Oral Health Status, Oral Health Behaviors, and Oral Health Care Utilization among Persons with Disabilities in Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Focused Question
2.2. Eligibility Criteria and Literature Search
2.3. Data Extraction
2.4. Quality Assessment
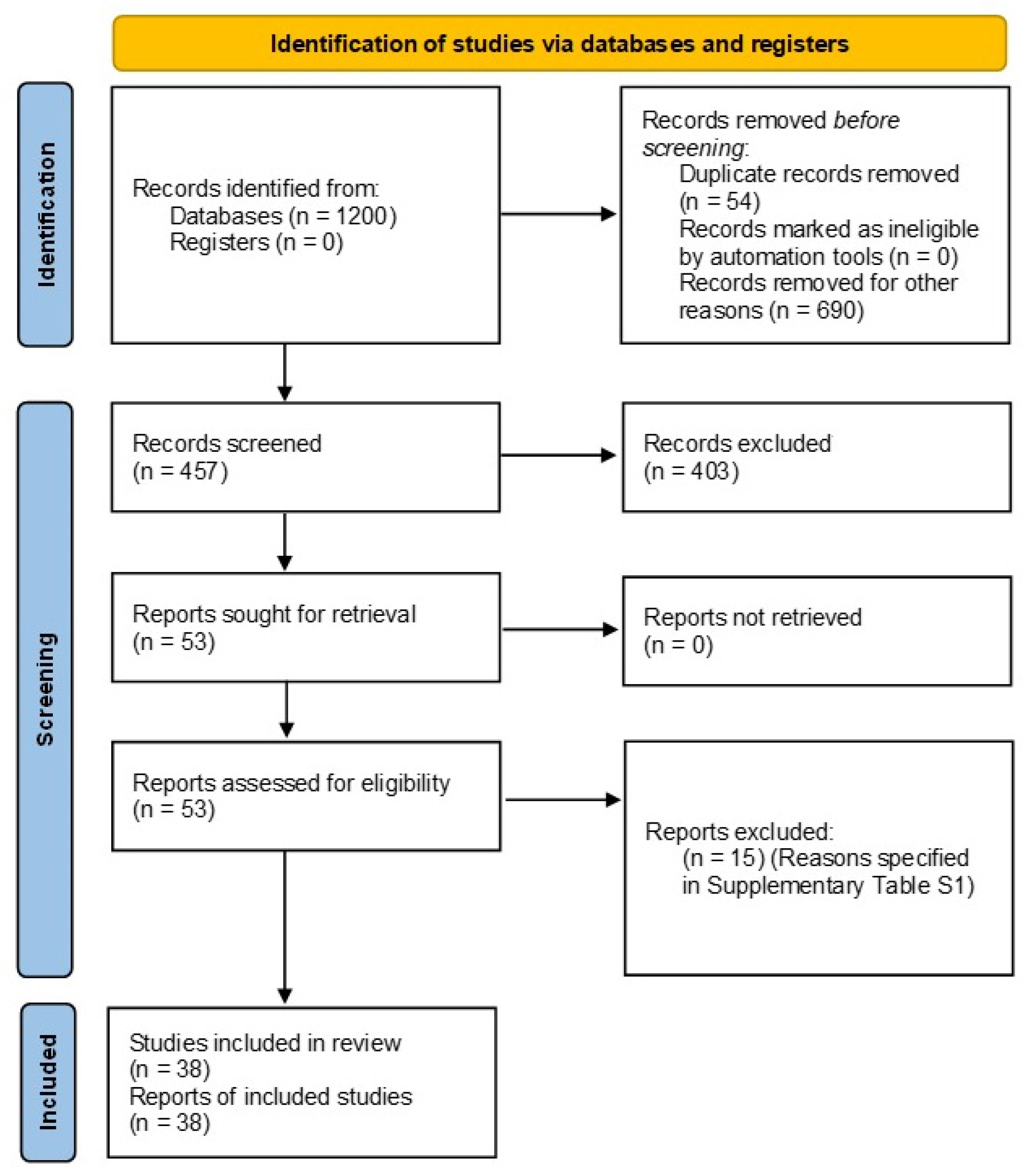
3. Results of the Literature Search
4. General Characteristics of Studies
5. Overall Outcomes of Studies
- -
- Oral health behavior:
Smoking and Substance Abuse
- -
- Oral health care attendance and barriers:
6. Results of the Quality Assessment
7. Discussion
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khayatzadeh-Mahani, A.; Wittevrongel, K.; Nicholas, D.B.; Zwicker, J.D. Prioritizing barriers and solutions to improve employment for persons with developmental disabilities. Disabil. Rehabilit. 2020, 42, 2696–2706. [Google Scholar] [CrossRef] [PubMed]
- Wilson, N.J.; Lin, Z.; Villarosa, A.; Lewis, P.; Philip, P.; Sumar, B.; George, A. Countering the poor oral health of people with intellectual and developmental disability: A scoping literature review. BMC Public Health 2019, 19, 1530. [Google Scholar] [CrossRef] [PubMed]
- Cougnard, A.; Goumilloux, R.; Monello, F.; Verdoux, H. Time between schizophrenia onset and first request for disability status in France and associated patient characteristics. Psychiatr. Serv. 2007, 58, 1427–1432. [Google Scholar] [CrossRef]
- Nations, U. Disability and Development Report. In Realizing the Sustainable Development Goals by, for and with Persons with Disabilities 2018; United Nations, Department of Economic and Social Affairs: New York, NY, USA, 2019. [Google Scholar]
- Lim, M.A.W.T.; Liberali, S.A.C.; Calache, H.; Parashos, P.; Borromeo, G.L. Perceived barriers encountered by oral health professionals in the Australian public dental system providing dental treatment to individuals with special needs. Spec. Care Dent. 2021, 41, 381–390. [Google Scholar] [CrossRef]
- Pradhan, A.; Slade, G.D.; Spencer, A.J. Access to dental care among adults with physical and intellectual disabilities: Residence factors. Aust. Dent. J. 2009, 54, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Najeeb, S.; Khurshid, Z.; Siddiqui, F.; Zohaib, S.; Zafar, M.S. Outcomes of dental implant therapy in patients with down syndrome: A systematic review. J. Evid. Based Dent. Prac. 2017, 17, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Dao, L.P.; Zwetchkenbaum, S.; Inglehart, M.R. General dentists and special needs patients: Does dental education matter? J. Dent. Educ. 2005, 69, 1107–1115. [Google Scholar] [CrossRef] [PubMed]
- General Authority for Statistics. 2.9% of Saudi Population Have Disability with (Extreme) Difficulty; General Authority for Statistics: Riyadh, Saudi Arabia, 2017. [Google Scholar]
- Alshehri, M.; Alghamdi, N.; Abdellatif, H. Assessment of oral health knowledge, status and awareness among visually impaired children in Saudi Arabia. J. Dent. Health Oral Disord. Ther. 2018, 9, 215–220. [Google Scholar]
- Al-Shehri, S.A.M. Access to dental care for persons with disabilities in Saudi Arabia (Caregivers’ perspective). J. Disabil. Oral Health 2012, 13, 51. [Google Scholar]
- Kotha, S.B.; AlFaraj, N.S.M.; Ramdan, T.H.; Alsalam, M.A.; Al Ameer, M.J.; Almuzin, Z.M. Associations between diet, dietary and oral hygiene habits with caries occurrence and severity in children with autism at Dammam City, Saudi Arabia. Open Access Maced. J. Med. Sci. 2018, 6, 1104. [Google Scholar] [CrossRef]
- Wyne, A.H. Attitude of parents of disabled children towards dental visits in Riyadh, Saudi Arabia. Odontostomatol. Trop. 2007, 30, 17–23. [Google Scholar] [PubMed]
- Alhammad, N.S.; Wyne, A.H. Caries experience and oral hygiene status of cerebral palsy children in Riyadh. Odontostomatol. Trop. 2010, 33, 5–9. [Google Scholar] [PubMed]
- Wyne, A.H.; Al-Hammad, N.S.; Splieth, C.H. Oral health comprehension in parents of Saudi cerebral palsy children. Saudi Dent. J. 2017, 29, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Al-Ansari, A.A. Prevalence, severity, and secular trends of dental caries among various Saudi populations: A literature review. Saudi J. Med. Med. Sci. 2014, 2, 142. [Google Scholar] [CrossRef]
- Idrees, M.M.; Azzeghaiby, S.N.; Hammad, M.M.; Kujan, O.B. Prevalence and severity of plaque-induced gingivitis in a Saudi adult population. Saudi Med. J. 2014, 35, 1373. [Google Scholar]
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef]
- Al-Sarheed, M.; Bedi, R.; Hunt, N.P. Orthodontic treatment need and self-perception of 11–16-year-old Saudi Arabian children with a sensory impairment attending special schools. J. Orthod. 2014, 30, 39–44. [Google Scholar] [CrossRef]
- AlSarheed, M.; Bedi, R.; Hunt, N.P. Traumatised permanent teeth in 11–16-year-old Saudi Arabian children with a sensory impairment attending special schools. Dent. Traumatol. 2003, 19, 123–125. [Google Scholar] [CrossRef]
- Al-Sarheed, M.; Bedi, R.; Hunt, N.P. The views and attitudes of parents of children with a sensory impairment towards orthodontic care. Eur. J. Orthod. 2004, 26, 87–91. [Google Scholar] [CrossRef][Green Version]
- Alkawari, H. Down Syndrome Children, Malocclusion Characteristics and the Need for Orthodontic Treatment Needs (IOTN): A Cross-Sectional Study. Children 2021, 8, 888. [Google Scholar] [CrossRef]
- Alkhadra, T. Characteristic of Malocclusion among Saudi Special Need Group Children. J. Contemp. Dent. Pract. 2017, 18, 959–963. [Google Scholar] [CrossRef]
- Al-Qahtani, Z.; Wyne, A.H. Caries experience and oral hygiene status of blind, deaf and mentally retarded female children in Riyadh, Saudi Arabia. Odontostomatol Trop. 2004, 27, 37–40. [Google Scholar] [PubMed]
- Ashour, N.A.; Ashour, A.A.; Basha, S. Association between body mass index and dental caries among special care female children in Makkah City. Ann. Saudi Med. 2018, 38, 28–35. [Google Scholar] [CrossRef]
- Murshid, E.Z. Parents’ dental knowledge and oral hygiene habits in Saudi children with autism spectrum disorder. Glob. J. Med. Res. 2014, 14, 11–18. [Google Scholar]
- Murshid, E.Z. Diet, oral hygiene practices and dental health in autistic children in Riyadh, Saudi Arabia. Oral Health Dent. Manag. 2014, 13, 91–96. [Google Scholar] [PubMed]
- Diab, H.M.; Motlaq, S.S.; Alsharare, A.; Alshammery, A.; Alshammery, N.; Khawja, S.G.; Shah, A.H. Comparison of gingival health and salivary parameters among autistic and non-autistic school children in Riyadh. J. Clin. Diagn. Res. 2016, 10, ZC110. [Google Scholar] [CrossRef]
- AlSadhan, S.A.; Al-Jobair, A.M.; Bafaqeeh, M.; Abusharifa, H.; Alagla, M. Dental and medical health status and oral health knowledge among visually impaired and sighted female schoolchildren in Riyadh: A comparative study. BMC Oral Health 2017, 17, 154. [Google Scholar] [CrossRef]
- Al-Qahtani, Y.; Al-Naser, H.; Al-Nahawi, D.; Al-Tuwaijri, F.; Al-Abdullati, M.; Al-Jewair, T. Dental caries prevalence and severity among deaf and hearing-impaired male students in Eastern Saudi Arabia. Adv. Dent. Oral Health 2017, 5, 1–6. [Google Scholar]
- Alhazmi, A.; Alshinqiti, I.; Aloufi, F.; Alhejali, A.; Alsulaimani, W.; Alharbi, M. Oral health knowledge, practice, oral hygiene status and dental caries prevalence among visually impaired student in Alnoor Institute of Almadinah Almunawwarah at Saudi Arabia. Int. J. Dent. Sci. Res. 2014, 2, 149–153. [Google Scholar] [CrossRef][Green Version]
- Wyne, A.H.; Al-Hammad, N.S.; Splieth, C.H. Dental caries and related risk factors in Saudi cerebral palsy children. Neurosci. J. 2017, 22, 282–286. [Google Scholar] [CrossRef]
- Al-Sehaibany, F.S. Occurrence of traumatic dental injuries among preschool children with Autism Spectrum Disorder. Pak. J. Med. Sci. 2018, 34, 859. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, M.; Asiri, F.Y.I.; AlGhannam, S.; AlQarni, I.A.M.; AlAteeg, M.A.; Anil, S. Extent of awareness regarding oral health and dental treatment needs among individuals with hearing and speech impairments in Saudi Arabia. J. Int. Soc. Prev. Community Dent. 2018, 8, 70. [Google Scholar] [CrossRef] [PubMed]
- Alkahtani, F.H.; Baseer, M.A.; Ingle, N.A.; Assery, M.K.; Al Sanea, J.A.; AlSaffan, A.D.; Al-Shammery, A. Oral health status, treatment needs and oral health related quality of life among hearing impaired adults in Riyadh City, Saudi Arabia. J. Contemp. Dent. Pract. 2019, 20, 744. [Google Scholar]
- Alzahrani, A.A.H. Parent perspectives on perceived dental pain and dental caries in Saudi schoolchildren with intellectual disability. Spec. Care Dent. 2019, 39, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Alaki, S.M.; Bakry, N.S. Dental pain in children with intellectual disabilities: Caregivers’ perspective. Int. J. Dent. 2012, 2012, 701608. [Google Scholar] [CrossRef][Green Version]
- Gufran, K.; Alqutaym, O.S.; Alqahtani, A.A.M.; Alqarni, A.M.; Hattan, E.A.E.; Alqahtani, R.O. Prevalence of dental caries and periodontal status among Down’s syndrome population in Riyadh City. J. Pharm. Bioallied Sci. 2019, 11, S252. [Google Scholar] [CrossRef] [PubMed]
- AlHumaid, J.; Gaffar, B.; AlYousef, Y.; Alshuraim, F.; Alhareky, M.; El Tantawi, M. Oral health of children with autism: The influence of parental attitudes and willingness in providing care. Sci. World J. 2020, 2020, 8329426. [Google Scholar] [CrossRef] [PubMed]
- Basha, S.; Mohamed, R.N.; Al-Thomali, Y.; Ashour, A.A.; Zahrani, F.S.A.; Almutair, N.E. Traumatic dental injuries in special health care needs children and association with obesity. Ann. Saudi Med. 2021, 41, 51–58. [Google Scholar] [CrossRef]
- Shah, A.; Bindayel, N.; AlOlaywi, F.; Sheehan, S.; AlQahtani, H.; AlShalwi, A. Oral health status of a group at a special needs centre in AlKharj, Saudi Arabia. J. Disabil. Oral Health 2015, 16, 79–85. [Google Scholar]
- Mohamed, R.; Basha, S.; Al-Thomali, Y.; AlZahrani, F.; Ashour, A.; Almutair, N. Association between dental caries and obesity among children with special health care needs. Oral Health Prev. Dent. 2021, 19, 101–106. [Google Scholar]
- Sandeepa, N.C.; Al Hagbani, S.A.; Alhammad, F.A.; Al Shahrani, A.S.; Al Asmari, S.E. Oral health status of Down’s syndrome patients in Aseer, Saudi Arabia. J. Pharm. Bioallied Sci. 2021, 13, S656. [Google Scholar] [CrossRef] [PubMed]
- Alfaraj, A.; Halawany, H.S.; Al-Hinai, M.T.; Al-Badr, A.H.; Alalshaikh, M.; Al-Khalifa, K.S. Barriers to Dental Care in Individuals with Special Healthcare Needs in Qatif, Saudi Arabia: A Caregiver’s Perspective. Patient Prefer. Adher. 2021, 15, 69. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.H.; Wyne, A.H.; Asiri, F.Y.; Gulzar, S.; Sheehan, S.A.; Alghmlas, A.S.; Alomari, O.; AlJameel, A.H. Effectiveness of Preventive Oral Health Measures among Special Care School Children (boys) in Al-Kharj, Saudi Arabia. J. Clin. Diagn. Res. 2020, 14, ZC36–ZC40. [Google Scholar] [CrossRef]
- Al-damri, H.; Al-humaid, R.; Al-shehri, S.; Al-otaibi, S.; Abdulwahid, A. A comparison of DMF index and oral hygiene index between Downs syndrome subjects and a control group in Riyadh. Oral Health Care 2017, 2, 1–3. [Google Scholar] [CrossRef]
- Alzughaibi, O.S.; Filimban, L.A.; Arafa, A.A. Assessment of Salivary Immunoglobulin A, α-amylase, pH and Flow-rate Effects on Dental Caries Experience of Down’s Syndrome Children in Makkah, Saudi Arabia. Int. J. Health Sci. Res. 2017, 143–149. [Google Scholar]
- Al-Otaibi, S.M.; Rizk, H.; Riyaz, M.A. Prevalence of dental caries, salivary streptococcus mutans, lactobacilli count, pH level and buffering capacity among children with down’s syndrome in al-qassim region, KSA. Int. J. Contemp. Med. Res. 2016, 3, 2793–2797. [Google Scholar]
- Brown, A. Caries prevalence and treatment needs of healthy and medically compromised children at a tertiary care institution in Saudi Arabia. East. Mediterr. Health J. 2009, 15, 378–386. [Google Scholar] [CrossRef]
- El Tantawi, M.; AlAgl, A. Disability and the impact of need for periodontal care on quality of life: A cross-sectional study. J. Int. Med. Res. 2017, 45, 1949–1960. [Google Scholar] [CrossRef]
- Alshihri, A.A.; Al-Askar, M.H.; Aldossary, M.S. Barriers to Professional Dental Care among Children with Autism Spectrum Disorder. J. Autism. Dev. Disord. 2021, 51, 2988–2994. [Google Scholar] [CrossRef]
- Carter, A.; Clarke, L.; Stevens, C. Dental health for children with special educational needs and disability. Paediatr. Child Health 2022, 32, 290–296. [Google Scholar] [CrossRef]
- Alharbi, M.F. An analysis of the Saudi health-care system’s readiness to change in the context of the Saudi National Health-care Plan in Vision 2030. Int. J. Health Sci. 2018, 12, 83. [Google Scholar]
- Chowdhury, S.; Mok, D.; Leenen, L. Transformation of health care and the new model of care in Saudi Arabia: Kingdom’s Vision 2030. J. Med. Life 2021, 14, 347. [Google Scholar] [PubMed]
- Baskaradoss, J.K.; AlSumait, A.; Behbehani, E.; Qudeimat, M.A. Association between the caregivers’ oral health literacy and the oral health of children and youth with special health care needs. PLoS ONE 2022, 17, e0263153. [Google Scholar] [CrossRef] [PubMed]
- Mac Giolla Phadraig, C.; Guerin, S.; Nunn, J. Train the trainer? A randomized controlled trial of a multi-tiered oral health education programme in community-based residential services for adults with intellectual disability. Community Dent. Oral Epidemiol. 2013, 41, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Federation, FDI World Dental. FDI/IADH policy statement on Oral health and dental care of people with disabilities: Adopted by the FDI General Assembly, September 2016, Poznan, Poland. Int. Dent. J. 2017, 67, 16–17. [Google Scholar] [CrossRef]
- Leal Rocha, L.; Vieira de Lima Saintrain, M.; Pimentel Gomes Fernandes Vieira-Meyer, A. Access to Dental Public Services by Disabled Persons. BMC Oral Health 2015, 15, 35. [Google Scholar] [CrossRef]
- Al-Jadid, M.S. Disability in Saudi Arabia. Saudi Med. J. 2013, 34, 453–460. [Google Scholar]
- Bindawas, S.M.; Vennu, V. The national and regional prevalence rates of disability, type, of disability and severity in Saudi Arabia—Analysis of 2016 demographic survey data. Int. J. Environ. Res. Public Health 2018, 15, 419. [Google Scholar] [CrossRef]
- Asma’a, A.F.; Alsalhani, A.B.; Idrees, M.M.; Alshehri, M.A.; Nassani, M.Z.; Kujan, O.B. Knowledge, attitudes, and practice behavior of dental hygienists regarding the impact of systemic diseases on oral health. Saudi Med. J. 2018, 39, 1139. [Google Scholar]
| Study (Author, Year) | Study Design and Aims | City and/or Province | Study Setting (n, Number of Centres if Provided) | Target Population (Sample Size, n) | Special Needs Included (n, if Applicable) | Ages (Range, Mean) | Gender, Female (n, %) | Responders/Subjects Included/Groups (n) | Variables Measured/Dental Indices | Main Oral Health Outcomes and/or Observations |
|---|---|---|---|---|---|---|---|---|---|---|
| AlSarheed et al., 2003 | Cross-sectional | Riyadh | schools (n = 2) | 781 | VI, HI | 11–16 years | n = 423, 54.1% | Group 1: VI (n = 77) Group 2: HI: (n = 210) Group 3: Healthy controls (n = 494) | OH status (IOTN) (DHC) index aesthetic component (AC). | A total of 21.8% of HI, 65% of VI, and 18.7% of controls needed orthodontic treatment. Patients with special needs had a higher need of orthodontic treatment (with males with VI impairment requiring the highest). |
| AlSarheed et al., 2003 | Cross-sectional | Riyadh | schools (n = 2), (1 = VI) and (1 = HI) | 781 | VI, HI | 11–16 years | n = 423, 54.1% | Group 1: VI (n = 77) Group 2: HI: (n = 210) Group 3: Healthy controls (n = 494) | OH status (TDI index). | Both HI (11.4%) and VI (9%) had higher incisor trauma rate than controls (6.7%). HI statistically higher than controls (p < 0.05). |
| AlSarheed, 2004 | Cross-sectional | Riyadh | Special needs schools vs. mainstream schools (n = not stated) | 781 parents | VI, HI | 11–16 years | n = 423 (54.1%) | Parents of 3 groups: Group 1: VI (n = 77) Group 2: HI: (n = 210) Group 3: Healthy controls (n = 494) | OH status (IOTN). | Parent attitude to children’s teeth; 77% of VI parents, 47% of HI parents, and 62.5% of control parents believed their children’s teeth were maligned. Parents attitude towards OTN of their children: 31.1% of VI parents, 23.6% of control parents and 17.9% of HI parents believed their children were concerned with their dental appearance (VI vs. HI (p < 0.05)). Parents attitude towards OH and OT: Approximately 25% of parents believed that oral hygiene would be difficult during OT (no difference between groups). Approximately 50% parents believed that OT would be difficult to commence. |
| AlKawari, 2021 | Cross-sectional | Riyadh | Special needs institutes (n not stated) | n = 23 children with DS | DS | 10–14 years | 74% | N/A | OH status
| A total of 81.9% of children with DS needed OT, with the majority having severe malocclusion. A total of 59.1% had Angle Class III malocclusion, and 36.4% had Angle Class I. |
| Alkhadra et al., 2017 | Riyadh city | Rehabilitation centers (n = 5) | 200 children (100 DS and 100 AD) | (DS) and AD | 6 to 14 years | n = 69 DS 34 AD 35 | N/A | OH status
| Malocclusion: DS: 66% (mostly Class III); cross bites, 48% AD: 3–4% (mostly class I). | |
| Qahtani and Wyne, 2004 | Cross-sectional | Riyadh | Special needs school | 219 children | VI, HI, ID | 6–7 years and 11–12 years | n = 219 (100%) | Group 1: VI (n = 12), 6–7-year-olds Group 2: HI (n = 23), 6–7-year-olds Group 3: ID (n = 32), 6–7-year-olds Group 4: VI (n = 17), 11–12-year-olds Group 5: HI, (n = 57), 11–12-year-olds Group 6: ID (n = 109) | OH status (DMT/dmft). | Aged: 6–7-year-olds VI dmft = 7.58 ± 2.02 (decay component: 6.33 ± 2.74); DMFT: 1.67 ± 1.67 (only decay component) Caries prevalence: NR HI dmft = 7.35 ± 3.82 (decay component: 7.09 ± 3.55); DMFT: 0.87 ± 1.25 (only decay component) Caries prevalence: 95.7% DI dmft = 8.00 ± 4.1 (decay component: 2.39 ± 1.64); DMFT: 3.00 ± 2.11 (2.39 ± 1.64) Caries prevalence: 93.9% 11–12-year-olds VI dmft = 1.00 ± 1.9 (only decay component); DMFT = 3.80 ± 2.67 (decay component: 3.76 ± 2.66) Caries prevalence: 88.2% HI dmft = 2.11 ± 2.53 (decay component: 1.9 ± 2.37); DMFT: 5.12 ± 3.45 (decay component: 4.79 ± 3.14) Caries prevalence: 93% DI dmft: 3.2 ± 3.18 (decay component: 3.16 ± 3.05); DMFT: 5.81 ± 2.95 (decay component: 5.16 ± 2.62) Caries prevalence: NR Children with DI had the worst oral hygiene. |
| Wyne, 2007 | Survey | Riyadh | centre (n = 7) | 315 parents | DS (n = 117), CP (n = 106), ID (n = 54), Others (n = 38) | 36.3 years (parents); 7.7 years (children) | n = 245 (88.2%) mothers; 39% female children | <5 years 6–10 years >11 years | OH care utilization. Dental visits and barriers. | Only 17.1% of children had visited the dentists by age 7. A total of 26.3% of children had never visited a dentist before. The reasons for not visiting a dentist: A total of 43.4% was due to child’s behavior difficulties. A total of 30.1% was because parents are too busy in the medical care of their child. A total of 26.5% was due to the inaccessibility of dental services for children with disabilities. A total of 73.7% had already visited a dentist for 22.0%, their last visit was due to pain in teeth, for 32.7% it was for a follow-up appointment, and for 45.3% their last dental visit was their first ever dental check-up. Parents with a higher education level had a more positive attitude towards dental visits than those with a lower education level (p < 0.05). |
| Sharifa and Al-Shehri, 2012 | Survey | Riyadh and Al-Hfouf | Centres | 119 caregivers | Autism (n = 2), DS (n = 22), ID (n = 45), LD (n = 41), Others (n = 9) | Between 16 and 60 years | Caregiver 63% disabled 75.2% | 1–10 years 11–15 years 16–20 years >21 | OH behavior (tooth brushing). OH care utilization (dental visits/barriers). | A total of 41.2% could not brush independently. A total of 32.8% could not brush their teeth at all. A total of 51.3% had not visited the dentist in the last year. A strong association was found between caregivers’ level of education and tooth brushing (p = 0.046). Barriers: Fear of the dentist (52.1%). Cost (48.7%). Unable to sit in dental chair (28.2%). Transportation (26.9%). Distance (18.5%). Skills of dentists (16.8%). A total of 54.6% required dental treatment, while 30% did not need treatment; 46.2% of individuals with disabilities had difficulty in getting dental care in their community. |
| Ashour et al., 2018 | Analytical cross-sectional study | Makkah | Schools | 272 Females | ID (n = 79) AD (n = 41) CP (n = 17) DS (n = 52) DB (n = 61) others (n = 25) | Age group: 6–11 years, 12–17 years | 272 Females | Age group: 6–11 years, 12–17 years | OH status (dmft/DMFT). OH behavior (sugar consumption, toothbrushing, and fluoridated toothpaste). | The overall prevalence of caries was 56.7% and the mean caries score (dmft = 3.9, DMFT = 3.2) for the entire study population was high. The caries prevalence was high among intellectually disabled children (77.2%), autistic children (65.8%), and Down syndrome children (61.5%). Regression analysis showed a strong association between intellectually disabled children (adjusted OR = 2.2), autistic children (adjusted OR = 1.2), Down syndrome children (adjusted OR = 1.2), and caries prevalence. A total of 21% of the children were overweight and 21.8% were obese. Mean BMI was 20.2 (2.8). When adjusted for covariates, the logistic regression model showed strong association between caries and obesity (adjusted odds ratio = 2.9; 95% CI = 1.2–4.9). Sugar consumption: 203 answered YES. Tooth brushing frequency (64) ≥ 2 times/day. Fluoridated toothpaste: n = 148 answered YES. Children who consume sugar have a 1.9 times greater risk of developing caries. Children brushing their teeth ≥1 per day had a 2.7 times greater risk of dental caries. |
| Murshid 2014 | Cross-sectional | Riyadh | Centers (n = 3) | 450 parents of children with ASD | ASD | 3–14 years | 24.1% | n = 344 parents of children with ASD | OH behavior (tooth brushing). OH care Utilization (dental visits). | Majority (61.3%) of children are not able to brush teeth themselves. Only 29.1% of children brushed twice a day. Time of first dental visit only in an emergency was 28.2%, necessary only at signs of pain or dental problems. Only 2% of parents thought it should be during the 1st year after the child’s birth. |
| Murshid 2014 | Cross-sectional study | Riyadh | Special needs centers (n = 3) | 450 parents of children with ASD | ASD | 3–14 years | 24.1% | n = 344 parents of children with ASD | OH behavior (sugary food consumption, soft drink consumption, and tooth brushing).OH care utilization(dental visits and type of dental treatment that had been utilized). | A total of 70.9% preferred food that is high in sugar. A total of 96.7% consumed soft drinks regularly. A total of 34.0% brushed their teeth once a day, while 29.0% brushed twice a day, and 28.8% brushed on an irregular basis. Dental visit: A total of 51.5% had no previous dental visits or dental treatment. A total of 10.1% were using nitrous oxide. About 25% received treatment under general anesthesia. A total of 48.5% used different behavioral management techniques for dental treatment. A total of 48.5% of the children had dental problems treated. |
| Diab et al., 2016 | Retrospective | Riyadh | Special needs school | 50 children | ASD | 8.5 years (4–15 years) | n = 26 | n = 50 children with ASD n = 50 children without ASD | OH status (GI, PI, salivary pH, and salivary buffering capacity). | Children with ASD have higher gingival inflammation (p < 0.005), poor oral hygiene (p < 0.005), and lower salivary pH (p < 0.05), when compared to children without ASD. |
| AlSadhan et al., 2017 | Cross-sectional | Riyadh | VI school vs. Mainstream school | n = 162 children | VI | 9.81 years (6–12 years) | n = 162 (100%) | n = 79 children with VI n = 83 children without VI | OH status (DMFT/DMFS)/(dmft/dmfs) (OHI) (PI) (GI). OH behavior (tooth brushing). OH care Utilization (dental visits). | Children with VI had poorer DMFS (p < 0.05), lower OHI (p < 0.001), and poorer systemic health (p < 0.005). Tooth brushing: Only 78.5% of the VI children and 90.4% of children without VI; the difference was statistically significant (p = 0.043). A total of 71% of the children without VI had been to the dentist, compared with 54.5% of the VI children (p = 0.028). |
| Al-Qahtani et al., 2017 | Cross-sectional | Eastern Province, cities of: Khobar, Dammam, and Qatif. | Schools (n = 7). | n = 327 | Deaf, HI | NR | 0% | n = 109 children with HI n = 218 children without HI | Oral H status (Dental caries) (DMFT/DMFS). Oral H behavior (brushing, flossing). Oral H care utilization (dental visits). | More than 97% of the deaf and 81.8% of the HI in the 12–14 age group had decay, compared to 64.9% in the controls (p = 0.009). The differences between the children with HI and children without HI were statistically significant (Tukey’s test, p = 0.005). More severe forms of caries were common in the deaf children (34.9%) than in the children with HI (30.4) and children without HI (16.8%). The overall mean DMF/S for all children was 10.03, greater than the finding in Indian and Kuwaiti adults with special needs. The 12–14-year-old group was statistically significant for the “D” component and the “DMF/S” (p = 0.005) and (p = 0.003), respectively. The difference was also significant for the “F” component for the same disability and age groups (p-value of 0.003). The DMF/S score (prevalence of dental caries) increased with age in all the groups. A total of 10% do not brush, and 88% do not floss. Around 40% of the deaf students reported never visiting a dentist before. |
| Alhazmi, et al., 2014 | Al Madinah | n = 80 children | VI | 7–24 years | (29 female) | 64 children | OH status (dmft or DMFT). ➢ Plaque and calculus index.OH behavior (brushing, flossing). | Caries prevalence of the VI children is 95.16%, which is very high. Low DMFT/dmft 0.24/0.59 and more than 2/3 have equal or greater than 1–2 soft debris accumulation. There is no significant difference between the mean of DMFT/dmft for both male and female genders and the mean of plaque index. A total of 85.9% brush their teeth (43.1% brush their teeth twice per day). Independent in brushing: A total of 62% brush teeth without any help. Dental floss: 10.9% used it, and 89% never used it before. | ||
| Wyne et al., 2017 | Cross-sectional | Riyadh | Special needs school (n = 2) | n = 52 children | CP | 6.3 years (3–10 years) | 38.5% | n = 52 children with CP | OH status (DMFT + dmft). | A total of 98.1% of children with CP had dental caries (DMFT + dmft: 9.98 ± 3.99). |
| Al-Sehaibany 2018 | Cross-sectional | Riyadh | Special needs schools (n = 3) vs. mainstream schools (n = 3) | n = 514 children | AD | 4.15 years | F to M ratio: 1:2.3 | n = 257 children with ASD n = 257 children without ASD | OH status clinical examination TDIs. | Prevalence of TDIs in children with ASD (25.7%) is significantly higher than without ASD (16.3%) (p < 0.05). |
| Kotha et al., 2018 | Cross-sectional/survey | Dammam | Special needs schools (n = 3) | NR | AD | 5.8 years | NR | Children with ASD (n not stated) | OH status (dmfts). OH behavior (tooth brushing, sugar, and soft drinks consumption). OH care utilization (dental visits). | Frequency of sugar intake between meals increased dental caries occurrence.
|
| Mustafa et al., 2018 | Cross-sectional/analytical survey | AlKharj, Riyadh, Dammam, Abha | Special needs schools and institutes (n not stated) | n = 240 children and adults | HI, SI | 15–30 years | NR | N/A | OH behavior (brushing, flossing). OH care utilization (dental visits). | A total of 69% were not aware of the right way of brushing. Majority did not use dental floss. Lack of awareness of OH and dental treatment among individuals with HI and SI. −A total of 72% of the participants had never visited a dentist before. |
| AlKahtani et al., 2019 | Cross-sectional | Riyadh | Teaching dental institute (n = 1) | n = 146 | HI | 18–21 years | 105 (71.9%) | N/A | OH status (DMFT) (GI) (PI) simplified (OHI-S). OH behavior (tooth brushing). OH, care utilization (dental visits). | High dental caries experience and need for dental treatment in the majority of adults with HI. Oral hygiene was fair. n = 55 (37.7%) brushed their teeth twice daily. n = 68 (46.6%) visited dentist in the last 6 months. A total of 40 (55.6%) of 18–21 years, 19 (26.4%) 22–25 years, and 13 (18.1%) in >25 years were in need of preventive caries with statistically significant differences (p = 0.036). |
| AlZahrani et al., 2019 | Cross-sectional (mixed methods) | Albaha province | Special needs school (n = 1) | n = 92 children (only male); oral control (n = 46); ILD (n = 46) | ID | 12–16 years | 0 | ID = 92 oral control (n = 46) ILD (n = 46) | OH status DMFT. | High prevalence of dental caries, dental pain, and poor oral health in majority of children with ID. |
| Alaki and Bakry 2012 | Cross-sectional (mixed methods) | (Jeddah) | Children visiting the hospital dental clinics at King Abdelaziz University (KAU), | 86 children | ID | Age: 12–16 years | ID = 33 Without ID = 53 | OH status (DFT/dft). | DFT score was significantly higher in participants with ID (p = 0.04). Higher ‘D’ component compared to that in children without ID (p = 0.03). DFT score was higher in healthy children (p = 0.04) with higher ‘d’ component (p = 0.05). DFT/dft scores did not include the (M/m) component. ID group had significantly more salivation (p = 0.01), and more put their hands inside their mouths (p = 0.003). | |
| Gufran et al., 2019 | Cross-sectional (analytical) | Riyadh | Special needs school (n = 1) | n = 81 young adults and adults | DS | 16–40 years | 0 | N/A | OH status. (DMFT) (GI) (PI). | Poor periodontal health and high prevalence of dental caries and PI in the majority of males with DS. No association of age with GI. Younger subjects had higher PI (p < 0.001). |
| AlHumaid et al., 2020 | Cross-sectional (analytical) | Eastern Province: Dammam, AlKhobar, Dhahra, Al-Qatif | Special needs schools (n = 13) | n = 75 children with ASD | ASD | 6–18 years (10.8 years) | F: M ratio = 1:1.27 | N/A | OH status (DMF) (GI) (PI). OH behavior (tooth brushing, flossing, sugar consumption). | The prevalence of dental caries in primary dentition was 76% and 68% in the permanent teeth, with a mean of 0.85 ± 1.9 and 1.03 ± 2.9, respectively. A total of 31 had gingival disease, mean gingival index was 1.03 ± 0.88, Mean plaque index was 0.95 ± 0.43 n = 17/22.7% did not brush. A total of 61.3% did not floss. A total of 18 (24%) always consumed sugar. Positive parental attitude resulted in lower sugar intake and better oral health. |
| Basha et al., 2021 | Cross sectional | Taif | Special needs schools | n = 350 children with MD | Obesity, ID, ASD, CP, HI, DS, MD ID (n = 121) A (n = 74) CP (n = 40) DS (n = 65) DB (n = 30) MD (n = 20) | 6–16 years | n = 219 | 6–11 years n = 118) 12–16 years n = 232) | OH status (TDI). | A total of 23.1% of children with special needs had TDIs. Children with obesity had a high prevalence of TDIs (30.3%). Children with CP were 3.18 times more likely to experience TDIs than other disabilities. |
| Shah et al., 2015 ([41]) | Cross-sectional | Al-Kharj | Special needs center | n = 80 | Learning Disability—22 Epilepsy—14 Cerebral Palsy—26 Down syndrome —4 Behavior Disorder—5 Attention Deficit Hyperactivity disorder (ADHD)—2 Multiple Diagnosis-7 | 16–50 years | OH status (DMFT/ (DMFS) Clinically examined periodontal conditions. Retained teeth cross-tabulation. | Mean DMFT: a mean DMFT of 3.75, slightly higher than 3.34 of the Saudi population. The majority presented with poor oral hygiene and a higher periodontal treatment complexity. Retained deciduous tooth: (25%) 20 patients had at least one retained deciduous tooth. Higher numbers were found in those with a learning disability, multiple diagnoses, and Down syndrome. | ||
| Mohamed et al., 2021 ([42]) | Cross-sectional | Taif | NR | n = 400 children with MD | ASD (n = 107), CP (n = 43), DS (n = 70), ID (n = 123); HI/VI (n = 33), MD (n = 24) | 6–16 years | n = 171 (77.7%) | Underweight/normal weight (n = 214) Obese (n = 186) | OH status (dmft or DMFT) (dmfs or DMFS) OH behavior (sugar consumption and brushing frequency). | Caries prevalence: CP, 76.7%; ASD, 78.5%; DS, 47.1%; ID, 79.7; HI/VI: 66.7%; MD, 79.2%. Obese, 77.9%; Non-obese: 67.3%. |
| Sandeepa et al., 2021 ([43]) | Cross-sectional | Aseer region | Special needs institute (n = 4) | n = 54 children with DS | DS | 0–24 years | 0–6 years 7–12 years 13–18 years 19–24 years | OH status (DMFT) (OHI) (PI) (PPD) Occlusal abnormalities (visually observed). | The 19–24-year-old individuals with DS had the highest prevalence of PD (71.4%; p < 0.05), compared to other age groups. No difference in DMFS among age groups. Females had a higher prevalence of PD and DMFS score, when compared to males. Females had a higher number of cases of poor oral hygiene (66.7%), compared to males (27.3%), which was statistically significant (p < 0.05). Malocclusion: All patients had class III skeletal relation. Malocclusion was seen in 42 (75%) and abnormality in the shape, number, or eruption was observed in 30 (53.6%) subjects. Hypoplasia was seen in 19.6% and attrition was seen in 17.9%. | |
| Alfaraj et al., 2021 ([44]) | Cross-sectional | Qatif | Special needs schools (n = 8), mainstream schools (n = 3) | n = 700 caregivers | MD | Age of individuals with special needs not reported. | n = 186 caregivers | OH care utilization (barriers). | Difficulties in accessing dental care: Lack of time—54.8%. Unsuitable clinic environment—60.8%. Transportation issues—51.9%. Medical issues—51%. Distance—51%. | |
| Shah et al., 2020 ([45]) | A longitudinal study | Al-Kharj: | Special Care School Children | 163 children with special needs | VI (n = 8) HI (n = 20) SI (n = 21) DS (n = 33) LD (n = 48) ADHD (n = 8) ASD (n = 20) MD (n = 5) | 6–15 years | 0 | According to their disabilities | OH status (DMFT/dmft) PI. | Total PI of the overall sample = 1.55. The HI and SI group had lower average mean plaque score of 1.02 (SD ± 0.59). This was statistically significant (p < 0.05). Plaque scores and mean decayed (D) component were significantly higher in intellectual disabilities, as compared to physical disabilities. There was no significant difference among caries prevalence and decayed components among various groups of disabilities. |
| Al-Damri et al., 2017 ([46]) | Cross-sectional | Riyadh | Special needs centers (n = 3) | NR | DS (n = 100) | 8–12 years | NR | DS (n = 100) non-DS (n = 100) | OH status (DMFT) (OHI). | No statistically significant difference was evident between any of the parameters in the control and study group. The results were calculated at 95% confidence level (p value = 0.05). After comparison, the values were: D = 0.059, M = 0.090, F = 0.65, and OHI = 0.098. |
| Alzughaibi et al., 2017 ([47]) | Cross-sectional | Makkah | Special needs centers (n unknown) | 203 children with DS and non-DS | DS (n = 100) | 4–15 years | 0 | DS (n = 100) Non-DS (n = 103) | OH status DMFT and deft (with salivary amylase, pH, and flow rate). | Deft: DS: 2.72 ± 4.0. Control: 3.88 ± 3.65. p = 0.03. DMFT: DS: 2.27 ± 3.9. Control: 1.21 ± 2.08. p = 0.02. |
| AL-Otaibi et al., 2016 ([48]) | Cross-sectional | Al-Qassim | NR | 206 children with DS and non-DS | DS (n = 121) | 6–12 years | Gender of only control mentioned (85 boys) | DS (n = 121) non-DS (n = 85) | OH status DMFT/dmft. | Permanent teeth: DS: 63.9% were caries free. Controls: 80% caries-free. Primary teeth: DS: 80.6. Control: 89.4%. p > 0.05. |
| AlHammad and Wyne 2010 ([14]) | Cross-sectional | Riyadh | Special needs center (n = 1) | 140 children with CP | CP (n = 140) | 3–12 years | 41.4% | 3–6 years (n = 41) 7–9 years (n = 52) 10–12 years (n = 47) | OH status (DMFT) (OHI). | Caries Prevalence: 98.6%. DMFS: Group 1 A total of 18.8 (±16.3). Group 2 A total of 23.4 (±17.7). Group 3 A total of 20.5 (±14.0). No statistically significant differences (p > 0.05) in DMFS scores between the three age groups. No significant difference in DMFS scores between male and female CP children. However, female CP children had significantly higher (p < 0.05) filled surfaces than male CP children. Oral hygiene status:The percentage of children with poor OH increased with the age (p < 0.05). There was no statistically significant difference between genders in caries and OH. A strong association (p < 0.001) was found between OH status and DMFS scores; the children with poor OH had higher DMFS scores |
| Brown et al., 2009 [49] | Retrospective | Riyadh | Dental clinic/tertiary care center | 386 medically compromised and healthy children | Medically compromised (n = 386) | 5 years | n = 183 | Medically compromised (n = 211) Healthy (n = 175) | OH status (deft index). | Caries prevalence: Medically compromised: 91.9%. Healthy: 84.0%. p > 0.05. |
| Tantawi et al., 2017 [50] | Cross-sectional | Dammam, Qatif, Dhahran, Anak, Dareen, UmulSahik, Al-Nabia, Khobar | Outreach programs | 819 adults with and without disabilities | Sensory disabilities (50.9%), motor (33.7%), ID (12.4%), and MD (3%) | 32.3 (healthy), 34 (disabled) | n = 401 | Special needs (169) Non-special needs (632) | OH status (need for periodontal care). OH behavior (brushing, smoking). OH care utilization (dental visits and treatment utilized). | No significant differences observed between groups in terms of periodontal needs, smoking habits, dental visits, or oral hygiene habits. In need of periodontal care: healthy 66.5% vs. individuals with disabilities 67.3%; overall = 66.8%). Smoking: 27.3% healthy vs. 17.9% in individuals with special needs. Brushing twice or more daily: 54.6% and 55.8%. Dental visits: 46.6% and 46.7%. Professional cleaning: (25.9% and 21.7%. |
| Al Shehri et al., 2018 ([10]) | Cross-sectional | Riyadh | Primary and middle schools (n = 16) | 269 children with VI | VI (n = 269) | 7–15 years (9.91 ± 2.41) | n = 119 female | None | OH care utilization (dental visits last year and reason). | A total of 28.3% of the females and 36.7% of the males did not receive dental care during the last 12 months. Pain with teeth, gums, or mouth was the main reason for the children’s last visit to the dentist. |
| Alshihri, Abdulmonem A. et al., 2021 ([51]) | Cross-sectional | Riyadh | Societies for special needs (n = 2) | 232 mothers | ASD Children (n = 232) | Children between 2.5 and 14 years | 29 (20.4%) girls | 142 mothers (who are the primary caregivers) | OH care utilization (Previous dental visits and barriers). | A total of 33.8% had not been to a dentist before. A total of 75.4% of children did not have insurance with dental coverage. Barriers reported: Cost (75.4%), finding a dentist (74.6%), uncooperative behavior of child (45.1%). Age did not impact finding a dentist (p = 0.429). Having medical insurance and a previous bad experience showed significant effects on the difficulty in finding dental care (p < 0.05). |
| Introduction | Methodology | Results | Discussion | Others | Overall Quality | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study (Author, Year) | Adequate Objectives of Study | Study Design | Sample Size Justification | Target Population Defined | Appropriate Population Base | Address Non-Responders | Appropriate risk/Outcome Variables Measured | Piloting/Validation of Measurement Instrument(s) | Appropriate Statistics Conducted | Description of Statistics | Basic Data | Response Rate Concerns | Non-Responder Information | Consistency | Adequate Reporting | Justification by Results | Limitations Discussed | Funding | Ethical Approval/Consent | |
| AlSarheed et al., 2003 | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | No | Yes | No | No | Yes | Yes | Yes | No | No | No | Moderate |
| AlSarheed et al., 2003b | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | No | Yes | No | No | Yes | Yes | Yes | No | No | No | Moderate |
| AlKawari, 2021 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Moderate |
| AlKhadra et al., 2017 | Yes | Yes | No | No | Yes | No | Yes | No | No | No | Yes | No | No | Yes | No | No | No | No | Yes | Low |
| AlSarheed, 2014 | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | No | Yes | No | No | Yes | Yes | Yes | No | No | No | Moderate |
| Qahtani and Wyne, 2004 | Yes | Yes | Yes | No | No | No | Yes | No | No | No | No | No | No | Yes | No | Yes | No | No | No | Low |
| Wyne, 2007 | Yes | Yes | Yes | No | No | No | No | No | No | No | No | No | No | Yes | Yes | Yes | No | No | Yes | Low |
| Sharifa and Al-Shehri, 2012 | Yes | Yes | No | No | No | No | No | Yes | No | No | No | No | No | Yes | Yes | Yes | No | No | Yes | Low |
| Ashour et al., 2018 | Yes | Yes | No | Yes | No | No | Yes | No | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| Murshid, 2014 | Yes | Yes | No | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| Murshid, 2014b | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| Diab et al., 2016 | Yes | Yes | No | No | No | No | Yes | Yes | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | No | Yes | Low |
| AlSadhan et al., 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Al-Qahtani et al., 2017 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Moderate |
| AlHazmi et al., 2014 | Yes | Yes | No | No | Yes | No | Yes | No | No | No | No | No | No | Yes | No | Yes | Yes | No | Yes | Low |
| Wyne et al., 2017 | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | Moderate |
| Al-Sehaibany, 2018 | Yes | No | No | No | Yes | No | Yes | No | Yes | No | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Kotha et al., 2018 | Yes | Yes | No | Yes | No | No | Yes | No | Yes | Yes | Yes | No | No | Yes | No | Yes | Yes | Yes | No | Moderate |
| Mustafa et al., 2018 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| AlKahtani et al., 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | Yes | Moderate |
| AlZahrani et al., 2019 | Yes | Yes | No | Yes | Yes | No | Yes | No | No | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Moderate |
| Alaki and Bakry, 2012 | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | No | Yes | Yes | Moderate |
| Gufran et al., 2019 | Yes | Yes | No | Yes | Yes | No | Yes | No | Yes | No | Yes | No | No | Yes | Yes | Yes | No | No | No | Low |
| Al Humaid, 2020 | Yes | Yes | No | No | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Basha et al., 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Shah et al., 2015 | Yes | Yes | No | No | Yes | No | Yes | No | No | No | Yes | Yes | No | Yes | No | Yes | No | Yes | No | Low |
| Mohamed et al., 2021 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | No | No | Yes | No | No | Yes | Moderate |
| Sandeepa et al., 2021 | Yes | Yes | No | No | No | No | Yes | No | Yes | No | Yes | No | No | Yes | Yes | Yes | No | No | No | Low |
| Alfaraj et al., 2021 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | No | No | Yes | Moderate |
| Shah et al., 2020 | Yes | Yes | No | No | Yes | No | Yes | Yes | No | No | Yes | No | No | No | Yes | Yes | No | No | No | Low |
| Al-Damri et al., 2017 | Yes | Yes | No | No | Yes | No | Yes | Yes | No | No | Yes | No | No | No | Yes | Yes | No | No | No | Low |
| Alzughaibi et al., 2017 | Yes | Yes | No | No | Yes | No | Yes | Yes | No | No | Yes | No | No | No | Yes | Yes | No | No | No | Low |
| Al-Otaibi et al., 2016 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No | No | Yes | No | No | No | Yes | Yes | No | Yes | No | Low |
| AlHammad and Wyne, 2010 | Yes | Yes | No | No | Yes | No | Yes | Yes | No | No | Yes | No | No | No | Yes | Yes | No | No | No | Low |
| Brown et al., 2009 | Yes | Yes | No | No | Yes | No | Yes | Yes | No | No | Yes | No | No | No | Yes | Yes | No | No | No | Low |
| Tantawi et al., 2017 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No | No | Yes | No | No | No | Yes | Yes | No | No | Yes | Low |
| Al Shehri et al., 2018 | Yes | Yes | No | No | Yes | No | Yes | Yes | No | No | Yes | No | No | No | Yes | Yes | No | No | No | Low |
| Al Shehri et al., 2021 | Yes | Yes | No | No | Yes | No | Yes | Yes | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Moderate |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asiri, F.Y.I.; Tennant, M.; Kruger, E. Oral Health Status, Oral Health Behaviors, and Oral Health Care Utilization among Persons with Disabilities in Saudi Arabia. Int. J. Environ. Res. Public Health 2022, 19, 16633. https://doi.org/10.3390/ijerph192416633
Asiri FYI, Tennant M, Kruger E. Oral Health Status, Oral Health Behaviors, and Oral Health Care Utilization among Persons with Disabilities in Saudi Arabia. International Journal of Environmental Research and Public Health. 2022; 19(24):16633. https://doi.org/10.3390/ijerph192416633
Chicago/Turabian StyleAsiri, Faris Yahya I., Marc Tennant, and Estie Kruger. 2022. "Oral Health Status, Oral Health Behaviors, and Oral Health Care Utilization among Persons with Disabilities in Saudi Arabia" International Journal of Environmental Research and Public Health 19, no. 24: 16633. https://doi.org/10.3390/ijerph192416633
APA StyleAsiri, F. Y. I., Tennant, M., & Kruger, E. (2022). Oral Health Status, Oral Health Behaviors, and Oral Health Care Utilization among Persons with Disabilities in Saudi Arabia. International Journal of Environmental Research and Public Health, 19(24), 16633. https://doi.org/10.3390/ijerph192416633







