How Do Primary Care Organizations Rate Their Level of Organizational Health Literacy? Results of a Swiss Pilot-Study
Abstract
1. Introduction
2. Methods
2.1. The OHL Self-AsseT
2.2. Setting and Sample
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. OHL from an Individual Level Perspective
3.1.1. Socio-Demographic Characteristics
3.1.2. Knowledge of Relevant Health Literacy-Related Terms
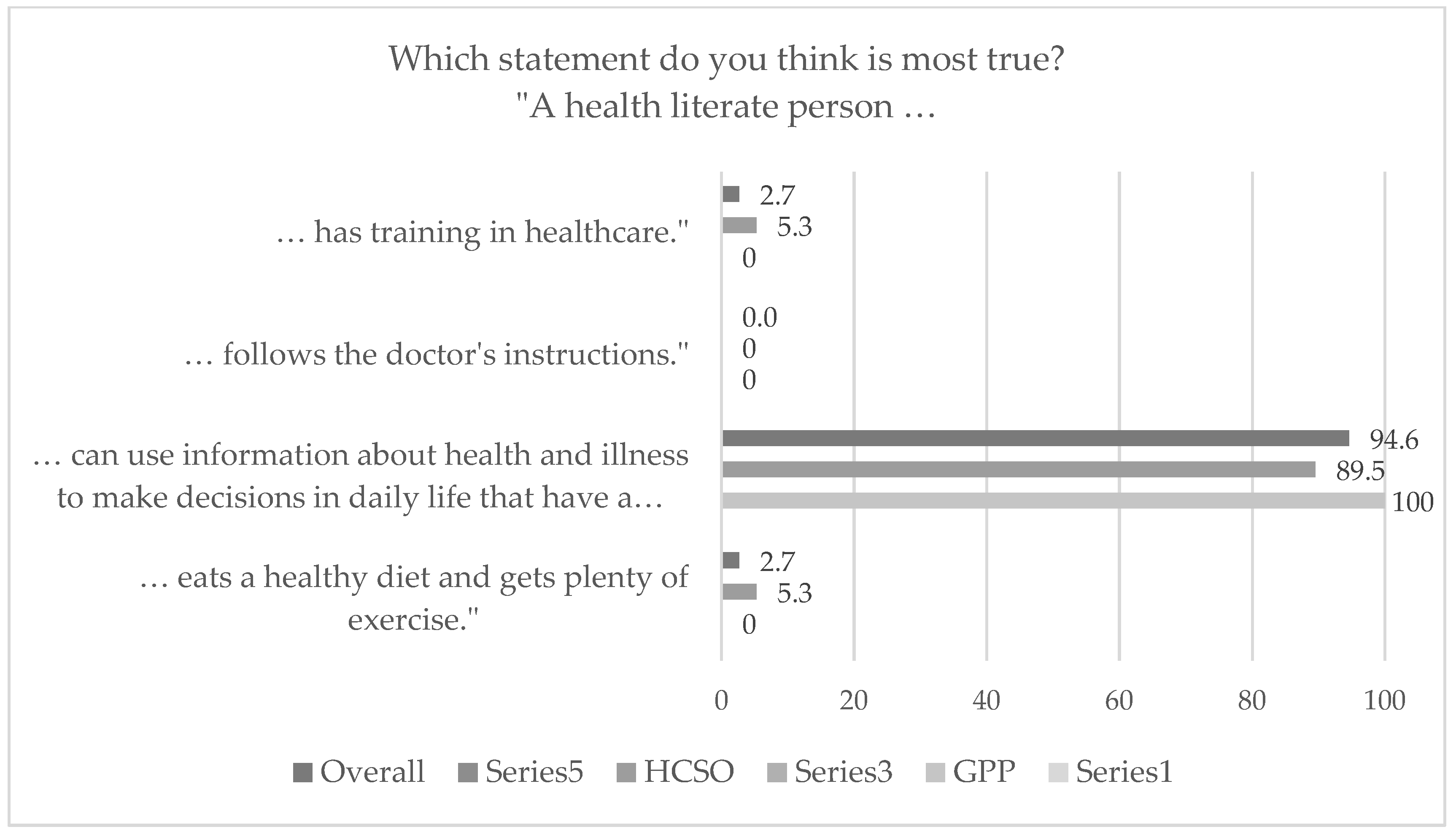
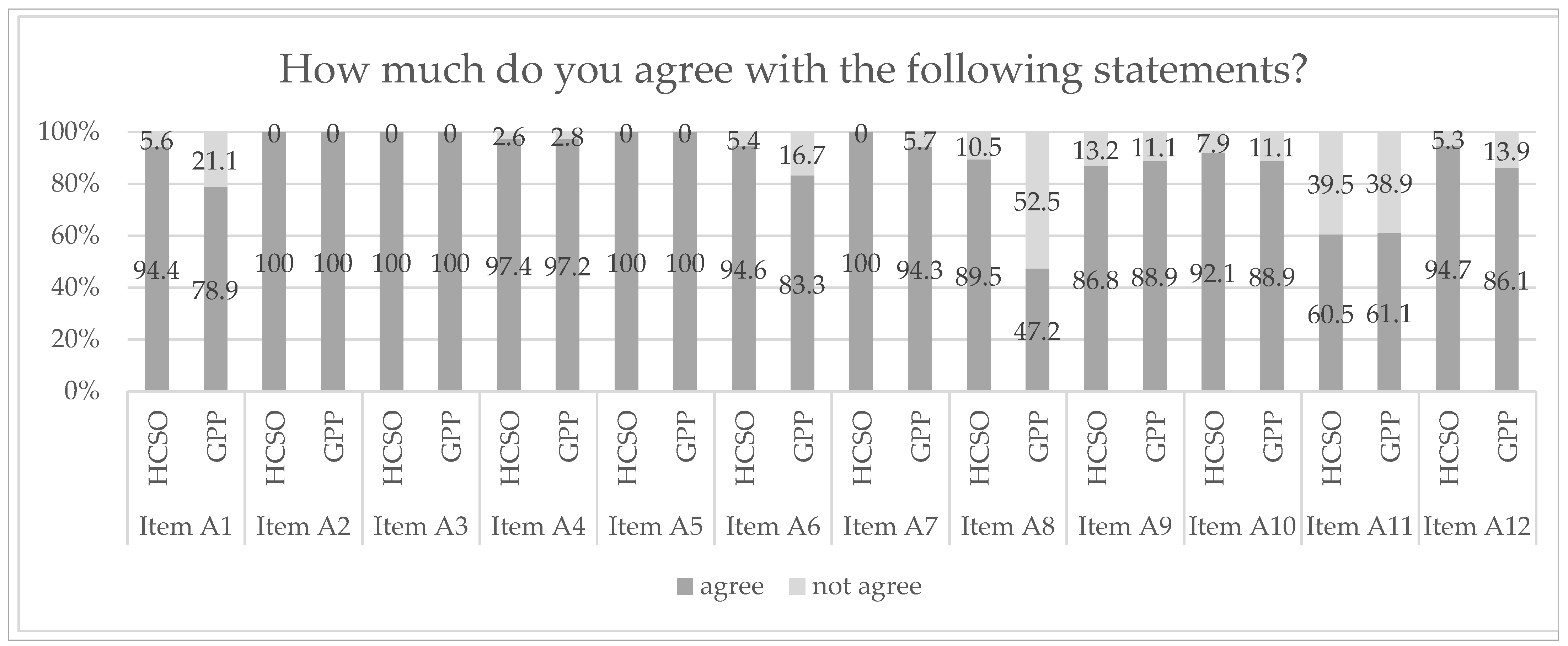
3.1.3. Knowledge of Health Literacy and Attitudes towards OHL
3.2. OHL from an Organizational Level Perspective
3.2.1. Primary Care Organizations Rating Their Level of OHL
3.2.2. Planned Measures to Promote and Strengthen Health Literacy
4. Discussion
4.1. Health Literacy—An (un)Familiar Concept in the Swiss Primary Care Setting?
4.2. Health Literacy as an Inherent Task of Primary Care Providers
4.3. The OHL Self-AsseT as a Tool to Support Health Literacy (Of Staff Members)
5. Limitations and Strengths
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sørensen, K.; Van Den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- de Gani, S.M.; Nowak-Flück, D.; Nicca, D.; Vogt, D. Self-Assessment Tool to Promote Organizational Health Literacy in Primary Care Settings in Switzerland. Int. J. Environ. Res. Public Health 2020, 17, 9497. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Trezona, A.; Levin-Zamir, D.; Kosir, U.; Nutbeam, D.; World Health Organization. Transforming health systems and societies by investing in health literacy policy and strategy. Public Health Panorama 2019, 5, 259–263. [Google Scholar]
- Nutbeam, D.; Levin-Zamir, D.; Rowlands, G. Health Literacy in Context. Int. J. Environ. Res. Public Health 2018, 15, 2657. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.; Kim, B.; Sacks, K. Health Literacy in the United States: Enhancing Assessments and Reducing Disparities; SSRN 4182046; SSRN: Rochester, NY, USA, 2022. [Google Scholar]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- The HLS19 Consortium of the WHO Action Network M-POHL. International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019–2021 (HLS19) of M-POHL; Austrian National Public Health Institute: Vienna, Austria, 2021. [Google Scholar]
- De Gani, S.M.; Jaks, R.; Bieri, U.; Kocher, J.P. Health Literacy Survey Schweiz 2019–2021; Schlussbericht im Auftrag des Bundesamtes für Gesundheit BAG: Zürich, Careum Stiftung, Switzerland, 2021. [Google Scholar]
- Farmanova, E.; Bonneville, L.; Bouchard, L. Organizational Health Literacy: Review of Theories, Frameworks, Guides, and Implementation Issues. Inquiry 2018, 55, 46958018757848. [Google Scholar] [CrossRef] [PubMed]
- Hersh, L.; Salzman, B.; Snyderman, D. Health literacy in primary care practice. Am. Fam. Physician 2015, 92, 118–124. [Google Scholar] [PubMed]
- Dewalt, D.A.; Callahan, L.F.; Hawk, V.H.; Broucksou, K.A.; Hink, A.; Rudd, R.; Brach, C. Health Literacy Universal Precautions Toolkit; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2010; pp. 1–227.
- Annarumma, C.; Palumbo, R. Contextualizing Health Literacy to Health Care Organizations. J. Health Manag. 2016, 18, 611–624. [Google Scholar] [CrossRef]
- Palumbo, R. Contextualizing co-production of health care: A systematic literature review. Int. J. Public Sect. Manag. 2016, 29, 72–90. [Google Scholar] [CrossRef]
- Parker, R. Measuring Health Literacy: What? So What? Now What? PowerPoint presentation at the Institute of Medicine workshop on measures of health literacy; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Stuermer, N.; De Gani, S.M.; Beese, A.-S.; Giovanoli Evack, J.; Jaks, R.; Nicca, D. Health Professionals’ Experience with the First Implementation of the Organizational Health Literacy Self-Assessment Tool for Primary Care (OHL Self-AsseT)—A Qualitative Reflexive Thematic Analysis. Int. J. Environ. Res. Public Health 2022, 19, 15916. [Google Scholar] [CrossRef]
- Greuter, S. Buurtzorg: Ganzheitliche Pflege, Made in the Netherlands; Denknetz: Zürich, Switzerland, 2018. [Google Scholar]
- Bieri, U.; Kocher, J.P.; Gauch, C.; Tschöppe, S.; Venetz, A.; Hagemann, M.; Schwab, J.; Schüpbach, S.; Frind, A. Bevölkerungsbefragung “Erhebung Gesundheits-Kompetenz 2015”: Schlussbericht; Gfs.bern: Bern, Switzerland, 2016. [Google Scholar]
- Groene, O.R.; Wills, J.; Crichton, N.; Rowlands, G.; Rudd, R.R. The health literacy dyad the contribution of future GPs in England. Educ. Prim. Care 2017, 28, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Nutbeam, D.; Lloyd, J.E. Understanding and Responding to Health Literacy as a Social Determinant of Health. Annu. Rev. Public Health 2021, 42, 159–173. [Google Scholar] [CrossRef] [PubMed]
- WHO Regional Office for Europe. Health Literacy in the Context of Health, Well-Being and Learning Outcomes—The Case of Children and Adolescents in Schools; Concept paper; WHO: Copenhagen, Denmark, 2021. [Google Scholar]
- Zängl, P.; Enrico, C. Übertragung des Buurtzorg-Modells auf Schweizerische Verhältnisse; FHNW: Olten, Switzerland, 2019. [Google Scholar]
- Gray, B.H.; Sarnak, D.O.; Burgers, J.S. Home Care by Self-Governing Nursing Teams: The Netherlands’ Buurtzorg Model; Commonwealth Fund: NewYork, NY, USA, 2015. [Google Scholar]
- Brunnschweiler, C. Spitex-Fachtagung 2019 «Die Zukunft ist Heute—Neue Versorgungsmodelle»; Spitex Schweiz: Bern, Switzerland, 2019. [Google Scholar]
- Reynolds, A. Patient-centered Care. Radiol. Technol. 2009, 81, 133–147. [Google Scholar] [PubMed]
- Kickbusch, I.; Pelikan, J.M.; Apfel, F.; Tsouros Agis, D. Health Literacy. The Solid Facts; World Health Organization: Copenhagen, Denmark, 2013; ISBN 978 92 890 00154. [Google Scholar]
- Okan, O.; Bauer, U.; Levin-Zamir, D.; Pinheiro, P.; Sørensen, K. (Eds.) International Handbook of Health Literacy: Research, Practice and Policy Across the Lifespan; Policy Press: Bristol, UK, 2019. [Google Scholar]
- Faragher, E.B.; Cass, M.; Cooper, C.L. The relationship between job satisfaction and health: A meta-analysis. Stress Wellbeing 2013, 1, 254–271. [Google Scholar]
- Black, D.C. Why healthcare organisations must look after their staff. Nurs. Manag. 2012, 19, 27. [Google Scholar] [CrossRef] [PubMed]
- Barker, P.M.; Reid, A.; Schall, M.W. A framework for scaling up health interventions: Lessons from large-scale improvement initiatives in Africa. Implement. Sci. 2016, 11, 12. [Google Scholar] [CrossRef] [PubMed]


| Level | Timepoint | Method | Sample |
|---|---|---|---|
| Individual level | Prior to the intervention | Online survey | 74 health professionals |
| Organizational level | During the intervention | Checklist (i.e., module 2 of the OHL Self-AsseT 1) Intervention documentation | 10 teams (six teams from the HCSO and four GPPs) |
| Sample Characteristics | HCSO N = 38 (%) | GPP N = 36 (%) | Overall N = 74 (%) | |
|---|---|---|---|---|
| Gender, n (%) | Male | 1 (2.6) | 5 (14.0) | 6 (8.1) |
| Female | 37 (97.4) | 31 (86.0) | 68 (91.9) | |
| Age, n (%) | Younger than 20 years | 1 (2.6) | 4 (11.0) | 5 (6.8) |
| Between 20 and 40 years | 11 (28.9) | 22 (61.0) | 33 (44.6) | |
| Between 41 and 65 years | 26 (68.4) | 9 (25.0) | 35 (47.3) | |
| Older than 65 years | 0 (0.0) | 1 (3.0) | 1 (1.4) | |
| Function GPP 1, n (%) | Medical doctor | - | 9 (25.0) | - |
| Practice manager | - | 1 (2.8) | - | |
| Medical practice assistant (MPA) | - | 23 (63.9) | - | |
| Apprentice | - | 2 (5.6) | - | |
| Not specified | - | 4 (11.1) | - | |
| Function HCSO 1, n (%) | Nursing specialist | 11 (28.9) | - | - |
| Healthcare specialist | 9 (23.7) | - | - | |
| Home nurse | 4 (10.5) | - | - | |
| Nursing assistant Swiss Red Cross | 8 (21.1) | - | - | |
| Housekeeping assistant | 9 (23.7) | - | - | |
| Apprentice | 1 (2.6) | - | - | |
| Not specified | 4 (10.5) | - | - | |
| Managing function, n (%) | Yes | 2 (5.3) | 13 (36.0) | 15 (20.3) |
| No | 35 (92.1) | 23 (64.0) | 58 (78.4) | |
| Not specified | 1 (2.6) | 1 (1.4) | ||
| FTE, n (%) | From 0% to 40% | 1 (2.6) | 1 (2.8) | 2 (2.7) |
| Between 41% and 60% | 6 (15.8) | 8 (22.2) | 14 (18.9) | |
| Between 61% and 80% | 20 (52.6) | 6 (16.7) | 26 (35.1) | |
| More than 80% | 11 (28.9) | 20 (55.6) | 31 (41.9) | |
| Not specified | 0 (0.0) | 1 (2.8) | 1 (1.4) | |
| Years in the organization, n (%) | Less than 2 years | 11 (28.9) | 7 (19.4) | 18 (24.3) |
| Between 2 and 5 years | 7 (18.4) | 16 (44.4) | 23 (31.1) | |
| Between 6 and 10 years | 5 (13.2) | 8 (22.2) | 13 (17.6) | |
| More than 10 years | 15 (39.5) | 5 (13.9) | 20 (27.0) | |
| Work experience, n (%) | Still in training | 1 (2.6) | 2 (5.6) | 3 (4.1) |
| Less than 5 years | 5 (13.2) | 5 (13.9) | 10 (13.5) | |
| Between 5 and 14 years | 13 (34.2) | 19 (52.8) | 32 (43.2) | |
| Between 15 and 25 years | 8 (21.1) | 7 (19.4) | 15 (20.3) | |
| More than 25 years | 8 (21.1) | 3 (8.3) | 11 (14.9) | |
| Not specified | 3 (7.9) | 0 (0.0) | 3 (4.1) |
| No. | Which Statements Do You Think Apply to the Swiss Population? | HCSO (N = 38) | GPP (N = 36) | Overall (N = 74) | |||
|---|---|---|---|---|---|---|---|
| True | False | True | False | True | False | ||
| 1 | Dealing with health information is difficult for most of the population *. (true) | 52.6% | 47.4% | 75% | 25% | 63.5% | 36.5% |
| 2 | More than half of the population finds it difficult to assess the advantages and disadvantages of treatments. (true) | 76.3% | 23.7% | 75% | 25% | 75.7% | 24.3% |
| 3 | For many individuals, it is easy to assess how trustworthy health information in the media is *. (false) | 39.5% | 60.5% | 5.6% | 94.4% | 23% | 77% |
| 4 | It is particularly difficult for older people to deal with information on health and illness *. (true) | 94.7% | 5.3% | 66.7% | 33.3% | 81.1% | 18.9% |
| 5 | Individuals with higher health literacy rate their health status more positively. (true) | 68.4% | 31.6% | 80.6% | 19.4% | 74.3% | 25.7% |
| 6 | Individuals with higher health literacy are less likely to go to the doctor. (true) | 63.2% | 36.8% | 77.8% | 22.2% | 70.3% | 29.7% |
| 7 | Individuals with higher levels of education find it easier to understand information about health and illness. (true) | 76.3% | 23.7% | 63.9% | 36.1% | 70.3% | 29.7% |
| Dimensions of a Health Literate Organization | HCSO (N = 6) in % | GPP (N = 4) in % | Overall (N = 10) in % | |||
|---|---|---|---|---|---|---|
| M 1 | SD 1 | M | SD | M | SD | |
| 1. Provide easy access to primary care service and facilitate navigation within | 65.9 | 6 | 84.5 | 6 | 73.3 | 11 |
| 1.1 Contact (5 items) | 74.5 | 12 | 88.3 | 7 | 80.0 | 12 |
| 1.2 Navigation within the primary care service (2 items) | 44.5 | 12 | 75.0 | 8 | 56.7 | 19 |
| 2. Communicating in plain and easy-to-understand language | 74.3 | 13 | 75.0 | 9 | 74.6 | 12 |
| 2.1 Oral communication (9 items) | 74.7 | 16 | 75.9 | 4 | 75.2 | 13 |
| 2.2 Written communication (7 items) | 73.8 | 14 | 73.8 | 15 | 73.8 | 15 |
| 3. Promoting health literacy of our users | 76.4 | 18 | 73.6 | 14 | 75.3 | 16 |
| 3.1 Empowering our users to use health information (4 items) | 82.0 | 23 | 75.0 | 17 | 79.2 | 21 |
| 3.2 Promoting an active role and self-management of our users (8 items) | 73.6 | 17 | 72.9 | 16 | 73.3 | 17 |
| 4. Promoting health literacy of staff members | 58.9 | 11 | 60.6 | 18 | 59.6 | 14 |
| 4.1 Know-how and professional competence (3 items) | 79.6 | 23 | 58.3 | 32 | 71.1 | 29 |
| 4.2 Personnel development (10 items) | 52.2 | 19 | 57.5 | 18 | 54.3 | 19 |
| 4.3 Staff members’ health (2 items) | 61.1 | 18 | 79.2 | 14 | 68.3 | 19 |
| 5. Incorporating health literacy into the management and organizational structure | 73.5 | 14 | 65.6 | 9 | 70.3 | 13 |
| 5.1 Health literacy as an organizational responsibility (4 items) | 80.6 | 15 | 52.1 | 15 | 69.2 | 20 |
| 5.2 Health literacy as a development goal (4 items) | 66.7 | 10 | 70.8 | 7 | 68.3 | 9 |
| 5.3 Organizational culture (4 items) | 75.9 | 17 | 68.8 | 14 | 73.1 | 15 |
| 5.4 User involvement—feedback (4 items) | 71.3 | 22 | 70.8 | 14 | 71.1 | 19 |
| 6. Promoting health literacy at care interfaces, networks and further activities of the organization | 66.2 | 11 | 73.2 | 11 | 69.0 | 12 |
| 6.1 Care interfaces (3 items) | 93.5 | 7 | 69.5 | 12 | 83.9 | 15 |
| 6.2 Networking and further activities (6 items) | 50.0 | 14 | 75.7 | 11 | 60.3 | 18 |
| All dimensions (75 items) | 69.2 | 6 | 72.1 | 8 | 70.3 | 5 |
| OHL Dimension | Planned Measures by Self-Assessment Teams of the GPPs | Planned Measures by Self-Assessment Teams of the HCSO | Overall No. of Planned Improvement Measures |
|---|---|---|---|
| 1. Provide easy access to primary care service and facilitate navigation within | “Labeling access for the underground parking lot” (GPP-1) | “At the inter-disciplinary meeting, a responsible person is appointed to create the labels for the premises/activities” (HCSO-3) | 8 |
| “Homepage will be adapted by external administrator after team discussion” (GPP-2) | “[Name] is in contact with the housekeeper. We will receive an update after two weeks on how to best improve measures to provide easy access” (HCSO-4) | ||
| “We create a pictogram and hang it on the wall in front of the toilet to make it clearly visible from all angles where the toilet is located” (GPP-3) | “Improve the forwarding to the department, which is responsible for health literacy issues (within the center)” (HCSO-6) | ||
| “We will contact tele-search, since entry of the tele-search platform is not correct” (GPP-4) | “Hand out flyer to medical doctors for people with dementia” (HCSO-6) | ||
| 2. Communicating in plain and easy-to-understand language | “Internal training at team meetings by medical doctors” (GPP-1) | “Implementation and usage of the measurements are being evaluated at the summer meeting in 2021” (HCSO-3) | 5 |
| “Internal forms are distributed to MPAs and processed. After approval by the medical doctors, the forms will be used more frequently again” (GPP-2) | |||
| “Create guideline and file it in the practice manual for everyone to refer to” (GPP-3) | |||
| “Restock brochures and draft fact sheets” (GPP-4) | |||
| 3. Promoting health literacy of users | “Communicate existing information more actively to patients” (GPP-1) | “Recruiting another PH staff member so that all HW clients have a reference person” (HCSO-2) | 5 |
| “Plan information event/open day in cooperation with partner organizations, e.g., HCSO” (GPP-1) | “Create an information folder on health literacy and store it in the team office, accessible to every staff member” (HCSO-6) | ||
| “In December, we will plan a patient consultation on the subject of diabetes” (GPP-2) | |||
| 4. Promoting health literacy of staff members | “Guidelines by medical doctors including evidence-based sources of information” (GPP-2) | “The topic of health literacy was forwarded to the management level. More information will follow” (HCSO-2) | 9 |
| “Defining creditable sources at the meeting with the CEO, so everyone shares the same information with patients” (GPP-3) | “Each staff member can provide an input on OHL. Every two months there will be a technical input. Start in January 2021” (HCSO-3) | ||
| “Providing guidelines on our internal digital platform, implementation in team meetings” (HCSO-4) | |||
| “Adapting staff communication guidelines” (GPP-4) | “Include a health literacy refresher in our team meeting, where a staff member introduces a specific topic. In each team meeting, it is re-determined what topic will be discussed next time and who will present it” (HCSO-6) | ||
| “Work supervision has already taken place, improving feedback culture” (HCSO-6) | |||
| “Case discussions are considered to take place twice a year” (HCSO-6) | |||
| 5. Incorporating health literacy into the management and organizational structure | “Demonstrating practices 1:1, viewed by MPA and management” (GPP-4) | “We regularly discuss the topic of staying healthy and strengthening one’s own health in sessions. To do this, we use the battery method from 0 to 10 and regularly reflect on our own health status to support each other” (HCSO-1) | 2 |
| 6. Promoting health literacy at care interfaces, networks and further activities of the organization | “Providing a link list on the homepage and an overview list with relevant links for staff members” (GPP-4) | “We organize a training for our team to improve health literate communication in the organization” (HCSO-1) | 4 |
| “Someone from the center or organizational development department will be appointed to take part in the reports and pass on feedback/information to the other teams” (HCSO-3) | |||
| “Increase participation at organizational offers regarding health literacy from 2021 onwards” (HCSO-3) | |||
| All dimensions | 33 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beese, A.-S.; Nicca, D.; Jaks, R.; Stuermer, N.; De Gani, S.M. How Do Primary Care Organizations Rate Their Level of Organizational Health Literacy? Results of a Swiss Pilot-Study. Int. J. Environ. Res. Public Health 2022, 19, 16139. https://doi.org/10.3390/ijerph192316139
Beese A-S, Nicca D, Jaks R, Stuermer N, De Gani SM. How Do Primary Care Organizations Rate Their Level of Organizational Health Literacy? Results of a Swiss Pilot-Study. International Journal of Environmental Research and Public Health. 2022; 19(23):16139. https://doi.org/10.3390/ijerph192316139
Chicago/Turabian StyleBeese, Anna-Sophia, Dunja Nicca, Rebecca Jaks, Natascha Stuermer, and Saskia Maria De Gani. 2022. "How Do Primary Care Organizations Rate Their Level of Organizational Health Literacy? Results of a Swiss Pilot-Study" International Journal of Environmental Research and Public Health 19, no. 23: 16139. https://doi.org/10.3390/ijerph192316139
APA StyleBeese, A.-S., Nicca, D., Jaks, R., Stuermer, N., & De Gani, S. M. (2022). How Do Primary Care Organizations Rate Their Level of Organizational Health Literacy? Results of a Swiss Pilot-Study. International Journal of Environmental Research and Public Health, 19(23), 16139. https://doi.org/10.3390/ijerph192316139





