Long COVID Classification: Findings from a Clustering Analysis in the Predi-COVID Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clustering and Statistical Analysis
3. Results
3.1. Population Study Characteristics
3.2. Clusters
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ballering, A.V.; van Zon, S.K.R.; Hartman, T.C.O.; Rosmalen, J.G.M.; Lifelines Corona Research Initiative. Persistence of somatic symptoms after COVID-19 in the Netherlands: An observational cohort study. Lancet 2022, 400, 452–461. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Disease (COVID-19): Post COVID-19 Condition. Available online: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition (accessed on 21 October 2022).
- World Health Organization. A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus, 6 October 2021. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (accessed on 29 September 2022).
- Carfì, A.; Bernabei, R.; Landi, F. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Halpin, S.J.; McIvor, C.; Whyatt, G.; Adams, A.; Harvey, O.; McLean, L.; Walshaw, C.; Kemp, S.; Corrado, J.; Singh, R.; et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J. Med. Virol. 2021, 93, 1013–1022. [Google Scholar] [CrossRef] [PubMed]
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef] [PubMed]
- Tenforde, M.W.; Kim, S.S.; Lindsell, C.J.; Rose, E.B.; Shapiro, N.I.; Files, D.C.; Gibbs, K.W.; Erickson, H.L.; Steingrub, J.S.; Smithline, H.A.; et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network—United States, March–June 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 993–998. [Google Scholar] [CrossRef] [PubMed]
- Ziauddeen, N.; Gurdasani, D.; O’Hara, M.E.; Hastie, C.; Roderick, P.; Yao, G.; Alwan, N.A. Characteristics and impact of Long Covid: Findings from an online survey. PLoS ONE 2022, 17, e0264331. [Google Scholar] [CrossRef] [PubMed]
- Amenta, E.M.; Spallone, A.; Rodriguez-Barradas, M.C.; El Sahly, H.M.; Atmar, R.L.; Kulkarni, P. Postacute COVID-19: An Overview and Approach to Classification. Open Forum Infect. Dis. 2020, 7, ofaa509. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Zhang, L.; Elbéji, A.; Wilmes, P.; Oustric, P.; Staub, T.; Nazarov, P.V.; Ollert, M.; Fagherazzi, G. Long COVID Symptomatology After 12 Months and Its Impact on Quality of Life According to Initial Coronavirus Disease 2019 Disease Severity. Open Forum Infect. Dis. 2022, 9, ofac397. [Google Scholar] [CrossRef] [PubMed]
- Fernández-De-Las-Peñas, C.; Martín-Guerrero, J.D.; Florencio, L.L.; Navarro-Pardo, E.; Rodríguez-Jiménez, J.; Torres-Macho, J.; Pellicer-Valero, O.J. Clustering analysis reveals different profiles associating long-term post-COVID symptoms, COVID-19 symptoms at hospital admission and previous medical co-morbidities in previously hospitalized COVID-19 survivors. Infection 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kenny, G.; McCann, K.; O’Brien, C.; Savinelli, S.; Tinago, W.; Yousif, O.; Lambert, J.S.; O’Broin, C.; Feeney, E.R.; De Barra, E.; et al. Identification of Distinct Long COVID Clinical Phenotypes Through Cluster Analysis of Self-Reported Symptoms. Open Forum Infect. Dis. 2022, 9, ofac060. [Google Scholar] [CrossRef] [PubMed]
- Fagherazzi, G.; Fischer, A.; Betsou, F.; Vaillant, M.; Ernens, I.; Masi, S.; Mossong, J.; Staub, T.; Brault, D.; Bahlawane, C.; et al. Protocol for a prospective, longitudinal cohort of people with COVID-19 and their household members to study factors associated with disease severity: The Predi-COVID study. BMJ Open 2020, 10, e041834. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health (NIH). COVID-19 Treatment Guidelines, Clinical Spectrum of SARS-CoV-2 Infection. 2021. Available online: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/ (accessed on 2 March 2022).
- Capelle, C.M.; Ciré, S.; Domingues, O.; Ernens, I.; Hedin, F.; Fischer, A.; Snoeck, C.J.; Ammerlaan, W.; Konstantinou, M.; Grzyb, K.; et al. Combinatorial analysis reveals highly coordinated early-stage immune reactions that predict later antiviral immunity in mild COVID-19 patients. Cell Rep. Med. 2022, 3, 100600. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Ninot, G.; Soyez, F.; Préfaut, C. A short questionnaire for the assessment of quality of life in patients with chronic obstructive pulmonary disease: Psychometric properties of VQ11. Health Qual. Life Outcomes 2013, 11, 179. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 30 October 2022).
- Gómez-Rubio, V. ggplot2—Elegant Graphics for Data Analysis (2nd Edition). J. Stat. Softw. 2017, 77, 1–3. [Google Scholar] [CrossRef]
- Reese, J.; Blau, H.; Bergquist, T.; Loomba, J.J.; Callahan, T.; Laraway, B.; Antonescu, C.; Casiraghi, E.; Coleman, B.; Gargano, M.; et al. Generalizable Long COVID Subtypes: Findings from the NIH N3C and RECOVER Programs. medRxiv. 2022. [Google Scholar] [CrossRef]
- Antonelli, M.; Pujol, J.C.; Spector, T.D.; Ourselin, S.; Steves, C.J. Risk of long COVID associated with delta versus omicron variants of SARS-CoV-2. Lancet 2022, 399, 2263–2264. [Google Scholar] [CrossRef] [PubMed]
- Morioka, S.; Tsuzuki, S.; Suzuki, M.; Terada, M.; Akashi, M.; Osanai, Y.; Kuge, C.; Sanada, M.; Tanaka, K.; Maruki, T.; et al. Post COVID-19 condition of the Omicron variant of SARS-CoV-2. J. Infect Chemother. 2022, 28, 1546–1551. [Google Scholar] [CrossRef] [PubMed]
- Taquet, M.; Sillett, R.; Zhu, L.; Mendel, J.; Camplisson, I.; Dercon, Q.; Harrison, P.J. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: An analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry 2022, 9, 815–827. [Google Scholar] [CrossRef] [PubMed]

| Overall Population N = 288 | Cluster-Mild N = 139 (48.26%) | Cluster-Moderate N = 106 (36.81%) | Cluster-Severe N = 43 (14.93%) | p-Value * | ||
|---|---|---|---|---|---|---|
| Sociodemographic Characteristics and Initial Severity Classification | Female N (%) | 170 (59%) | 73 (53%) | 66 (62%) | 31 (72%) | 0.053 |
| Age (Years) | 43 ± 12 | 42 ± 12 | 43 ± 12 | 45 ± 14 | 0.360 | |
| Body Mass Index (kg/m2) | 26.4 ± 5.5 | 25.8 ± 5.1 | 27.0 ± 5.8 | 26.7 ± 5.7 | 0.224 | |
| Smoker N (%) | 45 (16%) | 16 (12%) | 15 (14%) | 14 (33%) | 0.027 | |
| Moderate/severe illness N (%) | 95 (33%) | 34 (24%) | 41 (39%) | 20 (47%) | 0.015 | |
| Comorbidities | At least one comorbidity N (%) | 40 (14%) | 12 (8.6%) | 16 (15%) | 12 (28%) | 0.007 |
| Number of comorbidities Mean (SD) | 2.38 ± 0.33 | 2.37 ± 0.25 | 2.34 ± 0.16 | 2.48 ± 0.68 | 0.001 | |
| Hypertension N (%) | 38 (13%) | 14 (10%) | 12 (11%) | 12 (28%) | 0.015 | |
| Cardiac diseases N (%) | 11 (3.8%) | 3 (2.2%) | 6 (5.7%) | 2 (4.7%) | 0.311 | |
| Asthma N (%) | 14 (4.9%) | 4 (2.9%) | 8 (7.5%) | 2 (4.7%) | 0.200 | |
| Diabetes N (%) | 13 (4.5%) | 3 (2.2%) | 4 (3.8%) | 6 (14%) | 0.009 | |
| Symptoms at inclusion N (%) | Fever | 98 (34%) | 45 (32%) | 36 (34%) | 17 (40%) | 0.688 |
| Cough | 96 (33%) | 41 (29%) | 38 (36%) | 17 (40%) | 0.362 | |
| Cough sputum | 27 (9.4%) | 11 (7.9%) | 9 (8.5%) | 7 (16%) | 0.279 | |
| Sore throat | 50 (17%) | 17 (12%) | 24 (23%) | 9 (21%) | 0.076 | |
| Rhinorrhea | 76 (26%) | 35 (25%) | 31 (29%) | 10 (23%) | 0.708 | |
| Earache | 22 (7.6%) | 8 (5.8%) | 10 (9.4%) | 4 (9.3%) | 0.490 | |
| Chest pain | 19 (6.6%) | 4 (2.9%) | 11 (10%) | 4 (9.3%) | 0.036 | |
| Myalgia | 51 (18%) | 11 (7.9%) | 28 (26%) | 12 (28%) | <0.001 | |
| Arthralgia | 25 (8.7%) | 4 (2.9%) | 14 (13%) | 7 (16%) | 0.001 | |
| Fatigue | 136 (47%) | 47 (34%) | 60 (57%) | 29 (67%) | <0.001 | |
| Dyspnea | 33 (11%) | 10 (7.2%) | 16 (15%) | 7 (16%) | 0.067 | |
| Cephalea | 77 (27%) | 27 (19%) | 36 (34%) | 14 (33%) | 0.022 | |
| Abdominal pain | 14 (4.9%) | 4 (2.9%) | 3 (2.8%) | 7 (16%) | 0.004 | |
| Nausea | 13 (4.5%) | 5 (3.6%) | 4 (3.8%) | 4 (9.3%) | 0.289 | |
| Diarrhea | 20 (6.9%) | 5 (3.6%) | 8 (7.5%) | 7 (16%) | 0.019 | |
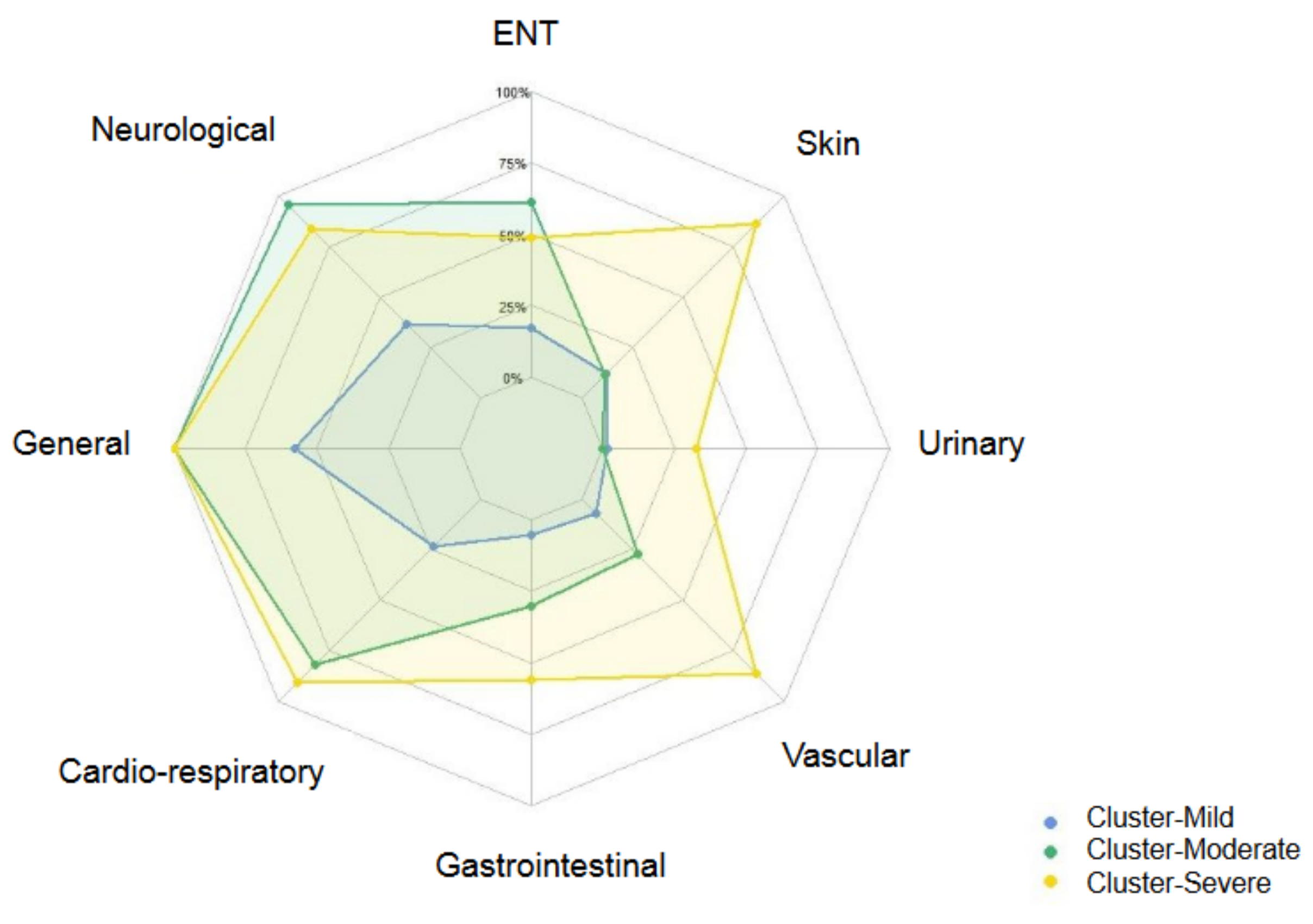
| Persisting symptoms at 12 months N (%) | Ear Nose Throat (ENT) symptoms | 110 (38%) | 24 (17%) | 65 (61%) | 21 (49%) | <0.001 |
| Neurological symptoms | 188 (65%) | 51 (37%) | 101 (95%) | 36 (84%) | <0.001 | |
| General symptoms | 229 (80%) | 80 (58%) | 106 (100%) | 43 (100%) | <0.001 | |
| Cardiorespiratory symptoms | 159 (55%) | 33 (24%) | 87 (82%) | 39 (91%) | <0.001 | |
| Gastrointestinal symptoms | 63 (22%) | 7 (5.0%) | 32 (30%) | 24 (56%) | <0.001 | |
| Vascular symptoms | 76 (26%) | 10 (7.2%) | 29 (27%) | 37 (86%) | <0.001 | |
| Urinary symptoms | 16 (5.6%) | 2 (1.4%) | 0 (0%) | 14 (33%) | <0.001 | |
| Skin symptoms | 66 (23%) | 17 (12%) | 12 (11%) | 37 (86%) | <0.001 | |
| Number of persisting symptoms at 12 months Mean (SD) | Total number of symptoms | 8 ± 8 | 2.89 ± 2.15 | 11.5 ± 5.7 | 18 ± 9 | <0.001 |
| Number ENT symptoms | 0.70 ± 1.11 | 0.25 ± 0.63 | 1.12 ± 1.24 | 1.09 ± 1.44 | 0.079 | |
| Number neurological symptoms | 2.12 ± 2.28 | 0.72 ± 1.27 | 3.27 ± 2.07 | 3.79 ± 2.63 | <0.001 | |
| Number general symptoms | 3.02 ± 2.86 | 1.19 ± 1.48 | 4.04 ± 2.30 | 6.44 ± 3.13 | <0.001 | |
| Number cardiorespiratory symptoms | 1.36 ± 1.72 | 0.42 ± 0.92 | 2.02 ± 1.65 | 2.81 ± 2.11 | 0.002 | |
| Number gastrointestinal symptoms | 0.39 ± 0.87 | 0.079 ± 0.382 | 0.48 ± 0.86 | 1.19 ± 1.35 | 0.010 | |
| Number vascular symptoms | 0.39 ± 0.75 | 0.09 ± 0.33 | 0.41 ± 0.73 | 1.35 ± 0.95 | 0.356 | |
| Number urinary symptoms | 0.07 ± 0.32 | 0.01 ± 0.11 | 0.00 ± 0.00 | 0.44 ± 0.70 | 0.610 | |
| Number skin symptoms | 0.27 ± 0.54 | 0.14 ± 0.38 | 0.13 ± 0.39 | 1.05 ± 0.62 | 0.570 | |
| Quality of life N (%) | Could not envisage coping with symptoms long term | 45 (16%) | 11 (7.9%) | 24 (23%) | 10 (23%) | 0.002 |
| Poor sleep # | 239 (83%) | 102 (73%) | 99 (93%) | 38 (88%) | <0.001 | |
| Altered respiratory quality of life at 1 year | 81 (28%) | 8 (5.8%) | 51 (48%) | 22 (51%) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fischer, A.; Badier, N.; Zhang, L.; Elbéji, A.; Wilmes, P.; Oustric, P.; Benoy, C.; Ollert, M.; Fagherazzi, G. Long COVID Classification: Findings from a Clustering Analysis in the Predi-COVID Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 16018. https://doi.org/10.3390/ijerph192316018
Fischer A, Badier N, Zhang L, Elbéji A, Wilmes P, Oustric P, Benoy C, Ollert M, Fagherazzi G. Long COVID Classification: Findings from a Clustering Analysis in the Predi-COVID Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(23):16018. https://doi.org/10.3390/ijerph192316018
Chicago/Turabian StyleFischer, Aurélie, Nolwenn Badier, Lu Zhang, Abir Elbéji, Paul Wilmes, Pauline Oustric, Charles Benoy, Markus Ollert, and Guy Fagherazzi. 2022. "Long COVID Classification: Findings from a Clustering Analysis in the Predi-COVID Cohort Study" International Journal of Environmental Research and Public Health 19, no. 23: 16018. https://doi.org/10.3390/ijerph192316018
APA StyleFischer, A., Badier, N., Zhang, L., Elbéji, A., Wilmes, P., Oustric, P., Benoy, C., Ollert, M., & Fagherazzi, G. (2022). Long COVID Classification: Findings from a Clustering Analysis in the Predi-COVID Cohort Study. International Journal of Environmental Research and Public Health, 19(23), 16018. https://doi.org/10.3390/ijerph192316018






