Feasibility of Remote Delivering an Exercise and Lifestyle Education Program for Individuals Living with Prediabetes and Diabetes in Brazil
Abstract
1. Introduction
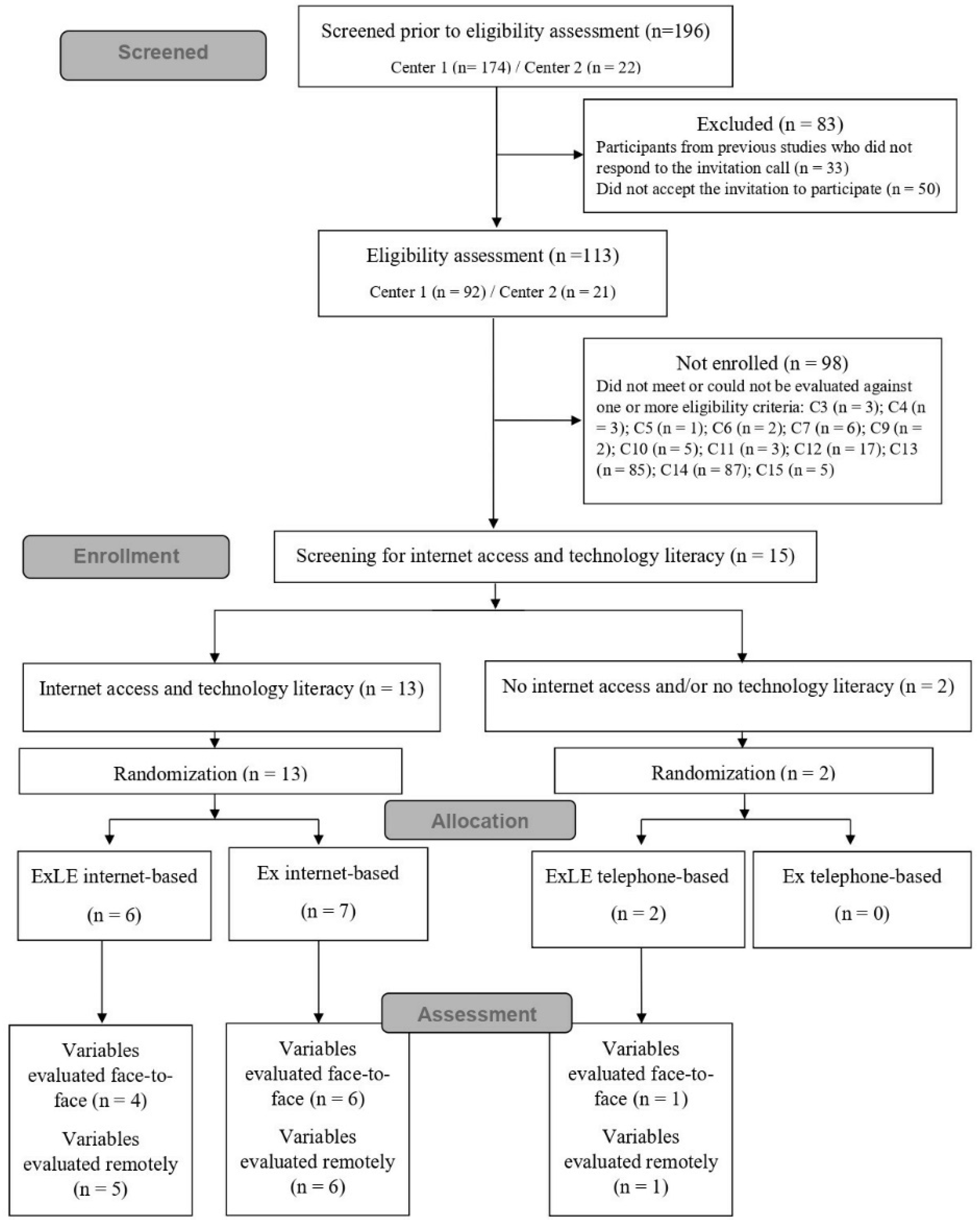
2. Materials and Methods
2.1. Study Design and Ethical Aspects
2.2. Participants
2.3. Procedures
2.4. Study Variables’ Measurement
2.5. Interventions
2.6. Feasibility Outcomes
2.7. Statistical Analysis
3. Results
3.1. Acceptability
Satisfaction with the Interventions
3.2. Implementation
3.2.1. Rate of Obtaining the Measures Used to Assess Study Variables
3.2.2. Delivery Rate of the Filled Exercise and Study Diaries
3.2.3. Total Attempts and Answer Rate to the Phone Calls or Text Messages in the Weekly Follow-Up
3.2.4. Questions Asked by Participants during the Weekly Follow-Up
3.2.5. Reported utilization rate of educational materials
3.2.6. Website Visits and Barriers to Website Navigation
3.3. Practicality
Adherence Rate to Study Interventions
3.4. Limited Efficacy
3.4.1. Intervention Preliminary Effects on Study Variables
3.4.2. Adverse Effects of Exercise Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Federation. IDF Diabetes Atlas 2021, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Sociedade Brasileira de Diabetes. Diretrizes Da Sociedade Brasileira de Diabetes 2019–2020; Sociedade Brasileira de Diabetes: São Paulo, Brazil, 2019; ISBN 9788593746024. [Google Scholar]
- Kuziemski, K.; Słomiński, W.; Jassem, E. Impact of Diabetes Mellitus on Functional Exercise Capacity and Pulmonary Functions in Patients with Diabetes and Healthy Persons. BMC Endocr. Disord. 2019, 19, 2. [Google Scholar] [CrossRef] [PubMed]
- Baktir, M.A.; Ceran, Y.; Myers, J. Exercise Capacity and Mortality in Veterans with and without Type-2 Diabetes: An Analysis Using Propensity Matching. Acta Endocrinol. 2017, 13, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Peterson, P.N.; Magid, D.J.; Ross, C.; Ho, P.M.; Rumsfeld, J.S.; Lauer, M.S.; Lyons, E.E.; Smith, S.S.; Masoudi, F.A. Association of Exercise Capacity on Treadmill with Future Cardiac Events in Patients Referred for Exercise Testing. Arch. Intern. Med. 2008, 168, 174–179. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45 (Suppl. S1), S60–S80. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.; Fischl, A.H.; Beck, J.; Browning, L.; Carter, A.; Condon, J.E.; Dennison, M.; Francis, T.; Hughes, P.J.; Jaime, S.; et al. 2022 National Standards for Diabetes Self-Management Education and Support. Sci. Diabetes Self-Manag. Care 2022, 48, 44–59. [Google Scholar] [CrossRef] [PubMed]
- Powers, M.A.; Bardsley, J.K.; Cypress, M.; Funnell, M.M.; Harms, D.; Hess-Fischl, A.; Hooks, B.; Isaacs, D.; Mandel, E.D.; Maryniuk, M.D.; et al. Diabetes Self-Management Education and Support in Adults With Type 2 Diabetes: A Consensus Report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care 2020, 43, 1636–1649. [Google Scholar] [CrossRef]
- Odgers-Jewell, K.; Ball, L.E.; Kelly, J.T.; Isenring, E.A.; Reidlinger, D.P.; Thomas, R. Effectiveness of Group-Based Self-Management Education for Individuals with Type 2 Diabetes: A Systematic Review with Meta-Analyses and Meta-Regression. Diabet. Med. 2017, 34, 1027–1039. [Google Scholar] [CrossRef]
- Chrvala, C.A.; Sherr, D.; Lipman, R.D. Diabetes Self-Management Education for Adults with Type 2 Diabetes Mellitus: A Systematic Review of the Effect on Glycemic Control. Patient Educ. Couns. 2016, 99, 926–943. [Google Scholar] [CrossRef]
- Batalha, A.P.D.B.; Ponciano, I.C.; Chaves, G.; Felício, D.C.; Britto, R.R.; da Silva, L.P. Behavior Change Interventions in Patients with Type 2 Diabetes: A Systematic Review of the Effects on Self-Management and A1c. J. Diabetes Metab. Disord. 2021, 20, 1815–1836. [Google Scholar] [CrossRef]
- Ellis, S.E.; Speroff, T.; Dittus, R.S.; Brown, A.; Pichert, J.W.; Elasy, T.A. Diabetes Patient Education: A Meta-Analysis and Meta-Regression. Patient Educ. Couns. 2004, 52, 97–105. [Google Scholar] [CrossRef]
- Sigurdardottir, A.K.; Jonsdottir, H.; Benediktsson, R. Outcomes of Educational Interventions in Type 2 Diabetes: WEKA Data-Mining Analysis. Patient Educ. Couns. 2007, 67, 21–31. [Google Scholar] [CrossRef]
- Teljeur, C.; Moran, P.S.; Walshe, S.; Smith, S.M.; Cianci, F.; Murphy, L.; Harrington, P.; Ryan, M. Economic Evaluation of Chronic Disease Self-Management for People with Diabetes: A Systematic Review. Diabet. Med. 2017, 34, 1040–1049. [Google Scholar] [CrossRef]
- Hunt, C.W. Technology and Diabetes Self-Management: An Integrative Review. World J. Diabetes 2015, 6, 225. [Google Scholar] [CrossRef]
- Vanzella, L.M.; Oh, P.; Pakosh, M.; Ghisi, G.L.d.M. Barriers and Facilitators to Virtual Education in Cardiac Rehabilitation: A Systematic Review of Qualitative Studies. Eur. J. Cardiovasc. Nurs. 2022, 21, 414–429. [Google Scholar] [CrossRef]
- Greenwood, D.A.; Gee, P.M.; Fatkin, K.J.; Peeples, M. A Systematic Review of Reviews Evaluating Technology-Enabled Diabetes Self-Management Education and Support. J. Diabetes Sci. Technol. 2017, 11, 1015–1027. [Google Scholar] [CrossRef]
- Noh, J.H.; Cho, Y.J.; Nam, H.W.; Kim, J.H.; Kim, D.J.; Yoo, H.S.; Kwon, Y.W.; Woo, M.H.; Cho, J.W.; Hong, M.H.; et al. Web-Based Comprehensive Information System for Self-Management of Diabetes Mellitus. Diabetes Technol. Ther. 2010, 12, 333–337. [Google Scholar] [CrossRef]
- Sepah, S.C.; Jiang, L.; Peters, A.L. Long-Term Outcomes of a Web-Based Diabetes Prevention Program: 2-Year Results of a Single-Arm Longitudinal Study. J. Med. Internet Res. 2015, 17, e92. [Google Scholar] [CrossRef]
- Pereira, K.; Phillips, B.; Johnson, C.; Vorderstrasse, A. Internet Delivered Diabetes Self-Management Education: A Review. Diabetes Technol. Ther. 2015, 17, 55–63. [Google Scholar] [CrossRef]
- Dening, J.; Islam, S.M.S.; George, E.; Maddison, R. Web-Based Interventions for Dietary Behavior in Adults With Type 2 Diabetes: Systematic Review of Randomized Controlled Trials. J. Med. Internet Res. 2020, 22, e16437. [Google Scholar] [CrossRef]
- Liang, X.; Wang, Q.; Yang, X.; Cao, J.; Chen, J.; Mo, X.; Huang, J.; Wang, L.; Gu, D. Effect of Mobile Phone Intervention for Diabetes on Glycaemic Control: A Meta-Analysis. Diabet. Med. 2011, 28, 455–463. [Google Scholar] [CrossRef]
- Ghisi, G.L.M.; Seixas, M.B.; Pereira, D.S.; Cisneros, L.L.; Ezequiel, D.G.A.; Aultman, C.; Sandison, N.; Oh, P.; Silva, L.P. Patient Education Program for Brazilians Living with Diabetes and Prediabetes: Findings from a Development Study. BMC Public Health 2021, 21, 1236. [Google Scholar] [CrossRef]
- Seixas, M.B.; Pereira, D.A.G.; Ghisi, G.L.M.; Batalha, A.P.D.B.; Santos, C.V.O.; Ponciano, I.C.; Oh, P.; Silva, L.P. Exercise and Lifestyle Education program for Brazilians living with prediabetes and diabetes: A pilot randomized trial. Diabetes Metab. Syndr. Clin. Res. Rev. 2022, 12, 102614. [Google Scholar] [CrossRef]
- Eldridge, S.; Chan, C.; Campbell, M.; Bond, C.; Hopewell, S.; Thabane, L.; Lancaster, G. PAFS consensus group CONSORT 2010 Statement: Extension to Randomised Pilot and Feasibility Trials. BMJ 2016, 355, i5239. [Google Scholar] [CrossRef]
- Felix, C.M.d.M.; Ghisi, G.L.d.M.; Seixas, M.B.; Batalha, A.P.D.B.; Ezequiel, D.G.A.; Trevizan, P.F.; Pereira, D.A.G.; da Silva, L.P. Translation, Cross-Cultural Adaptation, and Psychometric Properties of the Brazilian Portuguese Version of the DiAbeTes Education Questionnaire (DATE-Q). Braz. J. Phys. Ther. 2021, 25, 583–592. [Google Scholar] [CrossRef]
- Machado, C.C.d.S.; Malaguti, C.; Trevizan, P.F.; Ezequiel, D.G.A.; Seixas, M.B.; da Silva, L.P. Psychometric Validation of the Brazilian Portuguese Version of Bandura’s Exercise Self-Efficacy Scale in Diabetes Patients. J. Diabetes Metab. Disord. 2020, 19, 925–932. [Google Scholar] [CrossRef]
- Teixeira, R.L.; Jansen, A.K.; Pereira, D.A.; de M Ghisi, G.L.; da Silva, L.P.; Cisneros, L.d.L.; Britto, R.R. Brazilian Portuguese Version of the Mediterranean Diet Scale: Translation Procedures and Measurement Properties. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 102165. [Google Scholar] [CrossRef]
- Callahan, C.M.; Unverzagt, F.W.; Hui, S.L.; Perkins, A.J.; Hendrie, H.C. Six-Item Screener to Identify Cognitive Impairment among Potential Subjects for Clinical Research. Med. Care 2002, 40, 771–781. [Google Scholar] [CrossRef]
- Netto, A.P.; Andriolo, A.; Fraige Filho, F.; Tambascia, M.; Gomes, M.B.; Melo, M.; Sumita, N.M.; Lyra, R.; Cavalcanti, S. Atualização Sobre Hemoglobina Glicada (A1C) Para Avaliação Do Controle Glicêmico e Para o Diagnóstico Do Diabetes: Aspectos Clínicos e Laboratoriais. J. Bras. Patol. Med. Lab. 2009, 45, 31–48. [Google Scholar] [CrossRef]
- Conard, S. Best Practices in Digital Health Literacy. Int. J. Cardiol. 2019, 292, 277–279. [Google Scholar] [CrossRef]
- Singh, S.J.; Morgan, M.D.; Scott, S.; Walters, D.; Hardman, A.E. Development of a Shuttle Walking Test of Disability in Patients with Chronic Airways Obstruction. Thorax 1992, 47, 1019–1024. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Williams, J.E.; Reis, J.P.; Pluto, D. Utility of Pedometers for Assessing Physical Activity. Sport. Med. 2004, 34, 281–291. [Google Scholar] [CrossRef]
- Rodrigues, R.; De Andrade, S.M.; González, A.D.; Birolim, M.M.; Mesas, A.E. Cross-Cultural Adaptation and Validation of the Newest Vital Sign (NVS) Health Literacy Instrument in General Population and Highly Educated Samples of Brazilian Adults. Public Health Nutr. 2017, 20, 1907–1913. [Google Scholar] [CrossRef]
- Tavares Batistoni, S.S.; Neri, A.L.; Bretas Cupertino, A.P.F. Validity of the Center for Epidemiological Studies Depression Scale among Brazilian Elderly. Rev. Saude Publica 2007, 41, 598–605. [Google Scholar] [CrossRef]
- Ciconelli, R.M.; Ferraz, M.B.; Santos, W.; Meinão, I.; Quaresma, M.R. Tradução Para a Língua Portuguesa e Validação Do Questionário Genérico de Avaliação de Qualidade de Vida SF-36 (Brasil SF-36). Rev. Bras. Reumatol. 1999, 39, 143–150. [Google Scholar]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical Bases of Perceived Exertion. Med. Sci. Sport. Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How We Design Feasibility Studies. Am. J. Prev. Med. 2009, 36, 452. [Google Scholar] [CrossRef]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef]
- Pereira, W.V.C.; Vancea, D.M.M.; Oliveira, R.d.A.; Freitas, Y.G.P.C.d.; Lamounier, D.R.N.; Zagury, R.L.; Bertoluci, M. Atividade Física e Exercício No DM1. In Diretriz Oficial da Sociedade Brasileira de Diabetes; Sociedade Brasileira de Diabetes: São Paulo, Brazil, 2022. [Google Scholar] [CrossRef]
- Silva Junior, W.S.d.; Fioretti, A.M.B.; Vancea, D.M.M.; Macedo, C.L.D.; Zagury, R.; Bertoluci, M. Atividade Física e Exercício No Pré-Diabetes e DM2. In Diretriz Oficial da Sociedade Brasileira de Diabetes; Sociedade Brasileira de Diabetes: São Paulo, Brazil, 2022. [Google Scholar] [CrossRef]
- Adu, M.D.; Malabu, U.H.; Malau-Aduli, A.E.O.; Drovandi, A.; Malau-Aduli, B.S. Efficacy and Acceptability of My Care Hub Mobile App to Support Self-Management in Australians with Type 1 or Type 2 Diabetes. Int. J. Environ. Res. Public Health 2020, 17, 2573. [Google Scholar] [CrossRef]
- Wu, X.; Guo, X.; Zhang, Z. The Efficacy of Mobile Phone Apps for Lifestyle Modification in Diabetes: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2019, 7, e12297. [Google Scholar] [CrossRef]
- Hamine, S.; Gerth-Guyette, E.; Faulx, D.; Green, B.B.; Ginsburg, A.S. Impact of MHealth Chronic Disease Management on Treatment Adherence and Patient Outcomes: A Systematic Review. J. Med. Internet Res. 2015, 17, e52. [Google Scholar] [CrossRef]
- Knowles, M.S. Andragogy: Adult Learning Theory in Perspective. Community Coll. Rev. 1978, 5, 9–20. [Google Scholar] [CrossRef]
- Loo, R. Kolb’s Learning Styles and Learning Preferences: Is There a Linkage? Educ. Psychol. 2004, 24, 99–108. [Google Scholar] [CrossRef]
- Awotidebe, T.O.; Adedoyin, R.A.; Oke, K.I.; Ativie, R.N.; Opiyo, R.; Ikujeyisi, E.O.; Ikem, R.T.; Afolabi, M.A. Relationship between Functional Capacity and Health-Related Quality of Life of Patients with Type-2 Diabetes. Diabetes Metab. Syndr. 2017, 11, 1–5. [Google Scholar] [CrossRef]
- Bruce, D.G.; Davis, W.A.; Davis, T.M.E. Longitudinal Predictors of Reduced Mobility and Physical Disability in Patients With Type 2 Diabetes: The Fremantle Diabetes Study. Diabetes Care 2005, 28, 2441–2447. [Google Scholar] [CrossRef][Green Version]
| Feasibility Outcomes | Data Source | Data Analysis | |
|---|---|---|---|
| Acceptability |
| The satisfaction questionnaire answered by the participant in the face-to-face stage of post-intervention assessment | Descriptive statistics of numerical data and qualitative analysis of open questions of the satisfaction questionnaire |
| Implementation |
| Research files: assessment sheetsResearch files: exercise and study diaries Research files: spreadsheet used to report weekly follow-ups carried out by the research team Specific questions from the satisfaction questionnaire answered by the participant in the face-to-face stage of post-intervention assessment and study diary reports Data recorded on the website platform | Descriptive statistics of numerical data and qualitative analysis of the questions asked by the participants during the weekly follow-up and of the open questions of the satisfaction questionnaire |
| Practicality |
| Research files: exercise and study diaries | Descriptive statistics of numerical data |
| Limited Efficacy |
| Research files: data obtained from pre- and post-intervention assessments sheets and exercise diary | Descriptive statistics of numerical data |
| Variables | ExLE Internet-Based (n = 6) | ExLE Telephone-Based (n = 2) | Ex Internet-Based (n = 7) | Total Sample (n = 15) |
|---|---|---|---|---|
| Sociodemographic Characteristics | ||||
| Age (years) | 50.2 ± 11.3 | 70.5 ± 6.4 | 43.0 ± 14.9 | 49.5 ± 15.1 |
| Female—% (n) | 50.0 (3) | 100.0 (2) | 85.7 (6) | 73.3 (11) |
| Years of study | 16.7 ± 3.7 | 4.5 ± 0.7 | 16.7 ± 6.7 | 15.1 ± 6.5 |
| Household income (USD) | 2295.0 ± 2076.2 1735.8 (742.5–4050.1) | 771.4 ± 0 771.4 (771.4–771.4) | 2093.9 ± 1143.3 2507.2 (964.3–2893.0) | 1998.0 ± 1535.3 1542.9 (771.4–2893.0) |
| Work status—% (n) | ||||
| Retired | 16.7 (1) | 100.0 (2) | 14.3 (1) | 26.7 (4) |
| Employed | 83.3 (5) | 0 (0) | 57.1 (4) | 60.0 (9) |
| Student | 0 (0) | 0 (0) | 28.6 (2) | 13.3 (2) |
| Marital status—% (n) | ||||
| Single | 16.7 (1) | 0 (0) | 14.3 (1) | 13.3 (2) |
| Married | 83.3 (5) | 50.0 (1) | 71.4 (5) | 73.3 (11) |
| Widow | 0 (0) | 0 (0) | 14.3 (1) | 6.7 (1) |
| Divorced | 0 (0) | 50.0 (1) | 0 (0) | 6.7 (1) |
| Clinical Characteristics | ||||
| Diabetes type—% (n) | ||||
| Type 1 | 16.7 (1) | - | 0 (0) | 6.7 (1) |
| Type 2 | 33.3 (2) | 100.0 (2) | 57.1(4) | 53.3 (8) |
| Prediabetes | 50.0 (3) | - | 42.9 (3) | 40.0 (6) |
| Time elapsed since diagnosis (years) | 7.9 ± 8.8 | 3.2 ± 3.9 | 2.3 ± 2.4 | 2.0 (0.1–23.6) |
| Oral antidiabetics—% Yes (n) | 66.7 (4) | 100.0 (2) | 85.7 (6) | 80.0 (12) |
| Insulin therapy—% Yes (n) | 16.7 (1) | 0 (0) | 0 (0) | 6.7 (1) |
| Diabetes complications self-reported—% Yes (n) | 0 (0) | 50.0 (1) | 0 (0) | 6.7 (1) |
| Regular exercise self-reported—% Yes (n) | 50.0 (3) | 0 (0) | 28.6 (2) | 33.3 (5) |
| Smoking—% Yes (n) | 16.7 (1) | 0 (0) | 0 (0) | 6.7 (1) |
| Hypertension—% Yes (n) | 33.3 (2) | 100.0 (2) | 14.3 (1) | 33.3 (5) |
| Stress—% Yes (n) | 16.7 (1) | 100.0 (2) | 42.9 (3) | 40.0 (6) |
| Dyslipidemia—% Yes (n) | 66.7 (4) | 50.0 (1) | 57.1 (4) | 60.0 (9) |
| Healthcare service—% (n) | ||||
| Public | 16.7 (1) | 0 (0) | 28.6 (2) | 20.0 (3) |
| Private | 66.7 (4) | 50.0 (1) | 57.1 (4) | 60.0 (9) |
| Not reported | 16.7 (1) | 50.0 (1) | 14.3 (1) | 20.0 (3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seixas, M.B.; Ghisi, G.L.d.M.; Oh, P.; Pereira, D.S.; Moreira, A.P.B.; Jansen, A.K.; Batalha, A.P.D.B.; Cândido, G.d.N.; Almeida, J.A.d.; Pereira, D.A.G.; et al. Feasibility of Remote Delivering an Exercise and Lifestyle Education Program for Individuals Living with Prediabetes and Diabetes in Brazil. Int. J. Environ. Res. Public Health 2022, 19, 16697. https://doi.org/10.3390/ijerph192416697
Seixas MB, Ghisi GLdM, Oh P, Pereira DS, Moreira APB, Jansen AK, Batalha APDB, Cândido GdN, Almeida JAd, Pereira DAG, et al. Feasibility of Remote Delivering an Exercise and Lifestyle Education Program for Individuals Living with Prediabetes and Diabetes in Brazil. International Journal of Environmental Research and Public Health. 2022; 19(24):16697. https://doi.org/10.3390/ijerph192416697
Chicago/Turabian StyleSeixas, Mariana Balbi, Gabriela Lima de Melo Ghisi, Paul Oh, Daniele Sirineu Pereira, Ana Paula Boroni Moreira, Ann Kristine Jansen, Ana Paula Delgado Bomtempo Batalha, Gabriela do Nascimento Cândido, Josiane Aparecida de Almeida, Danielle Aparecida Gomes Pereira, and et al. 2022. "Feasibility of Remote Delivering an Exercise and Lifestyle Education Program for Individuals Living with Prediabetes and Diabetes in Brazil" International Journal of Environmental Research and Public Health 19, no. 24: 16697. https://doi.org/10.3390/ijerph192416697
APA StyleSeixas, M. B., Ghisi, G. L. d. M., Oh, P., Pereira, D. S., Moreira, A. P. B., Jansen, A. K., Batalha, A. P. D. B., Cândido, G. d. N., Almeida, J. A. d., Pereira, D. A. G., & Silva, L. P. d. (2022). Feasibility of Remote Delivering an Exercise and Lifestyle Education Program for Individuals Living with Prediabetes and Diabetes in Brazil. International Journal of Environmental Research and Public Health, 19(24), 16697. https://doi.org/10.3390/ijerph192416697







