Changes in the Retail Food Environment in Mexican Cities and Their Association with Blood Pressure Outcomes
Abstract
1. Introduction
The Retail Food Environment
2. Materials and Methods
2.1. Setting
2.2. Data Sources
2.2.1. Individual-Level Data
2.2.2. Retail Food Environment Data
2.3. Measures
2.3.1. Blood Pressure
2.3.2. Food Store Density Changes
2.3.3. Individual-Level Covariates
2.3.4. Area-Level Covariates
2.4. Analytic Strategy
3. Results
3.1. Descriptive Statistics
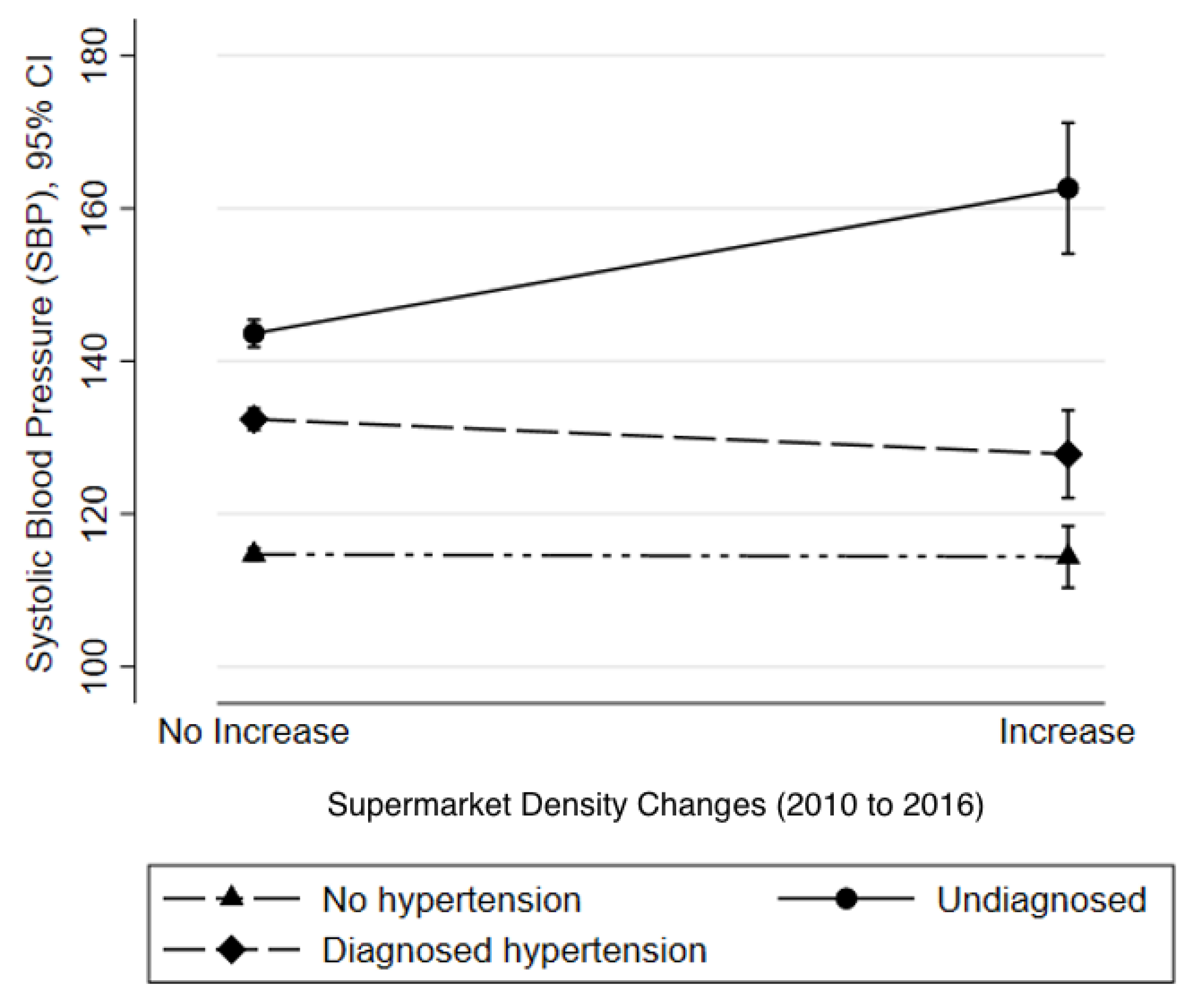
3.2. Multilevel Linear Regression
4. Discussion
4.1. Sensitivity Analysis
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Food Store Type | NAICS Code |
|---|---|
| Fruit and vegetable stores | 461130 |
| Supermarkets | 462,111 minus ‘chain convenience stores’ (see below) |
| Small food retail | 461,110 (small grocery stores) + 461,213 (non-alcoholic beverage stores) + 462,112 (minimarkets) minus ‘chain convenience stores’ |
| Fresh food retail | 46,112 (meat, poultry & fish shops) + 461,150 (dairy shops) + 461,140 (stores selling grains and seeds) |
| Chain convenience stores | Searched by name because NAICS does not identified them as a distinct store format. Names searched: OXXO, 7-Eleven, Extra, Circle K, Bodega Aurrera Express, and Chedraui Supercito |
Appendix B
| Density Change | Sample Size (n = 2512) | Hypertension (n = 553) | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|---|
| Fruit and vegetable shops | |||||
| (1) No change | 922 | 197 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| (2) Decline | 590 | 148 | 1.23 (0.90, 1.67) | 1.17 (0.87, 1.60) | 1.12 (0.83, 1.52) |
| (3) Increase | 1000 | 208 | 0.98 (0.75, 1.30) | 1.03 (0.79, 1.35) | 1.00 (0.77, 1.31) |
| Convenience stores | |||||
| (1) No change | 2030 | 448 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| (2) Increase | 482 | 105 | 1.01 (0.87, 1.17) | 1.03 (0.89, 1.19) | 0.97 (0.85, 1.13) |
| Supermarkets (large) | |||||
| (1) No change | 2410 | 528 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| (2) Increase | 102 | 25 | 1.09 (0.81, 1.47) | 0.90 (0.72, 1.12) | 1.05 (0.79, 1.40) |
References
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef]
- Miranda, J.J.; Barrientos-Gutiérrez, T.; Corvalan, C.; Hyder, A.A.; Lazo-Porras, M.; Oni, T.; Wells, J.C.K. Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat. Med. 2019, 25, 1667–1679. [Google Scholar] [CrossRef] [PubMed]
- Dávila-Cervantes, C.A. Cardiovascular disease in Mexico 1990–2017: Secondary data analysis from the global burden of disease study. Int. J. Public Health 2020, 65, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Campos, I.; Hernández-Barrera, L.; Pedroza-Tobías, A.; Medina, C.; Barquera, S. Hipertensión arterial en adultos mexicanos: Prevalencia, diagnóstico y tipo de tratamiento. Ensanut MC 2016. Salud Pública México 2018, 60, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Reardon, T. Obesity and the food system transformation in Latin America. Obes. Rev. 2018, 19, 1028–1064. [Google Scholar] [CrossRef]
- Vandevijvere, S.; Barquera, S.; Caceres, G.; Corvalan, C.; Karupaiah, T.; Kroker-Lobos, M.F.; L’Abbé, M.; Ng, S.H.; Phulkerd, S.; Ramirez-Zea, M.; et al. An 11-country study to benchmark the implementation of recommended nutrition policies by national governments using the Healthy Food Environment Policy Index, 2015–2018. Obes. Rev. 2019, 20, 57–66. [Google Scholar] [CrossRef]
- Basto-Abreu, A.; Torres-Alvarez, R.; Reyes-Sánchez, F.; González-Morales, R.; Canto-Osorio, F.; Colchero, M.A.; Barquera, S.; Rivera, J.A.; Barrientos-Gutierrez, T. Predicting obesity reduction after implementing warning labels in Mexico: A modeling study. PLoS Med. 2020, 17, e1003221. [Google Scholar] [CrossRef]
- Rivera, J.A.; Barquera, M.S.; González-Cossío, M.T.; Olaiz, M.G.; Sepúlveda, M.J. Nutrition Transition in Mexico and in Other Latin American Countries. Nutr. Rev. 2004, 62, S149–S157. [Google Scholar] [CrossRef]
- Secretaria de gobernación. MODIFICACIÓN a la Norma Oficial Mexicana NOM-051-SCFI/SSA1-2010, Especificaciones Generales de Etiquetado Para Alimentos y Bebidas no Alcohólicas Preenvasados-Información Comercial y Sanitaria, Publicada el 5 de Abril de 2010 [Internet]. Secretaria de Economia; 2020 [cited 15 January 2020]. Available online: https://www.dof.gob.mx/2020/SEECO/NOM_051.pdf (accessed on 17 January 2022).
- Ni Mhurchu, C.; Vandevijvere, S.; Waterlander, W.; Thornton, L.; Kelly, B.; Cameron, A.; Snowdon, W.; Swinburn, B. Informas Monitoring the availability of healthy and unhealthy foods and non-alcoholic beverages in community and consumer retail food environments globally. Obes. Rev. 2013, 14, 108–119. [Google Scholar] [CrossRef]
- Turner, C.; Kalamatianou, S.; Drewnowski, A.; Kulkarni, B.; Kinra, S.; Kadiyala, S. Food Environment Research in Low- and Middle-Income Countries: A Systematic Scoping Review. Adv. Nutr. 2020, 11, 387–397. [Google Scholar] [CrossRef]
- Hawkes, C. Dietary Implications of Supermarket Development: A Global Perspective. Dev. Policy Rev. 2008, 26, 657–692. [Google Scholar] [CrossRef]
- Popkin, B.M. Nutrition Transition and the Global Diabetes Epidemic. Curr. Diabetes Rep. 2015, 15, 64. [Google Scholar] [CrossRef] [PubMed]
- Machado, P.P.; Claro, R.M.; Martins, A.P.B.; Costa, J.C.; Levy, R.B. Is food store type associated with the consumption of ultra-processed food and drink products in Brazil? Public Health Nutr. 2018, 21, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Clark, S.E.; Hawkes, C.; Murphy, S.M.E.; Hansen-Kuhn, K.A.; Wallinga, D. Exporting obesity: US farm and trade policy and the transformation of the Mexican consumer food environment. Int. J. Occup. Environ. Health 2012, 18, 53–64. [Google Scholar] [CrossRef]
- Hernández-F, M.; Figueroa, J.L.; Colchero, M.A. Association between density of stores and purchases of ultra-processed food and sugar-sweetened beverages in Mexico. Health Place 2021, 68, 102528. [Google Scholar] [CrossRef]
- Nieto, C.; Rodríguez, E.; Sánchez-Bazán, K.; Tolentino-Mayo, L.; Carriedo-Lutzenkirchen, A.; Vandevijvere, S.; Barquera, S. The INFORMAS healthy food environment policy index (Food-EPI) in Mexico: An assessment of implementation gaps and priority recommendations. Obes. Rev. 2019, 20, 67–77. [Google Scholar] [CrossRef]
- da Cousta Louzada, M.L.; Martins, A.P.B.; Canella, D.S.; Baraldi, L.G.; Levy, R.B.; Claro, R.M.; Moubarac, J.-C.; Cannon, G.; Monteiro, C.A. Ultra-Processed Foods and the Nutritional Dietary Profile in Brazil. Rev. Saude Publica 2015, 49, 38. [Google Scholar] [CrossRef]
- Tavares, L.F.; Fonseca, S.C.; Garcia Rosa, M.L.; Yokoo, E.M. Relationship between Ultra-Processed Foods and Metabolic Syndrome in Adolescents from a Brazilian Family Doctor Program. Public Health Nutr. 2012, 15, 82–87. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.-C.; Louzada, M.L.C.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-Processed Foods: What They Are and How to Identify Them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Duran, A.C.; Roux, A.V.D.; Latorre, M.D.R.D.; Jaime, P. Neighborhood socioeconomic characteristics and differences in the availability of healthy food stores and restaurants in Sao Paulo, Brazil. Health Place 2013, 23, 39–47. [Google Scholar] [CrossRef]
- Molina, M.; Serván-Mori, E.; Quezada, A.D.; Colchero, M.A. Is there a link between availability of food and beverage establishments and BMI in Mexican adults? Public Health Nutr. 2017, 20, 3326–3332. [Google Scholar] [CrossRef][Green Version]
- Duran, A.C.; de Almeida, S.L.; Latorre, M.D.R.D.; Jaime, P.C. The role of the local retail food environment in fruit, vegetable and sugar-sweetened beverage consumption in Brazil. Public Health Nutr. 2016, 19, 1093–1102. [Google Scholar] [CrossRef] [PubMed]
- Jaime, P.C.; Duran, A.C.; Sarti, F.M.; Lock, K. Investigating Environmental Determinants of Diet, Physical Activity, and Overweight among Adults in Sao Paulo, Brazil. J. Hered. 2011, 88, 567–581. [Google Scholar] [CrossRef] [PubMed]
- Barrera, L.H.; Rothenberg, S.J.; Barquera, S.; Cifuentes, E. The Toxic Food Environment Around Elementary Schools and Childhood Obesity in Mexican Cities. Am. J. Prev. Med. 2016, 51, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Ferrer, C.; Auchincloss, A.H.; de Menezes, M.C.; Kroker-Lobos, M.F.; Cardoso, L.D.O.; Barrientos-Gutierrez, T. The food environment in Latin America: A systematic review with a focus on environments relevant to obesity and related chronic diseases. Public Health Nutr. 2019, 22, 3447–3464. [Google Scholar] [CrossRef]
- Pérez-Ferrer, C.; Auchincloss, A.H.; Barrientos-Gutierrez, T.; Colchero, M.A.; Cardoso, L.D.O.; de Menezes, M.C.; Bilal, U. Longitudinal changes in the retail food environment in Mexico and their association with diabetes. Health Place 2020, 66, 102461. [Google Scholar] [CrossRef]
- Pineda, E.; Brunner, E.J.; Llewellyn, C.H.; Mindell, J.S. The retail food environment and its association with body mass index in Mexico. Int. J. Obes. 2021, 45, 1215–1228. [Google Scholar] [CrossRef]
- Nieto, C.; Tolentino-Mayo, L.; Medina, C.; Monterrubio-Flores, E.; Denova-Gutiérrez, E.; Barquera, S. Sodium Content of Processed Foods Available in the Mexican Market. Nutrients 2018, 10, 2008. [Google Scholar] [CrossRef]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; Lefevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef]
- Quistberg, D.A.; the SALURBAL Group; Roux, A.V.D.; Bilal, U.; Moore, K.; Ortigoza, A.; Rodriguez, D.A.; Sarmiento, O.L.; Frenz, P.; Friche, A.A.; et al. Building a Data Platform for Cross-Country Urban Health Studies: The SALURBAL Study. J. Hered. 2018, 96, 311–337. [Google Scholar] [CrossRef]
- Roux, A.V.D.; Slesinski, S.C.; Alazraqui, M.; Caiaffa, W.T.; Frenz, P.; Fuchs, R.J.; Miranda, J.J.; Rodriguez, D.A.; Dueñas, O.L.S.; Siri, J.; et al. A Novel International Partnership for Actionable Evidence on Urban Health in Latin America: LAC-Urban Health and SALURBAL. Glob. Chall. 2018, 3, 1800013. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Geografía y Estadística. Principales Resultados Por AGEB y Manzana Urbana 2010. Available online: https://datos.gob.mx/busca/dataset/censo-de-poblacion-y-vivienda-2010-principales-resultados-por-ageb-y-manzana-urbana (accessed on 17 January 2022).
- Romero-Martínez, M.; Shamah-Levy, T.; Cuevas-Nasu, L.; Humaran, I.M.G.; Pineda, E.B.G.; Acosta, L.M.G.; Rivera-Dommarco, J.Á.; Hernández-Ávila, M. Diseño metodológico de la Encuesta Nacional de Salud y Nutrición de Medio Camino 2016. Salud Pública México 2017, 59, 299–305. [Google Scholar] [CrossRef] [PubMed]
- United Nations Economic Commission for Europe. National Statistical Directory of Economic Units (DENUE) Mexico. 2011. Available online: https://www.unece.org/fileadmin/DAM/stats/documents/ece/ces/ge.42/2011/mtg1/Mexico_nationalstatistics.pdf (accessed on 17 January 2022).
- Instituto Nacional de Geografía y Estadística. Manual de Cartografía Geostadística. 2010. Available online: https://www.inegi.org.mx/contenidos/temas/mapas/mg/metadatos/manual_cartografia_censal.pdf (accessed on 17 January 2022).
- United States Census Bureau. North American Industry Classification System. 2017. Available online: https://www.census.gov/eos/www/naics/ (accessed on 1 March 2019).
- America Retail. México: Proximidad y Precio, Factores que Atraen Clientes. 2018. Available online: https://www.america-retail.com/mexico/mexico-proximidad-y-precio-factores-que-atraen-clientes-euromonitor/ (accessed on 17 January 2022).
- Howe, L.D.; Galobardes, B.; Matijasevich, A.; Gordon, D.; Johnston, D.; Onwujekwe, O.; Patel, R.; Webb, E.; Lawlor, A.D.; Hargreaves, J.R. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: A methods of measurement in epidemiology paper. Int. J. Epidemiol. 2012, 41, 871–886. [Google Scholar] [CrossRef] [PubMed]
- Consejo Nacional de Población. Indice de Marginación Urbana 2010. Available online: http://www.conapo.gob.mx/work/models/CONAPO/indices_margina/marginacion_urbana/AnexoA/Documento/04A_AGEB.pdf (accessed on 17 January 2022).
- Stata Statistical Software; Release 16 [computer program]; StateCorp LLC: College Station, TX, USA, 2019.
- Carle, A.C. Fitting multilevel models in complex survey data with design weights: Recommendations. BMC Med. Res. Methodol. 2009, 9, 1–13. [Google Scholar] [CrossRef]
- USDA Foreign Agricultural Service. Mexico Retail Foods. 2016 Annual Report. Global Agricultural Information Network (GAIN). 2016. Available online: https://apps.fas.usda.gov/newgainapi/api/report/downloadreportbyfilename?filename=Retail%20Foods_Mexico%20City%20ATO_Mexico_12-30-2016.pdf (accessed on 17 January 2022).
- Zavala, G.A.; Tenorio-Palos, Y.; Campos-Ponce, M.; Elton-Puente, J.E.; López-González, C.A.; Doak, C.M.; Rosado, J.L.; García, O.P. Proximity and High Density of Convenience Stores Was Associated with Obesity in Children of a Rural Community of Mexico: Using a Geographic Information System Approach. Food Nutr. Bull. 2021, 42, 490–501. [Google Scholar] [CrossRef]
- Ghosh-Dastidar, M.; Hunter, G.; Collins, R.L.; Zenk, S.N.; Cummins, S.; Beckman, R.; Nugroho, A.K.; Sloan, J.C.; Wagner, L.; Dubowitz, T. Does opening a supermarket in a food desert change the food environment? Health Place 2017, 46, 249–256. [Google Scholar] [CrossRef]
- Mayne, S.L.; Auchincloss, A.H.; Michael, Y.L. Impact of policy and built environment changes on obesity-related out-comes: A systematic review of naturally occurring experiments. Obes. Rev. 2015, 16, 362–375. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2020 Update: A Report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef]
- Chrisinger, B.W.; Kallan, M.J.; Whiteman, E.D.; Hillier, A. Where do U.S. households purchase healthy foods? An analysis of food-at-home purchases across different types of retailers in a nationally representative dataset. Prev. Med. 2018, 112, 15–22. [Google Scholar] [CrossRef]
- Chavez, J.R.; Bruening, M.; Ohri-Vachaspati, P.; Lee, R.; Jehn, M. Street Food Stand Availability, Density, and Distribution Across Income Levels in Mexico City. Int. J. Environ. Res. Public Health 2021, 18, 3953. [Google Scholar] [CrossRef]
- Bridle-Fitzpatrick, S. Food deserts or food swamps? A mixed-methods study of local food environments in a Mexican city. Soc. Sci. Med. 2015, 142, 202–213. [Google Scholar] [CrossRef] [PubMed]
- Bilal, U.; Auchincloss, A.H.; Diez-Roux, A.V. Neighborhood Environments and Diabetes Risk and Control. Curr. Diabetes Rep. 2018, 18, 62. [Google Scholar] [CrossRef] [PubMed]
- Lanas, F.; Avezum, A.; Bautista, L.E.; Diaz, R.; Luna, M.; Islam, S.; Yusuf, S. Risk Factors for Acute Myocardial Infarction in Latin America: The INTERHEART Latin American study. Circulation 2007, 115, 1067–1074. [Google Scholar] [CrossRef] [PubMed]
| Hypertension Status | ||||
|---|---|---|---|---|
| Total Sample | Non- Hypertensive | Undiagnosed Hypertensive | Diagnosed Hypertensive | |
| N = 2798 | (1959) | (297) | (542) | |
| Person level | Mean (SE) or % (SE) | |||
| Blood Pressure | ||||
| SBP | 120.8 (0.7) | 113.5 (0.5) | 146.7 (1.4) | 137.4 (2.4) |
| DBP | 73.8 (0.4) | 70.5 (0.4) | 87.9 (0.9) | 80.1 (0.9) |
| Age | 42.1 (0.6) | 38.0 (0.5) | 51.8 (1.3) | 54.0 (1.5) |
| Female, % | 50.7 (1.6) | 49.7 (1.6) | 39.5 (3.4) | 61.9 (5.5) |
| Education, % | ||||
| Incomplete H.S. or less | 66.1 (1.9) | 61.8 (2.2) | 77.9 (3.0) | 78.0 (5.6) |
| Wealth Index, % | ||||
| Poorest (Tertile) | 13.2 (1.3) | 13.2 (1.4) | 18.4 (4.1) | 10.4 (2.2) |
| Middle (Tertile) | 27.2 (2.2) | 25.8 (2.3) | 33.3 (5.7) | 30.0 (4.8) |
| Richest (Tertile) | 59.6 (2.4) | 61.1 (2.7) | 48.3 (5.1) | 59.5 (5.2) |
| AGEB | Blood Pressure Outcomes | ||||
|---|---|---|---|---|---|
| SBP | DBP | ||||
| Density Changes | N | % Change | N ♦ | Mean (SE) | |
| Fruit/vegetable | |||||
| Decrease | 37 | 25.2 | 651 | 122.5 (1.5) | 74.8 (0.9) |
| No increase | 52 | 35.4 | 1030 | 119.5 (1.3) | 72.8 (0.7) |
| Increase | 58 | 39.5 | 1117 | 120.9 (1.0) | 74.3 (0.4) |
| Convenience stores | |||||
| No increase | 119 | 80.9 | 2251 | 120.3 (0.8) | 73.5 (0.4) |
| Increase | 28 | 19.1 | 547 | 122.7 (1.5) | 75.2 (0.9) |
| Supermarkets | |||||
| No increase | 141 | 95.9 | 2680 | 121.0 (0.7) | 74.0 (0.4) |
| Increase | 6 | 4.1 | 118 | 117.3 (4.9) | 71.0 (2.2) |
| Density Change | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Fruit and vegetable shops | |||
| (1) Decrease | 2.67 (0.14, 5.19) | 1.92 (0.06, 3.78) | 1.76 (−0.15, 3.67) |
| (2) No increase (ref.) | |||
| (3) Increase | 0.77 (−1.43, 2.98) | 0.75 (−0.87, 2.52) | 0.64 (−0.98, 2.61) |
| Convenience stores | |||
| (1) No increase | |||
| (2) Increase | 0.71 (−1.72, 3.14) | 0.72 (−1.06, 2.51) | 0.82 (−0.94, 2.60) |
| Supermarkets (large) | |||
| (1) No increase | |||
| (2) Increase | 0.77 (−4.06, 3.14) | 0.99 (−3.08, 5.06) | 0.53 (−3.03, 4.10) |
| Density Change | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Fruit and vegetable shops | |||
| (1) Decline | 1.19 (−0.01, 2.38) | 0.93 (−0.08, 1.94) | 0.82 (−0.24, 1.88) |
| (2) No increase (ref.) | |||
| (3) Increase | 0.64 (−0.39, 1.69) | 0.52 (−0.35, 1.41) | 0.48 (−0.42, 1.37) |
| Convenience stores | |||
| (1) No increase | |||
| (2) Increase | 0.45 (−0.70, 1.59) | 0.31 (−0.64, 1.28) | 0.37 (−0.60, 1.35) |
| Supermarkets (large) | |||
| (1) No increase | |||
| (2) Increase | −0.93 (−3.21, 1.35) | −1.70 (−3.63, 0.23) | −1.46 (−3.42, 0.51) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Armendariz, M.; Pérez-Ferrer, C.; Basto-Abreu, A.; Lovasi, G.S.; Bilal, U.; Barrientos-Gutiérrez, T. Changes in the Retail Food Environment in Mexican Cities and Their Association with Blood Pressure Outcomes. Int. J. Environ. Res. Public Health 2022, 19, 1353. https://doi.org/10.3390/ijerph19031353
Armendariz M, Pérez-Ferrer C, Basto-Abreu A, Lovasi GS, Bilal U, Barrientos-Gutiérrez T. Changes in the Retail Food Environment in Mexican Cities and Their Association with Blood Pressure Outcomes. International Journal of Environmental Research and Public Health. 2022; 19(3):1353. https://doi.org/10.3390/ijerph19031353
Chicago/Turabian StyleArmendariz, Marina, Carolina Pérez-Ferrer, Ana Basto-Abreu, Gina S. Lovasi, Usama Bilal, and Tonatiuh Barrientos-Gutiérrez. 2022. "Changes in the Retail Food Environment in Mexican Cities and Their Association with Blood Pressure Outcomes" International Journal of Environmental Research and Public Health 19, no. 3: 1353. https://doi.org/10.3390/ijerph19031353
APA StyleArmendariz, M., Pérez-Ferrer, C., Basto-Abreu, A., Lovasi, G. S., Bilal, U., & Barrientos-Gutiérrez, T. (2022). Changes in the Retail Food Environment in Mexican Cities and Their Association with Blood Pressure Outcomes. International Journal of Environmental Research and Public Health, 19(3), 1353. https://doi.org/10.3390/ijerph19031353






