COVID-19 Progression: A County-Level Analysis of Vaccination and Case Fatality in Mississippi, USA
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Data Term and Variable Description
2.3. Statistical Analysis
- EP_POV: Percentage of persons below the poverty estimate.
- EP_UNEMP: Unemployment Rate estimate.
- EP_PCI: Per capita income estimate, 2014–2018 ACS.
- EP_NOHSDP: Percentage of persons with no high school diploma (age 25+) estimate.
- EP_AGE65: Percentage of persons aged 65 and older estimate, 2014-2018 ACS.
- EP_MINRTY: Percentage minority (all persons except white, non-Hispanic) estimate, 2014–2018 ACS.
- EP_UNINSUR: Percentage of uninsured in the total civilian noninstitutionalized population estimate, 2014–2018 ACS.
- Urban-Rural Classification: 2013 NCHS urban-rural classification scheme for counties.
- CDC SVI: Social vulnerability index (SVI) scores, which range from 0 to 1.
- CCVI: COVID-19 community vulnerability index (CCVI) scores, which also vary from 0 to 1, are from Surgo Ventures.
- Total COVID-19 cases in Mississippi (as of 3 March 2022).
- Total COVID-19 deaths in Mississippi (as of 3 March 2022).
- Full Vaccinated Population in Mississippi (as of 3 March 2022).
- No correlation between target and feature variables is established (independence).
- The target and feature variables are statistically correlated (dependence).
- The feature of interest and county-level vaccination rate.
- The feature of interest and county-level total cases.
- The feature of interest and county-level death rate.
2.4. Data Visualization
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosenthal, M. Fauci: COVID-19 Worst Pandemic in 100 Years. Available online: https://www.idse.net/COVID-19/Article/10-20/Fauci-COVID-19-Worst-Pandemic-in-100-Years/60937 (accessed on 24 April 2022).
- Spiteri, G.; Fielding, J.; Diercke, M.; Campese, C.; Enouf, V.; Gaymard, A.; Bella, A.; Sognamiglio, P.; Sierra Moros, M.J.; Riutort, A.N.; et al. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill. 2020, 25, 2000178. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. CDC Covid Data Tracker. Centers for Disease Control and Prevention. Available online: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (accessed on 24 April 2022).
- US Census Bureau. Available online: https://www.census.gov/ (accessed on 24 April 2022).
- Centers for Disease Control and Prevention. How to Protect Yourself and Others. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html (accessed on 4 December 2022).
- Pradhan, D.; Biswasroy, P.; Kumar Naik, P.; Ghosh, G.; Rath, G. A review of current interventions for COVID-19 prevention. Arch. Med. Res. 2020, 51, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Donadio, G.; Choudhary, M.; Lindemer, E.; Pawlowski, C.; Soundararajan, V. Counties with Lower Insurance Coverage and Housing Problems Are Associated with Both Slower Vaccine Rollout and Higher COVID-19 Incidence. Vaccines 2021, 9, 973. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.C.; Young, S.G.; Pro, G.C. COVID-19 vaccination rates vary by community vulnerability: A county-level analysis. Vaccine 2021, 39, 4245–4249. [Google Scholar] [CrossRef] [PubMed]
- Katella, K. Comparing the COVID-19 Vaccines: How Are They Different? Yale Medicine. Available online: https://www.yalemedicine.org/news/COVID-19-vaccine-comparison (accessed on 24 April 2022).
- World Health Organization. Coronavirus. World Health Organization. Available online: https://www.who.int/health-topics/coronavirus#tab=tab_1 (accessed on 24 April 2022).
- Centers for Disease Control and Prevention. Vaccines for COVID-19. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html (accessed on 24 April 2022).
- Graham, H.; White, P.C.L. Social Determinants and lifestyles: Integrating Environmental and Public Health Perspectives. Public Health 2016, 141, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Social Determinants of Health. Social Determinants of Health—Healthy People 2030. Available online: https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed on 24 April 2022).
- Bayati, M.; Noroozi, R.; Ghanbari-Jahromi, M.; Jalali, F.S. Inequality in the distribution of Covid-19 vaccine: A systematic review. Int. J. Equity. Health 2022, 21, 122. [Google Scholar] [CrossRef] [PubMed]
- Barry, V.; Dasgupta, S.; Weller, D.L.; Kriss, J.L.; Cadwell, B.L.; Rose, C.; Pingali, C.; Musial, T.; Sharpe, J.D.; Flores, S.A.; et al. Patterns in COVID-19 vaccination coverage, by social vulnerability and urbanicity—United States, December 14, 2020–May 1, 2021. MMWR 2021, 70, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Singu, S.; Acharya, A.; Challagundla, K.; Byrareddy, S.N. Impact of social determinants of health on the emerging COVID-19 pandemic in the United States. Front. Public Health 2020, 8, 406. [Google Scholar] [CrossRef] [PubMed]
- Explore Health Topics. America’s Health Rankings. (n.d.). Available online: https://www.americashealthrankings.org/health-topics/tag-122/comparison-plot?topics=category-15 (accessed on 18 May 2022).
- Zhang, L.; McLeod, S.T.; Vargas, R.; Liu, X.; Young, D.K.; Dobbs, T.E. Subgroup comparison of covid-19 case and mortality with associated factors in Mississippi: Findings from analysis of the first four months of public data. J. Biomed. Res. 2020, 34, 446. [Google Scholar] [CrossRef] [PubMed]
- Mississippi State Department of Health. Coronavirus Disease 2019 (COVID-19). Coronavirus COVID-19—Mississippi State Department of Health. Available online: https://msdh.ms.gov/msdhsite/_static/14,0,420.html (accessed on 24 April 2022).
- Centers for Disease Control and Prevention. CDC—NCHS—National Center for Health Statistics. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/nchs/index.htm (accessed on 24 April 2022).
- McLaughlin, J.M.; Khan, F.; Pugh, S.; Swerdlow, D.L.; Jodar, L. County-level vaccination coverage and rates of COVID-19 cases and deaths in the United States: An ecological analysis. Lancet Reg. Health Am. 2022, 9, 100191. [Google Scholar] [CrossRef]
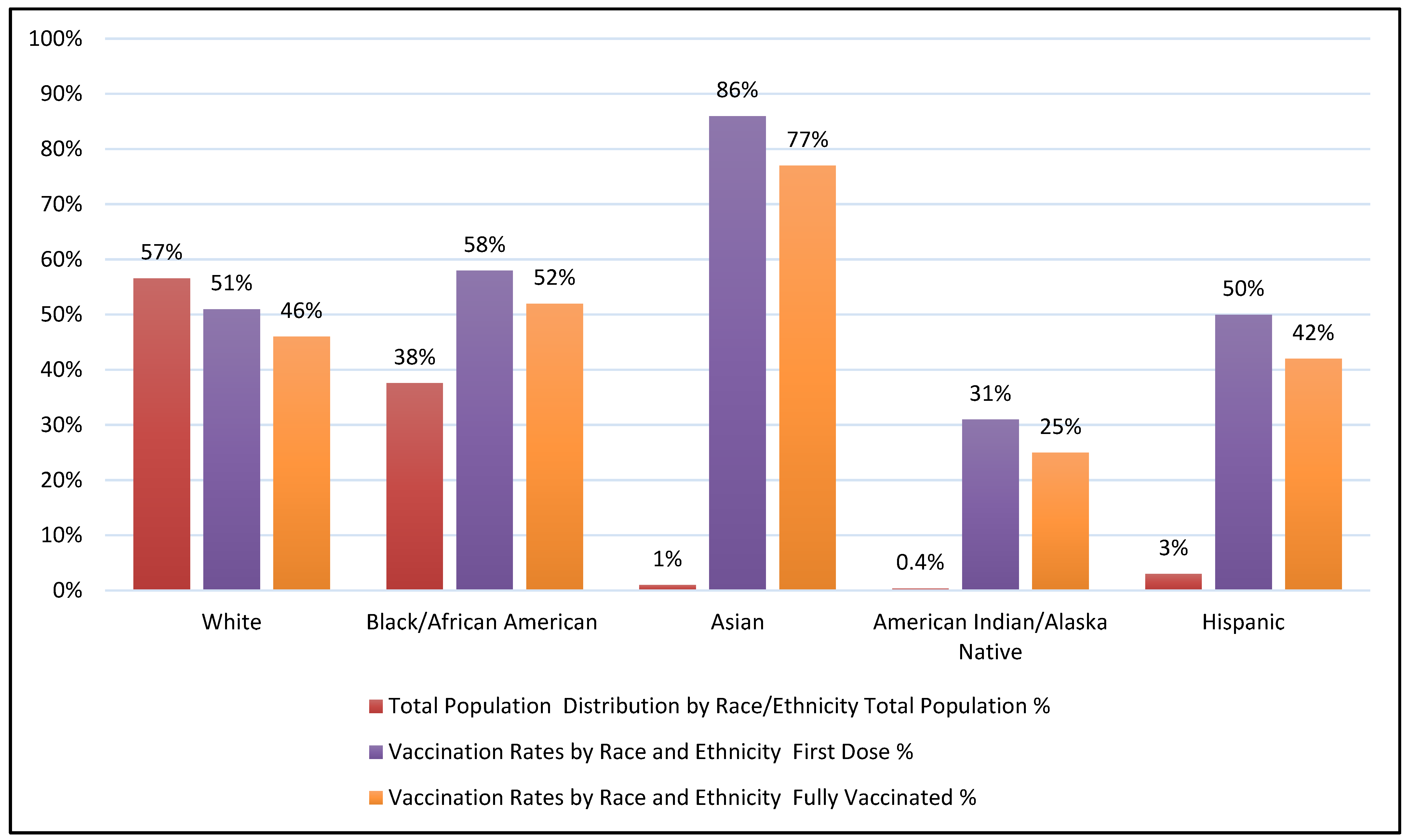
- Wang, C. Asian Americans Have High Vaccine Rates, But It Hasn’t Come Easy, Nonprofit Groups Say. NBCNews.com. Available online: https://www.nbcnews.com/news/asian-america/asian-americans-high-vaccine-rates-hasnt-come-easy-nonprofit-groups-sa-rcna1639 (accessed on 24 May 2022).
- Olson, D. Asian Vaccination Rate for 15 and Older Highest among LONG Island’s Ethnic Groups. Newsday. Available online: https://www.newsday.com/news/health/coronavirus/asian-vaccination-rates-r23227 (accessed on 24 May 2022).
- Hughes, M.M.; Wang, A.; Grossman, M.K.; Pun, E.; Whiteman, A.; Deng, L.; Hallisey, E.; Sharpe, J.D.; Ussery, E.N.; Stokley, S.; et al. County-level COVID-19 vaccination coverage and social vulnerability—United States, December 14, 2020–March 1, 2021. MMWR 2021, 70, 431. [Google Scholar] [CrossRef] [PubMed]
- Murthy, B.P.; Sterrett, N.; Weller, D.; Zell, E.; Reynolds, L.; Toblin, R.L.; Murthy, N.; Kriss, J.; Rose, C.; Cadwell, B.; et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties—United States, December 14, 2020-April 10, 2021. MMWR 2021, 70, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Rasul, M.E.; Cho, J. Social media news use induces COVID-19 vaccine hesitancy through skepticism regarding its efficacy: A longitudinal study from the United States. Front. Psychol. 2022, 13, 900386. [Google Scholar] [CrossRef]
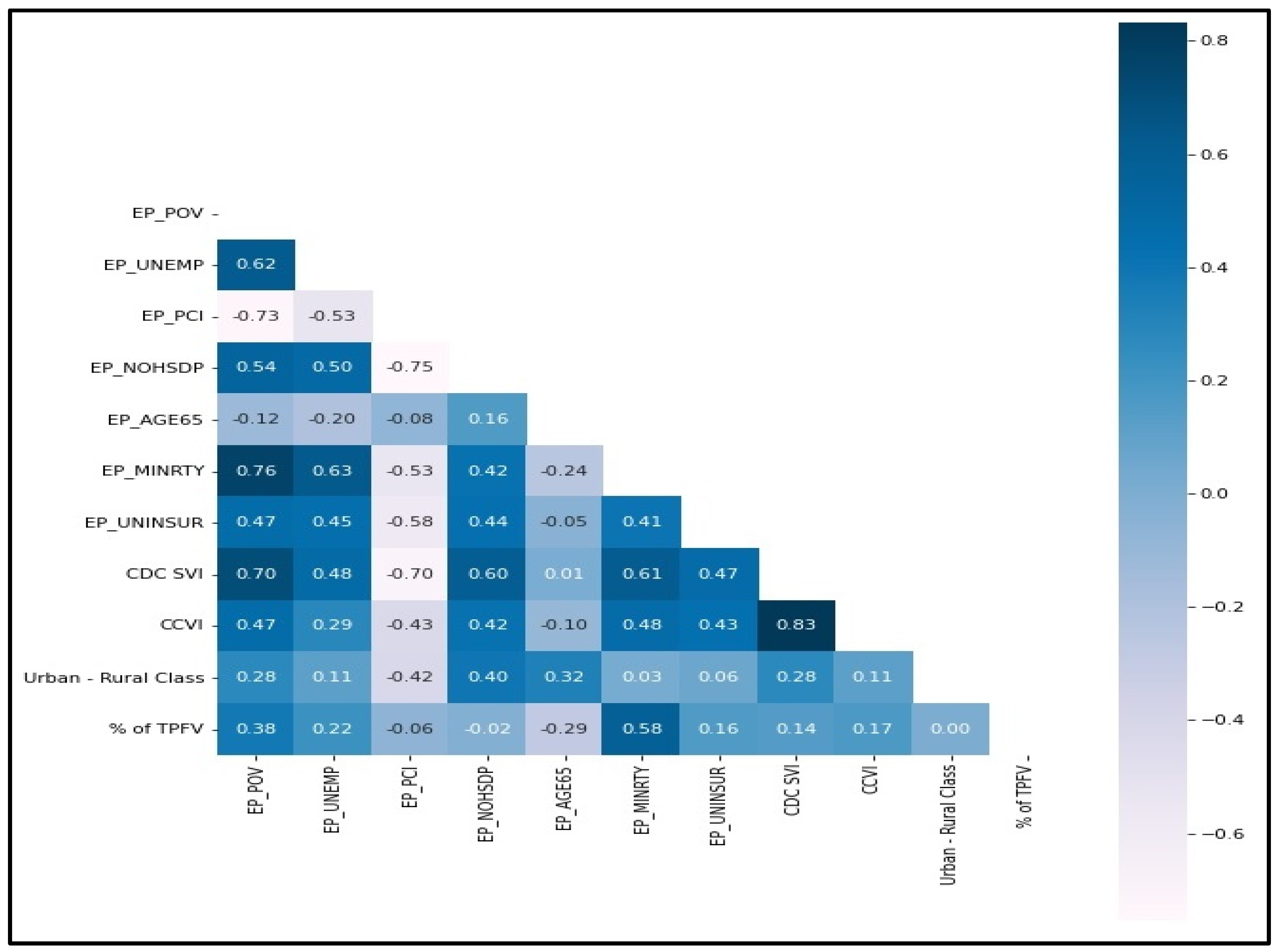
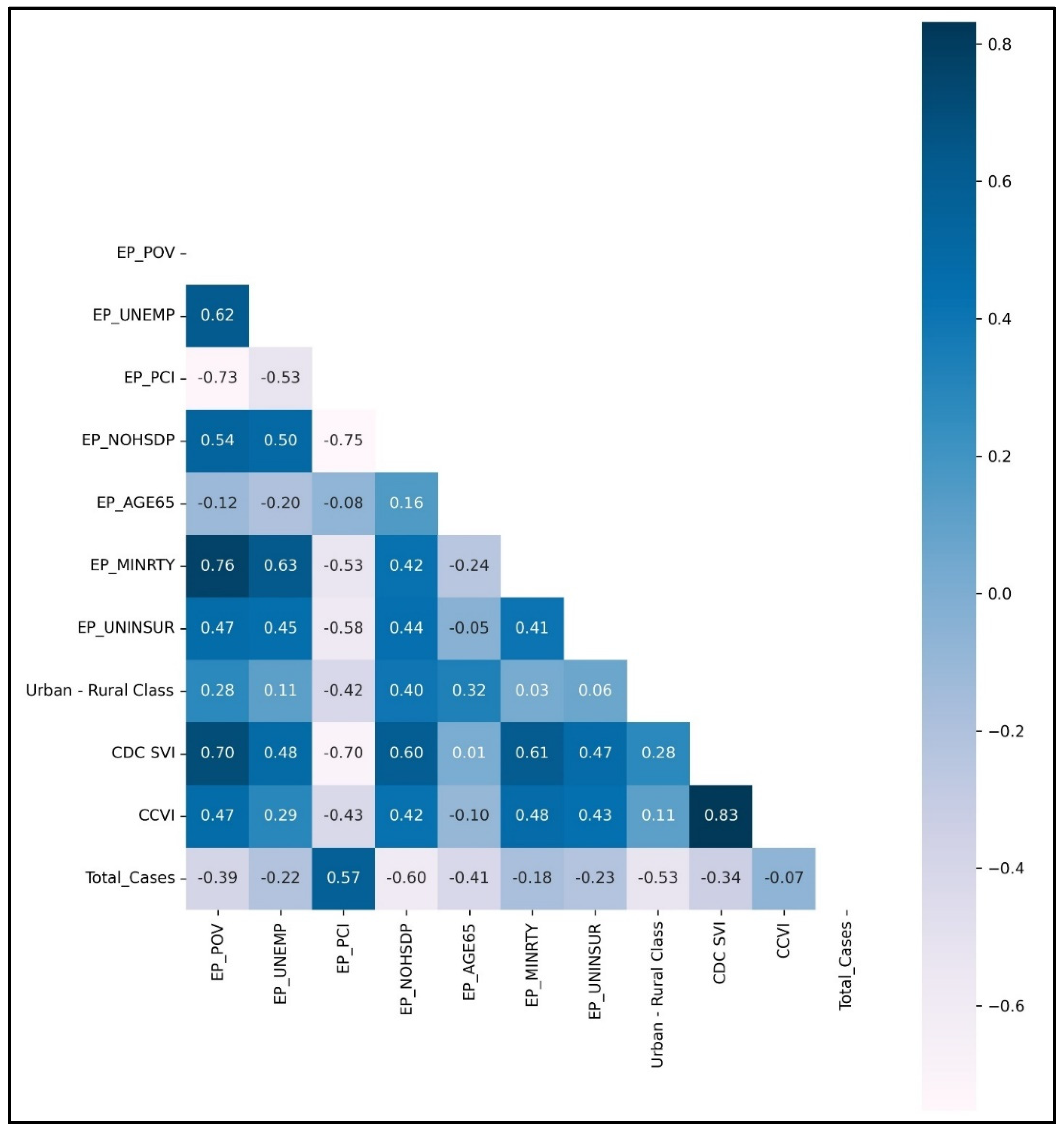
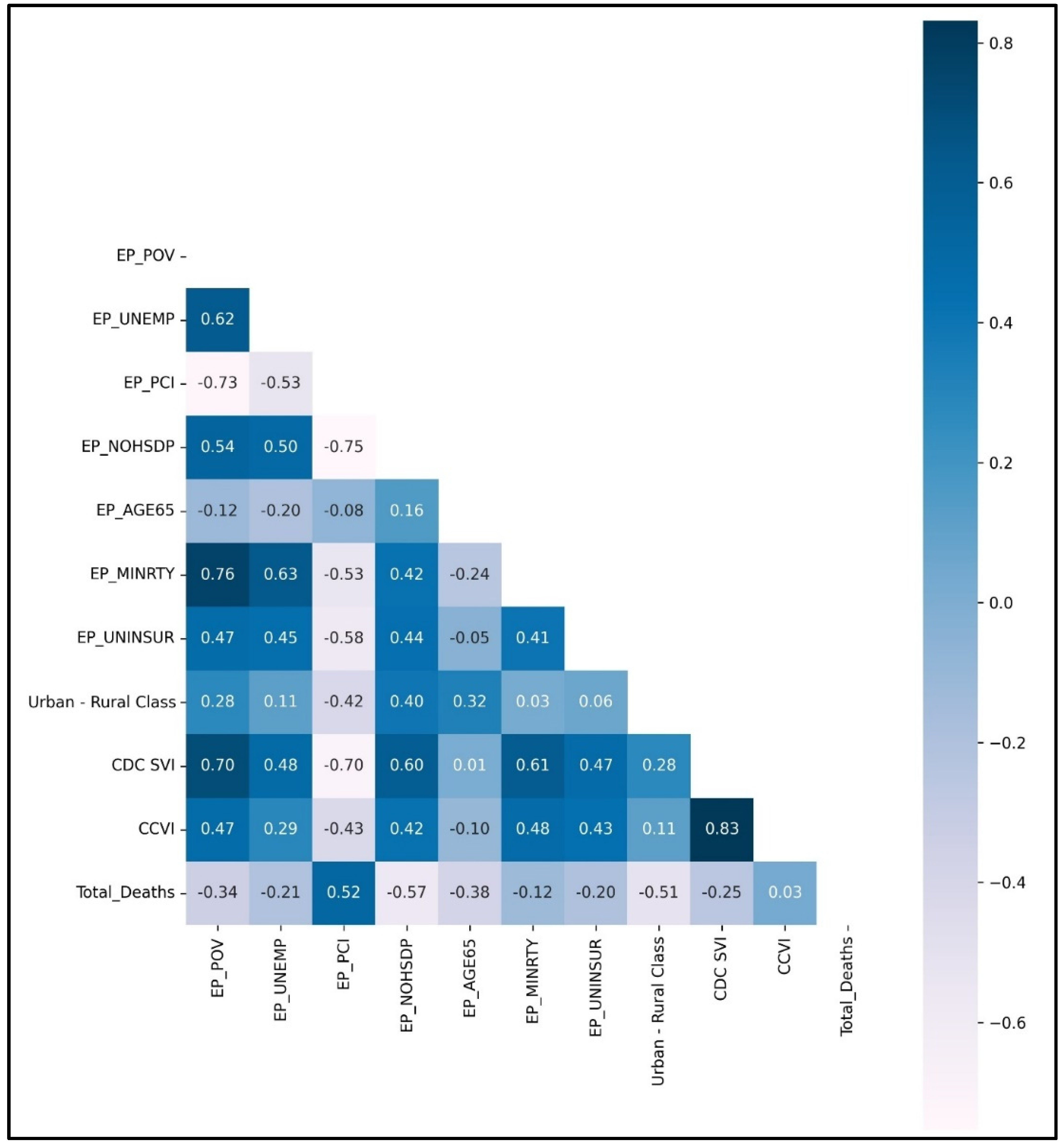
| County-Level Feature | Vaccination Rate Correlation Value | Vaccination Rate 95% Cl | Vaccination Rate p-Value | Total Cases Correlation Value | Total Cases 95% Cl | Total Cases p-Value | Total Deaths Correlation Value | Total Deaths 95% Cl | Total Deaths p-Value |
|---|---|---|---|---|---|---|---|---|---|
| EP_POV | 0.3797 | [0.18, 0.55] | <0.05 | −0.394 | [−0.56, −0.19] | <0.05 | −0.3413 | [−0.52, −0.13] | <0.05 |
| EP_UNEMP | 0.223 | [0.01, 0.42] | <0.05 | −0.2177 | [−0.42, −0.0] | <0.05 | −0.2083 | [−0.41, 0.01] | >0.05 |
| EP_PCI | −0.0637 | [−0.28, 0.16] | >0.05 | 0.5728 | [0.41, 0.7] | <0.05 | 0.5216 | [0.34, 0.66] | <0.05 |
| EP_NOHSDP | −0.0181 | [−0.23, 0.2] | >0.05 | −0.5978 | [−0.72, −0.44] | <0.05 | −0.5674 | [−0.7, −0.4] | <0.05 |
| EP_AGE65 | −0.2859 | [−0.47, −0.07] | <0.05 | −0.413 | [−0.58, −0.22] | <0.05 | −0.3825 | [−0.55, −0.18] | <0.05 |
| EP_MINRTY | 0.5784 | [0.41, 0.71] | <0.05 | −0.1767 | [−0.38, 0.04] | >0.05 | −0.1224 | [−0.33, 0.1] | >0.05 |
| EP_UNINSUR | 0.1567 | [−0.06, 0.36] | >0.05 | −0.2267 | [−0.42, −0.01] | <0.05 | −0.1984 | [−0.4, 0.02] | >0.05 |
| CDC SVI | 0.1412 | [−0.08, 0.35] | >0.05 | −0.3399 | [−0.52, −0.13] | <0.05 | −0.2535 | [−0.45, −0.04] | >0.05 |
| CCVI | 0.1652 | [−0.05, 0.37] | >0.05 | −0.0721 | [−0.28, 0.15] | >0.05 | 0.0311 | [−0.19, 0.25] | >0.05 |
| Urban-Rural Class | 0.0045 | [−0.21, 0.22] | >0.05 | −0.5282 | [−0.67, −0.35] | <0.05 | −0.5068 | [−0.65, −0.33] | <0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghosh, S.; Ahmad, H.A.; Akil, L.; Tchounwou, P.B. COVID-19 Progression: A County-Level Analysis of Vaccination and Case Fatality in Mississippi, USA. Int. J. Environ. Res. Public Health 2022, 19, 16552. https://doi.org/10.3390/ijerph192416552
Ghosh S, Ahmad HA, Akil L, Tchounwou PB. COVID-19 Progression: A County-Level Analysis of Vaccination and Case Fatality in Mississippi, USA. International Journal of Environmental Research and Public Health. 2022; 19(24):16552. https://doi.org/10.3390/ijerph192416552
Chicago/Turabian StyleGhosh, Shinjita, Hafiz A. Ahmad, Luma Akil, and Paul B. Tchounwou. 2022. "COVID-19 Progression: A County-Level Analysis of Vaccination and Case Fatality in Mississippi, USA" International Journal of Environmental Research and Public Health 19, no. 24: 16552. https://doi.org/10.3390/ijerph192416552
APA StyleGhosh, S., Ahmad, H. A., Akil, L., & Tchounwou, P. B. (2022). COVID-19 Progression: A County-Level Analysis of Vaccination and Case Fatality in Mississippi, USA. International Journal of Environmental Research and Public Health, 19(24), 16552. https://doi.org/10.3390/ijerph192416552







