Game of Mirrors: Health Profiles in Patient and Physician Perceptions
Abstract
1. Introduction
2. Materials and Methods
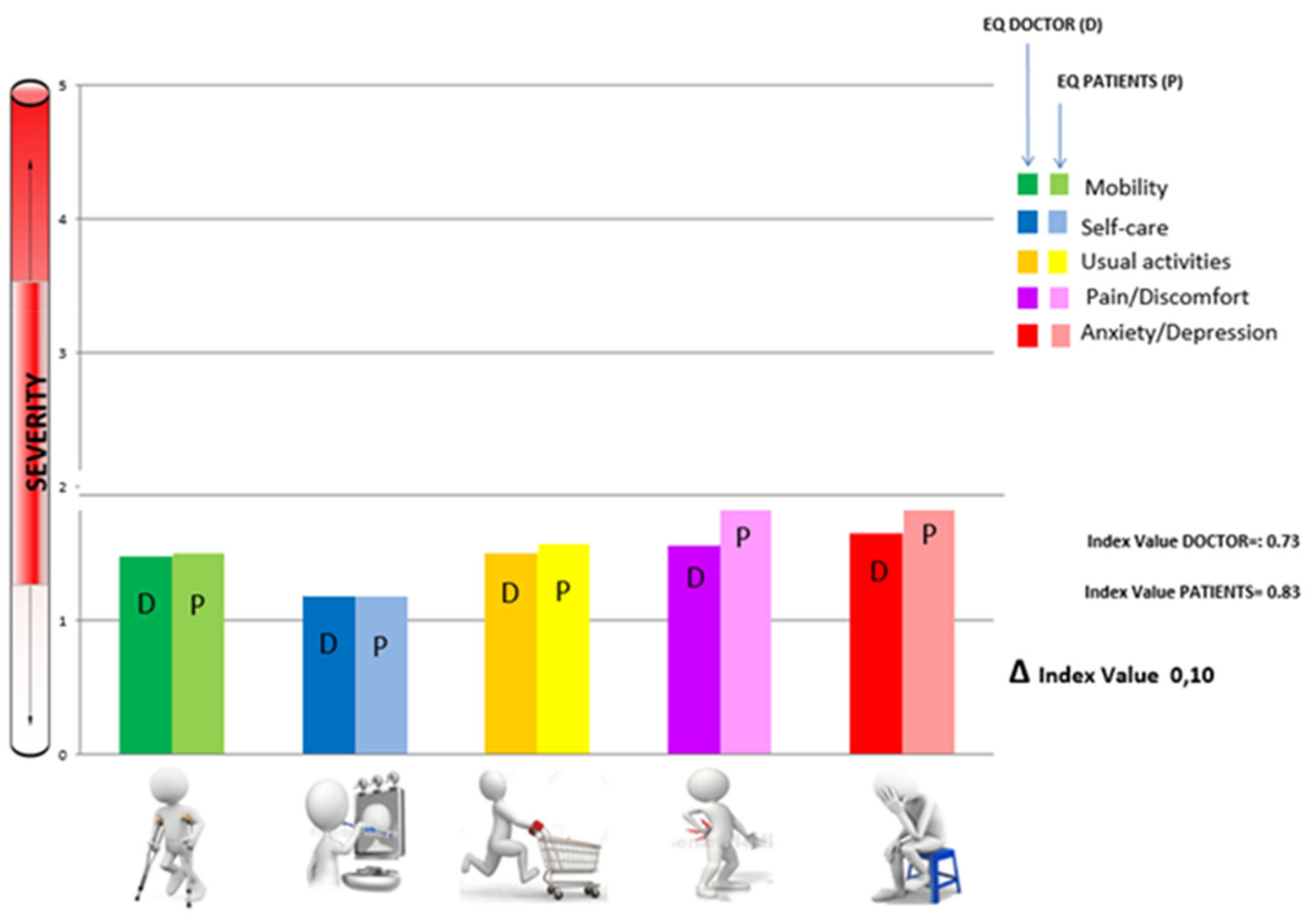
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mulhern, B.; Norman, R.; De Abreu Lourenco, R.; Malley, J.; Street, D.; Viney, R. Investigating the relative value of health and social care related quality of life using a discrete choice experiment. Soc. Sci. Med. 2019, 233, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Moons, P. Why Call it Health-Related Quality of Life When You Mean Perceived Health Status? Eur. J. Cardiovasc. Nurs. 2004, 3, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Stolk, E.A.; Oppe, M.; Scalone, L.; Krabbe, P.F.M. Discrete Choice Modeling for the Quantification of Health States: The Case of the EQ-5D. Value Health 2010, 13, 1005–1013. [Google Scholar] [CrossRef] [PubMed]
- Quercioli, C.; Messina, G.; Barbini, E.; Carriero, G.; Fanì, M.; Nante, N. Importance of sociodemographic and morbidity aspects in measuring health-related quality of life: Performances of three tools: Comparison of three questionnaire scores. Eur. J. Health Econ. 2009, 10, 389–397. [Google Scholar] [CrossRef]
- Nante, N.; Gialluca, L.; De Corso, M.; Troiano, G.; Verzuri, A.; Messina, G. Quality of life in refugees and asylum seekers in Italy: A pilot study. Ann. Dell Istituto Super. Di Sanita 2016, 52, 424–427. [Google Scholar] [CrossRef]
- Kozloff, N.; Pinto, A.D.; Stergiopoulos, V.; Hwang, S.W.; O’Campo, P.; Bayoumi, A.M. Convergent validity of the EQ-5D-3L in a randomized-controlled trial of the Housing First model. BMC Health Serv. Res. 2019, 19, 482. [Google Scholar] [CrossRef]
- Longworth, L.; Rowen, D. Mapping to Obtain EQ-5D Utility Values for Use in NICE Health Technology Assessments. Value Health 2013, 16, 202–210. [Google Scholar] [CrossRef]
- Strada, L.; Vanderplasschen, W.; Buchholz, A.; Schulte, B.; Muller, A.E.; Verthein, U.; Reimer, J. Measuring quality of life in opioid-dependent people: A systematic review of assessment instruments. Qual. Life Res. 2017, 26, 3187–3200. [Google Scholar] [CrossRef]
- Scoggins, J.F.; Patrick, D.L. The use of patient-reported outcomes instruments in registered clinical trials: Evidence from ClinicalTrials.gov. Contemp. Clin. Trials 2009, 30, 289–292. [Google Scholar] [CrossRef]
- Moons, P.; Budts, W.; De Geest, S. Critique on the conceptualisation of quality of life: A review and evaluation of different conceptual approaches. Int. J. Nurs. Stud. 2006, 43, 891–901. [Google Scholar] [CrossRef]
- Messina, G.; Quercioli, C.; Troiano, G. Italian medical students quality of life: Years 2005–2015. Ann. Hyg. Prev. Community Med. 2016, 28, 245–251. [Google Scholar]
- Dakin, H.; Abel, L.; Burns, R.; Yang, Y. Review and critical appraisal of studies mapping from quality of life or clinical measures to EQ-5D: An online database and application of the MAPS statement. Health Qual. Life Outcomes 2018, 16, 31. [Google Scholar] [CrossRef]
- Buchholz, I.; Janssen, M.F.; Kohlmann, T.; Feng, Y.-S. A Systematic Review of Studies Comparing the Measurement Properties of the Three-Level and Five-Level Versions of the EQ-5D. PharmacoEconomics 2018, 36, 645–661. [Google Scholar] [CrossRef]
- Devlin, N.J.; Brooks, R. EQ-5D and the EuroQol Group: Past, Present and Future. Appl. Health Econ. Health Policy 2017, 15, 127–137. [Google Scholar] [CrossRef]
- Luo, N.; Liu, G.; Li, M.; Guan, H.; Jin, X.; Rand, K. Estimating an EQ-5D-5L Value Set for China. Value Health 2017, 20, 662–669. [Google Scholar] [CrossRef]
- Silva, A.; Cancela, J.; Mollinedo, I.; Camões, M.; Bezerra, P. The Relationship between Health Perception and Health Predictors among the Elderly across European Countries. Int. J. Environ. Res. Public Health 2021, 18, 4053. [Google Scholar] [CrossRef]
- Dwamena, F.; Holmes-Rovner, M.; Gaulden, C.M.; Jorgenson, S.; Sadigh, G.; Sikorskii, A.; Lewin, S.; Smith, R.C.; Coffey, J.; Olomu, A.; et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst. Rev. 2012, 12, CD003267. [Google Scholar] [CrossRef]
- Purkaple, B.A.; Mold, J.W.; Chen, S. Encouraging Patient-Centered Care by Including Quality-of-Life Questions on Pre-Encounter Forms. Ann. Fam. Med. 2016, 14, 221–226. [Google Scholar] [CrossRef]
- Bernardo, M.O.; Cecilio-Fernandes, D.; de Abreu Lima, A.R.; Silva, J.F.; Ceccato, H.D.; Costa, M.J.; de Carvalho-Filho, M.A. Investigating the relation between self-assessment and patients’ assessments of physicians-in-training empathy: A multicentric, observational, cross-sectional study in three teaching hospitals in Brazil. BMJ Open 2019, 9, e029356. [Google Scholar] [CrossRef]
- Couture, É.M.; Chouinard, M.-C.; Fortin, M.; Hudon, C. The relationship between health literacy and quality of life among frequent users of health care services: A cross-sectional study. Health Qual. Life Outcomes 2017, 15, 137. [Google Scholar] [CrossRef]
- Di Lillo, M.; Cicchetti, A.; Scalzo, A.L.; Taroni, F.; Hojat, M. The Jefferson Scale of Physician Empathy: Preliminary Psychometrics and Group Comparisons in Italian Physician. Acad. Med. 2009, 84, 1198–1202. [Google Scholar] [CrossRef]
- Hojat, M.; Gonnella, J.S. What Matters More About the Interpersonal Reactivity Index and the Jefferson Scale of Empathy? Their Underlying Constructs or Their Relationships with Pertinent Measures of Clinical Competence and Patient Outcomes? Acad. Med. 2017, 92, 743–745. [Google Scholar] [CrossRef]
- Mercer, S.W.; Reynolds, W.J. Empathy and quality of care. Br. J. Gen. Pract. 2002, 52, S9–S12. [Google Scholar]
- Lee, M.; Noh, Y.; Youm, C.; Kim, S.; Park, H.; Noh, B.; Kim, B.; Choi, H.; Yoon, H. Estimating Health-Related Quality of Life Based on Demographic Characteristics, Questionnaires, Gait Ability, and Physical Fitness in Korean Elderly Adults. Int. J. Environ. Res. Public Health 2021, 18, 11816. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Neumann, M.; Wirtz, M.A.; Bollschweiler, E.; Mercer, S.; Warm, M.; Wolf, J.; Pfaff, H. Determinants and patient-reported long-term outcomes of physician empathy in oncology: A structural equation modelling approach. Patient Educ. Couns. 2007, 69, 63–75. [Google Scholar] [CrossRef]
- Bernardo, M.O.; Cecílio-Fernandes, D.; Costa, P.; Quince, T.A.; Costa, M.J.; Carvalho-Filho, M.A. Physicians’ self-assessed empathy levels do not correlate with patients’ assessments. PLoS ONE 2018, 13, e0198488. [Google Scholar] [CrossRef]
- Cánovas, L.; Carrascosa, A.-J.; García, M.; Fernández, M.; Calvo, A.; Monsalve, V.; Soriano, J.-F.; Empathy Study Group. Impact of Empathy in the Patient-Doctor Relationship on Chronic Pain Relief and Quality of Life: A Prospective Study in Spanish Pain Clinics. Pain Med. 2018, 19, 1304–1314. [Google Scholar] [CrossRef]
- Lucas-Molina, B.; Pérez-Albéniz, A.; Ortuño-Sierra, J. Dimensional structure and measurement invariance of the Interpersonal Reactivity Index (IRI) across gender. Psicothema 2017, 29, 590–595. [Google Scholar]
- Silva, R.G.; Figueiredo-Braga, M. The roles of empathy, attachment style, and burnout in pharmacy students’ academic satisfaction. Am. J. Pharm. Educ. 2018, 83, ajpe6706. [Google Scholar] [CrossRef]
- Kim, K. To Feel or Not to Feel: Empathy and Physician Burnout. Acad. Psychiatry 2018, 42, 157–158. [Google Scholar] [CrossRef] [PubMed]
| Mobility | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| None | Slight | Moderate | Severe | Extreme | ||||||
| N° | % | N° | % | N° | % | N° | % | N° | % | |
| FEMALES | 164 | 70.1 | 42 | 17.9 | 14 | 6 | 10 | 4.3 | 4 | 1.7 |
| MALES | 139 | 73.5 | 31 | 16.5 | 14 | 7.4 | 5 | 2.6 | 0 | 0 |
| Fisher’s exact = 0.4 | ||||||||||
| Self-Care | ||||||||||
| None | Slight | Moderate | Severe | Extreme | ||||||
| N° | % | N° | % | N° | % | N° | % | N° | % | |
| FEMALES | 188 | 80.4 | 23 | 9.8 | 13 | 5.6 | 5 | 2.1 | 5 | 2.1 |
| MALES | 162 | 85.7 | 19 | 10.1 | 7 | 3.7 | 1 | 0.5 | 0 | 0 |
| Fisher’s exact = 0.1 | ||||||||||
| Usual Activities | ||||||||||
| None | Slight | Moderate | Severe | Extreme | ||||||
| N° | % | N° | % | N° | % | N° | % | N° | % | |
| FEMALES | 151 | 64.5 | 44 | 18.8 | 22 | 9.4 | 10 | 4.3 | 7 | 3 |
| MALES | 141 | 74.6 | 34 | 18 | 13 | 6.9 | 0 | 0 | 1 | 0.5 |
| Fisher’s exact < 0.01 | ||||||||||
| Pain/Discomfort | ||||||||||
| None | Slight | Moderate | Severe | Extreme | ||||||
| N° | % | N° | % | N° | % | N° | % | N° | % | |
| FEMALES | 89 | 38 | 73 | 31.3 | 56 | 23.9 | 11 | 4.7 | 5 | 2.1 |
| MALES | 102 | 53.9 | 55 | 29.1 | 30 | 15.9 | 2 | 1.1 | 0 | 0 |
| Fisher’s exact < 0.01 | ||||||||||
| Anxiety/Depression | ||||||||||
| None | Slight | Moderate | Severe | Extreme | ||||||
| N° | % | N° | % | N° | % | N° | % | N° | % | |
| FEMALES | 90 | 38.5 | 83 | 35.5 | 48 | 20.5 | 9 | 3.8 | 4 | 1.7 |
| MALES | 114 | 60.3 | 54 | 28.6 | 19 | 10.1 | 0 | 0 | 2 | 1 |
| Fisher’s exact < 0.01 | ||||||||||
| P-Pain/Discomfort | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| None | Slight | Moderate | Severe | Extreme | ||||||
| N° | % | N° | % | N° | % | N° | % | N° | % | |
| FEMALES | 133 | 56.8 | 56 | 23.9 | 39 | 16.8 | 5 | 2.1 | 1 | 0.4 |
| MALES | 123 | 65.1 | 45 | 23.8 | 18 | 9.5 | 3 | 1.6 | 0 | 0 |
| Fisher’s exact = 0.16 | ||||||||||
| P-Anxiety/Depression | ||||||||||
| None | Slight | Moderate | Severe | Extreme | ||||||
| N° | % | N° | % | N° | % | N° | % | N° | % | |
| FEMALES | 116 | 49.6 | 61 | 26 | 37 | 15.8 | 17 | 7.3 | 3 | 1.3 |
| MALES | 120 | 63.5 | 39 | 20.6 | 18 | 9.5 | 10 | 5.3 | 2 | 1.1 |
| Fisher’s exact = 0.06 | ||||||||||
| Agreement | Expected Agreement | Kappa | Standard Error | Z | Prob > Z | |
|---|---|---|---|---|---|---|
| Mobility | 83.7% | 56.7% | 0.62 | 0.03 | 18.19 | <0.01 |
| Self-Care | 83.7% | 68.9% | 0.48 | 0.04 | 13.38 | <0.01 |
| Usual activities | 76.6% | 53.5% | 0.50 | 0.03 | 14.73 | <0.01 |
| Pain/discomfort | 57.2% | 37.4% | 0.32 | 0.03 | 9.74 | <0.01 |
| Anxiety/depression | 60.52% | 36.8% | 0.38 | 0.03 | 11.70 | <0.01 |
| EQ INDEX | 30.73% | 12.6% | 0.21 | 0.01 | 14.61 | <0.01 |
| MALES | FEMALES | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Agreement | Expected Agreement | Kappa | Standard Error | Z | Prob > Z | Agreement | Expected Agreement | Kappa | Standard Error | Prob > Z | |
| Mobility | 82.5% | 58.6% | 0.58 | 0.05 | 11.0 | <0.01 | 84.6% | 55.3% | 0.66 | 14.5 | <0.01 |
| Self-Care | 83.1% | 72.5% | 0.38 | 0.06 | 6.8 | <0.01 | 84.2% | 66.1% | 0.53 | 11.7 | <0.01 |
| Usual activities | 76.7% | 59.1% | 0.43 | 0.05 | 8.0 | <0.01 | 76.5% | 49.2% | 0.54 | 12.4 | <0.01 |
| Pain/discomfort | 64.6% | 43.6% | 0.37 | 0.05 | 7.1 | <0.01 | 51.3% | 33.2% | 0.27 | 6.5 | <0.01 |
| Anxiety/depression | 65.6% | 45.2% | 0.37 | 0.05 | 7.3 | <0.01 | 56.4% | 31.9% | 0.36 | 8.8 | <0.01 |
| EQ INDEX | 36.5% | 16.7% | 0.24 | 0.02 | 10.1 | <0.01 | 26.1% | 9.7% | 0.18 | 10.5 | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fineschi, D.; Acciai, S.; Napolitani, M.; Scarafuggi, G.; Messina, G.; Guarducci, G.; Nante, N. Game of Mirrors: Health Profiles in Patient and Physician Perceptions. Int. J. Environ. Res. Public Health 2022, 19, 1201. https://doi.org/10.3390/ijerph19031201
Fineschi D, Acciai S, Napolitani M, Scarafuggi G, Messina G, Guarducci G, Nante N. Game of Mirrors: Health Profiles in Patient and Physician Perceptions. International Journal of Environmental Research and Public Health. 2022; 19(3):1201. https://doi.org/10.3390/ijerph19031201
Chicago/Turabian StyleFineschi, Daniele, Sofia Acciai, Margherita Napolitani, Giovanni Scarafuggi, Gabriele Messina, Giovanni Guarducci, and Nicola Nante. 2022. "Game of Mirrors: Health Profiles in Patient and Physician Perceptions" International Journal of Environmental Research and Public Health 19, no. 3: 1201. https://doi.org/10.3390/ijerph19031201
APA StyleFineschi, D., Acciai, S., Napolitani, M., Scarafuggi, G., Messina, G., Guarducci, G., & Nante, N. (2022). Game of Mirrors: Health Profiles in Patient and Physician Perceptions. International Journal of Environmental Research and Public Health, 19(3), 1201. https://doi.org/10.3390/ijerph19031201







