Health Impacts of High BMI in China: Terrible Present and Future
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Statistical Analysis
3. Results
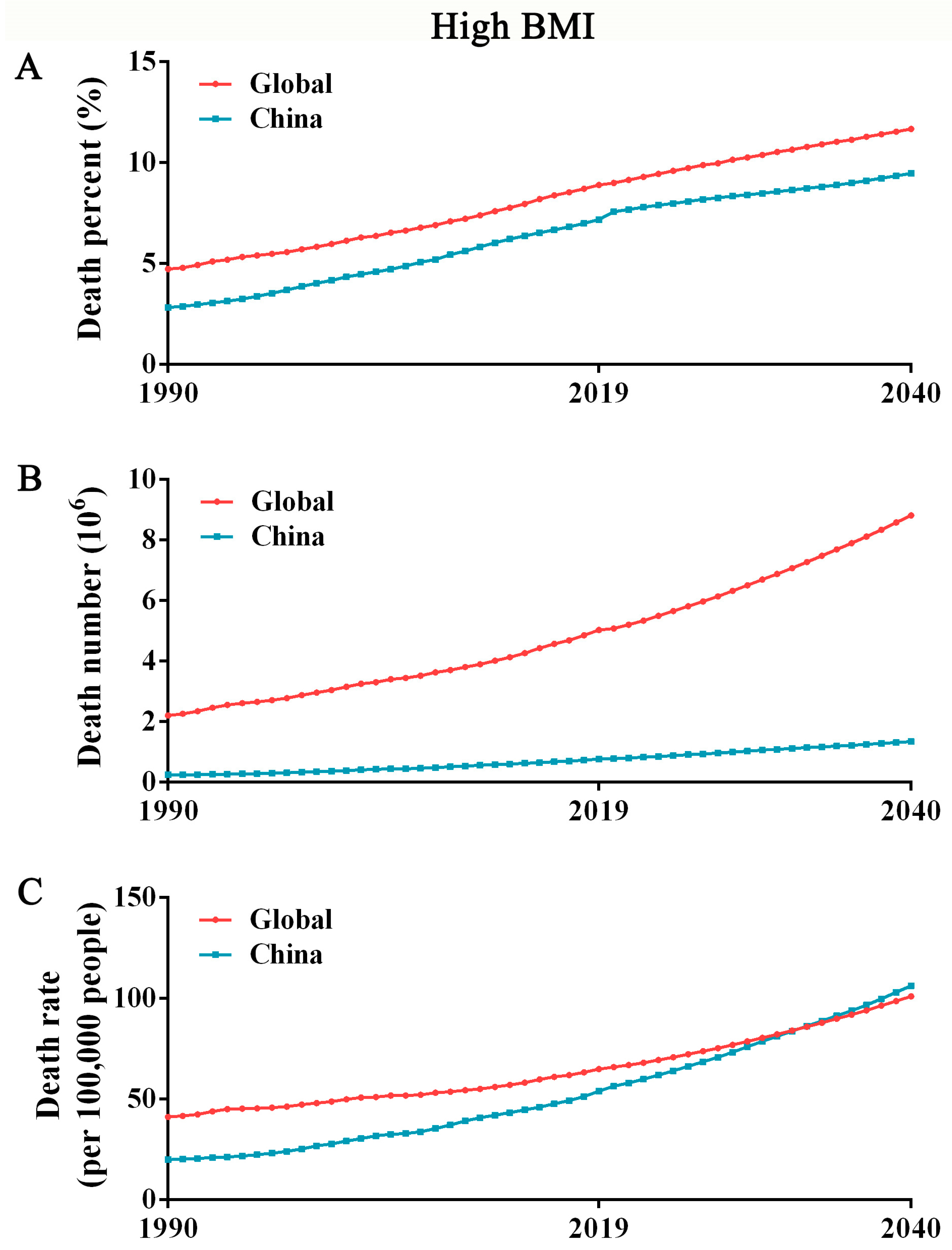
3.1. The Mortality of High BMI in China May Exceed That in Global in the Next 10 Years
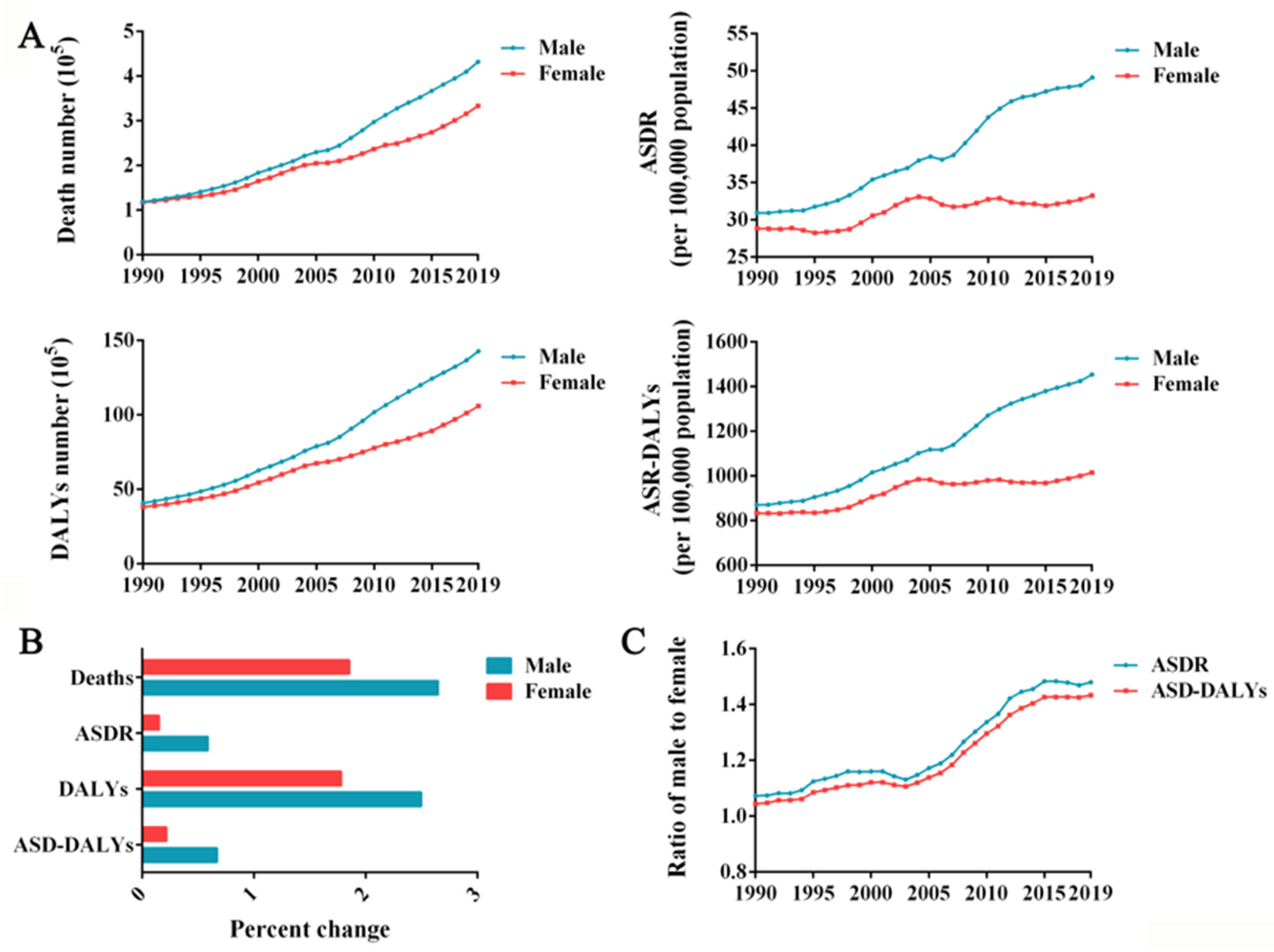
3.2. The Burden of High BMI Is Higher in Men Than in Women
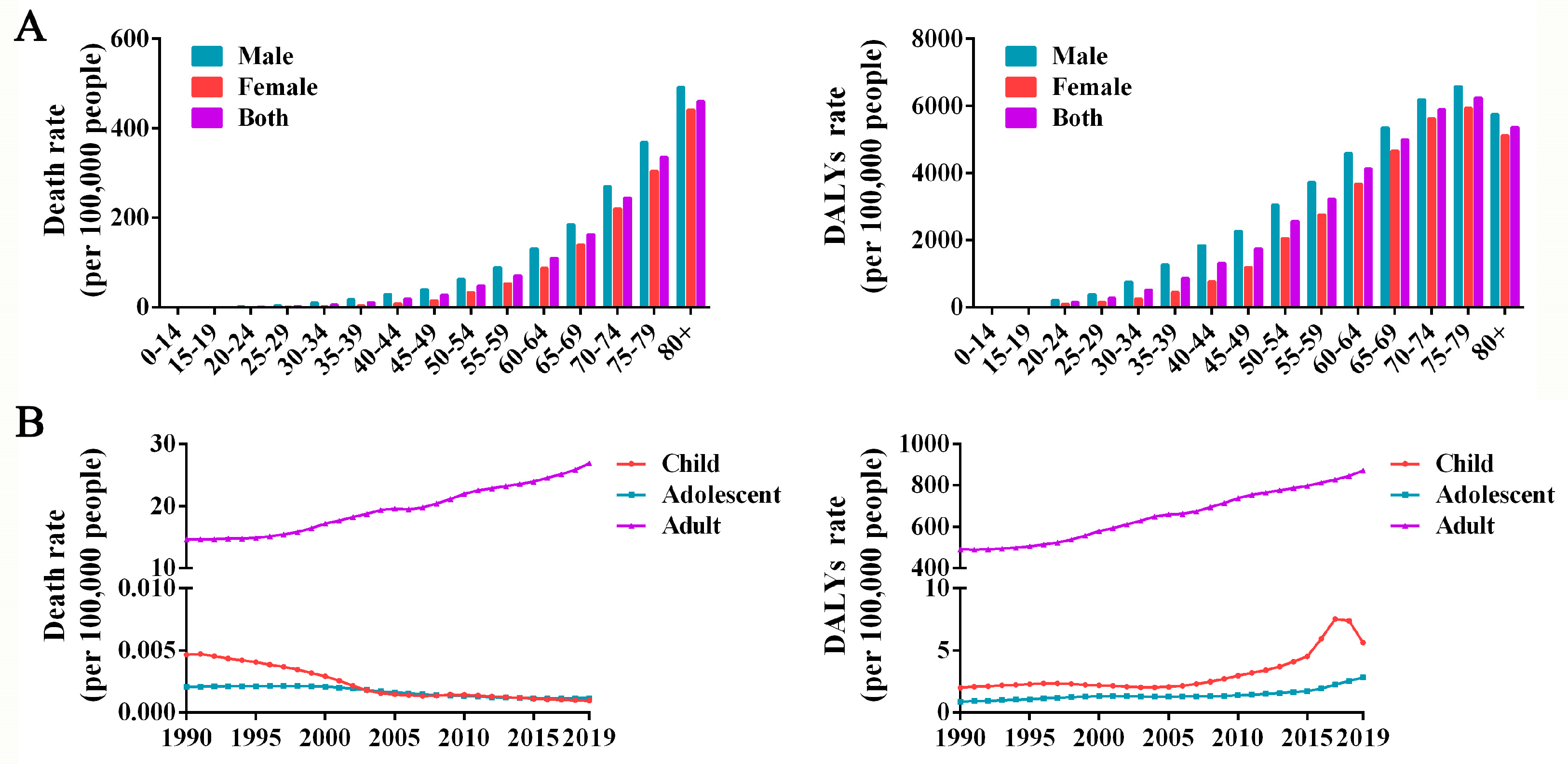
3.3. High-BMI-related Burden in Adults Exceeds That in Children and Adolescents
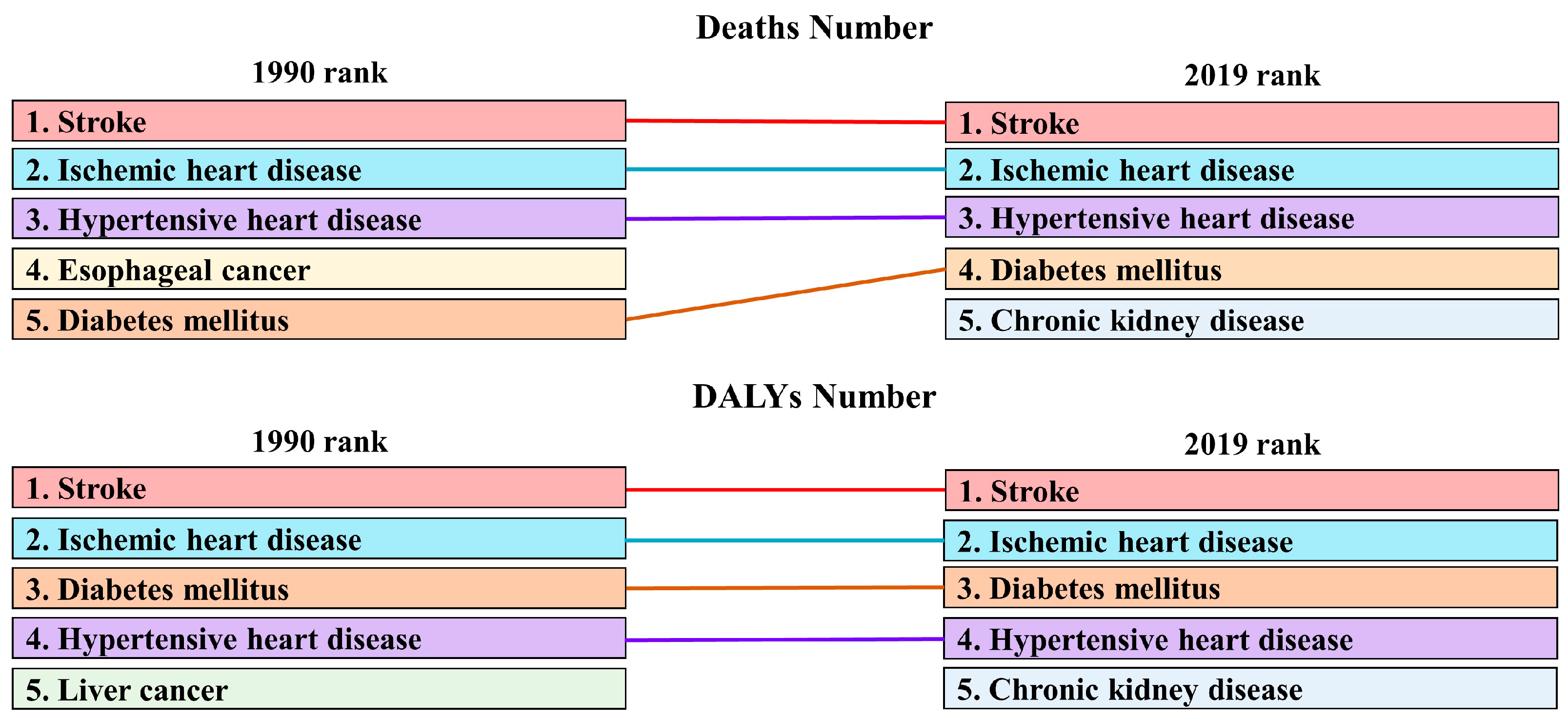
3.4. Each Disease Is Affected Differently by a High BMI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Caballero, B. Humans against Obesity: Who Will Win? Adv. Nutr. 2019, 10, S4–S9. [Google Scholar] [CrossRef] [PubMed]
- Dikaiou, P.; Björck, L.; Adiels, M.; Lundberg, C.E.; Mandalenakis, Z.; Manhem, K.; Rosengren, A. Obesity, overweight and risk for cardiovascular disease and mortality in young women. Eur. J. Prev. Cardiol. 2021, 28, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Shields, G.S.; Guo, C.; Liu, Y. Executive function performance in obesity and overweight individuals: A meta-analysis and review. Neurosci. Biobehav. Rev. 2018, 84, 225–244. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.M.; Liu, X.; Alhamzawi, R.; Becker, F.; Lord, J. Statistical methods for body mass index: A selective review. Stat. Methods Med. Res. 2018, 27, 798–811. [Google Scholar] [CrossRef]
- Bode, E.D.; Mathias, K.C.; Stewart, D.F.; Moffatt, S.M.; Jack, K.; Smith, D.L. Cardiovascular Disease Risk Factors by BMI and Age in United States Firefighters. Obesity 2021, 29, 1186–1194. [Google Scholar] [CrossRef]
- Wei, J.; Liu, X.; Xue, H.; Wang, Y.; Shi, Z. Comparisons of Visceral Adiposity Index, Body Shape Index, Body Mass Index and Waist Circumference and Their Associations with Diabetes Mellitus in Adults. Nutrients 2019, 11, 1580. [Google Scholar] [CrossRef]
- Azhar, A.; Hassan, N.; Tapolyai, M.; Molnar, M.Z. Obesity, Chronic Kidney Disease, and Kidney Transplantation: An Evolving Relationship. Semin. Nephrol. 2021, 41, 189–200. [Google Scholar] [CrossRef]
- Xing, J.; Guan, X.; Zhang, Q.; Chen, S.; Wu, S.; Sun, X. Triglycerides Mediate Body Mass Index and Nonalcoholic Fatty Liver Disease: A Population-Based Study. Obes. Facts 2021, 14, 190–196. [Google Scholar] [CrossRef]
- Zhang, G.; Cao, F.; Shi, L.; Ma, T.; Zhang, L. Contribution of high body mass index and alcohol use to liver cancer-related mortality: A study based on 195 countries or territories. Dig. Liver Dis. 2020, 52, 221–231. [Google Scholar] [CrossRef]
- Kim, J.; So, W.Y. High Body Mass Index is Associated with the Extent of Muscle Damage after Eccentric Exercise. Int. J. Environ. Res. Public Health 2018, 15, 1378. [Google Scholar] [CrossRef]
- Titchener, K.; Wong, Q.J. A weighty issue: Explaining the association between body mass index and appearance-based social anxiety. Eat. Behav. 2015, 16, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Horenstein, A.; Kaplan, S.C.; Butler, R.M.; Heimberg, R.G. Social anxiety moderates the relationship between body mass index and motivation to avoid exercise. Body Image 2021, 36, 185–192. [Google Scholar] [CrossRef] [PubMed]
- GBD 2015 Obesity Collaborators; Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [PubMed]
- Dai, H.; Alsalhe, T.A.; Chalghaf, N.; Riccò, M.; Bragazzi, N.L.; Wu, J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990-2017: An analysis of the Global Burden of Disease Study. PLoS Med. 2020, 17, e1003198. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Siegel, R.L.; Torre, L.A.; Pearson-Stuttard, J.; Islami, F.; Fedewa, S.A.; Goding Sauer, A.; Shuval, K.; Gapstur, S.M.; Jacobs, E.J.; et al. Global patterns in excess body weight and the associated cancer burden. CA Cancer J. Clin. 2019, 69, 88–112. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.R.; Chalise, B.; Shrestha, N.; Ojha, B.; Maskey, J.; Sharma, D.; Godwin, P.; Aryal, K.K. Mortality and risk factors of disease in Nepal: Trend and projections from 1990 to 2040. PLoS ONE 2020, 15, e0243055. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.X.; Hu, K.L.; Liu, H.; Zhang, X.Y.; Li, H.M.; Zhou, F.; Liu, Y.; Lei, F.; Qin, J.; Zhao, Y.; et al. Global Burden of Disease Study 2019 suggests that metabolic risk factors are the leading drivers of the burden of ischemic heart disease. Cell. Metab. 2021, 33, 1943–1956.e2. [Google Scholar] [CrossRef]
- Gutin, I. In BMI We Trust: Reframing the Body Mass Index as a Measure of Health. Soc. Theory Health 2018, 16, 256–271. [Google Scholar] [CrossRef]
- Felisbino-Mendes, M.S.; Cousin, E.; Malta, D.C.; Machado, I.E.; Ribeiro, A.L.P.; Duncan, B.B.; Schmidt, M.I.; Silva, D.A.S.; Glenn, S.; Afshin, A.; et al. The burden of non-communicable diseases attributable to high BMI in Brazil, 1990–2017: Findings from the Global Burden of Disease Study. Popul. Health Metr. 2020, 18, 18. [Google Scholar] [CrossRef]
- Lin, X.; Xu, Y.; Xu, J.; Pan, X.; Song, X.; Shan, L.; Zhao, Y.; Shan, P.F. Global burden of noncommunicable disease attributable to high body mass index in 195 countries and territories, 1990–2017. Endocrine 2020, 69, 310–320. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, L.; Qu, W. New national data show alarming increase in obesity and noncommunicable chronic diseases in China. Eur. J. Clin. Nutr. 2017, 71, 149–150. [Google Scholar] [CrossRef]
- Gahagan, J.; Gray, K.; Whynacht, A. Sex and gender matter in health research: Addressing health inequities in health research reporting. Int. J Equity Health 2015, 14, 12. [Google Scholar] [CrossRef] [PubMed]
- Alexander, S.; Hayes, S. Viewing Health Policy through a Gender Lens: Highlights from Several U.S. Communities. Womens Health Issues 2017, 27, S2–S5. [Google Scholar] [CrossRef] [PubMed]
- Brand, C.; Fochesatto, C.F.; Dias, A.F.; Gaya, A.R.; Martins, C.M.L.; Renner, J.D.P.; Reuter, C.P.; Kelishadi, R. Child’s body mass index and mother’s obesity: The moderating role of physical fitness. Eur. J. Pediatr. 2021, 180, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kubik, M.Y.; Fulkerson, J.A. Missed Work Among Caregivers of Children with a High Body Mass Index: Child, Parent, and Household Characteristics. J. Sch. Nurs. 2021, 37, 396–403. [Google Scholar] [CrossRef]
- Buscot, M.; Thomson, R.J.; Juonala, M.; Sabin, M.A.; Burgner, D.P.; Lehtimäki, T.; Hutri-Kähönen, N.; Viikari, J.S.A.; Jokinen, E.; Tossavainen, P.; et al. BMI Trajectories Associated with Resolution of Elevated Youth BMI and Incident Adult Obesity. Pediatrics 2018, 141, e20172003. [Google Scholar] [CrossRef]
- Huang, J.Y.; Qi, S.J. Childhood obesity and food intake. World J. Pediatr. 2015, 11, 101–107. [Google Scholar] [CrossRef]
- Andersen, C.J.; Murphy, K.E.; Fernandez, M.L. Impact of Obesity and Metabolic Syndrome on Immunity. Adv. Nutr. 2016, 7, 66–75. [Google Scholar] [CrossRef]
- Gomes, A.C.; Hoffmann, C.; Mota, J.F. The human gut microbiota: Metabolism and perspective in obesity. Gut Microbes 2018, 9, 308–325. [Google Scholar] [CrossRef]
- Mozaffarian, D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef]
- Piche, M.E.; Tchernof, A.; Despres, J.P. Obesity Phenotypes, Diabetes, and Cardiovascular Diseases. Circ. Res. 2020, 126, 1477–1500. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | 1990 | 2019 | 1990–2019 | ||
|---|---|---|---|---|---|
| Number of Deaths (95% UI) | ASDR per 100,000 (95% UI) | Number of Deaths (95% UI) | ASDR per 100,000 (95% UI) | EAPC of ASDR (95% CI) | |
| Breast cancer | 2191.12 (392.14–5324.64) | 0.26 (0.05–0.64) | 12,058.54 (3393.38–25,189.97) | 0.58 (0.16–1.22) | 2.94 (2.79–3.09) |
| Gallbladder and biliary tract cancer | 624.53 (142.68–1593.23) | 0.08 (0.02–0.21) | 3517.53 (1329.62–6901.31) | 0.18 (0.07–0.36) | 3.53 (3.07–3.98) |
| Multiple myeloma | 100.57 (18.39–261.68) | 0.01 (0.00–0.03) | 544.26 (169.31–1135.47) | 0.03 (0.01–0.06) | 2.92 (2.85–3.00) |
| Leukemia | 830.51 (160.30–2103.98) | 0.09 (0.02–0.22) | 2535.19 (919.85–5039.00) | 0.13 (0.05–0.26) | 1.54 (1.43–1.65) |
| Pancreatic cancer | 456.04 (78.27–1231.15) | 0.06 (0.01–0.15) | 4236.32 (1108.12–9601.90) | 0.21 (0.06–0.48) | 5.02 (4.80–5.24) |
| Ovarian cancer | 71.26 (−1.64–221.51) | 0.01 (0.00–0.03) | 571.41 (−13.46–1496.10) | 0.03 (0.00–0.07) | 4.36 (4.22–4.51) |
| Thyroid cancer | 106.51 (22.34–263.82) | 0.01 (0.00–0.03) | 536.33 (173.56–1120.49) | 0.03 (0.01–0.06) | 3.08 (2.88–3.27) |
| Non-Hodgkin lymphoma | 225.80 (45.16–598.83) | 0.03 (0.01–0.07) | 1593.08 (528.29–3315.29) | 0.08 (0.03–0.17) | 4.58 (4.31–4.86) |
| Kidney cancer | 275.97 (64.58–626.64) | 0.03 (0.01–0.08) | 2589.07 (1081.71–4699.44) | 0.13 (0.05–0.24) | 5.61 (5.13–6.09) |
| Liver cancer | 10,362.46 (1928.75–26,875.56) | 1.13 (0.21–2.98) | 18,964.67 (6165.35–40,278.41) | 0.93 (0.30–1.97) | −2.30 (−3.10 to −1.49) |
| Uterine cancer | 1222.16 (315.72–2618.43) | 0.14 (0.04–0.30) | 2967.44 (1305.70–5508.34) | 0.14 (0.06–0.27) | 0.36 (−0.26–0.98) |
| Esophageal cancer | 11,782.83 (1921.94–32,264.22) | 1.44 (0.23–3.96) | 36,180.91 (9426.32–79,605.50) | 1.80 (0.47–3.95) | 0.64 (0.15–1.13) |
| Colon and rectum cancer | 1817.51 (399.60–4351.24) | 0.22 (0.05–0.53) | 14,146.85 (5479.98–26,647.74) | 0.72 (0.28–1.36) | 4.64 (4.35–4.93) |
| Ischemic heart disease | 39,406.17 (9213.83–89,039.24) | 5.14 (1.18–12.02) | 203,608.68 (84,285.47–367,441.47) | 11.20 (4.53–20.83) | 3.39 (3.12–3.65) |
| Hypertensive heart disease | 31,034.85 (7085.40–70,850.56) | 4.89 (1.00–12.37) | 73,299.84 (28,352.47–142,307.78) | 4.41 (1.50–9.21) | −0.30 (−1.06–0.47) |
| Chronic kidney disease | 8450.27 (2079.25–18,788.22) | 1.08 (0.25–2.52) | 37,077.06 (15,764.13–65,371.62) | 1.94 (0.80–3.48) | 2.46 (2.29–2.64) |
| Gallbladder and biliary diseases | 1845.50 (427.84–4213.17) | 0.29 (0.07–0.67) | 3052.80 (1234.67–5627.09) | 0.19 (0.08–0.35) | −1.81 (−1.95 to −1.67) |
| Diabetes mellitus | 10,510.40 (2937.84–21,513.97) | 1.25 (0.34–2.60) | 47,529.62 (22,514.23–76,631.88) | 2.39 (1.12–3.90) | 2.40 (2.10–2.71) |
| Asthma | 2513.82 (548.84–6523.97) | 0.39 (0.08–1.04) | 3270.05 (1234.85–6226.72) | 0.19 (0.07–0.37) | −2.75 (−2.95 to −2.55) |
| Atrial fibrillation and flutter | 975.79 (209.46–2389.03) | 0.23 (0.05–0.59) | 5876.04 (2152.13–11,856.72) | 0.42 (0.15–0.86) | 1. 99(1.91–2.06) |
| Alzheimer’s disease and other dementias | 3530.64 (290.14–13,782.39) | 0.86 (0.07–3.26) | 23,787.11 (3263.72–78,659.44) | 1.67 (0.22–5.65) | 2.56 (2.46–2.66) |
| Stroke | 106,663.61 (25,825.88–233,294.20) | 12.17 (2.91–26.65) | 266,755.28 (119,930.67–453,820.00) | 13.15 (5.84–22.76) | 0.29 (0.07–0.50) |
| 1990 | 2019 | 1990–2019 | |||
|---|---|---|---|---|---|
| Characteristics | Number of DALYs (95% UI) | ASR-DALYs per 100,000 (95% UI) | Number of DALYs (95% UI) | ASR-DALYs per 100,000 (95% UI) | EAPC of ASDR (95% CI) |
| Breast cancer | 62,298.33 (11,393.67–150,486.60) | 6.83 (1.24–16.55) | 336,582.82 (93,778.62–680,213.61) | 15.25 (4.27–30.95) | 3.01 (2.83–3.19) |
| Gallbladder and biliary tract cancer | 16,054.25 (3730.29–40,845.03) | 1.82 (0.41–4.65) | 81,473.34 (31,251.45–157,724.94) | 3.95 (1.50–7.65) | 3.46 (3.00–3.91) |
| Multiple myeloma | 2828.46 (523.95–7429.59) | 0.30 (0.06–0.79) | 14,686.71 (4528.44–30,413.52) | 0.71 (0.22–1.47) | 3.01 (2.94–3.08) |
| Leukemia | 32,518.85 (6123.68–82,756.56) | 2.96 (0.57–7.46) | 84,302.69 (30,802.27–167,813.73) | 4.46 (1.61–8.86) | 1.41 (1.29–1.52) |
| Pancreatic cancer | 12,708.94 (2179.22–34,462.91) | 1.38 (0.23–3.71) | 106,354.05 (27,249.62–240,616.59) | 5.10 (1.31–11.54) | 4.91 (4.70–5.13) |
| Ovarian cancer | 2352.28 (−52.72–7378.61) | 0.24 (−0.01–0.75) | 16,701.07 (−398.19–43,257.40) | 0.78 (−0.02–2.06) | 4.17 (4.01–4.33) |
| Thyroid cancer | 3227.01 (681.69–7943.02) | 0.34 (0.07–0.84) | 14,811.37 (4838.85–30,476.19) | 0.73 (0.24–1.51) | 3.07 (2.90–3.23) |
| Non-Hodgkin lymphoma | 7343.51 (1462.21–19,494.52) | 0.74 (0.15–1.94) | 47,354.30 (16,139.48–99,616.69) | 2.34 (0.79–4.91) | 4.73 (4.45–5.01) |
| Kidney cancer | 8117.04 (1905.54–18,423.87) | 0.86 (0.20–1.95) | 70,543.60 (29,312.42–127,228.96) | 3.45 (1.44–6.26) | 5.71 (5.23–6.19) |
| Liver cancer | 339,787.93 (63,119.03–881,903.59) | 34.43 (6.37–89.39) | 570,373.28 (183,232.22–1,205,391.20) | 27.72 (8.88–58.69) | −2.40 (−3.24 to −1.56) |
| Uterine cancer | 38,377.85 (9763.96–83,099.05) | 4.00 (1.02–8.61) | 90,828.82 (40,885.43–166,471.87) | 4.31 (1.91–7.90) | 0.52 (−0.12–1.16) |
| Esophageal cancer | 306,708.88 (49,524.78–827,902.90) | 34.17 (5.61–93.35) | 859,654.43 (221,497.11–1,875,382.28) | 40.79 (10.61–88.68) | 0.46 (−0.06–0.98) |
| Colon and rectum cancer | 53,124.79 (11,759.47–127,188.90) | 5.68 (1.26–13.62) | 376,132.77 (149,260.15–689,707.75) | 18.45 (7.30–33.73) | 4.69 (4.39–4.98) |
| Ischemic heart disease | 1,183,843. 99(283,867.90–2,643,151.93) | 127.54 (30.11–286.07) | 5,073,254.14 (2,233,964.46–8,744,122.41) | 257.69 (112.34–447.18) | 2. 99(2.79–3.19) |
| Hypertensive heart disease | 727,467.32 (176,938.40–1,575,574.30) | 91.56 (21.30–208.35) | 1,514,532.28 (673,365.89–2,626,320.86) | 79.94 (34.45–145.14) | −0.43 (−1.10–0.25) |
| Chronic kidney disease | 297,281.58 (75,327.93–668,658.50) | 32.70 (8.15–73.76) | 1,200,356.40 (542,874.66–2,014,595.58) | 58.48 (26.44–98.96) | 2.66 (2.46–2.87) |
| Gallbladder and biliary diseases | 139,950.39 (32,647.51–342,137.02) | 15.12 (3.52–36.66) | 384,257.75 (158,489.35–746,026.51) | 19.26 (7.87–37.13) | 0.82 (0.68–0.96) |
| Diabetes mellitus | 771,801.60 (209,707.64–1,609,362.21) | 80.21 (21.50–167.40) | 3,737,575.96 (1,913,966.15–5,903,925.93) | 181.54 (93.71–286.33) | 3.11 (2.87–3.34) |
| Asthma | 98,457.09 (25,467.01–228,183.85) | 10.89 (2.69–26.17) | 175,324.55 (75,051.80–320,742.37) | 10.42 (4.61–18.60) | −0.78 (−1.12 to −0.44) |
| Atrial fibrillation and flutter | 40,270.29 (8841.24–97,699.67) | 6.03 (1.28–14.78) | 228,050.10 (88,026.96–445,218.48) | 12.30 (4.71–24.13) | 2.57 (2.47–2.67) |
| Alzheimer’s disease and other dementias | 72,968.85 (8730.45–252,707.00) | 13.17 (1.56–45.71) | 477,208.95 (101,059.42–1,388,765.94) | 28.22 (5.68–82.02) | 2.81 (2.75–2.88) |
| Stroke | 3,376,373.87 (849,026.71–7,253,492.17) | 351.82 (87.09–762.37) | 8,188,302.10 (3,891,288.26–13,434,158.41) | 397.52 (188.62–654.47) | 0.43 (0.26–0.60) |
| Low back pain | 155,486.15 (33,388.62–376,821.46) | 15.35 (3.33–36.83) | 460,684.90 (184,490.12–899,388.11) | 23.37 (9.16–45.50) | 2.12 (1.88–2.36) |
| Blindness and vision loss | 9122.33 (1860.75–23,629.60) | 1.29 (0.25–3.33) | 47,687.87 (15,902.11–101,631.30) | 2.50 (0.82–5.35) | 2.87 (2.50–3.23) |
| Gout | 18,679.84 (4002.65–47,522.96) | 1.94 (0.41–4.97) | 115,104.21 (44,197.45–231,849.93) | 5.64 (2.16–11.22) | 4.28 (4.08–4.49) |
| Osteoarthritis | 99,196.59 (16,850.73–280,351.94) | 10.94 (1.84–30.78) | 557,902.37 (165,070.11–1,343,750.30) | 25. 99(7.67–62.55) | 3.40 (3.26–3.54) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xiang, H.; Yang, R.; Tu, J.; Guan, X.; Tao, X. Health Impacts of High BMI in China: Terrible Present and Future. Int. J. Environ. Res. Public Health 2022, 19, 16173. https://doi.org/10.3390/ijerph192316173
Xiang H, Yang R, Tu J, Guan X, Tao X. Health Impacts of High BMI in China: Terrible Present and Future. International Journal of Environmental Research and Public Health. 2022; 19(23):16173. https://doi.org/10.3390/ijerph192316173
Chicago/Turabian StyleXiang, Hong, Runjuan Yang, Jiaxin Tu, Xi Guan, and Xufeng Tao. 2022. "Health Impacts of High BMI in China: Terrible Present and Future" International Journal of Environmental Research and Public Health 19, no. 23: 16173. https://doi.org/10.3390/ijerph192316173
APA StyleXiang, H., Yang, R., Tu, J., Guan, X., & Tao, X. (2022). Health Impacts of High BMI in China: Terrible Present and Future. International Journal of Environmental Research and Public Health, 19(23), 16173. https://doi.org/10.3390/ijerph192316173






