COVID-19-Related Social Isolation Predispose to Problematic Internet and Online Video Gaming Use in Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Survey Sampling
2.3. Clinical Measures
2.4. Statistical Analysis
3. Results
3.1. Socio-Demographic and Clinical Characteristics
3.2. Problematic Internet Use
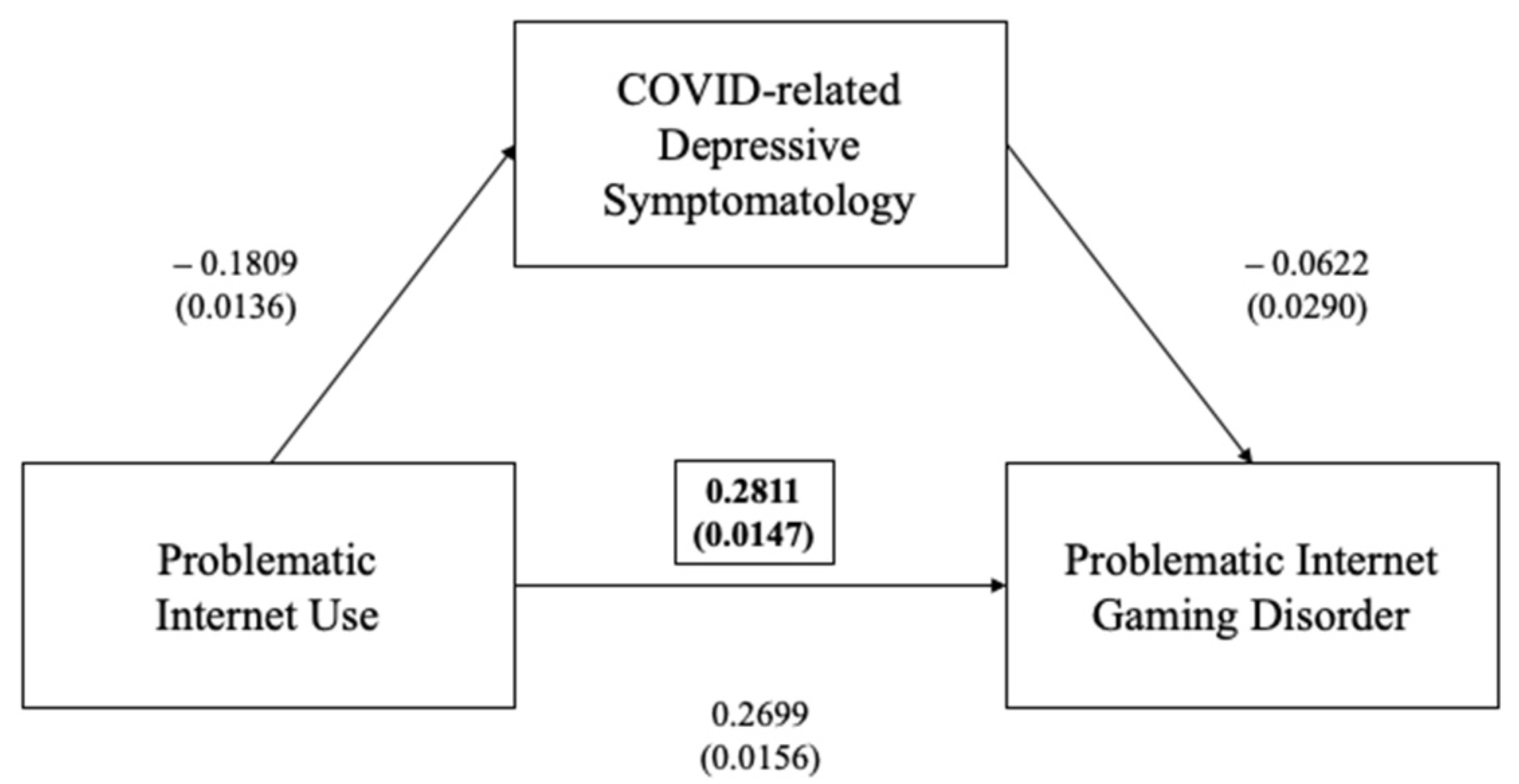
3.2.1. Problematic Internet Use and Videogaming
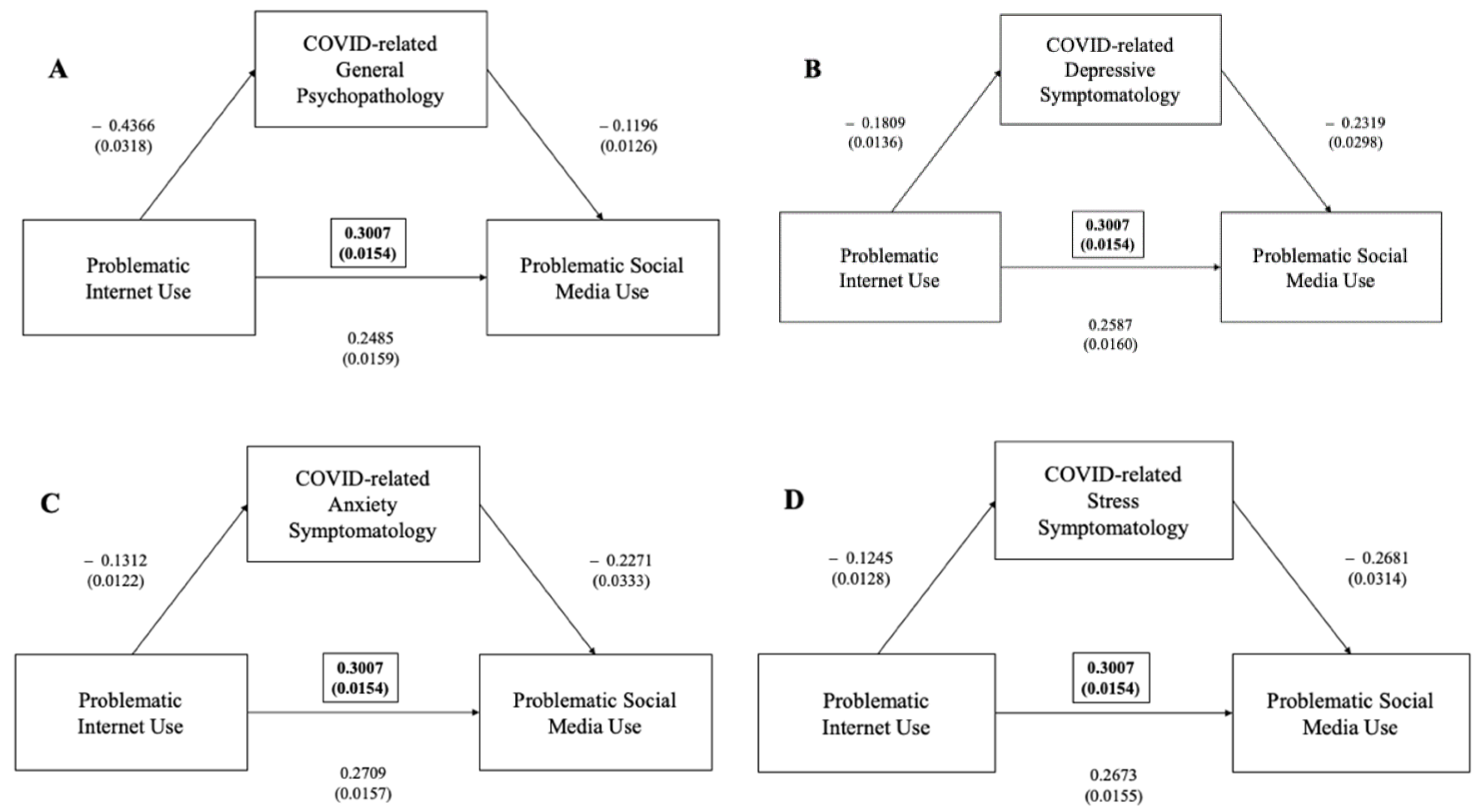
3.2.2. Problematic Internet Use and Problematic Social Media Use
3.3. Problematic Internet Gaming
3.3.1. Problematic Internet Gaming Disorder and Playing Videogames
3.3.2. Problematic Internet Gaming Disorder and Problematic Internet Use
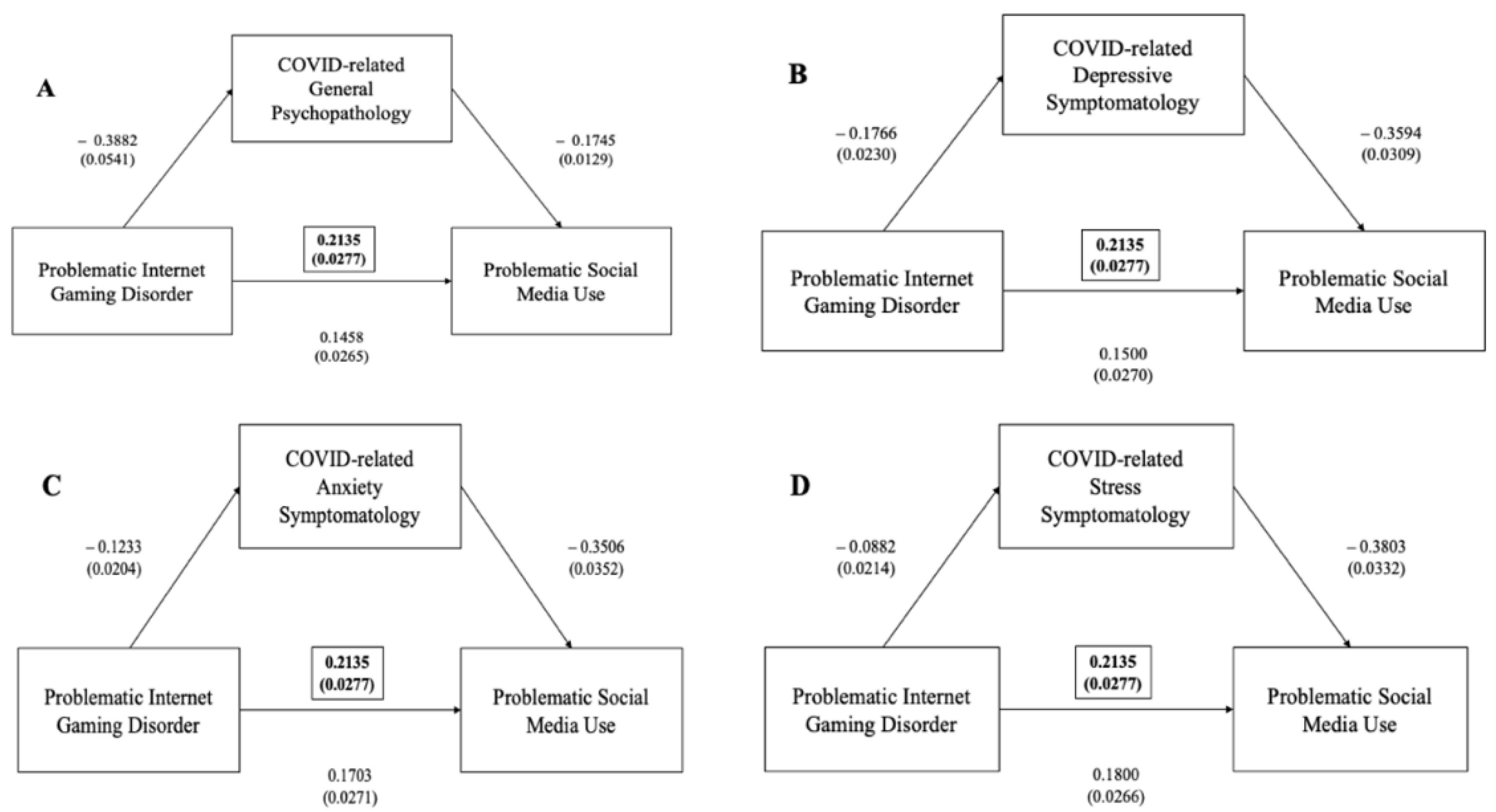
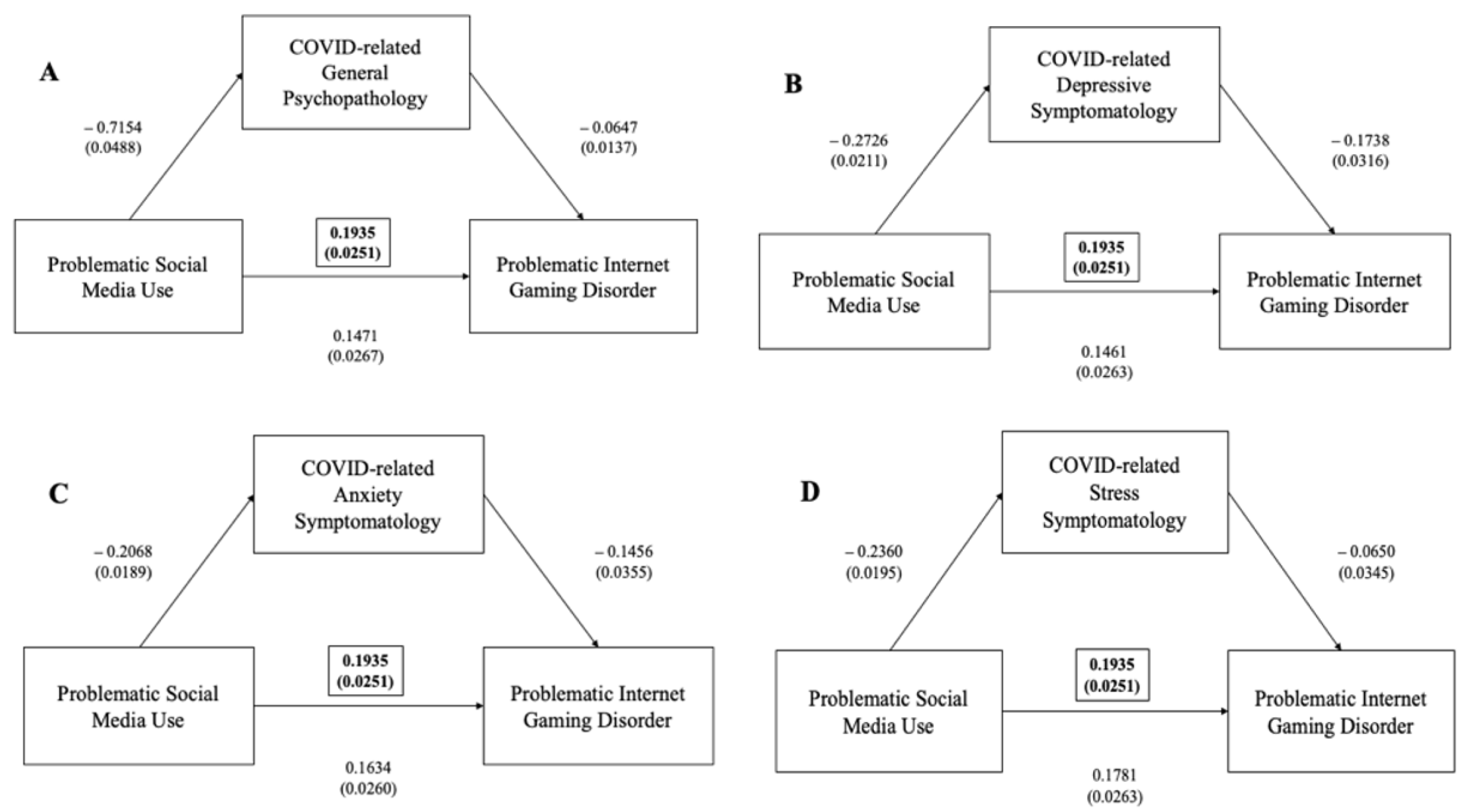
3.3.3. Problematic Internet Gaming Disorder and Problematic Social Media Use
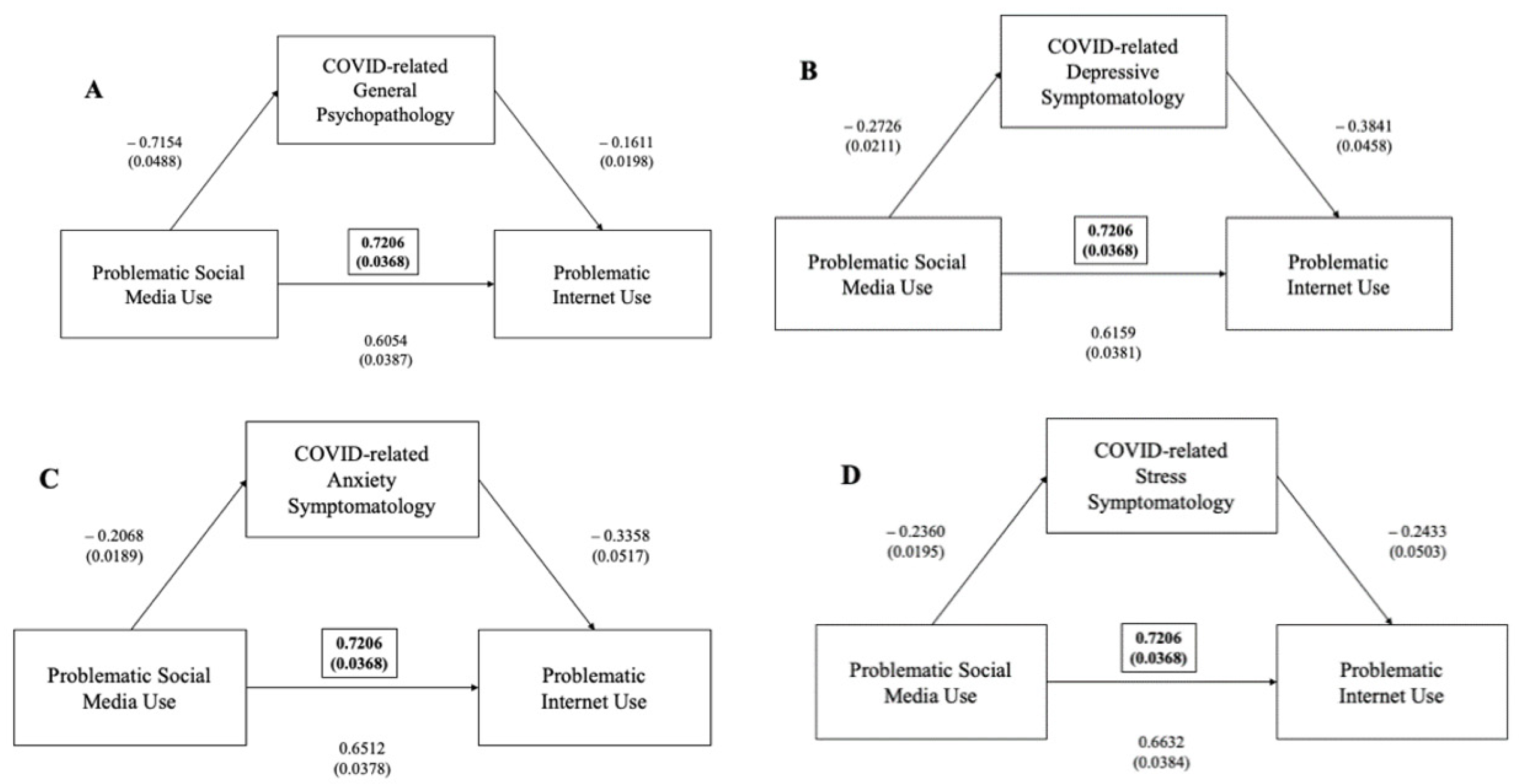
3.4. Problematic Social Media Use
Problematic Social Media Use, Internet and Videogaming
3.5. Binge Watching
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministero della Salute. COVID-19-Situazione in Italia. 2021. Available online: https://www.salute.gov.it (accessed on 20 May 2021).
- Percudani, M.; Corradin, M.; Moreno, M.; Indelicato, A.; Vita, A. Mental health services in Lombardy during COVID-19 outbreak. Psychiatry Res. 2020, 288, 112980. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization: WHO Announces COVID-19 Outbreak a Pandemic. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed on 20 May 2021).
- Abel, T.; McQueen, D. The COVID-19 pandemic calls for spatial distancing and social closeness: Not for social distancing! Int. J. Public Health 2020, 65, 231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holt-Lunstad, J. A pandemic of social isolation? World Psychiatry 2021, 20, 55–56. [Google Scholar] [CrossRef] [PubMed]
- Mucci, F.; Mucci, N.; Diolaiuti, F. Lock-down and isolation: Psychological aspects of COVID-19 pandemic in the general population. Clin. NeuroPsychiatry 2020, 17, 63–64. [Google Scholar] [PubMed]
- Ahrens, K.F.; Neumann, R.J.; Kollman, B.; Plichta, M.M.; Lieb, K.; Tüscher, O.; Reif, A. Differential impact of COVID-related lockdown on mental health in Germany. World Psychiatry 2021, 20, 140–141. [Google Scholar] [CrossRef] [PubMed]
- Unützer, J.; Kimmel, R.J.; Snowden, M. Psychiatry in the age of COVID-19. World Psychiatry 2020, 19, 130–131. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Gideon, J.R. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Caldarelli, G.; De Nicola, R.; Petrocchi, M.; Pratelli, M.; Saracco, F. Flow of online misinformation during the peak of the COVID-19 pandemic in Italy. EPJ Data Sci. 2021, 10, 34. [Google Scholar] [CrossRef]
- Guo, N.; Zhao, S.Z.; Weng, X.; Wu, Y.; Luk, T.T.; Wong, J.Y.H.; Lam, T.H.; Wang, M.P. Associations of COVID-19 online information sources and information overload with psychological distress symptoms: A population-based study. Transl. Behav. Med. 2021, 11, 1330–1338. [Google Scholar] [CrossRef]
- Beard, K.W.; Wolf, E.M. Modification in the proposed diagnostic criteria for Internet addiction. Cyberpsychol. Behav. 2001, 4, 377–383. [Google Scholar] [CrossRef]
- Naseri, L.; Mohamadi, J.; Sayehmiri, K.; Azizpoor, Y. Perceived social support, self-esteem, and Internet addiction among students of Al-Zahra University, Tehran, Iran. Iran. J. Psychiatry Behav. Sci. 2015, 9, e421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torous, J.; Choudhury, T.; Barnett, I.; Keshavan, M.; Kane, J. Smartphone relapse prediction in serious mental illness: A pathway towards personalized preventive care. World Psychiatry 2020, 19, 308–309. [Google Scholar] [CrossRef] [PubMed]
- Hickie, I.B. The role of new technologies in monitoring the evolution of psychopathology and providing measurement-based care in young people. World Psychiatry 2020, 19, 38–39. [Google Scholar] [CrossRef] [PubMed]
- Bozoglan, B.; Demirer, V.; Sahin, I. Loneliness, self-esteem, and life satisfaction as predictors of Internet addiction: A cross-sectional study among Turkish university students. Scand. J. Psychol. 2013, 54, 313–319. [Google Scholar] [CrossRef]
- Quinones, C.; Kakabadse, N.K. Self-concept clarity and compulsive Internet use: The role of preference for virtual interactions and employment status in British and North-American samples. J. Behav. Addict. 2015, 4, 289–298. [Google Scholar] [CrossRef] [Green Version]
- Yan, W.; Li, Y.; Sui, N. The relationship between recent stressful life events, personality traits, perceived family functioning and internet addiction among college students. Stress Health 2014, 30, 3–11. [Google Scholar] [CrossRef]
- King, D.L.; Delfabbro, P.H.; Billieux, J.; Potenza, M.N. Problematic online gaming and the COVID-19 pandemic. J. Behav. Addict. 2020, 9, 184–186. [Google Scholar] [CrossRef]
- Mestre-Bach, G.; Blycker, G.R.; Potenza, M.N. Pornography use in the setting of the COVID-19 pandemic. J. Behav. Addict. 2020, 9, 181–183. [Google Scholar] [CrossRef]
- Sun, Y.; Li, Y.; Bao, Y.; Meng, S.; Sun, Y.; Schumann, G.; Kosten, T.; Strang, J.; Lu, L.; Shi, J. Brief report: Increased addictive internet and substance use behavior during the COVID-19 pandemic in China. Am. J. Addict. 2020, 29, 268–270. [Google Scholar] [CrossRef]
- Alheneidi, H.; AlSumait, L.; AlSumait, D.; Smith, A.P. Loneliness and Problematic Internet Use during COVID-19 Lock-Down. Behav. Sci. 2021, 11, 5. [Google Scholar] [CrossRef]
- Lin, M.P. Prevalence of internet addiction during the COVID-19 outbreak and its risk factors among junior high school students in Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 8547. [Google Scholar] [CrossRef] [PubMed]
- Wiederhold, B.K. Social media use during social distancing. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 275–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiraly, O.; Griffiths, M.D.; Urban, R.; Farkas, J.; Kokonyei, G.; Elekes, Z.; Tamas, D.; Demetrovics, Z. Problematic internet use and problematic online gaming are not the same: Findings from a large nationally representative adolescent sample. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 749–754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Billieux, J.; Stein, D.J.; Castro-Calvo, J.; Higushi, S.; King, D.L. Rationale for and usefulness of the inclusion of gaming disorder in the ICD-11. World Psychiatry 2021, 20, 198–199. [Google Scholar] [CrossRef] [PubMed]
- Canale, N.; Marino, C.; Griffiths, M.D.; Scacchi, L.; Monaci, M.G.; Vieno, A. The association between problematic online gaming and perceived stress: The moderating effect of psychological resilience. J. Behav. Addict. 2019, 8, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Colder Carras, M.; Van Rooij, A.J.; Van de Mheen, D.; Musci, R.; Xue, Q.L.; Mendelson, T. Video gaming in a hyperconnected world: A cross-sectional study of heavy gaming, problematic gaming symptoms, and online socializing in adolescents. Comput. Hum. Behav. 2017, 68, 472–479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fiorillo, A.; Sampogna, G.; Giallonardo, V.; Del Vecchio, V.; Luciano, M.; Albert, U.; Carmassi, C.; Carra, G.; Cirulli, F.; Dell’Osso, B.; et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. Eur. Psychiatry 2020, 63, e87. [Google Scholar] [CrossRef] [PubMed]
- Giallonardo, V.; Sampogna, G.; Del Vecchio, V.; Luciano, M.; Albert, U.; Carmassi, C.; Carra, G.; Cirulli, F.; Dell’Osso, B.; Nanni, M.G.; et al. The impact of quarantine and physical distancing following COVID-19 on mental health: Study protocol of a multicentric Italian population trial. Front. Psychiatry 2020, 11, 533. [Google Scholar] [CrossRef] [PubMed]
- Marazziti, D.; Stahl, S.M. The relevance of COVID-19 pandemic to psychiatry. World Psychiatry 2020, 19, 261. [Google Scholar] [CrossRef]
- Janiri, D.; Moccia, L.; Dattoli, L.; Pepe, M.; Molinaro, M.; De Martin, V.; Chieffo, D.; Di Nicola, M.; Fiorillo, A.; Janiri, L.; et al. Emotional dysregulation mediates the impact of childhood trauma on psychological distress: First Italian data during the early phase of COVID-19 outbreak. Aust. N. Z. J. Psychiatry 2021, 9, 1071–1078. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Yang, Z.; Qiu, H.; Wang, Y.; Jian, L.; Ji, J.; Li, K. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry 2020, 19, 249–250. [Google Scholar] [CrossRef] [PubMed]
- Mei, Q.; Wang, F.; Bryant, A.; Wei, L.; Yuan, X.; Li, J. Mental health problems among COVID-19 survivors in Wuhan, China. World Psychiatry 2021, 20, 140–141. [Google Scholar] [CrossRef] [PubMed]
- Tyrer, P. COVID-19 health anxiety. World Psychiatry 2020, 19, 307–308. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, N.; Rafferty, L. Post-traumatic stress disorder in the aftermath of COVID-19 pandemic. World Psychiatry 2021, 20, 53–54. [Google Scholar] [CrossRef] [PubMed]
- Siste, K.; Hanafi, E.; Sen, L.T.; Christian, H.; Adrian; Siswidiani, L.P.; Limawan, A.P.; Murtani, B.J.; Suwartono, C. The impact of physical distancing and associated factors towards Internet addiction among adults in Indonesia during COVID-19 pandemic: A nationwide web-based study. Front. Psychiatry 2020, 11, 580977. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Zhu, K.; Xue, Q.; Zhou, Y.; Liu, Q.; Wu, H.; Wan, Z.; Zhang, J.; Meng, H.; Zhu, B.; et al. Problematic Internet use was associated with psychological problems among university students during COVID-19 outbreak in China. Front. Public Health 2021, 9, 675380. [Google Scholar] [CrossRef]
- Ritchie, K.; Chan, D. The emergence of cognitive COVID. World Psychiatry 2021, 20, 52–53. [Google Scholar] [CrossRef] [PubMed]
- Penninx, B.W.J.H. Psychiatric symptoms and cognitive impairment in “Long COVID”: The relevance of immunopsychiatry. World Psychiatry 2021, 20, 357–358. [Google Scholar] [CrossRef]
- Feldman, R. What is resilience: An affiliative neuroscience approach. World Psychiatry 2020, 19, 132–150. [Google Scholar] [CrossRef]
- World Medical Association (WPA). World Medical association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Fioravanti, G.; Casale, S. Evaluation of the psychometric properties of the Italian Internet Addiction Test. Cyberpsychol. Behav. Soc. Netw. 2015, 18, 120–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monacis, L.; Palo, V.; Griffiths, M.D.; Sinatra, M. Validation of the internet gaming disorder scale-short-form (IGDS9-SF) in an Italian-speaking sample. J. Behav. Addict. 2016, 5, 683–690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Bottesi, G.; Ghisi, M.; Altoe, G.; Conforti, E.; Melli, G.; Sica, C. The Italian version of the Depression Anxiety Stress Scales-21: Factor structure and psychometric properties on community and clinical samples. Compr. Psychiatry 2015, 60, 170–181. [Google Scholar] [CrossRef]
- Spinella, M. Normative data and a short form of the Barratt Impulsiveness Scale. Int. J. Neurosci. 2007, 117, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Patton, J.H.; Stanford, M.S.; Barratt, E.S. Factor structure of the Barratt impulsiveness scale. J. Clin. Psychol. 1995, 51, 768–774. [Google Scholar] [CrossRef]
- Orozco-Cabal, L.; Rodriguez, M.; Herin, D.V.; Gempeler, J.; Uribe, M. Validity and reliability of the abbreviated barratt impulsiveness scale in Spanish (BIS-15S). Rev. Colomb. Psiquiatr. 2010, 39, 93–109. [Google Scholar] [CrossRef] [Green Version]
- De Pasquale, C.; Sciacca, F.; Martinelli, V.; Chiappedi, M.; Dinaro, C.; Hichy, Z. Relationship of internet gaming disorder with psychopathology and social adaptation in Italian young adults. Int. J. Environ. Res. Public Health 2020, 17, 8201. [Google Scholar] [CrossRef]
- Fossati, A.; Maffei, C.; Cquarini, E.; Di Ceglie, A. Multigroup confirmatory component and factor analysis of the Italian version of the aggression questionnaire. Eur. J. Psychol. Assess. 2003, 19, 54–55. [Google Scholar] [CrossRef]
- Craparo, G.; Faraci, P.; Gori, A. Psychometric properties of the 20-item Toronto alexithymia scale in a group of Italian younger adolescents. Psychiatry Investig. 2015, 12, 500–507. [Google Scholar] [CrossRef] [Green Version]
- Monacis, L.; de Palo, V.; Griffiths, M.D.; Sinatra, M. Social networking addiction, attachment style, and validation of the Italian version of the Bergen Social Media Addiction Scale. J. Behav. Addict. 2017, 6, 178–186. [Google Scholar] [CrossRef] [Green Version]
- Hayes, A.F.; Preacher, K.J. Statistical mediation analysis with a multicategorical independent variable. Br. J. Math. Stat. Psychol. 2014, 67, 451–470. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- De Pasquale, C.; Chiappedi, M.; Sciacca, F.; Martinelli, V.; Hichy, Z. Online Videogames Use and Anxiety in Children during the COVID-19 Pandemic. Children 2021, 8, 205. [Google Scholar] [CrossRef] [PubMed]
- Menendez-García, A.; Jiménez-Arroyo, A.; Rodrigo-Yanguas, M.; Marin-Vila, M.; Sánchez-Sánchez, F.; Roman-Riechmann, E.; Blasco-Fontecilla, H. Internet, video game and mobile phone addiction in children and adolescents diagnosed with ADHD: A case-control study. Adicciones 2020, 1469. [Google Scholar] [CrossRef]
- First, M.B.; Gaebel, W.; Maj, M.; Stein, D.J.; Kogan, C.S.; Saunders, J.B.; Poznyak, V.B.; Gureje, O.G.; Lewis-Fernandez, R.; Maercker, A.; et al. An organization- and category-level comparison of diagnostic requirements for mental disorders in ICD-11 and DSM-5. World Psychiatry 2021, 20, 34–51. [Google Scholar] [CrossRef] [PubMed]
- Evren, C.; Evren, B.; Dalbudak, E.; Topcu, M.; Kutlu, N. Relationships of Internet addiction and Internet gaming disorder symptom severities with probable attention deficit/hyperactivity disorder, aggression and negative affect among university students. Attent. Defic. Hyperact. Disord. 2019, 11, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Zamboni, L.; Portoghese, I.; Congiu, A.; Carli, S.; Munari, R.; Federico, A.; Centoni, F.; Lodi Rizzini, A.; Lugoboni, F. Internet addiction and related clinical problems: A Study on Italian young adults. Front. Psychol. 2020, 11, 571638. [Google Scholar] [CrossRef] [PubMed]
- Poli, R.; Agrimi, E. Internet addiction disorder: Prevalence in an Italian student population. N. J. Psychiatry 2012, 66, 55–59. [Google Scholar] [CrossRef]
- Bianchini, V.; Cecilia, M.R.; Roncone, R.; Cofini, V. Prevalence and factors associated with problematic internet use: An Italian survey among l’Aquila students. Riv. Psichiatr. 2017, 52, 90–93. [Google Scholar]
- Ko, C.H.; Yen, J.Y.; Chen, C.S.; Chen, C.C.; Yen, C.F. Psychiatric comorbidity of internet addiction in college students: An interview study. CNS Spectr. 2008, 13, 147–153. [Google Scholar] [CrossRef]
- Wei, L.; Zhang, S.; Turel, O.; Bechara, A.; He, Q. A Tripartite neurocognitive model of internet gaming disorder. Front. Psychiatry 2017, 8, 285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perris, F.; Fabrazzo, M.; De Santis, V.; Luciano, M.; Sampogna, G.; Fiorillo, A.; Catapano, F. Comorbidity of obsessive-compulsive disorder and schizotypal personality disorder: Clinical response and treatment resistance to pharmacotherapy in a 3-year follow-up naturalistic study. Front. Psychiatry 2019, 10, 386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aboujaoude, E.; Gega, L.; Saltarelli, A.J. The retention challenge in remote therapy and learning seen through the lens of the COVID-19 pandemic. World Psychiatry 2021, 20, 138–139. [Google Scholar] [CrossRef]
- Di Carlo, F.; Pettorruso, M.; Alessi, M.C.; Picutti, E.; Collevecchio, R.; Migliara, G.; Baroni, G.; Gambi, F.; Cinosi, E. Characterizing the building blocks of Problematic Use of the Internet (PUI): The role of obsessional impulses and impulsivity traits among Italian young adults. Compr. Psychiatry 2021, 106, 152225. [Google Scholar] [CrossRef] [PubMed]
- Dalbudak, E.; Evren, C.; Topcu, M.; Aldemir, S.; Coskun, K.S.; Bozkurt, M.; Evren, B.; Canbal, M. Relationship of Internet addiction with impulsivity and severity of psychopathology among Turkish university students. Psychiatry Res. 2013, 210, 1086–1091. [Google Scholar] [CrossRef]
- Cao, F.; Su, L.; Liu, T.; Gao, X. The relationship between impulsivity and Internet addiction in a sample of Chinese adolescents. Eur. Psychiatry 2007, 22, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Torous, J.; Bucci, S.; Bell, L.H.; Kessing, L.V.; Faurholt-Jepsen, M.; Whelan, P.; Calvalho, A.F.; Keshavan, M.; Linardon, J.; Firth, J. The growing field of digital psychiatry: Current evidence and the future of apps, social media, chatbots, and virtual reality. World Psychiatry 2021, 20, 318–335. [Google Scholar] [CrossRef]
- Dong, H.; Yang, F.; Lu, X.; Hao, W. Internet addiction and related psychological factors among children and adolescents in China during the Coronavirus disease 2019 (COVID-19) epidemic. Front. Psychiatry 2020, 11, 00751. [Google Scholar] [CrossRef]
- Reynolds, C.F. Optimizing personalized management of depression: The importance of real-world contexts and the need for a new convergence paradigm in mental health. World Psychiatry 2020, 19, 266–268. [Google Scholar] [CrossRef]
- Maj, M.; Stein, D.J.; Parker, G.; Zimmerman, M.; Fava, G.A.; De Hert, M.; Demyttenaere, K.; McIntyre, R.S.; Widiger, T.; Wittchen, H.U. The clinical characterization of the adult patient with depression aimed at personalization of management. World Psychiatry 2020, 19, 269–293. [Google Scholar] [CrossRef]
- Jo, Y.S.; Bhang, S.Y.; Choi, J.S.; Lee, H.K.; Lee, S.Y.; Kweon, Y.S. Clinical characteristics of diagnosis for Internet gaming disorder: Comparison of DSM-5 IGD and ICD-11 GD diagnosis. J. Clin. Med. 2019, 8, 945. [Google Scholar] [CrossRef] [Green Version]
- Wasil, A.R.; Gillespie, S.; Schell, T.; Lorenzo-Luaces, L.; DeRubeis, R.J. Estimating the real-world usage of mobile apps for mental health: Development and application of two novel metrics. World Psychiatry 2021, 20, 137–138. [Google Scholar] [CrossRef] [PubMed]
- Wasil, A.R.; Weisz, J.R.; DeRubeis, R.J. Three questions to consider before developing a mental health app. World Psychiatry 2020, 19, 252–253. [Google Scholar] [CrossRef] [PubMed]
- Torous, J.; Andersson, G.; Bertagnoli, A.; Christensen, H.; Cuijpers, P.; Firth, J.; Haim, A.; Hsin, H.; Hollis, C.; Lewis, S.; et al. Towards a consensus around standards for smartphone apps and digital mental health. World Psychiatry 2019, 18, 97–98. [Google Scholar] [CrossRef] [PubMed]
- Kuss, D.J.; Griffiths, M.D.; Karila, L.; Billieux, J. Internet addiction: A systematic review of epidemiological research for the last decade. Curr. Pharm. Des. 2014, 20, 4026–4052. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.Y.; Lee, H.K.; Choo, H. Typology of Internet gaming disorder and its clinical implications. Psychiatry Clin. Neurosci. 2017, 71, 479–491. [Google Scholar] [CrossRef]
- Park, J.H.; Han, D.H.; Kim, B.N.; Cheong, J.H.; Lee, Y.S. Correlations among Social anxiety, self-esteem, impulsivity, and game genre in patients with problematic online game playing. Psychiatry Investig. 2016, 13, 297–304. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; Jeong, J.E.; Cho, H.; Jung, D.J.; Kwak, M.; Rho, M.J.; Yu, H.; Kim, D.-J.; Choi, I.Y. Personality factors predicting smartphone addiction predisposition: Behavioral inhibition and activation systems, impulsivity, and self-control. PLoS ONE 2016, 11, e0159788. [Google Scholar] [CrossRef]
- T’Ng, S.T.; Ho, K.H.; Sim, D.E.; Yu, C.H.; Wong, P.Y. The mediating effect of Internet gaming disorder’s symptoms on loneliness and aggression among undergraduate students and working adults in Malaysia. PsyCh J. 2020, 9, 96–107. [Google Scholar] [CrossRef]
- Mahmood, Q.K.; Jafree, S.R.; Mukhtar, S.; Fischer, F. Social media use, self-efficacy, perceived threat, and preventive behavior in times of COVID-19: Results of a cross-sectional study in Pakistan. Front. Psychol. 2021, 12, 562042. [Google Scholar] [CrossRef]
- Brailovskaia, J.; Truskauskaite-Kuneviciene, I.; Margraf, J.; Kazlauskas, E. Coronavirus (COVID-19) outbreak: Addictive social media use, depression, anxiety and stress in quarantine-an exploratory study in Germany and Lithuania. J. Affect. Disord. Rep. 2021, 5, 100182. [Google Scholar] [CrossRef] [PubMed]
- Pompili, M.; Innamorati, M.; Sampogna, G.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Erbuto, D.; Luciano, M.; Nanni, M.G.; et al. The impact of COVID-19 on unemployment across Italy: Consequences for those affected by psychiatric conditions. J. Affect. Disord. 2021, 296, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Sampogna, G.; Del Vecchio, V.; Giallonardo, V.; Luciano, M.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Dell’Osso, B.; Menculini, G.; et al. What Is the Role of Resilience and Coping Strategies on the Mental Health of the General Population during the COVID-19 Pandemic? Results from the Italian Multicentric COMET Study. Brain Sci. 2021, 17, 1231. [Google Scholar] [CrossRef]
- Wetzel, B.; Pryss, R.; Baumeister, H.; Edler, J.S.; Gonçalves, A.S.O.; Cohrdes, C. “How Come You Don’t Call Me?” Smartphone communication app usage as an indicator of loneliness and social well-being across the adult lifespan during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 6212. [Google Scholar] [CrossRef] [PubMed]
- Moccia, L.; Janiri, D.; Pepe, M.; Dattoli, L.; Molinaro, M.; De Martin, V.; Chieffo, D.; Janiri, L.; Fiorillo, A.; Sani, G.; et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: An early report on the Italian general population. Brain Behav. Immun. 2020, 87, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.A.; Kanba, S.; Teo, A.R. Defining pathological social withdrawal: Proposed diagnostic criteria for hikikomori. World Psychiatry 2020, 19, 116–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rooksby, M.; Furuhashi, T.; McLeod, H.J. Hikikomori: A hidden mental health need following the COVID-19 pandemic. World Psychiatry 2020, 19, 399–400. [Google Scholar] [CrossRef] [PubMed]
- Rojnic Kuzman, M.; Vahip, S.; Fiorillo, A.; Beezhold, J.; Pinto da Costa, M.; Skugarevsky, O.; Dom, G.; Pajevic, I.; Peles, A.M.; Mohr, P.; et al. Mental health services during the first wave of the COVID-19 pandemic in Europe: Results from the EPA Ambassadors Survey and implications for clinical practice. Eur. Psychiatry 2021, 9, e41. [Google Scholar] [CrossRef] [PubMed]
- Adhanom Ghebreyesus, T. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry 2020, 19, 129–130. [Google Scholar] [CrossRef]
- Stewart, D.E.; Appelbaum, P.S. COVID-19 and psychiatrists’ responsibilities: A WPA position paper. World Psychiatry 2020, 19, 406–407. [Google Scholar] [CrossRef]
- Gorwood, P.; Fiorillo, A. One year after the COVID-19: What have we learnt, what shall we do next? Eur. Psychiatry 2021, 64, e15. [Google Scholar] [CrossRef] [PubMed]
- De Hert, M.; Mazereel, V.; Detraux, J.; Van Assche, K. Prioritizing COVID-19 vaccination for people with severe mental illness. World Psychiatry 2021, 20, 54–55. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, Q.; Davis, P.B.; Volkow, N.D.; Xu, R. Increased risk for COVID-19 breakthrough infection in fully vaccinated patients with substance use disorders in the United States between December 2020 and August 2021. World Psychiatry 2021, 21, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Wasserman, D.; Iosue, M.; Westefeld, A.; Carli, V. Adaptation of evidence-based suicide prevention strategies during and after the COVID-19 pandemic. World Psychiatry 2020, 19, 294–306. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Lee, Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry 2020, 19, 250–251. [Google Scholar] [CrossRef]
- Brown, S. Perinatal mental health and the COVID-19 pandemic. World Psychiatry 2020, 19, 333–334. [Google Scholar] [CrossRef]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 2020, 63, e32. [Google Scholar] [CrossRef] [Green Version]
- Berry, H.L. Enabling a youth- and mental health-sensitive greener post-pandemic recovery. World Psychiatry 2021, 20, 152–153. [Google Scholar] [CrossRef]
- Ijzerman, H.; Lewis, N.A., Jr.; Przybylski, A.K.; Weinstein, N.; DeBruine, L.; Ritchie, S.J.; Vazire, S.; Forscher, P.S.; Morey, R.D.; Ivory, J.D.; et al. Use caution when applying behavioural science to policy. Nat. Hum. Behav. 2020, 4, 1092–1094. [Google Scholar] [CrossRef]



| Age, Years, Mean ± SD | 32.5 ± 12.9 |
| 18–19 years old, % (n) | 3.7% (52) |
| 20–24 years old, % (n) | 31.7% (439) |
| 25–29 years old, % (n) | 22.1% (306) |
| 30–39 years old, % (n) | 18.5% (256) |
| ≥40 years old, % (n) | 24.0% (332) |
| Gender, % (n) | |
| Female | 62.5% (865) |
| Male | 37.5% (520) |
| Marital status, % (n) | |
| Single | 59.7% (827) |
| Married or cohabiting | 36.4% (504) |
| Separated or divorced | 3.3% (46) |
| Widowed | 0.6% (8) |
| Education level, % (n) | |
| University degree, % (n) | 52.3% (724) |
| High school degree, % (n) | 46.6% (645) |
| Middle school, % (n) | 1.1% (15) |
| Elementary school, % (n) | 0.1% (1) |
| Employment level, % (n) | |
| Full-time employed, % (n) | 32.7% (453) |
| Unemployed, % (n) | 3.6% (50) |
| Student, % (n) | 47.7% (661) |
| Full-time homemaker, % (n) | 7.7% (106) |
| Lost job due to the pandemic, % (n) | 4.1% (57) |
| Any comorbid physical condition(s), % (n) | 10.5% (146) |
| Any mental health problem(s), % (n) | 6% (83) |
| Have you been infected by COVID-19, % (n) | 1.4% (19) |
| Have you been isolated due to COVID-19 infection, % (n) | 1.9% (27) |
| Have you been hospitalized due to COVID-19 infection, % (n) | 0.1% (2) |
| Have you been isolated due to a contact with someone affected by COVID-19, % (n) | 4% (56) |
| Have you played any video games in the last 12 months, % (n) | 60.4% (836) |
| Are you a professional video gamer, % (n) | 2.5% (34) |
| Hours per week in video gaming, mean ± SD | 4.2 ± 9.8 |
| Device used in video gaming, % (n) | |
| Computer, % (n) | 26.4% (366) |
| Smartphone, % (n) | 58.9% (816) |
| TV, % (n) | 14.7% (203) |
| IAT Total Score, Mean ± SD (Range: 0–100) | 46.5 ± 10.2 |
| Normal level of internet usage (range: 0–30), n (%) | 23 (1.6%) |
| Mild level of internet usage (range: 31–49), n (%) | 893 (64.5%) |
| Moderate level of internet usage (range: 50–79), n (%) | 458 (33.1%) |
| Severe level of internet usage (range: 80–100), n (%) | 11 (0.8%) |
| IAT, Salience subscale, mean ± SD | 8.9 ± 3.5 |
| IAT, Excessive Use subscale, mean ± SD | 11.1 ± 3.8 |
| IAT, Neglect Work subscale, mean ± SD | 6.4 ± 2.9 |
| IAT, Anticipation subscale, mean ± SD | 4.7 ± 1.9 |
| IAT, Lack of Control subscale, mean ± SD | 11.8 ± 2.6 |
| IAT, Neglect Social Life subscale, mean ± SD | 3.5 ± 1.6 |
| IGD9-SF total score, mean ± SD (range: 9–45) | 13.1 ± 6.3 |
| Normal level (range: 9–20), n (%) | 1194 (86.2%) |
| Pathological level (range: ≥21), n (%) | 191 (13.8%) |
| DASS-21, Stress subscale, mean ± SD | 16.8 ± 5.0 |
| Normal (range: 0–10), n (%) | 115 (8.3%) |
| Mild (range: 11–18), n (%) | 807 (58.3%) |
| Moderate (range: 19–26), n (%) | 353 (25.5%) |
| Severe (range 27–34), n (%) | 110 (7.9%) |
| Extremely severe (range: 35–42), n (%) | 0 (0%) |
| BIS-15 total score, mean ± SD (range: 15–60) | 39.3 ± 7.5 |
| BIS-15, Attentional Impulsiveness subscale, mean ± SD | 11.2 ± 3.5 |
| BIS-15, Motor Impulsiveness subscale, mean ± SD | 12.7 ± 4.5 |
| BIS-15, Nonplanning Impulsiveness subscale, mean ± SD | 10.7 ± 2.4 |
| Social Adjustment Index (SAI), SASS total score, mean ± SD (range: 0–60) | 49.6 ± 5.2 |
| Normal (range: 35–52), n (%) | 896 (64.7%) |
| Better functioning (range: ≥52), n (%) | 489 (35.3%) |
| Social maladjustment (range: <25), n (%) | 0 (0%) |
| AQ total score, mean ± SD (range: 29–145) | 97.7 ± 14.8 |
| AQ, Physical Aggression subscale, mean ± SD | 34.4 ± 5.1 |
| AQ, Verbal Aggression subscale, mean ± SD | 13.3 ± 3.8 |
| AQ, Anger subscale, mean ± SD | 24.9 ± 5.0 |
| AQ, Hostility subscale, mean ± SD | 25.1 ± 6.6 |
| TAS-20 total score, mean ± SD | 53.6 ± 9.5 |
| Non-alexithymia (range: ≤51), n (%) | 572 (41.3%) |
| Possible alexithymia (range: 52–60), n (%) | 496 (35.8%) |
| Alexithymia (range: ≥61), n (%) | 317 (22.9%) |
| TAS-20, Difficulty Describing Feelings subscale, mean ± SD | 14.5 ± 4.4 |
| TAS-20, Difficulty Identifying Feelings subscale, mean ± SD | 20.0 ± 4.9 |
| TAS-20, Externally-Oriented Thinking subscale, mean ± SD | 19.1 ± 4.3 |
| BSMAS total score, mean ± SD | 20.5 ± 6.6 |
| Pathological level (range: ≥16), n (%) | 1078 (77.8%) |
| Binge Watching scale total score, mean ± SD | 20.2 ± 9.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Volpe, U.; Orsolini, L.; Salvi, V.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Dell’Osso, B.; Luciano, M.; Menculini, G.; et al. COVID-19-Related Social Isolation Predispose to Problematic Internet and Online Video Gaming Use in Italy. Int. J. Environ. Res. Public Health 2022, 19, 1539. https://doi.org/10.3390/ijerph19031539
Volpe U, Orsolini L, Salvi V, Albert U, Carmassi C, Carrà G, Cirulli F, Dell’Osso B, Luciano M, Menculini G, et al. COVID-19-Related Social Isolation Predispose to Problematic Internet and Online Video Gaming Use in Italy. International Journal of Environmental Research and Public Health. 2022; 19(3):1539. https://doi.org/10.3390/ijerph19031539
Chicago/Turabian StyleVolpe, Umberto, Laura Orsolini, Virginio Salvi, Umberto Albert, Claudia Carmassi, Giuseppe Carrà, Francesca Cirulli, Bernardo Dell’Osso, Mario Luciano, Giulia Menculini, and et al. 2022. "COVID-19-Related Social Isolation Predispose to Problematic Internet and Online Video Gaming Use in Italy" International Journal of Environmental Research and Public Health 19, no. 3: 1539. https://doi.org/10.3390/ijerph19031539
APA StyleVolpe, U., Orsolini, L., Salvi, V., Albert, U., Carmassi, C., Carrà, G., Cirulli, F., Dell’Osso, B., Luciano, M., Menculini, G., Nanni, M. G., Pompili, M., Sani, G., Sampogna, G., Group, W., & Fiorillo, A. (2022). COVID-19-Related Social Isolation Predispose to Problematic Internet and Online Video Gaming Use in Italy. International Journal of Environmental Research and Public Health, 19(3), 1539. https://doi.org/10.3390/ijerph19031539













