How Many Hours of Device Wear Time Are Required to Accurately Measure Physical Activity Post Stroke?
Abstract
1. Introduction
- (a)
- measures of daytime physical activity, specifically sedentary awake time, light and moderate to vigorous physical activity
- (b)
- the attainment of guideline-recommended physical activity levels in stroke survivors
2. Materials and Methods
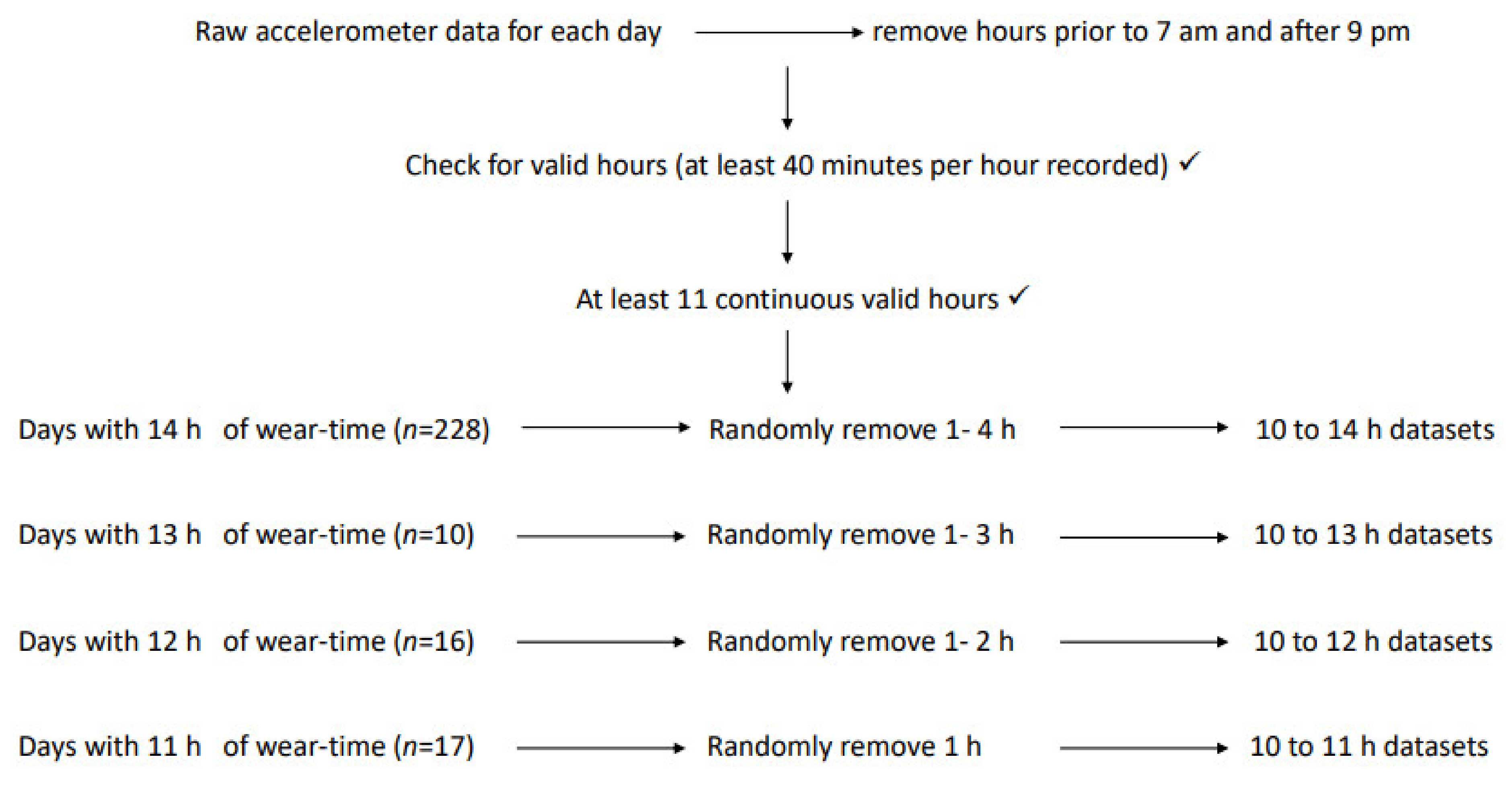
Data Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Warburton, D.E.R.; Bredin, S.S.D. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opionion Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef] [PubMed]
- Dhamoon, M.S.; Sciacca, R.R.; Rundek, T.; Sacco, R.L.; Elkind, M.S.V. Recurrent stroke and cardiac risks after first ischemic stroke: The Northern Manhattan Study. Neurology 2006, 66, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Fini, N.A.; Holland, A.E.; Keating, J.; Simek, J.; Bernhardt, J. How Physically Active Are People Following Stroke? Systematic Review and Quantitative Synthesis. Phys. Ther. 2017, 97, 707–717. [Google Scholar] [CrossRef]
- Morris, J.H.; Oliver, T.; Kroll, T.; Joice, S.; Williams, B. Physical activity participation in community dwelling stroke survivors: Synergy and dissonance between motivation and capability. A qualitative study. Physiotherapy 2017, 103, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Committee PAGA. 2018 Physical Activity Guidelines Advisory Commitee Scientfic Report; US Department of Health and Human Services: Washington, DC, USA, 2018. [Google Scholar]
- Department of Health and Social Care UK. UK Chief Medical Officers’ Physical Activity Guidelines; Department of Health and Social Care UK: London, UK, 2019. [Google Scholar]
- Australia’s Physical Activity and Sedentary Behaviour Guidelines; Australian Government: Canberra, Australia, 2014.
- WHO. ACTIVE: A Technical Package for Increasing Physical Activity; World Health Organisation: Geneva, Switzerland, 2018. [Google Scholar]
- Teasell, R.; Salbach, N.M.; Foley, N.; Mountain, A.; Cameron, J.I.; de Jong, A.; Acerra, N.E.; Bastasi, D.; Carter, S.L.; Fung, J.; et al. Canadian Stroke Best Practice Recommendations: Rehabilitation, Recovery, and Community Participation following Stroke. Part One: Rehabilitation and Recovery Following Stroke; 6th Edition Update 2019. Int. J. Stroke 2020, 15, 763–788. [Google Scholar] [CrossRef] [PubMed]
- Maranesi, E.; Riccardi, G.R.; Di Donna, V.; Di Rosa, M.; Fabbietti, P.; Luzi, R.; Pranno, L.; Lattanzio, F.; Bevilacqua, R. Effectiveness of Intervention Based on End-effector Gait Trainer in Older Patients with Stroke: A Systematic Review. J. Am. Med Dir. Assoc. 2019, 21, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Lynch, E.A.; Jones, T.M.; Simpson, D.B.; Fini, N.A.; Kuys, S.; Borschmann, K.; Kramer, S.; Johnson, L.; Callisaya, M.L.; Mahendran, N.; et al. Activity monitors for increasing physical activity in adult stroke survivors. Cochrane Database Syst. Rev. 2018, 7, CD012543. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Li, D.; Liu, Y.; Wang, J.; Xiao, Q. Virtual reality for limb motor function, balance, gait, cognition and daily function of stroke patients: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 77, 3255–3273. [Google Scholar] [CrossRef]
- Scott, A.L.; Hu, W.; Rangarajan, S.; Gasevic, D.; Leong, D.; Iqbal, R.; Casanova, A.; Swaminathan, S.; Anjana, R.M.; Kumar, R.; et al. The effect of physical activity on mortality and cardiovascular disease in 130,000 people from 17 high-income, middle-income, and low-income countries: The PURE study. Lancet 2017, 390, 2643–2654. [Google Scholar] [CrossRef]
- Resnick, B.; Michael, K.; Shaughnessy, M.; Nahm, E.S.; Kopunek, S.; Sorkin, J.; Orwig, D.; Goldberg, A.; Macko, R.F. Inflated Perceptions of Physical Activity After Stroke: Pairing Self-Report With Physiologic Measures. J. Phys. Act. Health 2008, 5, 308–318. [Google Scholar] [CrossRef]
- Kunkel, D.; Fitton, C.; Burnett, M.; Ashburn, A. Physical inactivity post-stroke: A 3-year longitudinal study. Disabil. Rehab. 2015, 37, 304–310. [Google Scholar] [CrossRef]
- Fini, N.A.; Bernhardt, J.; Churilov, L.; Clark, R.; Holland, A.E. Adherence to physical activity and cardiovascular recommendations during the 2 years after stroke rehabilitation discharge. Ann. Phys. Rehab. Med. 2021, 64, 101455. [Google Scholar] [CrossRef]
- Tinlin, L.; Fini, N.; Bernhardt, J.; Lewis, L.K.; Olds, T.; English, C. Best practice guidelines for the measurement of physical activity levels in stroke survivors: A secondary analysis of an observational study. Int. J. Rehab. Res. 2018, 41, 14–19. [Google Scholar] [CrossRef]
- Fini, N.A.; Burge, A.T.; Bernhardt, J.; Holland, A.E. Two Days of Measurement Provides Reliable Estimates of Physical Activity Poststroke: An Observational Study. Arch. Phys. Med. Rehab. 2019, 100, 883–890. [Google Scholar] [CrossRef]
- Herrmann, S.D.; Barreira, T.; Kang, M.; Ainsworth, B.E. How Many Hours Are Enough? Accelerometer Wear Time May Provide Bias in Daily Activity Estimates. J. Phys. Act. Health 2013, 10, 742–749. [Google Scholar] [CrossRef]
- McGrath, R.; Vella, C.A.; Scruggs, P.W.; Peterson, M.; Williams, C.; Paul, D.R. The Impact of Low Accelerometer Wear Time on the Estimates and Application of Sedentary Behavior and Physical Activity Data in Adults. J. Phys. Act. Health 2017, 14, 919–924. [Google Scholar] [CrossRef]
- Miller, G.D.; Jakicic, J.M.; Wejeski, W.J.; Whit-Glover, M.C.; Lang, W.; Walkup, M.P.; Hodges, M.L. Effect of Varying Accelerometry Criteria on Physical Activity: The Look AHEAD Study. Obesity 2013, 21, 32–44. [Google Scholar] [CrossRef]
- Fini, A.N.; Bernhardt, J.; Holland, A.E. What is the relationship between physical activity and cardiovascular risk factors in stroke survivors post completion of rehabilitation? Protocol for a longitudinal study. BMJ Open 2017, 7, e019193. [Google Scholar] [CrossRef]
- Moore, S.A.; Hallsworth, K.; Bluck, L.J.; Ford, G.A.; Rochester, L.; Trenell, M.I. Measuring energy expenditure after stroke: Validation of a portable device. Stroke J. Cereb. Circ. 2012, 43, 1660–1662. [Google Scholar] [CrossRef]
- Manns, P.J.; Haennel, R.G. SenseWear Armband and Stroke: Validity of Energy Expenditure and Step Count Measurement during Walking. Stroke Res. Treat. 2012, 2012, 247165. [Google Scholar] [CrossRef]
- Vanroy, C.; Vissers, D.; Cras, P.; Beyne, S.; Feys, H.; Vanlandewijck, Y.; Truijen, S. Physical activity monitoring in stroke: SenseWear Pro2 Activity accelerometer versus Yamax Digi-Walker SW-200 Pedometer. Disabil. Rehab. 2014, 36, 1695–1703. [Google Scholar] [CrossRef] [PubMed]
- Thilarajah, S.; Mentiplay, B.F.; Bower, K.J.; Tan, D.; Pua, Y.H.; Williams, G.; Koh, G.; Clark, R.A. Factors Associated With Post-Stroke Physical Activity: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 1876–1889. [Google Scholar] [CrossRef] [PubMed]
- Fini, N.A.; Bernhardt, J.; Churilov, L.; Clark, R.; Holland, A.E. A 2-Year Longitudinal Study of Physical Activity and Cardiovascular Risk in Survivors of Stroke. Phys. Ther. Rehab. J. 2020, 101, pzaa205. [Google Scholar] [CrossRef] [PubMed]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics, 6th ed.; Pearson: Boston, MA, USA, 2014. [Google Scholar]
- Magezi, D.A. Linear mixed-effects models for within-participant psychology experiments: An introductory tutorial and free, graphical user interface (LMMgui). Front. Psychol. 2015, 6, 2. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. The use of transformation when comparing two means. BMJ 1996, 312, 1153. [Google Scholar] [CrossRef]
- Schielzeth, H.; Dingemanse, N.J.; Nakagawa, S.; Westneat, D.F.; Allegue, H.; Teplitsky, C.; Réale, D.; Dochtermann, N.A.; Garamszegi, L.Z.; Araya-Ajoy, Y.G. Robustness of linear mixed-effects models to violations of distributional assumptions. Methods Ecol. Evol. 2020, 11, 1141–1152. [Google Scholar] [CrossRef]
- Alzahrani, M.A.; Ada, L.; Dean, C.M. Duration of physical activity is normal but frequency is reduced after stroke: An observational study. J. Physiother. 2011, 57, 47–51. [Google Scholar] [CrossRef][Green Version]
- Vanroy, C.; Vissers, D.; Vanlandewijck, Y.; Feys, H.; Truijen, S.; Michielsen, M.; Cras, P. Physical activity in chronic home-living and sub-acute hospitalized stroke patients using objective and self-reported measures. Top. Stroke Rehab. 2016, 23, 98–105. [Google Scholar] [CrossRef]
- Shimizu, N.; Hashidate, H.; Ota, T.; Saito, A. Reliability of intensity-based physical activity measurement using an activity monitor in people with subacute stroke in the hospital setting: A cross-sectional study. Top. Stroke Rehab. 2018, 25, 288–294. [Google Scholar] [CrossRef]
- Luker, J.; Lynch, E.; Bernhardsson, S.; Bennett, L.; Bernhardt, J. Stroke Survivors’ Experiences of Physical Rehabilitation: A Systematic Review of Qualitative Studies. Arch. Phys. Med. Rehab. 2015, 96, 1698–1708. [Google Scholar] [CrossRef]
- Ramage, E.R.; Fini, N.A.; Lynch, E.; Marsden, D.L.; Patterson, A.J.; Said, C.M.; English, C. Look Before You Leap: Interventions Supervised via Telehealth Involving Activities in Weight-Bearing or Standing Positions for People After Stroke—A Scoping Review. Phys. Ther. 2021, 101, pzab073. [Google Scholar] [CrossRef]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Informatics Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef]
- Kramer, S.F.; Johnson, L.; Bernhardt, J.; Cumming, T. Validity of Multisensor Array for Measuring Energy Expenditure of an Activity Bout in Early Stroke Survivors. Stroke Res. Treat. 2018, 2018, 9134547. [Google Scholar] [CrossRef]
- Compagnat, M.; Daviet, J.C.; Batcho, C.S.; David, R.; Salle, J.Y.; Mandigout, S. Quantification of energy expenditure during daily living activities after stroke by multi-sensor. Brain Inj. 2019, 33, 1341–1346. [Google Scholar] [CrossRef]
| Characteristics | n = 69 |
|---|---|
| Gender, n male (%) | 46 (67) |
| Age (years), mean (SD) | 65 (15) |
| Type of stroke (infarct/haemorrhage), n infarct (%) | 48 (70) |
| NIHSS, mean (IQR) | 9 (4, 12) |
| Time post-stroke (days), median (IQR) | 151 (99, 225) |
| Body mass index (kg/m2), mean (SD) | 27.0 (5.2) |
| Gait speed (m/s), median (IQR) | 1.2 (0.9, 1.4) |
| 6-min walk test (m), mean (SD) | 389 (181) |
| Original Data | Sedentary Awake Time | Time in LIPA | Time in MVPA | |||
|---|---|---|---|---|---|---|
| 14-h Reference Set | 519 (497 to 542) | 154 (138 to 170) | 75 (61 to 89) | |||
| MD (95% CI) | APE | MD (95% CI) | APE | MD (95% CI) | APE | |
| Δ 13 | −35 (−45 to −25) | 7% | −12 (−19 to −5) | 8% | −5 (−1 to −10) | 7% |
| Δ 12 | −69 (−80 to −59) | 13% | −23 (−30 to −17) | 15% | −11 (−17 to −4) | 14% |
| Δ 11 | −108 (−118 to −98) | 21% | −34 (−41 to −28) | 22% | −15 (−22 to −9) | 20% |
| Δ 10 | −145 (−155 to −135) | 28% | −45 (−52 to −38) | 29% | −20 (−27 to −14) | 27% |
| Did Not Record 30 min MVPA | Did Record 30 min MVPA | ||
|---|---|---|---|
| 14 h | 82 | 147 | Cochran’s Q |
| 13 h | 90 | 139 | p = 0.011 |
| 12 h | 99 | 130 | |
| 11 h | 107 | 122 | |
| 10 h | 112 | 117 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fini, N.A.; Holland, A.E.; Bernhardt, J.; Burge, A.T. How Many Hours of Device Wear Time Are Required to Accurately Measure Physical Activity Post Stroke? Int. J. Environ. Res. Public Health 2022, 19, 1191. https://doi.org/10.3390/ijerph19031191
Fini NA, Holland AE, Bernhardt J, Burge AT. How Many Hours of Device Wear Time Are Required to Accurately Measure Physical Activity Post Stroke? International Journal of Environmental Research and Public Health. 2022; 19(3):1191. https://doi.org/10.3390/ijerph19031191
Chicago/Turabian StyleFini, Natalie A., Anne E. Holland, Julie Bernhardt, and Angela T. Burge. 2022. "How Many Hours of Device Wear Time Are Required to Accurately Measure Physical Activity Post Stroke?" International Journal of Environmental Research and Public Health 19, no. 3: 1191. https://doi.org/10.3390/ijerph19031191
APA StyleFini, N. A., Holland, A. E., Bernhardt, J., & Burge, A. T. (2022). How Many Hours of Device Wear Time Are Required to Accurately Measure Physical Activity Post Stroke? International Journal of Environmental Research and Public Health, 19(3), 1191. https://doi.org/10.3390/ijerph19031191







