Neurological, Psychiatric, and Psychological Implications of the COVID-19 Pandemic: Protocol for a Large-Scale Umbrella Review of Observational Studies
Abstract
:1. Introduction
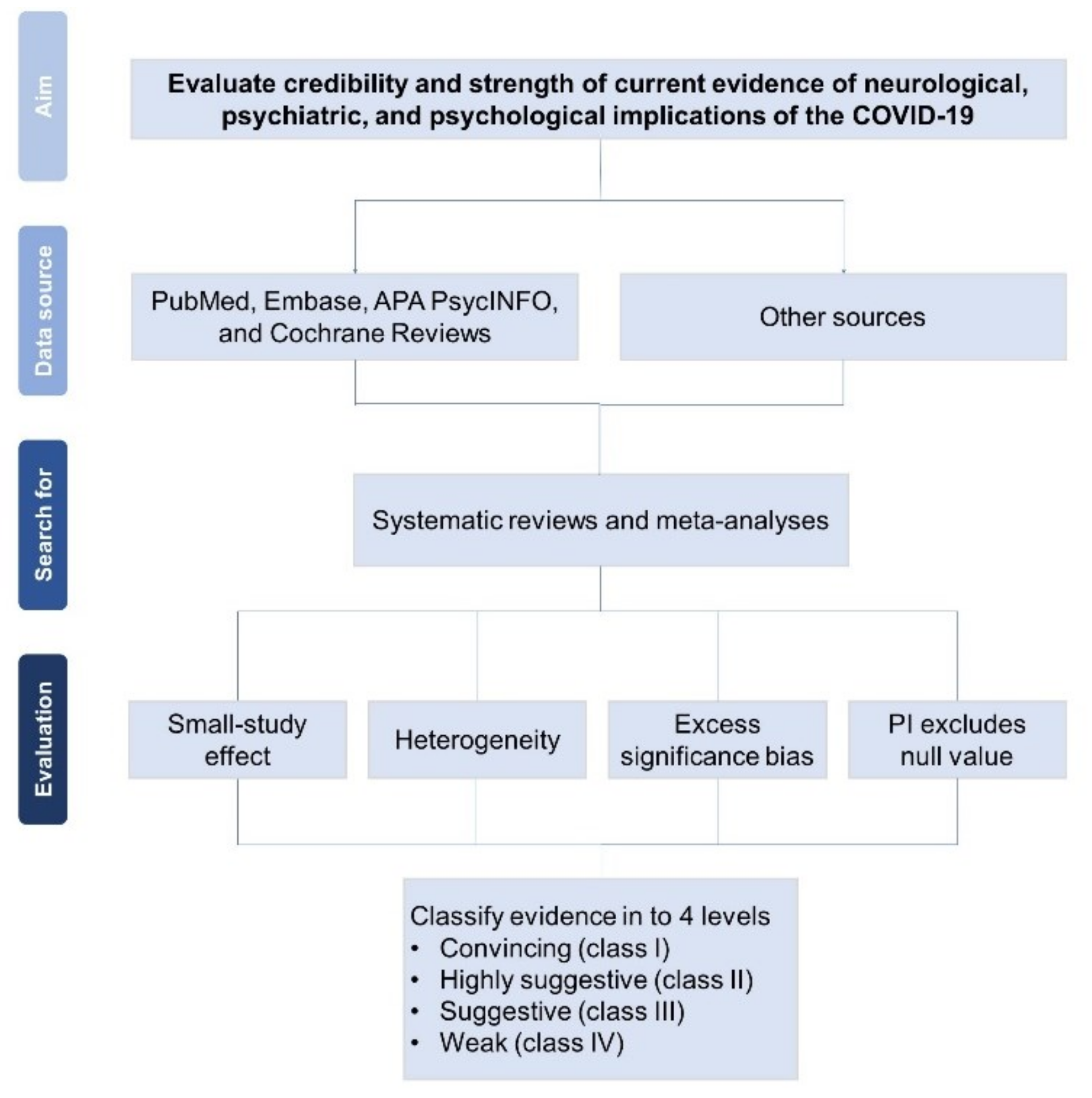
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Quality of Evidence
2.4. Data Extraction
2.5. Primary and Secondary Outcomes
2.6. Statistical Analysis
2.7. Credibility of Evidence
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Tay, M.Z.; Poh, C.M.; Rénia, L.; MacAry, P.A.; Ng, L.F. The trinity of COVID-19: Immunity, inflammation and intervention. Nat. Rev. Immunol. 2020, 20, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Madhavan, M.V.; Sehgal, K.; Nair, N.; Mahajan, S.; Sehrawat, T.S.; Bikdeli, B.; Ahluwalia, N.; Ausiello, J.C.; Wan, E.Y.; et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020, 26, 1017–1032. [Google Scholar] [CrossRef]
- Del Rio, C.; Collins, L.F.; Malani, P. Long-term Health Consequences of COVID-19. JAMA 2020, 324, 1723–1724. [Google Scholar] [CrossRef]
- Boldrini, M.; Canoll, P.D.; Klein, R.S. How COVID-19 Affects the Brain. JAMA Psychiatry 2021, 78, 682–683. [Google Scholar] [CrossRef]
- Marshall, M. How COVID-19 can damage the brain. Nature 2020, 585, 342–343. [Google Scholar] [CrossRef]
- Llach, C.D.; Vieta, E. Mind long COVID: Psychiatric sequelae of SARS-CoV-2 infection. Eur. Neuropsychopharmacol. 2021, 49, 119–121. [Google Scholar] [CrossRef]
- Blumenthal, D.; Fowler, E.J.; Abrams, M.; Collins, S.R. COVID-19—Implications for the henewalth care system. N. Engl. J. Med. 2020, 383, 1483–1488. [Google Scholar] [CrossRef] [PubMed]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Betty, P.; Carol, S.N. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar]
- Amsalem, D.; Dixon, L.B.; Neria, Y. The Coronavirus Disease 2019 (COVID-19) Outbreak and Mental Health: Current Risks and Recommended Actions. JAMA Psychiatry 2021, 78, 9–10. [Google Scholar] [CrossRef] [PubMed]
- Santomauro, D.F.; Herrera, A.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Cosentino, G.; Todisco, M.; Hota, N.; Della Porta, G.; Morbini, P.; Tassorelli, C.; Pisani, A. Neuropathological findings from COVID-19 patients with neurological symptoms argue against a direct brain invasion of SARS-CoV-2: A critical systematic review. Eur. J. Neurol. 2021, 28, 3856–3865. [Google Scholar] [CrossRef]
- Adibi, A.; Golitaleb, M.; Farrahi-Ashtiani, I.; Pirani, D.; Yousefi, K.; Jamshidbeigi, Y.; Sahebi, A. The prevalence of generalized anxiety disorder among health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. Front. Psychiatry 2021, 12, 658846. [Google Scholar] [CrossRef] [PubMed]
- Al Falasi, B.; Al Mazrouei, M.; Al Ali, M.; Al Dhamani, M.; Al Ali, A.; Al Kindi, M.; Dalkilinc, M.; Al Qubaisi, M.; Campos, L.A.; Al Tunaiji, H.; et al. Prevalence and determinants of immediate and long-term PTSD consequences of coronavirus-related (CoV-1 and CoV-2) pandemics among healthcare professionals: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 2182. [Google Scholar] [CrossRef] [PubMed]
- Allan, S.M.; Bealey, R.; Birch, J.; Cushing, T.; Parke, S.; Sergi, G.; Bloomfield, M.; Meiser-Stedman, R. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: A rapid systematic review and meta-analysis. Eur. J. Psychotraumatol. 2020, 11, 1810903. [Google Scholar] [CrossRef]
- Fusar-Poli, P. Mental disorders and risk of COVID-19 related mortality, hospitalization and intensive care unit admission: A systematic review and meta-analysis. Lancet Psychiatry 2021, 8, 797–812. [Google Scholar]
- Ceban, F.; Nogo, D.; Carvalho, I.P.; Lee, Y.; Nasri, F.; Xiong, J.; Lui, L.M.; Subramaniapillai, M.; Gill, H.; Liu, R.N.; et al. Association between Mood Disorders and Risk of COVID-19 Infection, Hospitalization, and Death: A Systematic Review and Meta-analysis. JAMA Psychiatry 2021, 78, 1079–1091. [Google Scholar] [CrossRef]
- Li, Y.; Cao, L.; Zhang, Z.; Hou, L.; Qin, Y.; Hui, X.; Li, J.; Zhao, H.; Cui, G.; Cui, X.; et al. Reporting and methodological quality of COVID-19 systematic reviews needs to be improved: An evidence mapping. J. Clin. Epidemiol. 2021, 135, 17–28. [Google Scholar] [CrossRef]
- Papatheodorou, S. Umbrella reviews: What they are and why we need them. Eur. J. Epidemiol. 2019, 34, 543–546. [Google Scholar] [CrossRef]
- Correll, C.U.; Cortese, S.; Croatto, G.; Monaco, F.; Krinitski, D.; Arrondo, G.; Ostinelli, E.G.; Zangani, C.; Fornaro, M.; Estradé, A.; et al. Efficacy and acceptability of pharmacological, psychosocial, and brain stimulation interventions in children and adolescents with mental disorders: An umbrella review. World Psychiatry 2021, 20, 244–275. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vieta, E.; Pérez, V.; Arango, C. Psychiatry in the aftermath of COVID-19. Rev. Psiquiatr. Salud. Ment. 2020, 13, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Grimshaw, J.M.; Wells, G.A.; Boers, M.; Andersson, N.; Hamel, C.; Porter, A.C.; Tugwell, P.; Moher, D.; Bouter, L.M. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med. Res. Methodol. 2007, 7, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pieper, D.; Antoine, S.L.; Mathes, T.; Neugebauer, E.A.; Eikermann, M. Systematic review finds overlapping reviews were not mentioned in every other overview. J. Clin. Epidemiol. 2014, 67, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Riley, R.D.; Higgins, J.P.T.; Deeks, J.J. Interpretation of random effects meta-analyses. BMJ 2011, 342, d549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Tsilidis, K.K.; Kasimis, J.C.; Lopez, D.S.; Ntzani, E.E.; Ioannidis, J.P. Type 2 diabetes and cancer: Umbrella review of meta-analyses of observational studies. BMJ 2015, 350, g7607. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [Green Version]
- Ioannidis, J.P.; Trikalinos, T.A. The appropriateness of asymmetry tests for publication bias in meta-analyses: A large survey. CMAJ 2007, 176, 1091–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsilidis, K.K.; Panagiotou, O.A.; Sena, E.S.; Aretouli, E.; Evangelou, E.; Howells, D.W.; Salman, R.A.; Macleod, M.R.; Ioannidis, J.P. Evaluation of excess significance bias in animal studies of neurological diseases. PLoS Biol. 2013, 11, e1001609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsilidis, K.K.; Papatheodorou, S.I.; Evangelou, E.; Ioannidis, J.P. Evaluation of excess statistical significance in meta-analyses of 98 biomarker associations with cancer risk. J. Natl. Cancer Inst. 2012, 104, 1867–1878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dragioti, E.; Karathanos, V.; Gerdle, B.; Evangelou, E. Does psychotherapy work? An umbrella review of meta-analyses of randomized controlled trials. Acta Psychiatr. Scand. 2017, 136, 236–246. [Google Scholar] [CrossRef] [PubMed]
- Naci, H.; Ioannidis, J.P. Comparative effectiveness of exercise and drug interventions on mortality outcomes: Metaepidemiological study. BMJ 2013, 347, f5577. [Google Scholar] [CrossRef] [Green Version]
- He, Y.; Li, X.; Gasevic, D.; Brunt, E.; McLachlan, F.; Millenson, M.; Timofeeva, M.; Ioannidis, J.P.; Campbell, H.; Theodoratou, E. Statins and Multiple Noncardiovascular Outcomes: Umbrella Review of Meta-analyses of Observational Studies and Randomized Controlled Trials. Ann. Intern. Med. 2018, 169, 543–553. [Google Scholar] [CrossRef]
- Chen, M.; Tang, T.C.; He, T.H.; Du, Y.J.; Qin, D.; Zheng, H. Management of haemorrhoids: Protocol of an umbrella review of systematic reviews and meta-analyses. BMJ Open 2020, 10, e035287. [Google Scholar] [CrossRef] [Green Version]
- Rosenberger, K.J.; Xu, C.; Lin, L. Methodological assessment of systematic reviews and meta-analyses on COVID-19: A meta-epidemiological study. J. Eval. Clin. Pract. 2021, 27, 1123–1133. [Google Scholar] [CrossRef]
| Evidence Classification | Detailed Criteria |
|---|---|
| Convincing (class I) | Associations with p < 10−6; having >1000 participants in a single meta-analysis; having low or moderate heterogeneity (I2 < 50%); having 95% PI 1 that excludes the null value; having no evidence of small-study effect; having no evidence of excess significance bias. |
| Highly suggestive (class II) | Associations with p < 10−6; having >1000 participants in a single meta-analysis; having low or moderate heterogeneity (I2 < 50%); having 95% PI that excludes the null value |
| Suggestive (class III) | Associations with p < 0.001 and having >1000 participants in a single meta-analysis. |
| Weak (class IV) | Remaining statistically significant associations with p < 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeh, T.-C.; Liang, C.-S.; Tsai, C.-K.; Solmi, M.; Lafer, B.; Tseng, P.-T.; Hsu, C.-W.; Lin, P.-Y.; Firth, J.; Stubbs, B.; et al. Neurological, Psychiatric, and Psychological Implications of the COVID-19 Pandemic: Protocol for a Large-Scale Umbrella Review of Observational Studies. Int. J. Environ. Res. Public Health 2022, 19, 1681. https://doi.org/10.3390/ijerph19031681
Yeh T-C, Liang C-S, Tsai C-K, Solmi M, Lafer B, Tseng P-T, Hsu C-W, Lin P-Y, Firth J, Stubbs B, et al. Neurological, Psychiatric, and Psychological Implications of the COVID-19 Pandemic: Protocol for a Large-Scale Umbrella Review of Observational Studies. International Journal of Environmental Research and Public Health. 2022; 19(3):1681. https://doi.org/10.3390/ijerph19031681
Chicago/Turabian StyleYeh, Ta-Chuan, Chih-Sung Liang, Chia-Kuang Tsai, Marco Solmi, Beny Lafer, Ping-Tao Tseng, Chih-Wei Hsu, Pao-Yen Lin, Joseph Firth, Brendon Stubbs, and et al. 2022. "Neurological, Psychiatric, and Psychological Implications of the COVID-19 Pandemic: Protocol for a Large-Scale Umbrella Review of Observational Studies" International Journal of Environmental Research and Public Health 19, no. 3: 1681. https://doi.org/10.3390/ijerph19031681
APA StyleYeh, T.-C., Liang, C.-S., Tsai, C.-K., Solmi, M., Lafer, B., Tseng, P.-T., Hsu, C.-W., Lin, P.-Y., Firth, J., Stubbs, B., Hassan, L., Fornaro, M., Vieta, E., Thompson, T., Shin, J., & Carvalho, A. F. (2022). Neurological, Psychiatric, and Psychological Implications of the COVID-19 Pandemic: Protocol for a Large-Scale Umbrella Review of Observational Studies. International Journal of Environmental Research and Public Health, 19(3), 1681. https://doi.org/10.3390/ijerph19031681










