weeks [11], 13 weeks [9], and 4 weeks [1]. The most common outcomes collected across the 15 studies were UI, PFM strength, endurance, urinary leakage, QoL, symptoms, PFM activity or function, vaginal squeeze pressure, self-esteem, and urodynamic test.
4.2. Overall Quality and Risk of Bias Assessing of Studies
Quality assessment of the studies was conducted using the “Cochrane ROB2” tool, as shown in Figure 2 and Figure 3 and Table 3. The studies were classified as at low risk of bias, some concerns, or high risk of bias. Overall, 7 studies [1,3,4,5,8,9,17] reported a low risk of bias, 3 studies [12,13] reported a high risk of bias, while the remaining 5 studies reported medium [2,10,11,14,18], or some risk of bias, as represented in Figure 3. Almost half of the studies had a low risk of bias in terms of the randomization process, missing outcome data, and selection of reported result, as shown in Figure 2. Around 76.9%, 69.2%, 84.6%, 61.5%, and 76.9% across all the studies reported low risk of bias in terms of the randomization process, deviation of intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result, respectively. Only 20% across all the studies reported a high risk of bias in terms of measurement of the outcome.
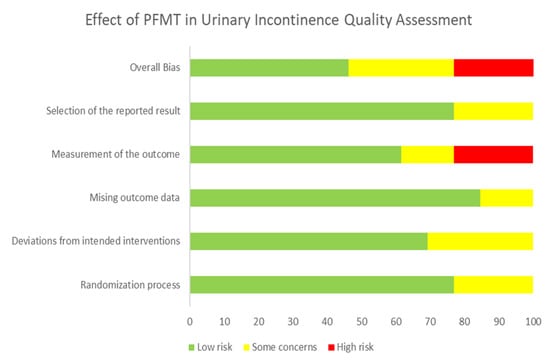
Figure 2.
Risk of bias for studies as percentage.
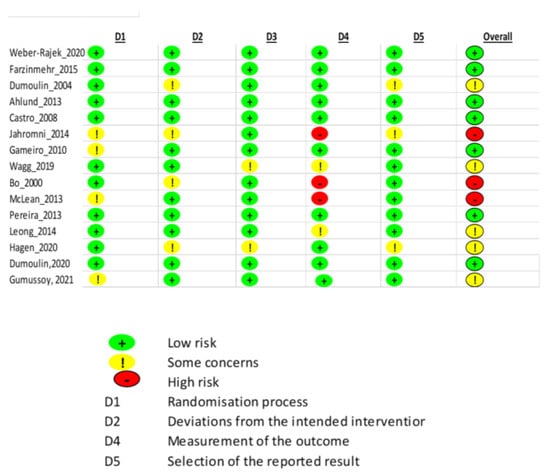
Figure 3.
Cochrane risk of bias for each component across all the studies.

Table 3.
Study outcome.
4.3. Study Outcome
Regarding outcome reporting, there was a lot of heterogeneity among the studies in terms of scales used for measuring the outcomes, reporting age, and other outcomes, as shown in Table 2. The most used scales for measuring muscle contraction, incontinence, and leakage were the pad test, VAS, I-QOL, Perineometer, ICIQ-UI SF, IIQ, and B-FLUTS. The age of women with incontinence ranged from 29.4 to 85 years across all the studies. In terms of reporting the outcome, there was a lot of dissimilarity across the studies.
Outcome on muscle contraction or muscle strength was reported by eight studies [3,5,8,11,16], urinary incontinence was reported by all the studies, and endurance was reported by one study [4].
In terms of muscle contraction, four studies [3,5,9,16] showed significant improvement between the groups; however, the instruments used for measuring the outcome for muscle contraction were different in all these studies. In four studies, improvements in muscle contraction were observed at the end of the study from baseline. In Hagen et al. [11], 8.5% of the patients in the PFMT + biofeedback and 6% in the PFMT group reported improvement in muscle contraction at 6 months. Ahlund et al. [4] showed a significant increase in PFM contraction from baseline in both groups at 26 weeks. Gameiro et al. [8] showed significant improvement from baseline in both the groups at 6 months but not at 12 months. For Gumussoy et al. [16], PFMC increased in both groups (PFMT with and without ExMI). However, there are few studies on ExMi and WBVT, and other studies are necessary to evaluate the use of these methods.
On the other hand, there were no significant results found for the endurance outcome across the studies. However, in one study by Ahlund et al. [4] at 26 weeks, improvement in endurance was observed from baseline.
All RCT studies showed significant reduction in severity of urinary incontinence from baseline after PFMT. However, the scale used for measuring the outcomes varied across the studies. For Dumoulin et al. [15], 70% of patients in individual PFMT group and 74% in group-based PFMT had a significant reduction in urinary incontinence at one year. For Gumussoy et al. [16], PFMT with BF with and without ExMI allowed the reduction in urinary loss. In Hagen et al. [11], 60% of patients in the PFMT + biofeedback and 62.6% in the PFMT group reported an improvement in symptoms at 24 months. In Ahlund et al. [4], a significant improvement was observed in both PFMT and control group at 26 weeks. In Jahromi et al. [7], a significant improvement from baseline was observed in both PFMT and control group for incontinence quality of life at 8.5 weeks, and in Leong et al. [2], more than 90% reduction was observed in PFMT group compared with control (7.2%) at 12 weeks.
Eight studies [2,3,5,7,10,14,15,16], used a similar outcome, i.e., the pad test method for measuring the outcome of urinary leakage, while the remaining three studies used different methods. In four studies, individual improvement was observed in the intervention groups from baseline. In Castro et al. [3], improvement in urinary leakage using the pad test was observed in 46% in PFMT, 48% in ES, 46% in VC, and 8% in the control at 26 weeks. In Jahromi et al. [7], a significant improvement from baseline was observed in both PFMT and control group for frequency of urine leakage and amount of urine leakage at 8.5 weeks. In Gameiro et al. [8], a significant improvement was observed from baseline in both the groups at 6 months but not at 12 months. Pereira et al. [5] reported significant decrease in urinary leakage in PFMT and VC group from baseline as compared with the control group at 52 weeks.
4.4. Sensitivity and Subgroup Synthesis
Overall, out of 997 PFMT or PFMT + education patients, 504 patients (50.5%) showed improvement in urinary incontinence, and 218 became continent (21.8%) (negative pad test). In total, 62% of patients significantly reduced their urinary incontinence or cured it and improved their pelvic floor muscle contraction.
On the other hand, significant improvements in endurance, muscle contraction, and urinary leakage were observed in 49 patients (23%), 168 patients (79.2%), and 97 patients (46%), respectively. However, the results across the outcome cannot be compared between the intervention groups, as the scales used for measuring the outcome varied across studies, except for urinary leakage.
5. Discussion
This systematic review demonstrated that PFMT is effective in reducing UI and improving muscle contraction.
Although previously, many systematic reviews have been published that assessed the efficacy of PFMT on pregnant and non-pregnant women, this review specifically focused on non-pregnant women [17,18,19,20,21]. Apart from UI, this is the first review that also focused on PMFT efficacy on endurance, muscle contraction, and urinary leakage. Moreover, in this review, only RCT studies were included, followed by quality assessment using the Cochrane risk of bias tool.
It focused on finding the clinical effectiveness of PFMT on non-pregnant women suffering from UI. Indeed, PFM dysfunction is associated with UI [22,23,24,25].
Overall, PFMT has almost proven to be effective in all the studies conducted. Some have used PFMT with biofeedback, which also has shown efficacious result [12,26]. It improved not only the physical but also the psychosocial aspects of women. Significant decline in depressive symptoms, with an improvement in UI severity and quality of life, was observed following the treatment [1]. There was also a significant decrease in incontinence among the groups treated with PFMT. Other observational studies also found a significant improvement in urinary continence after PFMT [26,27,28,29,30]. In almost every study, by increasing the pelvic muscle strength in women, it improved the quality of life index as well. Hence, it could be hypothesized that PFMT is a successful method for the treatment of incontinence and is recommended as first-line treatment [31].
Our study demonstrated that PFMT was effective in reducing UI. The duration of analyzed studies varied between 4 weeks and 52 weeks. A long-term follow-up was not evaluated, as our study was not focused on the recurrence of UI. The question of the duration of benefit effects of PFMT is important. However, as it is a conservative and minimally invasive treatment, other PFMT could be prescribed in case of recurrence of UI.
Another significant finding is that most of the studies, which used interventions such as ES, VC, WBVT, ExMi innervation, etc. along with PFMT, concluded that all these interventions were proven to be equally effective in treating UI. All these interventions also helped in the significant decrease in incontinence and improvement in quality of life [32,33,34]. No such significant difference was seen among the interventions [1,2,3,5,9]. In this review, in terms of study characteristics, the studies were similar, and in terms of reporting of outcomes, the studies were dissimilar. After conducting the sensitivity synthesis by vote-counting of the studies, all the good quality studies either showed significant improvement from baseline or significant improvement between the intervention groups. The majority of the patients had improvement in UI and in urinary leakage. However, improvement in muscle contraction and endurance could not be well established, as the scales used were different across the studies, but the pad test was used for measuring urinary leakage across the good-quality studies [3,5,8].
Strengths and Limitations of the Study
This study also has some important strengths and weaknesses. First, the search strategy used in this review was very robust, as it looked for citations on five databases and from four international grey literature sources (NICE, EMA, FDA, SMC). Throughout the review, the screening of the articles was based on the predesigned protocol, which was unchanged throughout the study. The quality of the studies was assessed and was taken into consideration while assessing the efficacy. No authors were contacted for gathering the missing data. Our systematic review was limited to articles written in English, which could constitute some bias. However, the majority of RCTs are written in English to reach an international scientific audience. We limited our study to the period 2000–2021; as methods and machine of physiotherapy changed, we did not extend our review before the year 2000. Meta-analysis was also not possible, as the scales used for measuring the outcomes and the measures of parameters were different across the studies.
However, better-quality RCT studies need to be included with similar parameters used for measuring the outcomes. Thus, this narrative sensitive synthesis showed enough evidence about the efficacy of PFMT in reducing UI and improving pelvic floor muscle contraction. Therefore, PFMT should be proposed before invasive surgical treatment for management of urinary incontinence.
Author Contributions
Conceptualization, S.A.; methodology, S.A.; software, Microsoft Excel 2017.; validation, S.A., S.M. and A.C.; formal analysis, S.A., S.M. and A.C.; investigation, S.A.; resources, S.A.; data curation, S.A.; writing—original draft preparation, S.A.; writing—review and editing, S.A., S.M. and A.C.; visualization, S.A.; supervision, S.A.; project administration, S.A.; funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available from the coresponding author under reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Weber-Rajek, M.; Strączyńska, A.; Strojek, K.; Piekorz, Z.; Pilarska, B.; Podhorecka, M.; Sobieralska-Michalak, K.; Goch, A.; Radzimińska, A. Assessment of the Effectiveness of Pelvic Floor Muscle Training (PFMT) and Extracorporeal Magnetic Innervation (ExMI) in Treatment of Stress Urinary Incontinence in Women: A Randomized Controlled Trial. BioMed Res. Int. 2020, 2020, 1019872. [Google Scholar] [CrossRef] [PubMed]
- Leong, B.S.; Mok, N.W. Effectiveness of a new standardized Urinary Continence Physiotherapy Program for community-dwelling older women in Hong Kong. Hong Kong Med. J. 2015, 21, 30–37. [Google Scholar] [PubMed]
- Castro, R.A.; Arruda, R.M.; Zanetti, M.R.D.; Santos, P.D.; Sartori, M.G.F.; Girão, M.J.B.C. Single-blind, randomized, controlled trial of pelvic floor muscle training, electrical stimulation, vaginal cones, and no active treatment in the management of stress urinary incontinence. Clinics 2008, 63, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Åhlund, S.; Nordgren, B.; Wilander, E.-L.; Wiklund, I.; Fridén, C. Is home-based pelvic floor muscle training effective in treatment of urinary incontinence after birth in primiparous women? A randomized controlled trial. Acta Obstet. Et Gynecol. Scand. 2013, 92, 909–915. [Google Scholar] [CrossRef]
- Pereira, V.S.; De Melo, M.V.; Correia, G.N.; Driusso, P. Long-term effects of pelvic floor muscle training with vaginal cone in post-menopausal women with urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2012, 32, 48–52. [Google Scholar] [CrossRef]
- Luginbuehl, H.; Lehmann, C.; Koenig, I.; Kuhn, A.; Buergin, R.; Radlinger, L. Involuntary reflexive pelvic floor muscle training in addition to standard training versus standard training alone for women with stress urinary incontinence: A randomized controlled trial. Int. Urogynecology J. 2021, 1–10. [Google Scholar] [CrossRef]
- Kargar Jahromi, M.; Talebizadeh, M.; Mirzaei, M. The effect of pelvic muscle exercises on urinary incontinency and self-esteem of elderly females with stress urinary incontinency, 2013. Glob. J. Health Sci. 2014, 7, 71–79. [Google Scholar] [CrossRef]
- Gameiro, M.O.; Moreira, E.H.; Gameiro, F.O.; Moreno, J.C.; Padovani, C.R.; Amaro, J.L. Vaginal weight cone versus assisted pelvic floor muscle training in the treatment of female urinary incontinence. A prospective, single-blind, randomized trial. Int. Urogynecology J. 2010, 21, 395–399. [Google Scholar] [CrossRef]
- Farzinmehr, A.; Moezy, A.; Koohpayehzadeh, J.; Kashanian, M. A comparative study of whole-body vibration training and pelvic floor muscle training on women’s stress urinary incontinence: Three-month follow-up. J. Fam. Reprod. Health 2015, 9, 147. [Google Scholar]
- Dumoulin, C.; Lemieux, M.-C.; Bourbonnais, D.; Gravel, D.; Bravo, G.; Morin, M. Physiotherapy for Persistent Postnatal Stress Urinary Incontinence: A Randomized Controlled Trial. Obstet. Gynecol. 2004, 104, 504–510. [Google Scholar] [CrossRef]
- Hagen, S.; Elders, A.; Stratton, S.; Sergenson, N.; Bugge, C.; Dean, S.; Hay-Smith, J.; Kilonzo, M.; Dimitrova, M.; Abdel-Fattah, M.; et al. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: Multicentre randomised controlled trial. BMJ 2020, 371, m3719. [Google Scholar] [CrossRef]
- Bø, K.; Talseth, T.; Vinsnes, A. Randomized controlled trial on the effect of pelvic floor muscle training on quality of life and sexual problems in genuine stress incontinent women. Acta Obstet Gynecol Scand. 2000, 4, 598–603. [Google Scholar]
- McLean, L.; Varette, K.; Gentilcore-Saulnier, E.; Harvey, M.-A.; Baker, K.; Sauerbrei, E. Pelvic floor muscle training in women with stress urinary incontinence causes hypertrophy of the urethral sphincters and reduces bladder neck mobility during coughing. Neurourol. Urodyn. 2013, 32, 1096–1102. [Google Scholar] [CrossRef] [PubMed]
- Wagg, A.; Chowdhury, Z.; Galarneau, J.-M.; Haque, R.; Kabir, F.; MacDonald, D.; Naher, K.; Yasui, Y.; Cherry, N. Exercise intervention in the management of urinary incontinence in older women in villages in Bangladesh: A cluster randomised trial. Lancet Glob. Health 2019, 7, e923–e931. [Google Scholar] [CrossRef]
- Dumoulin, C.; Morin, M.; Danieli, C.; Cacciari, L.; Mayrand, M.-H.; Tousignant, M.; Abrahamowicz, M.; Urinary Incontinence and Aging Study Group. Group-Based vs. Individual Pelvic Floor Muscle Training to Treat Urinary Incontinence in Older Women: A Randomized Clinical Trial. JAMA Intern. Med. 2020, 180, 1284–1293. [Google Scholar] [CrossRef]
- Gumussoy, S.; Kavlak, O.; Yeniel, A.O. Effects of Biofeedback-Guided Pelvic Floor Muscle Training with and without Extracorporeal Magnetic Innervation Therapy on Stress Incontinence: A Randomized Controlled Trial. J. Wound Ostomy Cont. Nurs. 2021, 48, 153–161. [Google Scholar] [CrossRef]
- Dumoulin, C.; Cacciari, L.P.; Hay-Smith, E.J.C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women (Review). Cochrane Database Syst. Rev. 2018, 10, CD005654. [Google Scholar]
- Bø, K.; Talseth, T.; Holme, I. Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. BMJ 1999, 318, 487–493. [Google Scholar] [CrossRef]
- Brennen, R.; Frawley, H.C.; Martin, J.; Haines, T.P. Group-based pelvic floor muscle training for all women during pregnancy is more cost-effective than postnatal training for women with urinary incontinence: Cost-effectiveness analysis of a systematic review. J. Physiother. 2021, 67, 105–114. [Google Scholar] [CrossRef]
- Radzimińska, A.; Strączyńska, A.; Weber-Rajek, M.; Styczyńska, H.; Strojek, K.; Piekorz, Z. The impact of pelvic floor muscle training on the quality of life of women with urinary incontinence: A systematic literature review. Clin. Interv. Aging. 2018, 13, 957–965. [Google Scholar] [CrossRef]
- Ayeleke, R.O.; Hay-Smith, E.J.C.; Omar, M.I. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women (Review). Cochrane Database Syst. Rev. 2015, 2015, CD010551. [Google Scholar] [CrossRef] [PubMed]
- Talasz, H.; Jansen, S.C.; Kofler, M.; Lechleitner, M. High prevalence of pelvic floor muscle dysfunction in hospitalized elderly women with urinary incontinence. Int. Urogynecology J. 2012, 23, 1231–1237. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Wong, V.; Moore, K.H. Why are some women with pelvic floor dysfunction unable to contract their pelvic floor muscles? Aust. N. Z. J. Obstet. Gynaecol. 2013, 53, 574–579. [Google Scholar] [CrossRef]
- Steensma, A.B.; Konstantinovic, M.L.; Burger, C.W.; De Ridder, D.; Timmerman, D.; Deprest, J. Prevalence of major levator abnormalities in symptomatic patients with an underactive pelvic floor contraction. Int. Urogynecology J. 2010, 21, 861–867. [Google Scholar] [CrossRef]
- Dietz, H.P.; Shek, C. Levator avulsion and grading of pelvic floor muscle strength. Int. Urogynecology J. 2007, 19, 633–636. [Google Scholar] [CrossRef]
- Yang, S.-J.; Liu, Y.-T.; Lo, S.-S.; Tsai, C.-C.; Pan, P.-J. Effect of a Comprehensive Rehabilitation Program for Community Women with Urinary Incontinence: A Retrospect Cohort Study. Healthcare 2021, 9, 1686. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Ashton-Miller, J.; DeLancey, J.O.L. A Pelvic Muscle Precontraction Can Reduce Cough-Related Urine Loss in Selected Women with Mild SUI. J. Am. Geriatr. Soc. 1998, 46, 870–874. [Google Scholar] [CrossRef] [PubMed]
- Tosun, O.C.; Mutlu, E.K.; Ergenoglu, A.M.; Yeniel, A.; Tosun, G.; Malkoc, M.; Askar, N.; Itil, I.M. Does pelvic floor muscle training abolish symptoms of urinary incontinence? A randomized controlled trial. Clin. Rehabil. 2014, 29, 525–537. [Google Scholar] [CrossRef]
- Luginbuehl, H.; Baeyens, J.-P.; Taeymans, J.; Maeder, I.-M.; Kuhn, A.; Radlinger, L. Pelvic floor muscle activation and strength components influencing female urinary continence and stress incontinence: A systematic review. Neurourol. Urodyn. 2015, 34, 498–506. [Google Scholar] [CrossRef]
- Thompson, J.A.; O’Sullivan, P.B.; Briffa, N.K.; Neumann, P. Assessment of voluntary pelvic floor muscle contraction in continent and incontinent women using transperineal ultrasound, manual muscle testing and vaginal squeeze pressure measurements. Int. Urogynecology J. 2006, 17, 624–630. [Google Scholar] [CrossRef]
- Cho, S.T.; Kim, K.H. Pelvic floor muscle exercise and training for coping with urinary incontinence. J. Exerc. Rehabil. 2021, 17, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Veldman, M.; Gondin, J.; Place, N.; Maffiuletti, N.A. Effects of Neuromuscular Electrical Stimulation Training on Endurance Performance. Front. Physiol. 2016, 7, 544. [Google Scholar] [CrossRef] [PubMed]
- Woodley, S.J.; Lawrenson, P.; Boyle, R.; Cody, J.D.; Mørkved, S.; Kernohan, A.; Hay-Smith, E.J.C. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst. Rev. 2020, 2021, CD007471. [Google Scholar] [CrossRef]
- Bech, S.R.; Villadsen, D.; Laursen, H.H.; Toft, A.; Reinau, H.S.; Raasted, T.H.; Christensen, K.W.; Corfitzen, L.H.; Christensen, S.W.M. The effect of group or individualised pelvic floor exercises with or without ultrasonography guidance for urinary incontinence in elderly women—A pilot study. J. Bodyw. Mov. Ther. 2021, 28, 34–41. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).