Abstract
(1) Background: Syrians are the largest forcibly displaced population in the world. Approximately 20,000 Syrian refugees have resettled in the United States (US) since the civil war in Syria began in 2011, with an estimated 130 families resettling in Houston, Texas. We conducted a pilot study with the objective of examining the physical and mental well-being of the Houston Syrian refugee population. (2) Methods: Online surveys were conducted using psychometrically valid instruments including Afghan Symptom Checklist (ASC), Refugee Post-Migration Stress Scale (RPMSS), Perceived Stress Scale (PSS), and Self-Report Questionnaire (SRQ) (3) Results: According to independent t-tests, Syrian refugee females scored higher than males on ASC (37.78 vs. 31.64, p = 0.0446), particularly in the subscales of sadness with social withdrawal (28.89 vs. 24.31, p = 0.0495), and stress-induced reactivity (6.56 vs. 4.86, p = 0.0004). Similarly, females scored higher than males in RPMSS (60.54 vs. 45.15, p = 0.0022), including the social strain domain (8.08 vs. 5.18, p = 0.0204). In PSS and SRQ, Syrian refugee females reported comparable stress and distress scores as males. (4) Conclusions: Syrian refugee females reported higher stress and distress than males. Displacement from their home country and social strain were the major sources of stress in Syrian refugee females, as indicated in RPMSS.
1. Introduction
The Syrian war, which began in 2011, is described as one of the world’s greatest humanitarian crises in modern history. As a result of the political turmoil, war, and destruction, Syrians have been forced to flee, making them the largest forcibly displaced population in the world, amounting to 13 million, including more than 6.7 million internally displaced. The Syrian population fled to several neighboring countries including Turkey, Lebanon, Iraq, Jordan, and Egypt [1]. Turkey hosts the largest number of Syrian refugees amounting to 3.6 million [2]. According to the data from the United Nations High Commissioner for Refugees (UNHCR), an estimated 20,000 Syrian refugees have come to the United States (US) since the civil war in Syria began in 2011. Approximately 130 families have resettled in Houston, Texas. Prior to their resettlement, most Syrian refugees reported experiencing traumatic events including torture of self or loved ones, death of family members or friends, and loss of property, income, and self-sufficiency [3].
The resettlement of refugees in general is a slow process involving temporary crowded, ill-managed, and poorly equipped refugee camps in multiple countries [4,5,6,7]. For Syrian refugees, it has been particularly hard, considering their long journey, often having lived in refugee camps in Jordan, Lebanon, Turkey, Egypt, and Iraq (UNHCR, 2015). Having lived through the traumatic experiences of war and displacement, the Syrian refugees face new stressors upon re-settlement in the US. Although the new environment in the host country, the US, is safe and protected, the new stressors of becoming a minority in a new country, learning a new language, and new social and cultural norms add multiple layers of stress on top of an already stressed and trauma-inflicted life. It is well-known that populations who live in places ravaged from armed conflict, terror, and war often develop posttraumatic stress disorder (PTSD) [3,8,9,10] and other mental health problems [11,12]. Interestingly, resilience following the experience of traumatic events also has been reported in some who have experienced traumatic events of war, conflict, and displacement [13,14,15,16,17].
The present study was designed to explore the mental health and general well-being of Syrian refugees who are resettled in Houston, Texas, US. Experience of PTSD-associated symptoms, aggression, general physical and metabolic health (presence of chronic illnesses like diabetes, hypertension, hypothyroidism, asthma, and irritable bowel syndrome), and sleep status were investigated. We also examined gender differences as women refugees are described as the most vulnerable among the refugee population [18,19,20]. The impact of the new conditions of the host communities of Houston, such as work status and general income, were also explored. Other factors such as age, gender, education, cigarette and hookah smoking habits were included, as they play a significant role in stress reactivity and stress management in this population [20,21].
2. Materials and Methods
All communication forms and survey questionnaires utilized in the study were approved by the Institutional Review Board (IRB) Committee (STUDY00002065) for the Protection of Human Subjects, University of Houston (UH), Houston, TX, US.
2.1. Subject Recruitment
Upon approval of the study protocol by the UH-IRB Committee, Syrian refugees were recruited to participate in the study through the Houston-based 501 (C) (3) non-profit organization IMPACTs, which facilitates re-settlement of Syrian refugees in the Houston area. The basic criteria of inclusion were exposure to Syrian war and conflict before coming to the US. The refugees might have arrived at another American city but must at present live in the Houston area. The Syrian refugees who agreed to participate in the study were contacted via phone in Arabic. The postdoctoral fellow involved in this study is an Arab American who was responsible for describing study objectives, protocol criteria, and survey instructions to the participants in their native language, following which a secure REDCap survey link was sent via text messages. Participants completed the survey questionnaire either independently or with some guidance via phone by the post-doctoral fellow. Upon survey completion, each participant received a $25 gift card.
2.2. Measures
Surveys included a sociodemographic questionnaire with general questions on the demographic and psychosocial circumstances of the respondents including age, gender, education level, socio-economic status, relationship status, and health care access. Questions related to smoking habits and prevalence of chronic diseases (diabetes, hypertension, hypothyroidism, asthma, and irritable bowel syndrome) were included in the participant characteristics section, as these measures are reported to be correlated with stress and mental well-being [21,22,23,24]. Measures of mental health, stress and distress, post-conflict situations, and post-migration stress sources included validated Arabic versions of Self-Reporting Questionnaire (SRQ), Perceived Stress Scale (PSS), Afghan Symptoms Checklist (ASC), and Refugee Post-Migration Stress Scale (RPMSS), respectively.
The SRQ was developed by the World Health Organization by collecting data of patients who contacted primary health care settings for the screening of mental disorder [25]. The questionnaire consists of 24 questions, 20 related to neurotic symptoms, and 4 related to psychotic symptoms. Each of the 24 questions is scored 1 or 0: a score of 1 indicates that the symptom was present during the past month; a score of 0 indicates that it was absent [26]. Different cut-off scores for the SRQ-20 have been selected in different studies, depending on the criteria, culture, and language, but the most prevalent cut-off is considered to be 7. A score of 7 or above indicates the presence of a potential psychological problem. In this study, we used the short form of the SRQ (SRQ-20), which consists of the first 20 non-psychotic items, as this instrument was previously validated in the Arab population [27,28,29]. In our sample, the SRQ-20 also showed high reliability, with a Cronbach’s alpha value of 0.87.
The PSS questionnaire is designed to assess the level of perceived stress experienced over a period of one month [28]. The PSS-14 instrument consists of 7 positive items and 7 negative items rated on a 5-point scale (0 = Never, 1 = Almost Never, 2 = Sometimes, 3 = Fairly Often, 4 = Very Often). Items 4, 5, 6, 7, 9, 10, and 13 are the positively stated items. The scores are calculated by re-versing the scores on the seven positive items, i.e., 0 = 4, 1 = 3, 2 = 2, 3 = 1, and 4 = 0, and then summing across all the 14 items [30]. The Arabic version of the PSS-14 has been previously validated [31]. The PSS-14 showed adequate reliability in our sample, with a Cronbach’s alpha coefficient of PSS of 0.79.
The ASC was developed and used in Kabul, Afghanistan, to identify local indicators of psychological distress in conflict and post-conflict situations [11]. The instrument demonstrated excellent reliability (α = 0.93) and good construct validity. The ASC is a 22-item instrument asking about one’s feelings and experience over a period of 2 weeks. The answers are rated on a 5-point scale (1 = never, 2 = one day each week, 3 = 2–3 days each week, 4 = 4–5 days each week, 5 = every day). The questionnaire consists of three interpretable factors: (1) sadness with social withdrawal and somatic distress, (2) ruminative sadness without social isolation and somatic distress, and (3) stress-induced reactivity, indicated by quarreling, beating one’s children, and nervousness. Among the items are three Dari terms (Dari is the native language spoken by people from Afghanistan) representing Afghan idioms of distress: jigar khun, a term describing a form of sadness that includes grief following interpersonal loss; asabi, a term for feeling nervous or highly stressed, and fishar, or “blood pressure”, which refers to internal agitation or low energy and motivation [11,32]. These terms were translated into Arabic utilizing culturally appropriate terms.
The RPMSS was recently developed and validated among refugees from Syria recently resettled in Sweden [31]. The survey consists of 21 items covering 7 hypothesized domains of post-migration stress: (1) perceived discrimination, (2) lack of host country-specific competencies, (3) material and economic strain, (4) loss of home country, (5) family and home country concerns, (6) social strain, and (7) family conflicts. Each domain has at least 3 items. The answers are rated on a 5-point scale (1 = never, 2 = seldom, 3 = sometimes, 4 = often, 5 = very often). The scores were calculated by adding the scores of all items. The RPMSS showed adequate reliability in our sample, with a Cronbach’s alpha coefficient of 0.92.
2.3. Translations
Validated Arabic versions of the PSS, RPMSS, and SRQ were used [28,29,31,33,34]. For ASC, linguistic translation was prepared following linguistic validation guidelines. The linguistic validation of translation consisted of four steps: in the first step, forward translation (English to Arabic) was prepared by a bilingual post-doctoral fellow working on this study. The post-doctoral fellow is a native Arabic speaker and was born and raised on the Syrian–Jordanian border town of Irbid, Jordan. In the second step, backward translation (Arabic to English) was kindly provided by two bilingual faculty members at the University of Houston. In the third step, comparison between back translation version and original questionnaire was conducted by the primary investigator; whenever discrepancies were found between the two versions, the Arabic expressions were adjusted until no further discrepancies were found between the two versions. In the fourth step, the translated version was tested on five Arabic respondents to determine whether the translation was acceptable.
2.4. Online Survey
Both versions (Arabic and English) of the survey questions were uploaded on the REDCap platform which enables secure building and management of online surveys. The survey link was sent to the participants via a text message. Upon clicking on the link in the text message, the participants were able to choose the language of survey completion. Some participants preferred the questions be read to them over the phone, so we collected their responses via a phone call interview.
2.5. Data Analysis
Data were first examined using descriptive statistics. Sample comparisons between males and females were performed using independent t-test or chi-square test for continuous and categorical variables, respectively. Analysis of covariance (ANCOVA) was used to examine the association of gender and the stress scale while controlling for participant age. ANCOVA was conducted separately for each stress scale. The intercorrelation between each stress scale and participant characteristics were examined. Significance was set at p < 0.05. All analyses were conducted using SAS software (SAS Institute Inc. Cary, NC, USA, 2014, version 9.4).
3. Results
Data were collected from a total of 94 Syrian refugees (38 males, 55 females, and 1 non-binary). The non-binary participant was not included in the analytic sample. Of the 94 participants, 22 completed the questionnaires in English, 72 in Arabic. Some of the young respondents, who completed some college here in the US, chose to answer the survey in English, while most of the respondents whose English language was poor or very limited preferred to complete the Arabic version of the survey.
3.1. Demographics
Table 1 depicts the demographic characteristics and social circumstances of the participants overall and by gender. Participant age ranged between 17 and 61 years (Mean = 36.11, SD = 9.85). Overall, 56.52% (N = 52) of this group reported as having education below high school, 25.27% (N = 23) reported working more than 15 h per week, and 80.22% (N = 73) reported as having health insurance. Further, 79.35% (N = 73) were married, 83.52% (N = 76) reported living with a spouse/partner, 60.23% (N = 53) reported a total household income < $10,000, 78.49% (N = 73) and 86.02% (N = 80) reported non-cigarette or Hookah smoking, respectively.

Table 1.
Participant Characteristics by Gender.
Chi-square tests indicated significant associations between gender and age group (p = 0.0313), household income (p = 0.0375) and smoking status (p < 0.001). Compared with male participants, female participants were more likely to be in the 26–39 years age group (53.70% vs. 26.32%), had higher total household income (49.02% vs. 27.03%), and reported as being non-smokers (98.18% vs. 50%).
3.2. Survey Scores and Gender
According to the independent t-tests, Syrian refugee females scored higher than males on ASC (37.78 vs. 31.64, p = 0.0446), see Figure 1, particularly in the subscales of sadness with social withdrawal (28.89 vs. 24.31, p = 0.0495) and stress-induced reactivity (6.56 vs. 4.86, p = 0.0004). Similarly, females scored higher than men in RPMSS (60.54 vs. 45.15, p = 0.0022), see Figure 2, including the social strain domain (8.08 vs. 5.18, p = 0.0204).

Figure 1.
The data are displayed as a box-and-whisker plot. The boxes indicate the intervals between the 25th and the 75th percentiles, the horizontal bars inside the boxes indicate the medians, and ◊ indicates the means. The whiskers indicate the data intervals. Data were analyzed using independent t-tests. N = 38 males and 55 females.
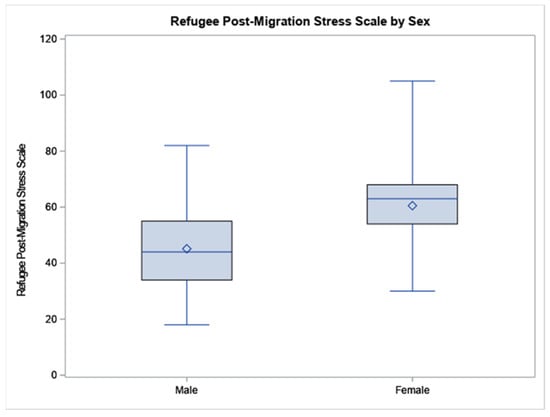
Figure 2.
The data are displayed as a box-and-whisker plot. The boxes indicate the intervals between the 25th and the 75th percentiles, the horizontal bars inside the boxes indicate the medians, and ◊ indicates the means. The whiskers indicate the data intervals. Data were analyzed using independent t-tests. N = 38 males and 55 females.
Similar results were yielded when controlling for refugee age in both ASC and RPMSS, except for RPMSS subscale loss of home country and ASC subscale sadness with social withdrawal. The results of ANCOVAs revealed that there were significant gender differences in RPMSS after controlling for age, but not in SRQ and PSS scales. Post hoc analyses showed that females reported significantly higher distress relative to males in ASC (p = 0.0469), particularly, in the stress-induced reactivity subscale (p = 0.0014). Similarly, in RPMSS, females reported significant higher stress relative to males (p = 0.0017), which was evident in the loss of home country domain (p = 0.0455) and social strain domain (p = 0.0195).
3.3. Correlation Analyses
Correlation analysis indicated that adults who reported a greater number of current health problems were more likely to report more mental health problems, (SRQ: r = 0.369, p < 0.001), higher psychological distress (ASC: total: r = 0.289, p = 0.006) related to higher sadness with social withdrawal (r = 0.28, p = 0.008), and ruminative sadness (r = 0.269, p = 0.011) and stress reactivity (r = 0.241, p = 0.022) than adults with fewer health concerns.
Socioeconomic and family risk factors were also related to adults’ mental health and stress. Lower income was associated with significantly greater social strain (r = 0.306, p = 0.036), poorer general mental health (SRQ: r = 0.249, p = 0.021), and higher psychological distress (ASQ: r = 0.277, p = 0.010), specifically related to greater sadness with social withdrawal (r = 0.265, p = 0.014) and to ruminative sadness (r = 0.3, p = 0.005). Adults living in households with a larger number of children were more likely to report concerns about discrimination (RPMSS: r = 0.300, p = 0.005) and more family conflict (r = 0.495, p = 0.001), than those with fewer children in the home, see Table 2. Variability on the PSS was generally not significantly associated with individual, family, or socio-economic risk scores.

Table 2.
Correlations between health/stress scales and participant characteristics.
4. Discussion
In the present study, Syrian refugee females reported significantly higher mental stress relative to males in RPMSS, which potentially arises from displacement from their home country and from the social strain of resettlement in a culturally novel environment. This seems highly probable, considering previous reports suggesting the prevalence of social strain in refugee women [35,36,37]. Several important factors may have contributed to the social strain: (1) Syrian refugee women expressed their inadequateness in communicating with non-Arabs, (2) the majority of the women were unemployed and did not drive, hence were mostly confined in their homes, (3) doctor’s visits or shopping trips were always chaperoned by a spouse, (4) spoke minimal or no English. Thus, it is obvious that the interaction of refugee women with Americans or individuals from other minorities was very limited. This, combined with the language barrier, adds to the social strain as it reduces the refugee women’s ability to share experiences and burdens with others, increasing the risk of low self-esteem and depression [38,39]. Furthermore, the language barrier is a well-recognized impediment in seeking employment, accessing health care services, and building social connections, thus inhibiting quick integration and adaptation into the host country [19,40]. In addition to language barrier and isolation, the longing for the home country and the loss of cultural belonging through forced migration may be an additional source of strain. Syrian refugee men, on the other hand, reported less stress related to the social strain domain, as they were not confined or isolated as the women. Since men were the breadwinners of the family, and through employment built social interaction, they were more proficient in English than women.
Our data showed that living with a partner was significantly associated with perceived stress and refugee post-migration stress. Previous studies have highlighted the fact that refugee women typically have many children, often live in a joint-family system, and consequently bear extra burden of child care, spouse care, as well as care for the elderly who in most cases have disabilities and/or chronic diseases [41]. Thus, the marital pressures, financial insecurity, and high expectations of the husband collectively create a high-stress environment for Arab women. Relevant to this, marriage has been reported as a mental health risk factor for Iraqi women in a study conducted in Sweden [42]. Iraqi and Syrian women share similar cultural pressures of the patriarchal Arab family patterns [43,44,45]. Correlation analysis also indicated that a number of health issues positively correlated with scores of RPMSS. This is not surprising, considering the intricate cause-and-effect relationship between stress and chronic diseases, such as diabetes, hypertension, and irritable bowel syndrome [46,47]. This is in agreement with previous evidence that suggests that stressful experiences affect body metabolism and predispose an individual to chronic diseases such as diabetes [48], hypertension [49], and irritable bowel syndrome [50,51].
Increased stress in Syrian refugee females, as identified in RPMSS, manifested in ASC symptoms. Syrian refugee women reported a significantly higher overall score in ASC when compared to men. Furthermore, refugee women reported higher scores in the ASC subscale of sadness with social withdrawal and somatic distress and in stress-induced reactivity. Correlation analysis indicated that the number of health issues and family income were positively correlated with all ASC domains. Our data and previous studies suggest that refugee women are at a greater risk of mental health problems, such as depression, anxiety, and PTSD, which increases the risk of psychopathological disorders among this vulnerable group [41,52].
In SRQ, Syrian refugee females and males reported comparable scores, which were below the clinical prevalence cutoff of 7. While significant differences were not obtained between males and females in SRQ, the scores of SRQ for both men and women significantly positively correlated with a number of health issues and also with family income. Perceived stress significantly correlated with living with a partner. The family demands, particularly caring for the children, contributed to the perceived stress. Finally, it seems that RPMSS and ASC are more culturally appropriate instruments for the evaluation of mental distress in Syrian refugees than SRQ or PSS. This is not surprising, considering previous studies where ASC and RPMSS were deemed more appropriate and culturally grounded instruments and particularly regarded as more salient for capturing mental distress in women [32].
5. Conclusions
In conclusion, our study has revealed the economic, health, and mental health vulnerabilities of Syrian refugees re-settled in Houston, TX. Our preliminary data suggest that Syrian refugees are highly vulnerable to mental health problems and trauma-related distress symptoms, particularly, female refugees who reported significantly higher distress and greater stress symptoms compared with male refugees. Although high trauma-susceptibility and high resilience have both been reported in refugee women [19,21], Syrian refugee women seem to be a highly vulnerable population [20,52]. Therefore, our recommendations for future interventions include the use of culturally sensitive language-tailored community enrichment programs (English language skills, health educational programs for refugees with low literacy, etc.) which will allow greater assimilation of Syrian refugee women into the American society.
6. Limitations
Our study has several limitations. First, the reliance on self-report, as opposed to clinical interview; second, a small sample size focused on one city. Therefore, the results cannot be generalized to other similar populations resettling in other cities. Third, the correlational nature of our observations mitigates cause-and-effect conclusions.
Author Contributions
Conceptualization was made by S.S. and F.A. F.A., G.A. and S.S., conducted the literature review, interacted with Syrian refugees, prepared the survey questionnaires. S.S. and F.A. wrote the first draft of the manuscript. T.A.C. conducted statistical analysis, B.B. and J.B. assisted with the survey and interpretation of results. S.S. finalized the draft after several layers of edits and iterations. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Institute on Minority Health and Health Disparities (NIMHD) of the National Institutes of Health (NIH) to the University of Houston under Award Number U54MD015946. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work also was supported by Grants to Enhance Research on Racism, UH Bridge and Provost’s 50-in-5 grants, University of Houston.
Institutional Review Board Statement
All communication forms and survey questionnaires utilized in the study were approved by the Institutional Review Board (IRB) Committee (STUDY00002065) for the Protection of Human Subjects, University of Houston (UH), Houston, TX, US. The study was conducted according to the guidelines of the Declaration of United States and approved by the Institutional Review Board (or Ethics Committee) of University of Houston (STUDY00002065, 14 May 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Acknowledgments
The authors gratefully acknowledge the help and support of the IMPACTs study coordinator Farzana Ahmad and Multicultural Center (MCC) study coordinator Uzma Khan (PharmD) for their help in the recruitment of Syrian refugees in this study. The authors are also grateful to Andreas Malm, Department of Health Sciences, The Swedish Red Cross University College, Huddinge, Sweden, and Petter Tinghog, Department of Clinical Neuroscience, Karolinska Institute, Division of Insurance Medicine, Stockholm, Sweden, for sharing the RPMSS instrument and for their valuable feedback on the study.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Nola, S. Legal Protection of Refugees from the Syrian Conflict in the View of International Human Rights. Research Gate. 2022. Available online: https://www.researchgate.net/publication/357553844_LEGAL_PROTECTION_OF_REFUGEES_FROM_THE_SYRIAN_CONFLICT_IN_THE_VIEW_OF_INTERNATIONAL_HUMAN_RIGHTS. (accessed on 1 December 2021).
- Acarturk, C.; Uygun, E.; Ilkkursun, Z.; Yurtbakan, T.; Kurt, G.; Adam-Troian, J.; Senay, I.; Bryant, R.; Cuijpers, P.; Kiselev, N.; et al. Group problem management plus (PM+) to decrease psychological distress among Syrian refugees in Turkey: A pilot randomised controlled trial. BMC Psychiatry 2022, 22, 8. [Google Scholar] [CrossRef] [PubMed]
- Kira, I.A.; Shuwiekh, H.; Rice, K.; Al Ibraheem, B.; Aljakoub, J. A threatened identity: The mental health status of Syrian refugees in Egypt and its etiology. Identity 2017, 17, 176–190. [Google Scholar] [CrossRef]
- Bart, D.B. The Living Conditions and Well-Being of Refugees; United Nations Development Programme: Human Development Reports Research Paper 2009/25 July 2009; UNDP: 2009. Available online: https://mpra.ub.uni-muenchen.de/19208/ (accessed on 1 December 2021).
- Ferris, E.; Winthrop, R. The hidden crisis: Armed conflict and education. In Education and Displacement: Assessing Conditions for Refugees and Internally Displaced Persons Affected by Conflict; Background paper for the EFA Global Monitoring Report 2011; Brookings Institution: Washington, DC, USA, 2010. [Google Scholar]
- Mirza, M.; Luna, R.; Mathews, B.; Hasnain, R.; Hebert, E.; Niebauer, A.; Mishra, U.D. Barriers to healthcare access among refugees with disabilities and chronic health conditions resettled in the US Midwest. J. Immigr. Minor. Heal. 2014, 16, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Tiltnes, Å.A.; Zhang, H.; Pedersen, J. The Living Conditions of Syrian Refugees in Jordan; Fafo: Oslo, Norway, 2019. [Google Scholar]
- Goren, C.; Neter, E. Stereotypical thinking as a mediating factor in the association between exposure to terror and post-traumatic stress disorder symptoms among Israeli youth. Anxiety Stress Coping 2016, 29, 644–659. [Google Scholar] [CrossRef]
- Kijewski, S.; Freitag, M. Civil war and the formation of social trust in Kosovo: Posttraumatic growth or war-related distress? J. Confl. Resolut. 2018, 62, 717–742. [Google Scholar] [CrossRef]
- Kletter, H.; Carrion, V.G. Posttraumatic Stress Disorder in Youth Exposed to War and Terror, in Sleep and Combat-Related Post Traumatic Stress Disorder; Springer: New York, NY, USA, 2018; pp. 363–372. [Google Scholar]
- Miller, K.E.; Rasmussen, A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma-focused and psychosocial frameworks. Soc. Sci. Med. 2010, 70, 7–16. [Google Scholar] [CrossRef]
- Steel, Z.; Chey, T.; Silove, D.; Marnane, C.; Bryant, R.A.; van Ommeren, M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. Jama 2009, 302, 537–549. [Google Scholar] [CrossRef]
- Fino, E.; Mema, D.; Russo, P. War trauma exposed refugees and posttraumatic stress disorder: The moderating role of trait resilience. J. Psychosom. Res. 2020, 129, 109905. [Google Scholar] [CrossRef]
- Gold, P.B.; Engdahl, B.; Eberly, R.E.; Blake, R.J.; Page, W.F.; Frueh, B.C. Trauma exposure, resilience, social support, and PTSD construct validity among former prisoners of war. Soc. Psychiatry Psychiatr. Epidemiol. 2000, 35, 36–42. [Google Scholar] [CrossRef]
- Hanbury, R.F.; Indart, M.J. Resilience Revisited: Toward an Expanding Understanding of Post-Disaster Adaptation. In Resilience in Children, Adolescents, and Adults; Springer: New York, NY, USA, 2013; pp. 213–225. [Google Scholar]
- Sherwood, K.; Liebling-Kalifani, H. A grounded theory investigation into the experiences of African women refugees: Effects on resilience and identity and implications for service provision. J. Int. Women’s Stud. 2012, 13, 86–108. [Google Scholar]
- Vindevogel, S.; Verelst, A. Supporting Mental Health in Young Refugees: A Resilience Perspective. In CHILD, Adolescent and Family Refugee Mental Health; Springer: New York, NY, USA, 2020; pp. 53–65. [Google Scholar]
- Kimerling, R.; Ouimette, P.; Weitlauf, J.C. Gender issues in PTSD. Handb. PTSD Sci. Pract. 2007, 29, 207–228. [Google Scholar]
- Robertson, C.L.; Halcon, L.; Savik, K.; Johnson, D.; Spring, M.; Butcher, J.; Westermeyer, J.; Jaranson, J. Somali and Oromo refugee women: Trauma and associated factors. J. Adv. Nurs. 2006, 56, 577–587. [Google Scholar] [CrossRef]
- Chung, M.C.; AlQarni, N.; Almazrouei, M.; Al Muhairi, S.; Shakra, M.; Mitchell, B.; Al Mazrouei, S.; Al Hashimi, S. Posttraumatic stress disorder and psychiatric co-morbidity among syrian refugees of different ages: The role of trauma centrality. Psychiatr. Q. 2018, 89, 909–921. [Google Scholar] [CrossRef]
- Basheti, I.A.; Ayasrah, S.M.; Basheti, M.M.; Mahfuz, J.; Chaar, B. The Syrian refugee crisis in Jordan: A cross sectional pharmacist-led study assessing post-traumatic stress disorder. Pharm. Pract. 2019, 17, 1475. [Google Scholar] [CrossRef]
- Gwozdziewycz, N.; Mehl-Madrona, L. Meta-analysis of the use of narrative exposure therapy for the effects of trauma among refugee populations. Perm. J. 2013, 17, 70. [Google Scholar]
- Huddy, L.; Feldman, S. Americans respond politically to 9/11: Understanding the impact of the terrorist attacks and their aftermath. Am. Psychol. 2011, 66, 455. [Google Scholar] [CrossRef]
- Powell, T.M.; Shin, O.J.; Li, S.-J.; Hsiao, Y. Post-traumatic stress, social, and physical health: A mediation and moderation analysis of Syrian refugees and Jordanians in a border community. PLoS ONE 2020, 15, e0241036. [Google Scholar] [CrossRef]
- Sartorius, N.; Janca, A. Psychiatric assessment instruments developed by the World Health Organization. Soc. Psychiatry Psychiatr. Epidemiol. 1996, 31, 55–69. [Google Scholar] [CrossRef]
- Beusenberg, M.; Orley, J.H.; Organization W.H.O. A User’s Guide to the Self Reporting Questionnaire (SRQ); World Health Organization: Geneva, Switzerland, 1994. [Google Scholar]
- Ghubash, R.; Daradkeh, T.; El-Rufaie, O.; Abou-Saleh, M. A comparison of the validity of two psychiatric screening questionnaires: The Arabic General Health Questionnaire (AGHQ) and Self-Reporting Questionnaire (SRQ-20) in UAE, using Receiver Operating Characteristic (ROC) analysis. Eur. Psychiatry 2001, 16, 122–126. [Google Scholar] [CrossRef]
- El-Rufaie, O.E.; Absood, G.H. Validity study of the Self-Reporting Questionnaire (SRQ-20) in primary health care in the United Arab Emirates. Int. J. Methods Psychiatr. Res. 1994, 4, 45–53. [Google Scholar]
- Al-Subaie, A.S.; Mohammed, K.; Al-Malik, T. The Arabic self-reporting questionnaire (SRQ) as a psychiatric screening instrument in medical patients. Ann. Saudi Med. 1998, 18, 308–310. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Almadi, T.; Cathers, I.; Mansour, A.M.H.; Chow, C.M. An Arabic version of the perceived stress scale: Translation and validation study. Int. J. Nurs. Stud. 2012, 49, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, A.; Ventevogel, P.; Sancilio, A.; Eggerman, M.; Panter-Brick, C. Comparing the validity of the self reporting questionnaire and the Afghan symptom checklist: Dysphoria, aggression, and gender in transcultural assessment of mental health. BMC Psychiatry 2014, 14, 206. [Google Scholar] [CrossRef]
- Malm, A.; Tinghög, P.; Narusyte, J.; Saboonchi, F. The refugee post-migration stress scale (RPMS)–development and validation among refugees from Syria recently resettled in Sweden. Confl. Health 2020, 14, 2. [Google Scholar] [CrossRef]
- Harpham, T.; Reichenheim, M.; Oser, R.; Thomas, E.; Hamid, N.; Jaswal, S.; Ludermir, A.; Aidoo, M. Measuring mental health in a cost-effective manner. Health Policy Plan. 2003, 18, 344–349. [Google Scholar] [CrossRef]
- Okello, J.; Onen, T.; Musisi, S. Psychiatric disorders among war-abducted and non-abducted adolescents in Gulu district, Uganda: A comparative study. Afr. J. Psychiatry 2007, 10, 225–231. [Google Scholar] [CrossRef][Green Version]
- True, J. The political economy of violence against women: A feminist international relations perspective. Aust. Fem. Law J. 2010, 32, 39–59. [Google Scholar] [CrossRef]
- Alsaba, K.; Kapilashrami, A. Understanding women’s experience of violence and the political economy of gender in conflict: The case of Syria. Reprod. Health Matters 2016, 24, 5–17. [Google Scholar] [CrossRef]
- Hashimoto-Govindasamy, L.; Rose, V. An ethnographic process evaluation of a community support program with Sudanese refugee women in western Sydney. Health Promot. J. Aust. 2011, 22, 107–112. [Google Scholar] [CrossRef]
- Baird, M.B. Well-being in refugee women experiencing cultural transition. Adv. Nurs. Sci. 2012, 35, 249–263. [Google Scholar] [CrossRef]
- Deacon, Z.; Sullivan, C. Responding to the complex and gendered needs of refugee women. Affilia 2009, 24, 272–284. [Google Scholar] [CrossRef]
- Shishehgar, S.; Gholizadeh, L.; DiGiacomo, M.; Green, A.; Davidson, P.M. Health and socio-cultural experiences of refugee women: An integrative review. J. Immigr. Minority Health 2017, 19, 959–973. [Google Scholar] [CrossRef]
- Tinghög, P.; Al-Saffar, S.; Carstensen, J.; Nordenfelt, L. The association of immigrant-and non-immigrant-specific factors with mental ill health among immigrants in Sweden. Int. J. Soc. Psychiatry 2010, 56, 74–93. [Google Scholar] [CrossRef]
- Phillimore, J. Refugees, acculturation strategies, stress and integration. J. Soc. Policy 2011, 40, 575–593. [Google Scholar] [CrossRef]
- Straiton, M.L.; Ledesma, H.M.L.; Donnelly, T.T. A qualitative study of Filipina immigrants’ stress, distress and coping: The impact of their multiple, transnational roles as women. BMC Women’s Health 2017, 17, 72. [Google Scholar] [CrossRef]
- Pavlish, C. Narrative inquiry into life experiences of refugee women and men. Int. Nurs. Rev. 2007, 54, 28–34. [Google Scholar] [CrossRef]
- Falco, G.; Pirro, P.S.; Castellano, E.; Anfossi, M.; Borretta, G.; Gianotti, L. The relationship between stress and diabetes mellitus. J. Neurol. Psychol. 2015, 3, 7. [Google Scholar]
- Kretchy, I.A.; Owusu-Daaku, F.T.; Danquah, S.A. Mental health in hypertension: Assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int. J. Ment. Health Syst. 2014, 8, 25. [Google Scholar] [CrossRef]
- Lloyd, C.; Smith, J.; Weinger, K. Stress and diabetes: A review of the links. Diabetes Spectr. 2005, 18, 121–127. [Google Scholar] [CrossRef]
- Zimmerman, R.; Frohlich, E. Stress and hypertension. J. Hypertension. Suppl. Off. J. Int. Soc. Hypertens. 1990, 8, S103–S107. [Google Scholar]
- Whitehead, W.E.; Crowell, M.D.; Robinson, J.C.; Heller, B.R.; Schuster, M.M. Effects of stressful life events on bowel symptoms: Subjects with irritable bowel syndrome compared with subjects without bowel dysfunction. Gut 1992, 33, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Mayer, E.A.; Naliboff, B.D.; Chang, L.; Coutinho, S.V.V. Stress and irritable bowel syndrome. Am. J. Physiol. Gastrointest. Liver Physiol. 2001, 280, G519–G524. [Google Scholar] [CrossRef] [PubMed]
- Acarturk, C.; Cetinkaya, M.; Senay, I.; Gulen, B.; Aker, T.; Hinton, D. Prevalence and predictors of posttraumatic stress and depression symptoms among Syrian refugees in a refugee camp. J. Nerv. Ment. Dis. 2018, 206, 40–45. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).