The Effect of Fire Smoke Exposure on Firefighters’ Lung Function: A Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Design and Eligibility Criteria
2.3. Data Extraction
2.4. Statistical Analysis
2.5. Risk of Bias Assessment
3. Results
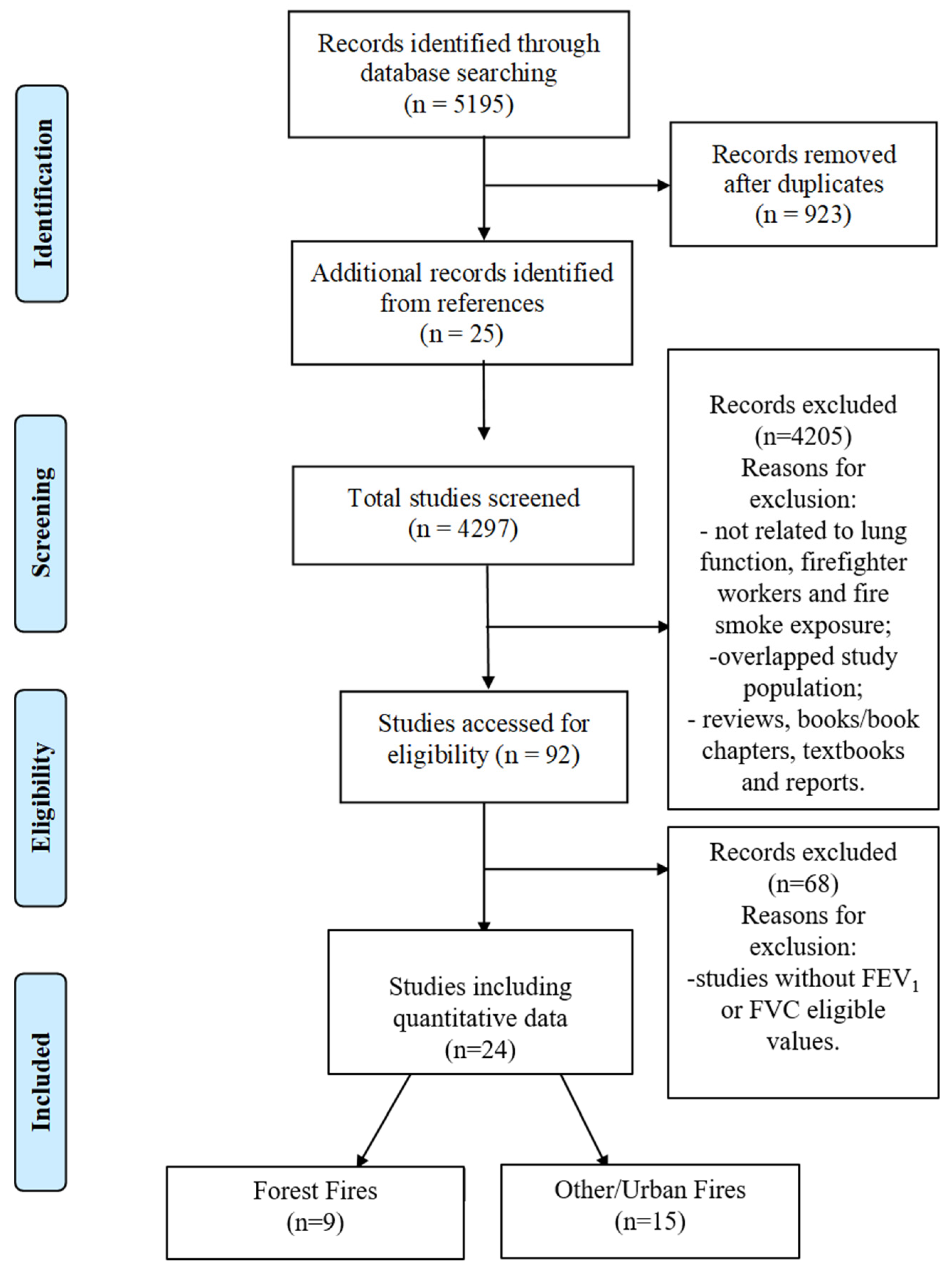
3.1. Literature Search and Study Characterisation
3.2. Lung Function Data
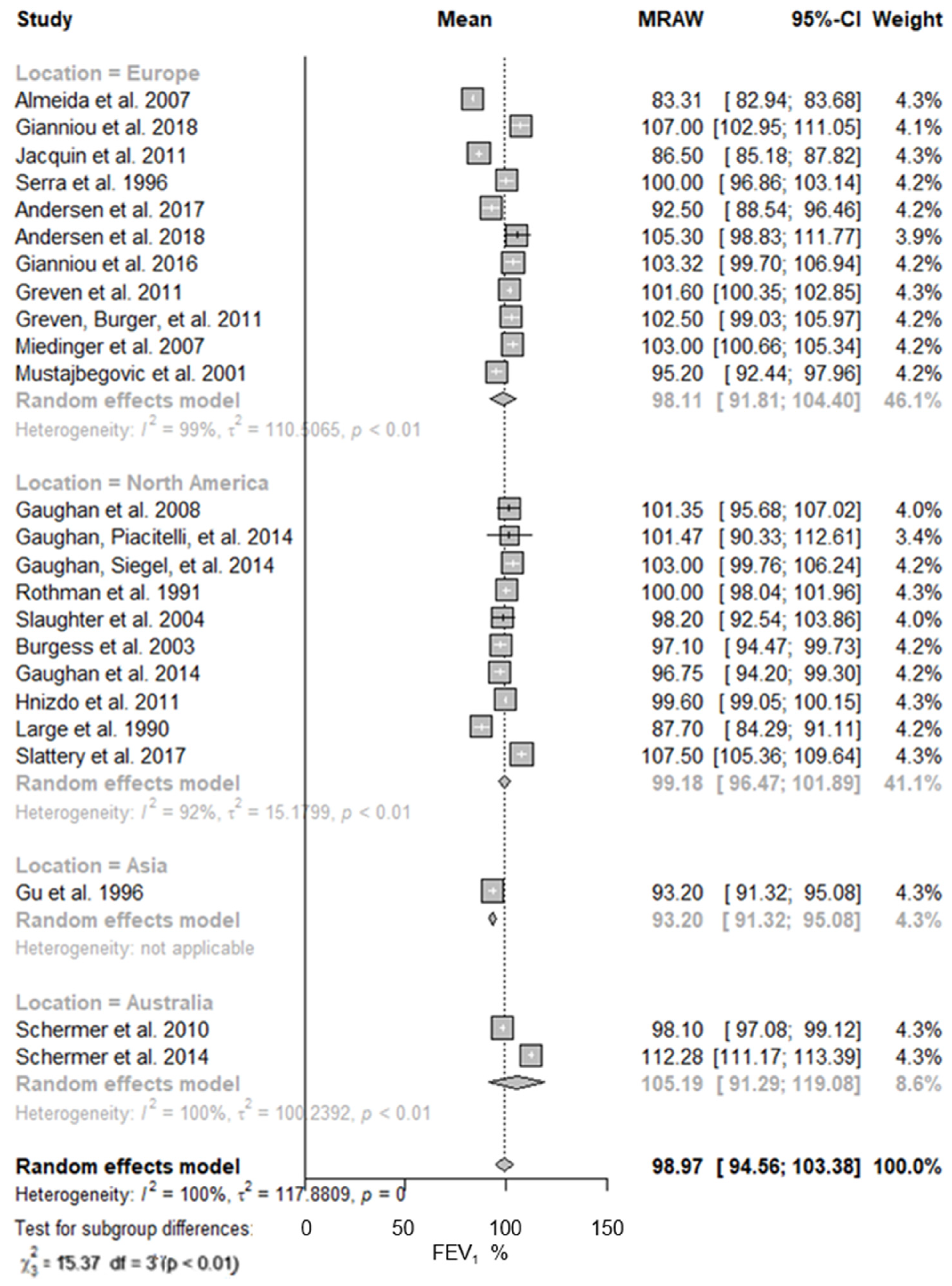
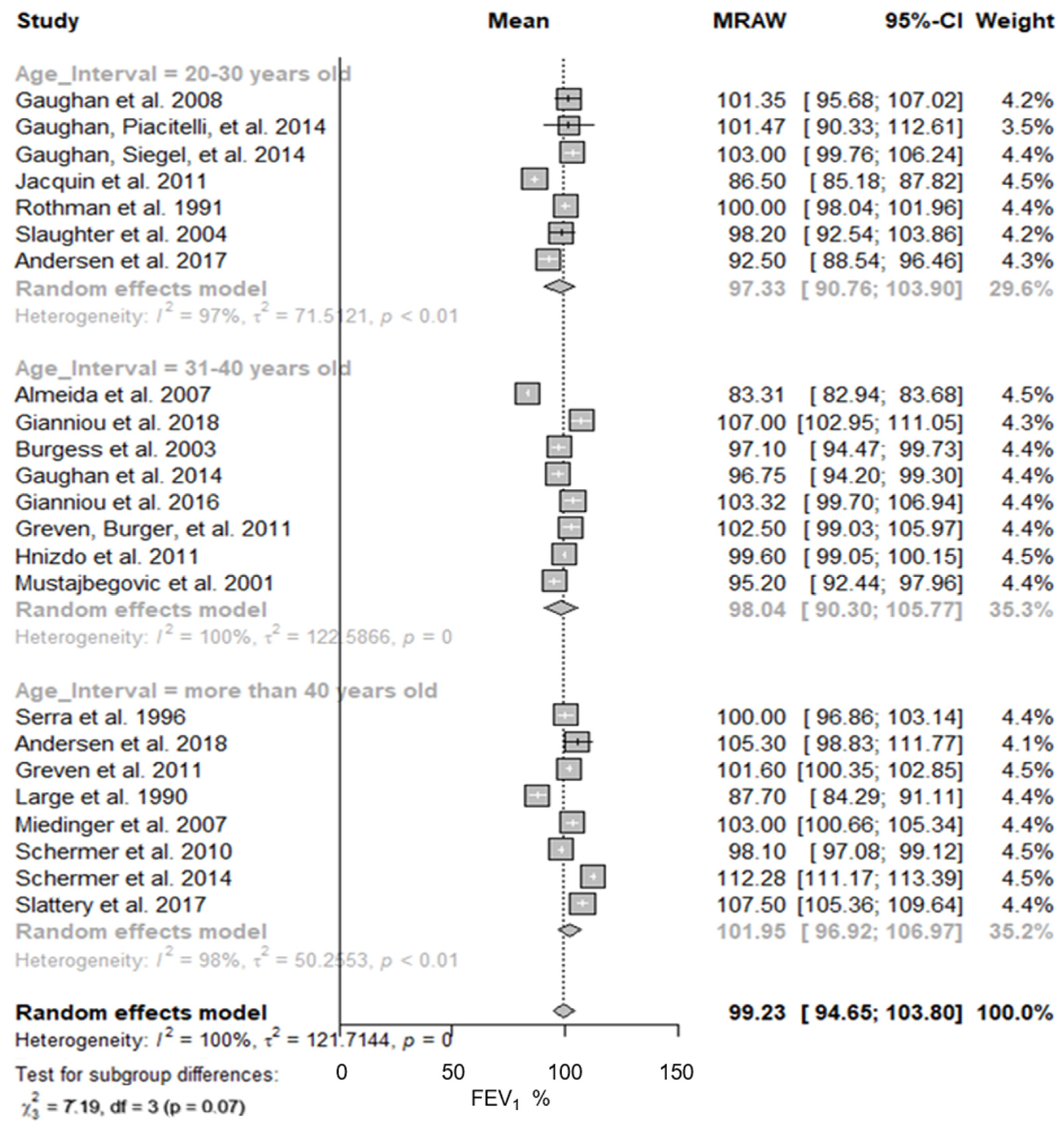
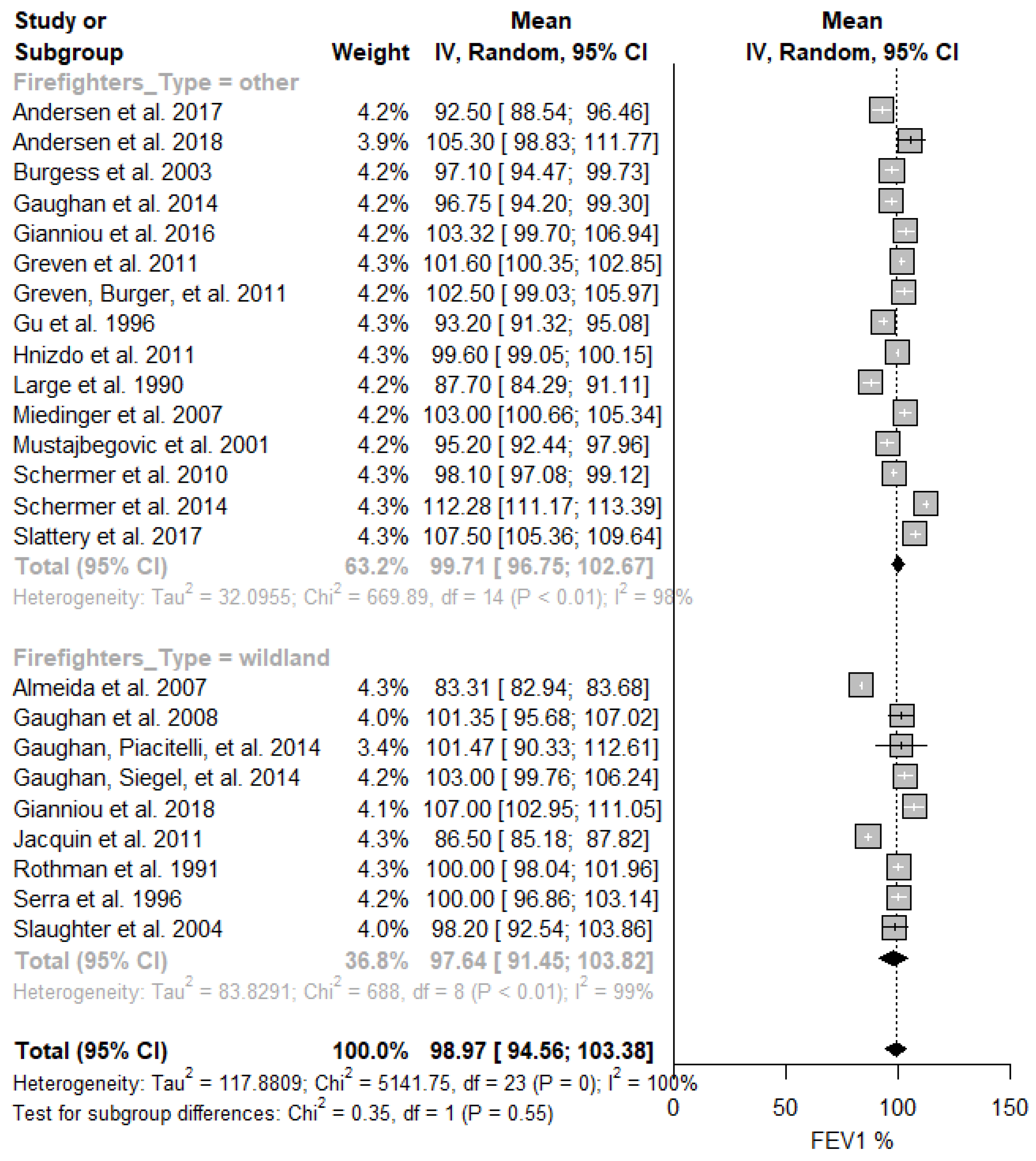
3.2.1. Sub-Group Analysis
3.2.2. Risk of Bias
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vardoulakis, S.; Jalaludin, B.B.; Morgan, G.G.; Hanigan, I.C.; Johnston, F.H. Bushfire smoke: Urgent need for a national health protection strategy. Med. J. Aust. 2020, 212, 349–353.e1. [Google Scholar] [CrossRef]
- Miranda, A.I.; Martins, V.; Cascão, P.; Amorim, J.H.; Valente, J.; Borrego, C.; Ferreira, A.J.; Cordeiro, C.R.; Viegas, D.X.; Ottmar, R. Wildland Smoke Exposure Values and Exhaled Breath Indicators in Firefighters. J. Toxicol. Environ. Health A 2012, 75, 831–843. [Google Scholar] [CrossRef]
- Fann, N.; Alman, B.; Broome, R.A.; Morgan, G.G.; Johnston, F.H.; Pouliot, G.; Rappold, A.G. The health impacts and economic value of wildland fire episodes in the U.S.: 2008–2012. Sci. Total Environ. 2018, 610–611, 802–809. [Google Scholar] [CrossRef]
- Black, C.; Tesfaigzi, Y.; Bassein, J.A.; Miller, L.A. Wildfire smoke exposure and human health: Significant gaps in research for a growing public health issue. Environ. Toxicol. Pharmacol. 2017, 55, 186–195. [Google Scholar] [CrossRef]
- Caamano-isorna, F.; Figueiras, A.; Sastre, I.; Montes-martínez, A.; Taracido, M. Respiratory and mental health effects of wildfires: An ecological study in Galician municipalities (north-west Spain). Environ. Health 2011, 10, 48. [Google Scholar] [CrossRef]
- Goldammer, J.G.; Statheropoulos, M.; Andreae, M.O. Chapter 1 Impacts of Vegetation Fire Emissions on the Environment, Human Health, and Security: A Global Perspective. Dev. Environ. Sci. 2008, 8, 3–36. [Google Scholar]
- Cascio, W.E. Wildland fire smoke and human health. Sci. Total Environ. 2018, 624, 586–595. [Google Scholar] [CrossRef]
- Vicedo-Cabrera, A.M.; Esplugues, A.; Iñíguez, C.; Estarlich, M.; Ballester, F. Health effects of the 2012 Valencia (Spain) wildfires on children in a cohort study. Environ. Geochem. Health 2016, 38, 703–712. [Google Scholar] [CrossRef]
- Clements, B.W.; Casani, J.A.P. Disasters and Public Health: Planning and Response, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar] [CrossRef]
- Groot, E.; Caturay, A.; Khan, Y.; Copes, R.A.Y. A systematic review of the health impacts of occupational exposure to wildland fires. Int. J. Occup. Med. Environ. Health 2019, 32, 121–140. [Google Scholar] [CrossRef]
- Kodom-Wiredu, J.K. The Relationship between Firefighters’ Work Demand and Work-related Musculoskeletal Disorders: The Moderating Role of Task Characteristics. Saf. Health Work 2019, 10, 61–66. [Google Scholar] [CrossRef]
- Adetona, O.; Reinhardt, T.E.; Domitrovich, J.; Broyles, G.; Adetona, A.M.; Kleinman, M.T.; Ottmar, R.D.; Naeher, L.P. Review of the health effects of wildland fire smoke on wildland firefighters and the public. Inhal. Toxicol. 2016, 28, 95–139. [Google Scholar] [CrossRef]
- Gaughan, D.M.; Cox-Ganser, J.M.; Enright, P.L.; Castellan, R.M.; Wagner, G.R.; Hobbs, G.R. Acute upper and lower respiratory effects in wildland firefighters. J. Occup. Environ. Med. 2008, 50, 1019–1028. [Google Scholar] [CrossRef]
- Doney, B.; Hnizdo, E.; Graziani, M.; Kullman, G.; Burchfiel, C.; Baron, S.; Fujishiro, K.; Enright, P.; Hankinson, J.L.; Stukovsky, K.H.; et al. Occupational risk factors for COPD phenotypes in the multi-ethnic study of atherosclerosis (mesa) lung study. COPD J. Chronic Obstr. Pulm. Dis. 2014, 11, 368–380. [Google Scholar] [CrossRef]
- Wettstein, Z.S.; Hoshiko, S.; Fahimi, J.; Harrison, R.J.; Cascio, W.E.; Rappold, A.G. Cardiovascular and cerebrovascular emergency department visits associated with wildfire smoke exposure in California in 2015. J. Am. Heart Assoc. 2018, 7, e007492. [Google Scholar] [CrossRef]
- Halbeisen, F.S.; Jose, A.; de Jong, C.; Nyilas, S.; Latzin, P.; Kuehni, C.E.; Goutaki, M. Spirometric indices in primary ciliary dyskinesia: Systematic review and meta-analysis. ERJ Open Res. 2019, 5, 00231–02018. [Google Scholar] [CrossRef]
- Divo, M.J.; Casanova, C.; Marin, J.M.; Pinto-Plata, V.M.; De-Torres, J.P.; Zulueta, J.J.; Cabrera, C.; Zagaceta, J.; Sanchez-Salcedo, P.; Berto, J.; et al. COPD comorbidities network. Eur. Respir. J. 2015, 46, 640–650. [Google Scholar] [CrossRef]
- Raherison, C.; Ouaalaya, E.H.; Bernady, A.; Casteigt, J.; Nocent-Eijnani, C.; Falque, L.; Guillou, F.L.; Nguyen, L.; Ozier, A.; Molimard, M. Comorbidities and COPD severity in a clinic-based cohort. BMC Pulm. Med. 2018, 18, 117. [Google Scholar] [CrossRef]
- Slattery, F.; Johnston, K.; Paquet, C.; Bennett, H.; Crockett, A. The long-term rate of change in lung function in urban professional firefighters: A systematic review. BMC Pulm. Med. 2018, 18, 149. [Google Scholar] [CrossRef]
- Aldrich, T.K.; Ye, F.; Hall, C.B.; Webber, M.P.; Cohen, H.W.; Dinkels, M.; Cosenza, K.; Weiden, M.D.; Nolan, A.; Christodoulou, V.; et al. Longitudinal pulmonary function in newly hired, non-world trade center-exposed fire department city of New York firefighters: The first 5 years. Chest 2013, 143, 791–797. [Google Scholar] [CrossRef][Green Version]
- Schermer, T.R.; Malbon, W.; Adams, R.; Morgan, M.; Smith, M.; Crockett, A.J. Change in lung function over time in male metropolitan firefighters and general population controls: A 3-year follow-up study. J. Occup. Health 2013, 55, 267–275. [Google Scholar] [CrossRef]
- Chowdhury, R.; Shah, D.; Payal, A.R. Healthy Worker Effect Phenomenon: Revisited with Emphasis on Statistical Methods—A Review. Indian J. Occup. Environ. Med. 2017, 21, 2–8. [Google Scholar] [CrossRef]
- Li, C.Y.; Sung, F.C. A review of the healthy worker effect in occupational epidemiology. Occup. Med. 1999, 49, 225–229. [Google Scholar] [CrossRef]
- Berninger, A.; Webber, M.P.; Weakley, J.; Gustave, J.; Zeig-Owens, R.; Lee, R.; Al-Othman, F.; Cohen, H.W.; Kelly, K.; Prezant, D.J. Quality of life in relation to upper and lower respiratory conditions among retired 9/11-exposed firefighters with pulmonary disability. Qual. Life Res. 2010, 19, 1467–1476. [Google Scholar] [CrossRef]
- Weakley, J.; Webber, M.P.; Gustave, J.; Kelly, K.; Cohen, H.W.; Hall, C.B.; Prezant, D.J. Trends in respiratory diagnoses and symptoms of firefighters exposed to the World Trade Center disaster: 2005–2010. Prev. Med. 2011, 53, 364–369. [Google Scholar] [CrossRef]
- Soo, J.; Webber, M.P.; Hall, C.B.; Cohen, H.W.; Schwartz, T.M.; Kelly, K.J.; Prezant, D.J. Pulmonary function predicting confirmed recovery from lower-respiratory symptoms in world trade center-exposed firefighters, 2001 to 2010. Chest 2012, 142, 1244–1250. [Google Scholar] [CrossRef][Green Version]
- Hejl, A.M.; Adetona, O.; Diaz-Sanchez, D.; Carter, J.D.; Commodore, A.A.; Rathbun, S.L.; Naeher, L.P. Inflammatory effects of woodsmoke exposure among wildland firefighters working at prescribed burns at the savannah river site, SC. J. Occup. Environ. Hyg. 2013, 10, 173–180. [Google Scholar] [CrossRef]
- Barboni, T.; Cannac, M.; Pasqualini, V.; Simeoni, A.; Leoni, E.; Chiaramonti, N. Volatile and semi-volatile organic compounds in smoke exposure of firefighters during prescribed burning in the Mediterranean region. Int. J. Wildl. Fire 2010, 19, 606. [Google Scholar] [CrossRef]
- Wu, C.M.; Warren, S.H.; Demarini, D.M.; Song, C.C.; Adetona, O. Urinary mutagenicity and oxidative status of wildland firefighters working at prescribed burns in a Midwestern US forest. Occup. Environ. Med. 2020, 78, 1–8. [Google Scholar] [CrossRef]
- Adetona, O.; Dunn, K.; Hall, D.B.; Achtemeier, G.; Stock, A.; Naeher, L.P. Personal PM2.5 exposure among wildland firefighters working at prescribed forest burns in Southeastern United States. J. Occup. Environ. Hyg. 2011, 8, 503–511. [Google Scholar] [CrossRef]
- Betchley, C.; Koenig, J.Q.; Belle, G.; van Checkoway, H.; Reinhardt, T. Pulmonary Function and Respiratory Symptoms in Forest Firefighters. J. Occup. Environ. Med. 1997, 31, 503–509. [Google Scholar] [CrossRef]
- Harvey, S.B.; Milligan-Saville, J.S.; Paterson, H.M.; Harkness, E.L.; Marsh, A.M.; Dobson, M.; Kemp, R.; Bryant, R.A. The mental health of fire-fighters: An examination of the impact of repeated trauma exposure. Aust. N. Z. J. Psychiatry 2016, 50, 649–658. [Google Scholar] [CrossRef]
- Stanley, I.H.; Boffa, J.W.; Hom, M.A.; Kimbrel, N.A.; Joiner, T.E. Differences in psychiatric symptoms and barriers to mental health care between volunteer and career firefighters. Psychiatry Res. 2017, 247, 236–242. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Chin. Integr. Med. 2009, 7, 889–896. [Google Scholar] [CrossRef]
- Quanjer, P.H.; Stanojevic, S.; Cole, T.J.; Baur, X.; Hall, G.L.; Culver, B.H.; Enright, P.L.; Hankinson, J.L.; Ip, M.S.M.; Zheng, J.; et al. Multi-ethnic Reference Values for Spırometry for the 3–95 Year Age Range: The Global Lung Functıon 2012 Equations: Report of the Global Lung Function Initiative (GLI), ERS Task Force to establish improved Lung Function Reference Values. Eur. Respir. J. 2012, 40, 1324–1343. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2011; Available online: www.handbook.cochrane.org (accessed on 12 May 2021).
- Schwarzer, G. Meta: An R Package for Meta-Analysis. R News. 2007. Available online: http://cran.r-project.org/doc/Rnews/ (accessed on 21 April 2021).
- Aromataris, E.; Munn, Z. JBI Manual for Evidence Synthesis. 2020. Available online: https://jbi-global-wiki.refined.site/space/MANUAL (accessed on 18 June 2021).
- Study Quality Assessment Tools. National Heart, Lung, and Blood Institute. 2018. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 31 May 2021).
- Almeida, A.G.; Duarte, R.; Mieiro, L.; Paiva, A.C.; Rodrigues, A.M.; Almeida, M.H. Pulmonary function in Portuguese firefighters. Rev. Port. Pneumol. A 2007, 13, 349–364. [Google Scholar] [CrossRef]
- Gaughan, D.M.; Piacitelli, C.A.; Chen, B.T.; Law, B.F.; Virji, M.A.; Edwards, N.T.; Enright, P.L.; Schwegler-Berry, D.E.; Leonard, S.S.; Wagner, G.R.; et al. Exposures and cross-shift lung function declines in wildland firefighters. J. Occup. Environ. Hyg. 2014, 11, 591–603. [Google Scholar] [CrossRef]
- Gaughan, D.M.; Siegel, Ã.P.D.; Hughes, M.D.; Chang, C.; Law, B.F.; Campbell, C.R.; Richards, J.C.; Kales, S.F.; Chertok, M.; Kobzik, L.; et al. Arterial Stiffness, Oxidative Stress, and Smoke Exposure in Wildland Firefighters. Am. J. Ind. Med. 2014, 756, 748–756. [Google Scholar] [CrossRef]
- Gianniou, N.; Giannakopoulou, C.-E.; Dima, E.; Kardara, M.; Katsaounou, P.; Tsakatikas, A.; Roussos, C.; Koulouris, N.; Rovina, N. Acute effects of smoke exposure on airway and systemic inflammation in forest firefighters. J. Asthma Allergy 2018, 11, 81–88. [Google Scholar] [CrossRef]
- Jacquin, L.; Michelet, P.; Brocq, F.X.; Houel, J.G.; Truchet, X.; Auffray, J.P.; Carpentier, J.P.; Jammes, Y. Short-term spirometric changes in wildland firefighters. Am. J. Ind. Med. 2011, 54, 819–825. [Google Scholar] [CrossRef]
- Rothman, N.; Ford, D.P.; Baser, M.E.; Hansen, J.A.; O’Toole, T.; Tockman, M.S.; Strickland, P.T. Pulmonary Function and Respiratory Symptoms in Wildland Firefighters. J. Occup. Med. 1991, 33, 1163–1167. [Google Scholar]
- Serra, A.; Mocci, F.; Randaccio, F.S. Pulmonary function in Sardinian fire fighters. Am. J. Ind. Med. 1996, 30, 78–82. [Google Scholar] [CrossRef]
- Slaughter, J.C.; Koenig, J.Q.; Reinhardt, T.E. Association between Lung Function and Exposure to Smoke among Firefighters at Prescribed Burns. J. Occup. Environ. Hyg. 2004, 1, 45–49. [Google Scholar] [CrossRef]
- Andersen, M.H.G.; Saber, A.T.; Clausen, P.A.; Pedersen, J.E.; Løhr, M.; Kermanizadeh, A.; Loft, S.; Ebbehøj, N.; Hansen, Å.M.; Pedersen, P.B.; et al. Association between polycyclic aromatic hydrocarbon exposure and peripheral blood mononuclear cell DNA damage in human volunteers during fire extinction exercises. Mutagenesis 2017, 33, 105–115. [Google Scholar] [CrossRef]
- Andersen, M.H.G.; Saber, A.T.; Pedersen, J.E.; Pedersen, P.B.B.; Clausen, P.A.; Løhr, M.; Kermanizadeh, A.; Loft, S.; Ebbehøj, N.E.; Hansen, Å.M. Assessment of polycyclic aromatic hydrocarbon exposure, lung function, systemic inflammation, and genotoxicity in peripheral blood mononuclear cells from firefighters before and after a work shift. Environ. Mol. Mutagen. 2018, 59, 539–548. [Google Scholar] [CrossRef]
- Burgess, J.L.; Witten, M.L.; Nanson, C.J.; Hysong, T.A.; Sherrill, D.L.; Quan, S.F.; Gerkin, R.; Bernard, A.M. Serum pneumoproteins: A cross-sectional comparison of firefighters and police. Am. J. Ind. Med. 2003, 44, 246–253. [Google Scholar] [CrossRef]
- Gaughan, D.M.; Christiani, D.C.; Hughes, M.D.; Baur, D.M.; Kobzik, L.; Wagner, G.R.; Kales, S.N. High hsCRP is associated with reduced lung function in structural firefighters. Am. J. Ind. Med. 2014, 57, 31–37. [Google Scholar] [CrossRef]
- Gianniou, N.; Katsaounou, P.; Dima, E.; Giannakopoulou, C.E.; Kardara, M.; Saltagianni, V.; Trigidou, R.; Kokkini, A.; Bakakos, P.; Markozannes, E. Prolonged occupational exposure leads to allergic airway sensitization and chronic airway and systemic inflammation in professional firefighters. Respir. Med. 2016, 118, 7–14. [Google Scholar] [CrossRef]
- Greven, F.E.; Krop, E.J.; Spithoven, J.J.; Burger, N.; Rooyackers, J.M.; Kerstjens, H.A.; van der Heide, S.; Heederik, D.J. Acute respiratory effects in firefighters. Am. J. Ind. Med. 2011, 55, 54–62. [Google Scholar] [CrossRef]
- Greven, F.; Krop, E.; Spithoven, J.; Rooyackers, J.; Kerstjens, H.; Heederik, D. Lung function, bronchial hyperresponsiveness, and atopy among firefighters. Scand. J. Work Environ. Health 2011, 37, 325–331. [Google Scholar] [CrossRef][Green Version]
- Gu, T.-L.; Liou, S.-H.; Hsu, C.-H.; Hsu, J.-C.; Wu, T.-N. Acute Health Hazards of Firefighters after Fighting a Department Store Fire. Ind. Health 1996, 34, 13–23. [Google Scholar] [CrossRef]
- Hnizdo, E.; Hakobyan, A.; Fleming, J.L.; Beeckman-Wagner, L.A. Periodic spirometry in occupational setting: Improving quality, accuracy, and precision. J. Occup. Environ. Med. 2011, 53, 1205–1209. [Google Scholar] [CrossRef] [PubMed]
- Large, A.A.; Owens, G.R.; Hoffman, L.A. The short-term effects of smoke exposure on the pulmonary function of firefighters. Chest. Am. Coll. Chest Physicians 1990, 97, 806–809. [Google Scholar]
- Miedinger, D.; Chhajed, P.N.; Stolz, D.; Gysin, C.; Wanzenried, A.B.; Schindler, C.; Surber, C.; Bucher, H.C.; Tamm, M.; Leuppi, J.D. Respiratory symptoms, atopy and bronchial hyperreactivity in professional firefighters. Eur. Respir. J. 2007, 30, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Mustajbegovic, J.; Zuskin, E.; Schachter, E.N.; Kern, J.; Vrcic-Keglevic, M.; Heimer, S.; Vitale, K.; Nada, T. Respiratory function in active firefighters. Am. J. Ind. Med. 2001, 40, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Schermer, T.; Malbon, W.; Newbury, W.; Holton, C.; Smith, M.; Morgan, M.; Crockett, A. Spirometry and impulse oscillometry (IOS) for detection of respiratory abnormalities in metropolitan firefighters. Respirology 2010, 15, 975–985. [Google Scholar] [CrossRef] [PubMed]
- Schermer, T.R.; Malbon, W.; Morgan, M.; Smith, M.; Crockett, A.J. Chronic respiratory conditions in a cohort of metropolitan fire-fighters: Associations with occupational exposure and quality of life. Int. Arch. Occup. Environ. Health 2014, 87, 919–928. [Google Scholar] [CrossRef][Green Version]
- Slattery, F.; Schermer, T.; Esterman, A.; Johnston, K.; Crockett, A. The Global Lung Function Initiative 2012 Equations Are as Well-Suited as Local Population Derived Equations to a Sample of Healthy Professional Firefighters. Can. Respir. J. 2017, 2017, 6327180. [Google Scholar] [CrossRef]
- Quanjer, P.H.; Weiner, D.J. Interpretative consequences of adopting the global lungs 2012 reference equations for spirometry for children and adolescents. Pediatr. Pulmonol. 2014, 49, 118–125. [Google Scholar] [CrossRef]
- Shah, D. Healthy worker effect phenomenon. Indian J. Occup. Environ. Med. 2009, 13, 77–79. [Google Scholar] [CrossRef]
- Sharma, G.; Goodwin, J. Effect of aging on respiratory system physiology and immunology. Clin. Interv. Aging 2006, 1, 253–260. [Google Scholar] [CrossRef]
- Kales, S.N.; Polyhronopoulos, G.N.; Christiani, D.C. Medical surveillance of hazardous materials response fire fighters: A two-year prospective study. J. Occup. Environ. Med. 1997, 39, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Landrigan, P.J.; Lioy, P.J.; Thurston, G.; Berkowitz, G.; Chen, L.C.; Chillrud, S.N.; Gavett, S.H.; Georgopoulos, P.G.; Geyh, A.S.; Levin, S.; et al. Health and environmental consequences of the World Trade Center disaster. Environ. Health Perspect. 2004, 112, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Hena, K.M.; Yip, J.; Jaber, N.; Goldfarb, D.; Fullam, K.; Cleven, K.; Moir, W.; Zeig-Owens, R.; Webber, M.P.; Spevack, D.M.; et al. Clinical Course of Sarcoidosis in World Trade Center-Exposed Firefighters. Chest 2018, 153, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Horn, G.P.; Kerber, S.; Fent, W.; Fernhall, B.; Smith, D.L. Cardiovascular & Chemical Exposure Risks in Modern Firefighting. 2016. Available online: https://www.fsi.illinois.edu/documents/research/CardioChemRisksModernFF_InterimReport2016.pdf (accessed on 20 October 2021).


| Study | Design | Location | Sample Size | Mean Age (Years) | Main Objective |
|---|---|---|---|---|---|
| Wildland fires | |||||
| Almeida et al. (2007) [40] | cross sectional | Portugal | 203 | 37.5 | To assess the lung function in active firefighters. |
| Gaughan et al. (2008) [13] | cross-shift | USA | 58 | 26.0 | To assess the acute respiratory effects experienced by firefighters. |
| Gaughan et al. (2014) [41] | cross-shift | USA | 17 | 26.0 | To characterise exposures of firefighters and examine their effects on lung function changes. |
| Gaughan et al. (2014) [42] | cross sectional | USA | 38 | 29.0 | To assess the association between exposure, oxidative stress, cardiorespiratory function and symptoms in firefighters. |
| Gianniou et al. (2018) [43] | cross season | Greece | 60 | 32.4 | To assess post-exposure respiratory health and inflammation in firefighters with acute exposure to forest fire smoke. |
| Jacquin et al. (2011) [44] | cross season | Corsica | 108 | 24.7 | To evaluate the acute decline of the lung function and its persistence after a fire season in firefighters. |
| Rothman et al. (1991) [45] | cross season | USA | 52 | 26.0 | To evaluate the effects of firefighting on forced expiratory flow and respiratory symptoms. |
| Serra et al. (1996) [46] | cross sectional | Sardinia | 92 | 40.9 | To compare the respiratory function of firefighters with that of a control group. |
| Slaughter et al. (2004) [47] | cross-shift | USA | 65 | 29.0 | Short-term effects of exposures to fire smoke pollutants on the lung function of firefighters performing prescribed burns. |
| Other/Urban fires | |||||
| Andersen et al. (2017) [48] | cross-shift | Danish | 53 | 21.4 | To investigate the effect of firefighters’ activities on lung function, systemic inflammation and DNA. |
| Andersen et al. (2018) [49] | cross-shift | Danish | 22 | 51.7 | To investigate PAH exposure, lung function, systemic inflammation and DNA damage in firefighters after a day of work. |
| Burgess et al. (2003) [50] | cross sectional | USA | 105 | 39.8 | To evaluate biomarkers of lung injury resulting from occupational fire smoke exposure comparing firefighters and police officers. |
| Gaughan et al. (2014) [51] | cross sectional | USA | 401 | 36.0 | To assess the association between markers of systemic inflammation and lung function in firefighters. |
| Gianniou et al. (2016) [52] | cross sectional | Greece | 92 | 30.0 | To characterise airway and systemic inflammation in firefighters with a maximum occupational exposure of 1 year (trainees) compared to professional firefighters subjected to long-term exposure. |
| Greven et al. (2011) [53] | cross sectional | Netherlands | 402 | 41.3 | To determine associations between lung function, bronchial hyperresponsiveness and atopy with exposure to fire smoke among firefighters. |
| Greven et al. (2011) [54] | cross-shift | Netherlands | 43 | 39.1 | To determine associations between acute respiratory inflammatory responses, changes in bronchial hyperresponsiveness, serum pneumoprotein levels and exposure to fire. |
| Gu et al. (1996) [55] | cross sectional | Taipei | 149 | NA | To evaluate the health hazards of firefighters after fighting a fire which lasted for 40 h. |
| Hnizdo et al. (2011) [56] | cross sectional | USA | 2043 | 39.2 | To evaluate the impact of the intervention on the accuracy and precision of the lung function measurements and their estimated rate of decline. |
| Large et al. (1990) [57] | cross sectional | USA | 60 | 42.0 | To evaluate whether firefighters experience a significant change in spirometric values following exposure to smoke from a fire. |
| Miedinger et al. (2007) [58] | cross sectional | Switzerland | 101 | 41.0 | To assess professional firefighters’ respiratory health. |
| Mustajbegovic et al. (2001) [59] | cross sectional | Croatia | 128 | 37.0 | To determine the prevalence of chronic nonspecific respiratory diseases and of lung function abnormalities in firefighters. |
| Shermer et al. (2010) [60] | cross sectional | Australia | 488 | 43.8 | To establish if the use of impulse oscillometry reveals respiratory abnormalities in metropolitan firefighters that were not disclosed during routine screening with spirometry. |
| Schermer et al. (2014) [61] | cross sectional | Australia | 570 | 46.63 | To assess the prevalence of chronic respiratory conditions in metropolitan firefighters and to study associations between occupational exposure and use of respiratory protection devices with respect to health-related quality of life in firefighters with and without chronic respiratory conditions |
| Slattery et al. (2017) [62] | cross sectional | USA | 212 | 46.4 | To assess the validity of using the Global Lung Function Initiative’s (GLI) 2012 equations to interpret lung function data in a healthy workforce. |
| Pooled Random Effect Sizes | ||||||
|---|---|---|---|---|---|---|
| Predicted FEV1 (%) | Predicted FVC (%) | |||||
| N (Studies) | Pooled Mean (95% CI) | Subgroup, p-Value | N (Studies) | Pooled Mean (95% CI) | Subgroup, p-Value | |
| Total | 24 | 99.23 (94.65; 103.80) | - | 23 | 103.08 (99.83; 106.32) | - |
| Subgroup | ||||||
| Publication year | ||||||
| Before 1996 | 4 | 95.29 (90.11; 100.47) | 0.07 | 4 | 98.10 (91.83; 104.37) | 0.01 |
| 1997–2006 | 3 | 96.40 (94.60; 98.20) | 3 | 99.85 (94.29; 101.40) | ||
| 2007–2013 | 8 | 96.82 (89.82; 104.03) | 8 | 103.74 (101.23; 106.25) | ||
| After 2014 | 9 | 103.34 (98.41; 108.28) | 9 | 106.81 (100.03; 113.59) | ||
| Location | ||||||
| Europe | 11 | 98.11 (91.81; 104.40) | 0.01 | 11 | 102.65 (98.92; 106.39) | 0.63 |
| North America | 10 | 99.18 (96.47; 95.08) | 10 | 101.60 (97.46; 105.74) | ||
| Asia | 1 | 93.20 (91.32; 95.08) | 1 | 103.90 (101.78; 106.02) | ||
| Australia | 2 | 105.19 (91.29; 119.08) | 2 | 111.10 (92.28; 129.91) | ||
| Age (years old) | ||||||
| 20–30 | 7 | 97.33 (90.76; 103.90) | 0.49 | 7 | 100.24 (96.11; 104.38) | 0.39 |
| 31–40 | 8 | 98.04 (90.30; 105.77) | 8 | 103.51 (100.89; 106.13) | ||
| More than 40 | 8 | 101.95 (96.92; 106.97) | 8 | 104.12 (100.89; 106.13) | ||
| Smokers | ||||||
| Non-smokers | 12 | 101.28 (97.59; 104.96) | 0.23 | 12 | 104.07 (99.09; 109.05) | 0.47 |
| Smokers | 11 | 97.03 (91.09; 102.98) | 15 | 101.67 (97.73; 105.94) | ||
| Fire type | ||||||
| Wildland | 9 | 97.64 (91.45; 103.82) | 0.55 | 9 | 102.34 (98.29; 106.39) | 0.74 |
| Others/Urban | 15 | 99.71 (96.75; 102.67) | 15 | 103.30 (99.45; 107.15) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbosa, J.V.; Farraia, M.; Branco, P.T.B.S.; Alvim-Ferraz, M.C.M.; Martins, F.G.; Annesi-Maesano, I.; Sousa, S.I.V. The Effect of Fire Smoke Exposure on Firefighters’ Lung Function: A Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 16799. https://doi.org/10.3390/ijerph192416799
Barbosa JV, Farraia M, Branco PTBS, Alvim-Ferraz MCM, Martins FG, Annesi-Maesano I, Sousa SIV. The Effect of Fire Smoke Exposure on Firefighters’ Lung Function: A Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(24):16799. https://doi.org/10.3390/ijerph192416799
Chicago/Turabian StyleBarbosa, Joana V., Mariana Farraia, Pedro T. B. S. Branco, Maria Conceição M. Alvim-Ferraz, Fernando G. Martins, Isabella Annesi-Maesano, and Sofia I. V. Sousa. 2022. "The Effect of Fire Smoke Exposure on Firefighters’ Lung Function: A Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 24: 16799. https://doi.org/10.3390/ijerph192416799
APA StyleBarbosa, J. V., Farraia, M., Branco, P. T. B. S., Alvim-Ferraz, M. C. M., Martins, F. G., Annesi-Maesano, I., & Sousa, S. I. V. (2022). The Effect of Fire Smoke Exposure on Firefighters’ Lung Function: A Meta-Analysis. International Journal of Environmental Research and Public Health, 19(24), 16799. https://doi.org/10.3390/ijerph192416799









