Exploring an Applied Ecological Model of the Effects of Household, School, and Community Environments on Adolescent Mental Health in Japan
Abstract
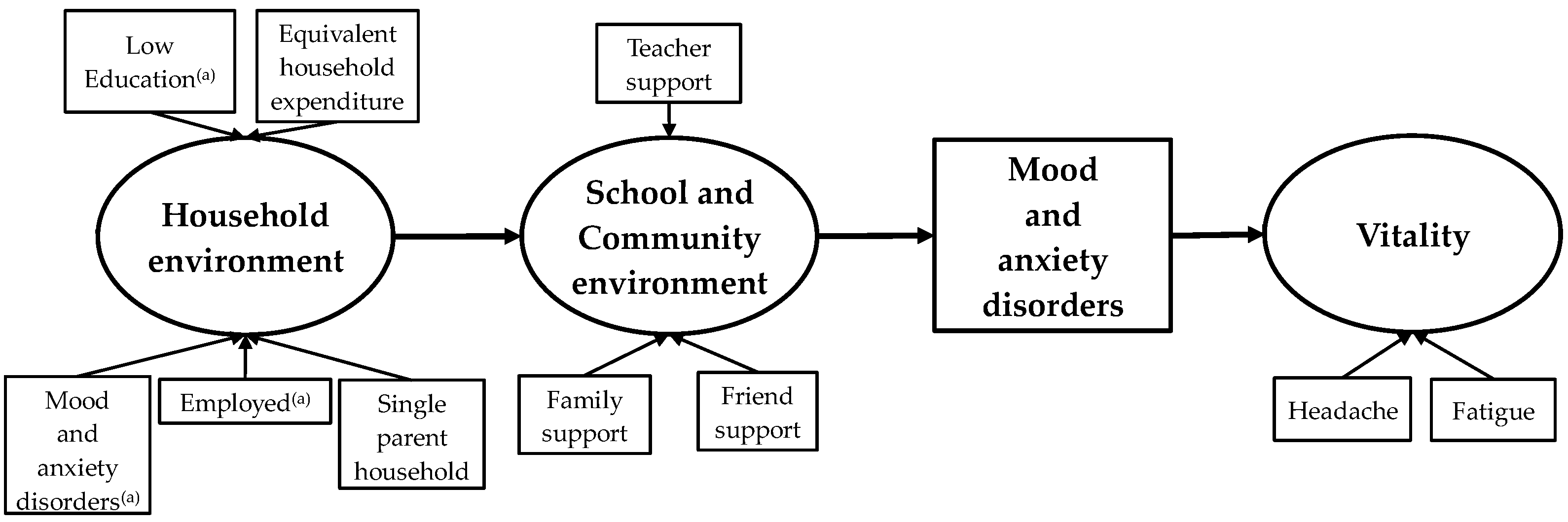
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants
2.3. Measures
2.3.1. Mental Health
2.3.2. Household Environment
2.3.3. School and Community Environment
2.3.4. Demographic Variables
2.4. Statistical Analysis
2.5. Ethical Considerations
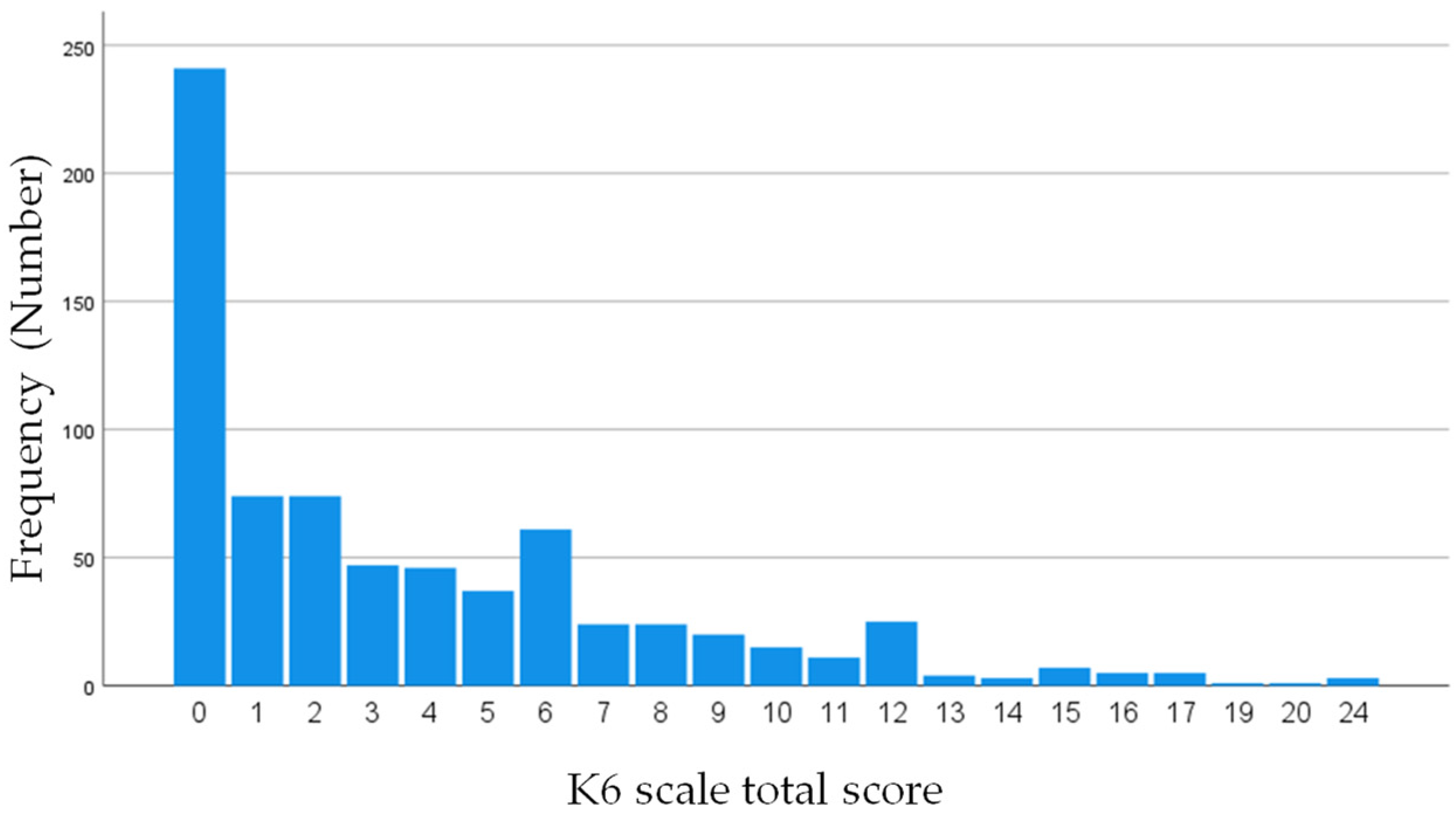
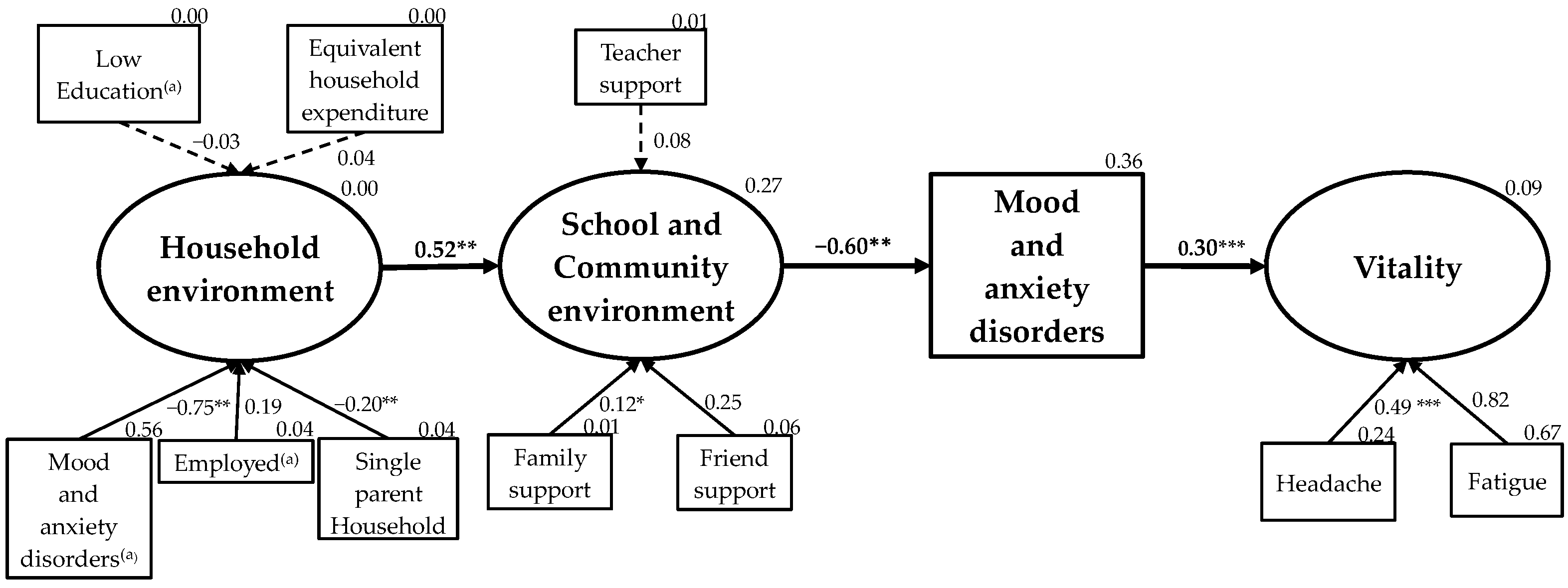
3. Results
4. Discussion
4.1. Model Validity
4.2. Japanese Adolescent Mood and Anxiety Disorders and Vitality: Strategies to Improve Mental Health and Related Factors
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kieling, C.; Baker-Henningham, H.; Belfer, M.; Conti, G.; Ertem, I.; Omigbodun, O.; Rohde, L.A.; Srinath, S.; Ulkuer, N.; Rahman, A. Child and Adolescent Mental Health Worldwide: Evidence for Action. Lancet 2011, 378, 1515–1525. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice, (Summary Report); World Health Organization: Geneva, Switzerland, 2004. Available online: https://apps.who.int/iris/bitstream/handle/10665/42940/9241591595.pdf (accessed on 4 October 2021).
- World Health Organization. Adolescent Mental Health. Available online: https://www-who-int.translate.goog/news-room/fact-sheets/detail/adolescent-mental-health?_x_tr_sl=en&_x_tr_tl=ja&_x_tr_hl=ja&_x_tr_pto=nui,op,sc (accessed on 14 October 2021).
- Hale, D.R.; Viner, R.M. How Adolescent Health Influences Education and Employment: Investigating Longitudinal Associations and Mechanisms. J. Epidemiol. Community Health 2018, 72, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Wasserman, D. Review of Health and Risk-Behaviours, Mental Health Problems and Suicidal Behaviours in Young Europeans on the Basis of the Results from the Eu-Funded Saving and Empowering Young Lives in Europe (SEYLE) Study. Psychiatr. Pol. 2016, 50, 1093–1107. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Green, J.G.; Hwang, I.; McLaughlin, K.A.; Sampson, N.A.; Zaslavsky, A.M.; Kessler, R.C. Prevalence, Correlates, and Treatment of Lifetime Suicidal Behavior among Adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry 2013, 70, 300–310. [Google Scholar] [CrossRef]
- Stapinski, L.A.; Montgomery, A.A.; Araya, R. Anxiety, Depression and Risk of Cannabis Use: Examining the Internalising Pathway to Use among Chilean Adolescents. Drug Alcohol Depend. 2016, 166, 109–115. [Google Scholar] [CrossRef]
- Weiss, J.W.; Mouttapa, M.; Cen, S.; Johnson, C.A.; Unger, J. Longitudinal Effects of Hostility, Depression, and Bullying on Adolescent Smoking Initiation. J. Adolesc. Health 2011, 48, 591–596. [Google Scholar] [CrossRef]
- Kim-Cohen, J.; Caspi, A.; Moffitt, T.E.; Harrington, H.L.; Milne, B.J.; Poulton, R. Prior Juvenile Diagnoses in Adults with Mental Disorder: Developmental Follow-Back of a Prospective-Longitudinal Cohort. Arch. Gen. Psychiatry 2003, 60, 709–717. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Hyakutake, A.; Kamijo, T.; Misawa, Y.; Washizuka, S.; Inaba, Y.; Tsukahara, T.; Nomiyama, T. Cross-Sectional Observation of the Relationship of Depressive Symptoms with Lifestyles and Parents’ Status among Japanese Junior High School Students. Environ. Health Prev. Med. 2016, 21, 265–273. [Google Scholar] [CrossRef]
- Ojio, Y.; Nishida, A.; Shimodera, S.; Togo, F.; Sasaki, T. Sleep Duration Associated with the Lowest Risk of Depression/Anxiety in Adolescents. Sleep 2016, 39, 1555–1562. [Google Scholar] [CrossRef]
- Ministry of Health Labour and Welfare of Japan. Patient Survey. Available online: https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00450022&tstat=000001031167 (accessed on 4 October 2021).
- Ryan, R.M.; Frederick, C. On Energy, Personality, and Health: Subjective Vitality as a Dynamic Reflection of Well-Being. J. Pers. 1997, 65, 529–565. [Google Scholar] [CrossRef]
- Gaston, J.E.; Vogl, L. Psychometric Properties of the General Well-Being Index. Qual. Life Res. 2005, 14, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.J.; Sherbourne, C.D. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Lucas, A.G.; Chang, E.C.; Morris, L.E.; Angoff, H.D.; Chang, O.D.; Duong, A.H.; Li, M.; Hirsch, J.K. Relationship between Hope and Quality of Life in Primary Care Patients: Vitality as a Mechanism. Soc. Work 2019, 64, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Balázs, J.; Miklósi, M.; Keresztény, A.; Hoven, C.W.; Carli, V.; Wasserman, C.; Hadlaczky, G.; Apter, A.; Bobes, J.; Brunner, R.; et al. Comorbidity of Physical and Anxiety Symptoms in Adolescent: Functional Impairment, Self-Rated Health and Subjective Well-Being. Int. J. Environ. Res. Public Health 2018, 15, 1698. [Google Scholar] [CrossRef]
- Guitera, V.; Muñoz, P.; Castillo, J.; Pascual, J. Quality of Life in Chronic Daily Headache: A Study in a General Population. Neurology 2002, 58, 1062–1065. [Google Scholar] [CrossRef]
- Bohman, H.; Jonsson, U.; Von Knorring, A.-L.; Von Knorring, L.; Päären, A.; Olsson, G. Somatic Symptoms as a Marker for Severity in Adolescent Depression. Acta Pædiatrica 2010, 99, 1724–1730. [Google Scholar] [CrossRef]
- Waza, K.; Graham, A.V.; Zyzanski, S.J.; Inoue, K. Comparison of Symptoms in Japanese and American Depressed Primary Care Patients. Fam. Pract. 1999, 16, 528–533. [Google Scholar] [CrossRef]
- Jörngården, A.; Mattsson, E.; von Essen, L. Health-Related Quality of Life, Anxiety and Depression among Adolescents and Young Adults with Cancer: A Prospective Longitudinal Study. Eur. J. Cancer 2007, 43, 1952–1958. [Google Scholar] [CrossRef]
- King, N.; Davison, C.M.; Pickett, W. Development of a Dual-Factor Measure of Adolescent Mental Health: An Analysis of Cross-Sectional Data from the 2014 Canadian Health Behaviour in School-Aged Children (HBSC) Study. BMJ Open 2021, 11, e041489. [Google Scholar] [CrossRef]
- Werner-Seidler, A.; Perry, Y.; Calear, A.L.; Newby, J.M.; Christensen, H. School-Based Depression and Anxiety Prevention Programs for Young People: A Systematic Review and Meta-Analysis. Clin. Psychol. Rev. 2017, 51, 30–47. [Google Scholar] [CrossRef] [PubMed]
- Schulte-Körne, G. Mental Health Problems in a School Setting in Children and Adolescents. Dtsch. Arztebl. Int. 2016, 113, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Smyth, N.; Siriwardhana, C.; Hotopf, M.; Hatch, S.L. Social Networks, Social Support and Psychiatric Symptoms: Social Determinants and Associations within a Multicultural Community Population. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1111–1120. [Google Scholar] [CrossRef] [PubMed]
- Mulvaney-Day, N.E.; Alegría, M.; Sribney, W. Social Cohesion, Social Support, and Health among Latinos in the United States. Soc. Sci. Med. 2007, 64, 477–495. [Google Scholar] [CrossRef]
- Devenish, B.; Hooley, M.; Mellor, D. The Pathways between Socioeconomic Status and Adolescent Outcomes: A Systematic Review. Am. J. Community Psychol. 2017, 59, 219–238. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design, 9th ed.; Harvard University Press: Cambridge, MA, USA, 1979; ISBN 9780674224575. [Google Scholar]
- Pilgrim, N.A.; Blum, R.W. Adolescent Mental and Physical Health in the English-Speaking Caribbean. Rev. Panam. Salud Pública 2012, 32, 62–69. [Google Scholar] [CrossRef][Green Version]
- Oriol, X.; Miranda, R.; Amutio, A.; Acosta, H.C.; Mendoza, M.C.; Torres-Vallejos, J. Violent Relationships at the Social-Ecological Level: A Multi-Mediation Model to Predict Adolescent Victimization by Peers, Bullying and Depression in Early and Late Adolescence. PLoS ONE 2017, 12, e0174139. [Google Scholar] [CrossRef]
- Piko, B.F.; Luszczynska, A.; Fitzpatrick, K.M. Social Inequalities in Adolescent Depression: The Role of Parental Social Support and Optimism. Int. J. Soc. Psychiatry 2013, 59, 474–481. [Google Scholar] [CrossRef]
- Rhee, S.; Lee, S.Y.; Jung, S.H. Ethnic Differences in Bullying Victimization and Psychological Distress: A Test of an Ecological Model. J. Adolesc. 2017, 60, 155–160. [Google Scholar] [CrossRef]
- Silberg, J.L.; Maes, H.; Eaves, L.J. Genetic and Environmental Influences on the Transmission of Parental Depression to Children’s Depression and Conduct Disturbance: An Extended Children of Twins Study. J. Child Psychol. Psychiatry Allied Discip. 2010, 51, 734–744. [Google Scholar] [CrossRef]
- Lee, D.E.; Kwon, S.W. Community-Level Factors and Adolescent Depression in South Korea: Socioeconomic Composition, Education Environment, and Community Wellbeing. Child Indic. Res. 2015, 8, 459–470. [Google Scholar] [CrossRef]
- Park, H.Y.; Heo, J.; Subramanian, S.V.; Kawachi, I.; Oh, J. Socioeconomic Inequalities in Adolescent Depression in South Korea: A Multilevel Analysis. PLoS ONE 2012, 7, e47025. [Google Scholar] [CrossRef] [PubMed]
- Hong, X.; Li, J.; Xu, F.; Tse, L.A.; Liang, Y.; Wang, Z.; Yu, I.T.S.; Griffiths, S. Physical Activity Inversely Associated with the Presence of Depression among Urban Adolescents in Regional China. BMC Public Health 2009, 9, 148. [Google Scholar] [CrossRef] [PubMed]
- Mizuta, A.; Suzuki, K.; Yamagata, Z.; Ojima, T. Teachers’ Support and Depression among Japanese Adolescents: A Multilevel Analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 211–219. [Google Scholar] [CrossRef]
- Muzi, S.; Rogier, G.; Pace, C.S. Peer Power! Secure Peer Attachment Mediates the Effect of Parental Attachment on Depressive Withdrawal of Teenagers. Int. J. Environ. Res. Public Health 2022, 19, 4068. [Google Scholar] [CrossRef]
- Gariépy, G.; Honkaniemi, H.; Quesnel-Vallée, A. Social Support and Protection from Depression: Systematic Review of Current Findings in Western Countries. Br. J. Psychiatry 2016, 209, 284–293. [Google Scholar] [CrossRef]
- Eugene, D.R. Connectedness to Family, School, and Neighborhood and Adolescents’ Internalizing Symptoms. Int. J. Environ. Res. Public Health 2021, 18, 12602. [Google Scholar] [CrossRef]
- Ministry of Health Labour and Welfare. Comprehensive Survey of Living Conditions. Available online: https://www.mhlw.go.jp/english/database/db-hss/cslc-index.html (accessed on 13 August 2021).
- Furukawa, T.A.; Kawakami, N.; Saitoh, M.; Ono, Y.; Nakane, Y.; Nakamura, Y.; Tachimori, H.; Iwata, N.; Uda, H.; Nakane, H.; et al. The Performance of the Japanese Version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 2008, 17, 152–158. [Google Scholar] [CrossRef]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.L.T.; Manderscheid, R.W.; Walters, E.E.; et al. Screening for Serious Mental Illness in the General Population. Arch. Gen. Psychiatry 2003, 60, 184–189. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Sung, H.Y.; Max, W.; Shi, Y.; Ong, M. Validity Study of the K6 Scale as a Measure of Moderate Mental Distress Based on Mental Health Treatment Need and Utilization. Int. J. Methods Psychiatr. Res. 2012, 21, 88–97. [Google Scholar] [CrossRef]
- Nishi, D.; Susukida, R.; Usuda, K.; Mojtabai, R.; Yamanouchi, Y. Trends in the Prevalence of Psychological Distress and the Use of Mental Health Services from 2007 to 2016 in Japan. J. Affect. Disord. 2018, 239, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Kachi, Y.; Otsuka, T.; Kawada, T. Socioeconomic Status and Overweight: A Population-Based Cross-Sectional Study of Japanese Children and Adolescents. J. Epidemiol. 2015, 25, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Van Loon, L.M.A.; Van de Ven, M.O.M.; Van Doesum, K.T.M.; Witteman, C.L.M.; Hosman, C.M.H. The Relation between Parental Mental Illness and Adolescent Mental Health: The Role of Family Factors. J. Child Fam. Stud. 2013, 23, 1201–1214. [Google Scholar] [CrossRef]
- Aguirre Velasco, A.; Cruz, I.S.S.; Billings, J.; Jimenez, M.; Rowe, S. What Are the Barriers, Facilitators and Interventions Targeting Help-Seeking Behaviours for Common Mental Health Problems in Adolescents? A Systematic Review. BMC Psychiatry 2020, 20, 293. [Google Scholar] [CrossRef]
- Leavey, G.; Rosato, M.; Harding, S.; Corry, D.; Divin, N.; Breslin, G. Adolescent Mental Health Problems, Suicidality and Seeking Help from General Practice: A Cross-Sectional Study (Northern Ireland Schools and Wellbeing Study). J. Affect. Disord. 2020, 274, 535–544. [Google Scholar] [CrossRef]
- Naicker, K.; Galambos, N.L.; Zeng, Y.; Senthilselvan, A.; Colman, I. Social, Demographic, and Health Outcomes in the 10 Years Following Adolescent Depression. J. Adolesc. Health 2013, 52, 533–538. [Google Scholar] [CrossRef] [PubMed]
- Margari, F.; Lucarelli, E.; Craig, F.; Petruzzelli, M.G.; Lecce, P.A.; Margari, L. Psychopathology in Children and Adolescents with Primary Headaches: Categorical and Dimensional Approaches. Cephalalgia 2013, 33, 1311–1318. [Google Scholar] [CrossRef] [PubMed]
- Ter Wolbeek, M.; Van Doornen, L.J.P.; Kavelaars, A.; Tersteeg-Kamperman, M.D.J.; Heijnen, C.J. Fatigue, Depressive Symptoms, and Anxiety from Adolescence up to Young Adulthood: A Longitudinal Study. Brain Behav. Immun. 2011, 25, 1249–1255. [Google Scholar] [CrossRef] [PubMed]
- Kristjánsdóttir, J.; Olsson, G.I.; Sundelin, C.; Naessen, T. Could SF-36 Be Used as a Screening Instrument for Depression in a Swedish Youth Population? Scand. J. Caring Sci. 2011, 25, 262–268. [Google Scholar] [CrossRef]

| N = 728 | |||
|---|---|---|---|
| Number | % | ||
| Demographic variables | |||
| Gender | Boys | 321 | 44.1 |
| Girls | 407 | 55.9 | |
| Household size (persons) | 2 | 20 | 2.7 |
| 3 | 128 | 17.6 | |
| 4 | 310 | 42.6 | |
| 5 | 179 | 24.6 | |
| 6 or more persons | 91 | 12.5 | |
| Household environment | |||
| Household structure | A couple and unmarried children only | 519 | 71.3 |
| Three-generation household | 110 | 15.1 | |
| Single parent and unmarried children only | 63 | 8.7 | |
| Other household | 36 | 4.9 | |
| Employment status of the household head | Employed | 668 | 91.8 |
| Not employed | 60 | 8.2 | |
| Educational attainment of the household head | Primary or junior high school | 68 | 9.3 |
| Completion of high school | 297 | 40.8 | |
| Vocational school | 77 | 10.6 | |
| Two-year college/technical college | 45 | 6.2 | |
| University | 218 | 29.9 | |
| Graduate school | 23 | 3.2 | |
| Equivalent household expenditure (Yen/A month) | 137,000 ± 67,000 | (13,000–608,000) | |
| Mood and anxiety disorders of the household head (K6 total score) | 3.8 ± 4.4 | (0–24) |
| N = 728 | |||
|---|---|---|---|
| Number | % | ||
| School and community environment | |||
| Mentor (Multiple answers) | 1. Family | 482 | 66.2 |
| 2. Friend | 400 | 54.9 | |
| 3. School teacher | 95 | 13.0 | |
| 4. Received counseling from a doctor at a hospital or clinic | 12 | 1.6 | |
| 5. Used the counseling services of public institutions | 6 | 0.8 | |
| 6. Consulted with someone other than the above | 4 | 0.5 | |
| 7. I do not consult with anyone because I do not need to consult | 86 | 11.8 | |
| 8. I would like to consult but cannot consult with anyone | 25 | 3.4 | |
| 9. I would like to consult but do not know where to consult | 14 | 1.9 | |
| Recategorized Mentor (Corresponds to the above number) | Family support (1) | 482 | 66.2 |
| Friend support (2) | 400 | 54.9 | |
| Teacher support (3) | 95 | 13.0 | |
| Other support (One or more of 4 to 6) | 20 | 2.7 | |
| No social support (8 or 9) | 31 | 4.3 | |
| Mood and anxiety disorders | |||
| Adolescents’ K6 total score | 3.7 ± 4.3 | (0–24) | |
| Severity | Standard (K6 total score: 0–4) | 482 | 66.2 |
| Moderate (K6 total score: 5–13) | 217 | 29.8 | |
| Severe (K6 total score: 14–24) | 29 | 4.0 | |
| Vitality | |||
| Somatic symptoms (Multiple answers) | Headache | 42 | 5.8 |
| Fatigue | 41 | 5.6 | |
| Irritability | 27 | 3.7 | |
| Stomachache | 23 | 3.2 | |
| Dizziness | 17 | 2.3 | |
| Difficulty falling asleep | 12 | 1.6 | |
| Anorexia | 6 | 0.8 |
| N = 728 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | |
| 1. Gender (2 = Girl) | 1 | ||||||||||
| 2. Single parent household (1 = Yes) | −0.042 | 1 | |||||||||
| 3. Employed (a) (1 = Yes) | −0.015 | −0.014 | 1 | ||||||||
| 4. Low education (a) (1 = Yes) | −0.086 * | −0.015 | −0.178 ** | 1 | |||||||
| 5. Equivalent household expenditure (Yen) | −0.061 † | −0.187 ** | 0.012 | −0.130 ** | 1 | ||||||
| 6. Mood and anxiety disorders (a) | −0.060 | 0.193 ** | −0.083 * | −0.003 | −0.004 | 1 | |||||
| 7. Family support (1 = Yes) | 0.103 * | 0.034 | 0.092 * | −0.080 * | 0.007 | −0.032 | 1 | ||||
| 8. Friend support (1 = Yes) | 0.213 ** | −0.055 | −0.020 | −0.041 | 0.006 | 0.006 | 0.129 ** | 1 | |||
| 9. Teacher support (1 = Yes) | −0.001 | 0.026 | −0.047 | 0.002 | −0.061 † | −0.046 | 0.130 ** | 0.031 | 1 | ||
| 10. Fatigue (1 = Yes) | 0.001 | 0.073 * | −0.035 | 0.024 | 0.007 | 0.006 | −0.014 | −0.042 | 0.029 | 1 | |
| 11. Headache (1 = Yes) | 0.065 † | 0.008 | −0.076 * | 0.002 | 0.011 | −0.002 | −0.010 | −0.025 | 0.044 | 0.400 ** | 1 |
| 12. Mood and anxiety disorders of adolescents | −0.030 | 0.042 | −0.073 * | 0.047 | 0.040 | 0.265 ** | −0.083 * | −0.032 | 0.024 | 0.223 ** | 0.149 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mori, N.; Arimoto, A.; Tadaka, E. Exploring an Applied Ecological Model of the Effects of Household, School, and Community Environments on Adolescent Mental Health in Japan. Int. J. Environ. Res. Public Health 2022, 19, 16820. https://doi.org/10.3390/ijerph192416820
Mori N, Arimoto A, Tadaka E. Exploring an Applied Ecological Model of the Effects of Household, School, and Community Environments on Adolescent Mental Health in Japan. International Journal of Environmental Research and Public Health. 2022; 19(24):16820. https://doi.org/10.3390/ijerph192416820
Chicago/Turabian StyleMori, Nagisa, Azusa Arimoto, and Etsuko Tadaka. 2022. "Exploring an Applied Ecological Model of the Effects of Household, School, and Community Environments on Adolescent Mental Health in Japan" International Journal of Environmental Research and Public Health 19, no. 24: 16820. https://doi.org/10.3390/ijerph192416820
APA StyleMori, N., Arimoto, A., & Tadaka, E. (2022). Exploring an Applied Ecological Model of the Effects of Household, School, and Community Environments on Adolescent Mental Health in Japan. International Journal of Environmental Research and Public Health, 19(24), 16820. https://doi.org/10.3390/ijerph192416820






