Narrative Review of the COVID-19 Pandemic’s First Two Years in Italy
Abstract
1. Introduction
2. Materials and Methods
3. Results
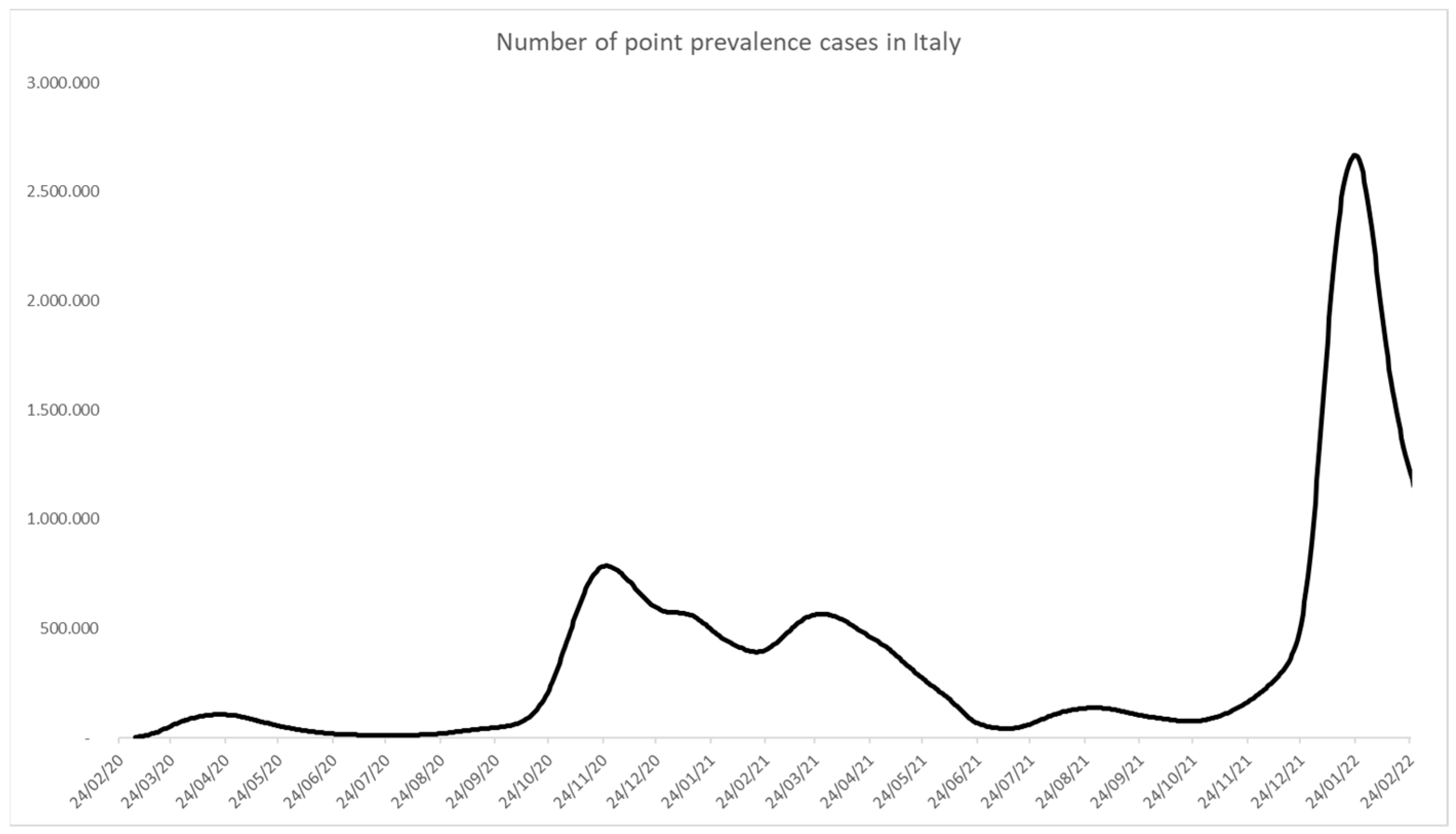
3.1. Framing of Epidemic Waves
3.2. Towards the Lockdown
3.3. Organizational Changes in the First Pandemic Year
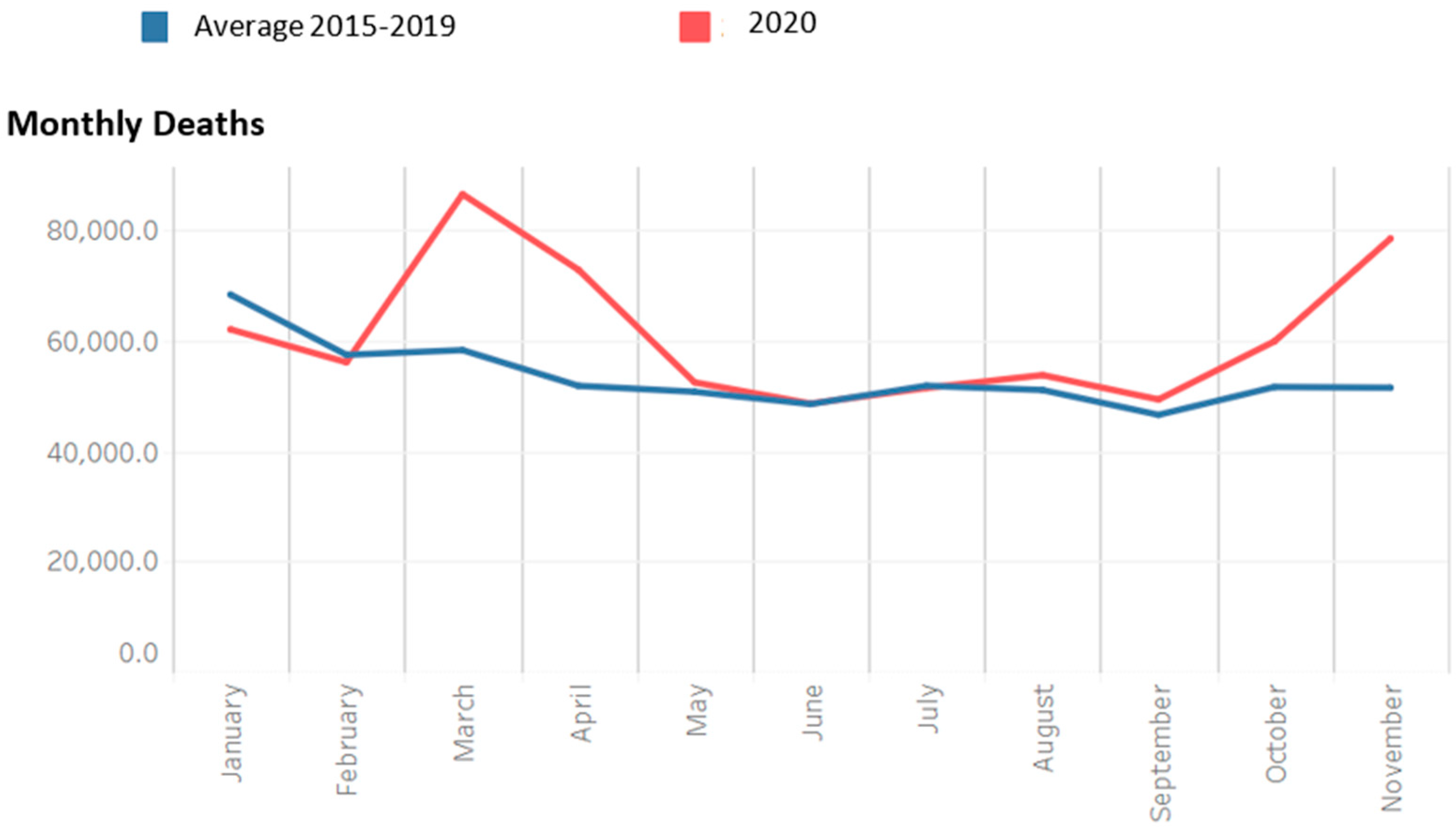
3.4. The End of the First Year of the Pandemic
3.5. The Arrival of Vaccines and How They Shaped the Second Pandemic Year
- -
- Basic Green pass: certificate of vaccination against COVID-19, negative antigenic or molecular test, or previous recovery from the disease.
- -
- Enhanced green pass: certificate attesting vaccination or recovery from previous COVID-19 disease. This certificate was introduced later to increase vaccination acceptance among skeptics by limiting access to specific services and activities only to those showing proof of vaccination, hence not including those with a negative swab, either antigenic or molecular.
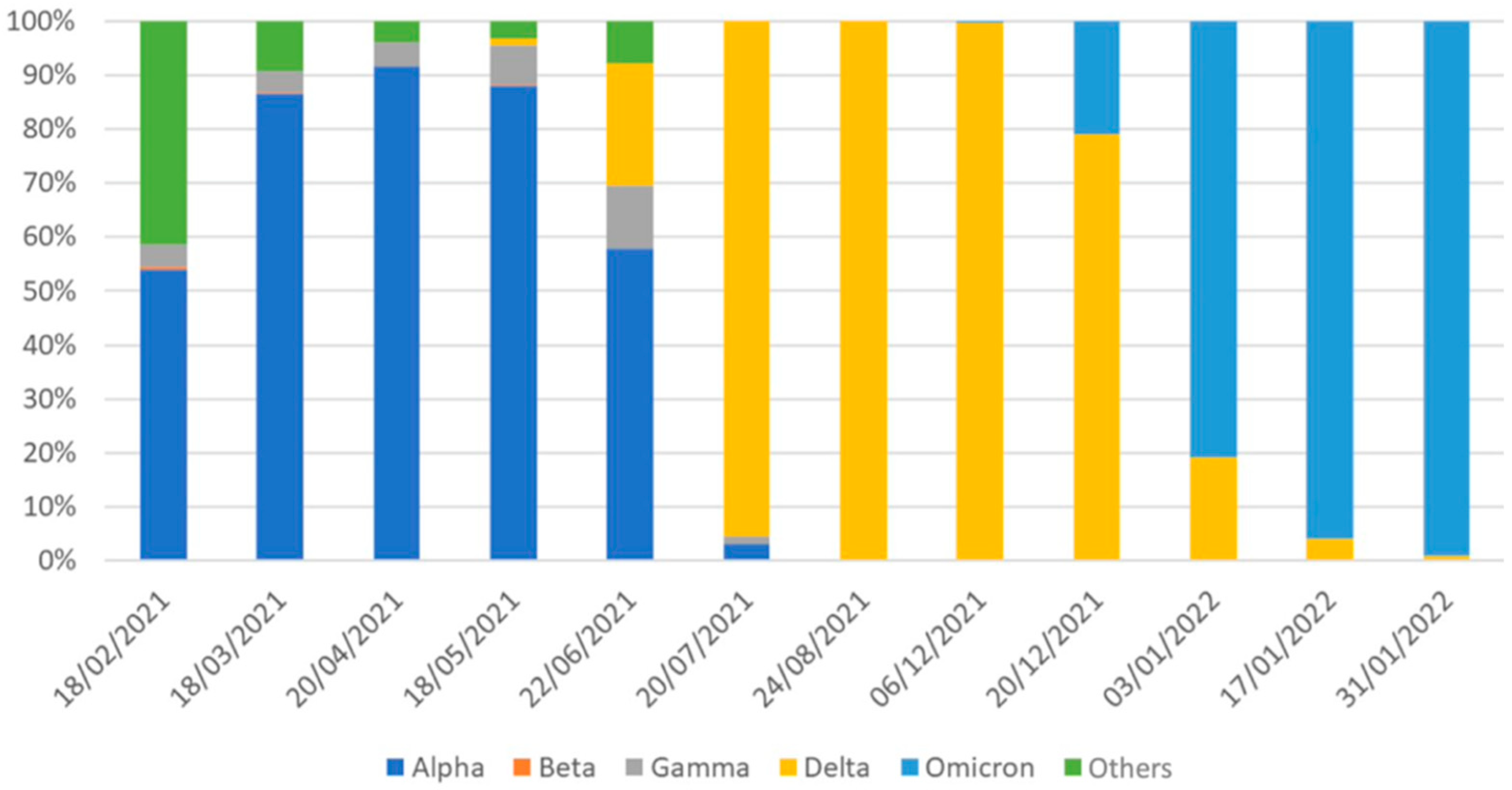
3.6. The Emergence and Spread of SARS-CoV-2 Variants
3.7. Towards “Multiple Pandemics”
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Explication of the indicators used
| Indicator Type | Indicator Name |
|---|---|
| Monitoring capability | |
| Monitoring capability | |
| Monitoring capability | |
| Monitoring capability | |
| Monitoring capability | Number of checklists administered to nursing homes (optional) |
| Monitoring capability | Number of nursing homes responding to checklists weekly and reporting at least one criticality (optional) |
| Diagnostic tests and contact tracing | Percentage of positive swabs, excluding screening initiatives and re-tested individuals, overall and divided by macro-setting (primary care, emergency department, hospital) per month |
| Diagnostic tests and contact tracing | Time elapsed between symptom onset and diagnosis |
| Diagnostic tests and contact tracing | Time elapsed between symptom onset and the start of isolation |
| Diagnostic tests and contact tracing | Number, type of professionals and time/person in each primary care service dedicated to contact tracing |
| Diagnostic tests and contact tracing | Number, type of professionals and time/person in each primary care service dedicated to sample collection and sending to reference labs and monitoring of close contacts and cases in quarantine and isolation |
| Diagnostic tests and contact tracing | |
| Transmission stability and health systems resilience | Number of cases reported to Civil Protection in the last 14 days |
| Transmission stability and health systems resilience | Rt as calculated by ISS Integrated Surveillance |
| Transmission stability and health systems resilience | Number of cases reported to the COVID-net network per week (optional) |
| Transmission stability and health systems resilience | Number of cases by date of diagnosis and date of symptom onset reported to the ISS Integrated Surveillance by day |
| Transmission stability and health systems resilience | Number of new transmission outbreaks (≥ 2 new related cases or unexpected increase in the number of cases in a defined time and place) |
| Transmission stability and health systems resilience | Number of new infection cases by Region, not associated to acknowledged transmission chains |
| Transmission stability and health systems resilience | Number of emergency department accesses with ICD-9 classification compatible with COVID-19 symptoms |
| Transmission stability and health systems resilience | Intensive care bed occupancy rate for COVID-19 patients |
| Transmission stability and health systems resilience | Bed occupancy rate for COVID-19 patients in medical wards |
References
- Pneumonia of Unknown Cause—China [Internet]. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON229 (accessed on 12 July 2022).
- Atzrodt, C.L.; Maknojia, I.; McCarthy, R.D.; Oldfield, T.M.; Po, J.; Ta, K.T.; Stepp, H.E.; Clements, T.P. A Guide to COVID-19: A global pandemic caused by the novel coronavirus SARS-CoV-2. FEBS J. 2020, 287, 3633–3650. Available online: https://pubmed.ncbi.nlm.nih.gov/32446285/ (accessed on 12 July 2022). [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. Available online: https://pubmed.ncbi.nlm.nih.gov/32191675/ (accessed on 12 July 2022). [PubMed]
- Portale COVID-19 [Internet]. Available online: https://www.agenas.gov.it/covid19/web/index.php (accessed on 12 July 2022).
- Wang, Z.; Fu, Y.; Guo, Z.; Li, J.; Li, J.; Cheng, H.; Lu, B.; Sun, Q. Transmission and prevention of SARS-CoV-2. Biochem. Soc. Trans. 2020, 48, 2307–2316. Available online: https://pubmed.ncbi.nlm.nih.gov/33084885/ (accessed on 12 July 2022). [CrossRef] [PubMed]
- ASPHER—How to Count Illness [Internet]. Available online: https://www.aspher.org/how-to-count-illness.html (accessed on 12 July 2022).
- Boccia, S.; Ricciardi, W.; Ioannidis, J.P.A. What Other Countries Can Learn from Italy During the COVID-19 Pandemic. JAMA Intern. Med. 2020, 180, 927–928. Available online: https://pubmed.ncbi.nlm.nih.gov/32259190/ (accessed on 18 October 2022). [CrossRef]
- Bubar, K.M.; Reinholt, K.; Kissler, S.M.; Lipsitch, M.; Cobey, S.; Grad, Y.H.; Larremore, D.B. Model-informed COVID-19 vaccine prioritization strategies by age and serostatus. Science 2021, 371, 916–921. [Google Scholar] [CrossRef]
- Coronavirus. Dipartimento della Protezione Civile. Available online: https://mappe.protezionecivile.gov.it/it/mappe-emergenze/mappe-coronavirus/situazione-desktop (accessed on 18 October 2022).
- Infografica Web—Dati della Sorveglianza Integrata COVID-19 in Italia—Epicentro ISS [Internet]. Available online: https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard (accessed on 18 October 2022).
- European Centre for Disease Prevention and Control. Available online: https://www.ecdc.europa.eu/en (accessed on 18 October 2022).
- Risorse Dati su COVID-19. Available online: https://dati-covid.italia.it/ (accessed on 18 October 2022).
- Istat.it [Internet]. Available online: https://www.istat.it/it/files//2020/03/tabella-regionale-decessi-totali20102022_1.xlsx (accessed on 18 October 2022).
- Talic, S.; Shah, S.; Wild, H.; Gasevic, D.; Maharaj, A.; Ademi, Z.; Li, C.; Xu, W.; Mesa-Eguiagaray, I.; Rostron, J.; et al. Effectiveness of public health measures in reducing the incidence of COVID-19, SARS-CoV-2 transmission, and COVID-19 mortality: Systematic review and meta-analysis. BMJ 2021, 375, e068302. Available online: https://pubmed.ncbi.nlm.nih.gov/34789505/ (accessed on 12 July 2022). [CrossRef]
- Coronavirus—News [Internet]. Available online: https://www.epicentro.iss.it/coronavirus/aggiornamenti (accessed on 12 July 2022).
- Specchia, M.L.; di Pilla, A.; Sapienza, M.; Riccardi, M.T.; Cicchetti, A.; Damiani, G.; Instant Report Group. Dealing with COVID-19 Epidemic in Italy: Responses from Regional Organizational Models during the First Phase of the Epidemic. Int. J. Environ. Res. Public Health 2021, 18, 5008. Available online: https://pubmed.ncbi.nlm.nih.gov/34065117/ (accessed on 12 July 2022). [CrossRef]
- Singer, B.J.; Thompson, R.N.; Bonsall, M.B. The effect of the definition of “pandemic” on quantitative assessments of infectious disease outbreak risk. Sci. Rep. 2021, 11, 584–585. [Google Scholar] [CrossRef]
- Zhang, S.X.; Arroyo Marioli, F.; Gao, R.; Wang, S. A Second Wave? What Do People Mean by COVID Waves?—A Working Definition of Epidemic Waves. Risk Manag. Healthc. Policy 2021, 14, 3775. [Google Scholar] [CrossRef]
- Peixoto, V.R.; McCallum, A.; Reintjes, R.; Lopes, H.; Franco, D.; Beccia, F.; Prikazsky, V.; Chatarajupalli, P.; Reid, J. ASPHER Report COVID-19 Pandemic Waves Surveillance in Another Severe Winter of 2021: A Basic Guide to Understand Epidemic Contexts, Interpret Pandemic Waves and Trends, Ahead of the Curve; ASPHER: Brussels, Belgium, 2021. [Google Scholar]
- Akin, L.; Gözel, M.G. Understanding dynamics of pandemics. Turk. J. Med. Sci. 2020, 50, 515–519. Available online: https://pubmed.ncbi.nlm.nih.gov/32299204/ (accessed on 12 July 2022). [CrossRef]
- Janik, E.; Niemcewicz, M.; Podogrocki, M.; Majsterek, I.; Bijak, M. The Emerging Concern and Interest SARS-CoV-2 Variants. Pathogens 2021, 10, 633. Available online: https://pubmed.ncbi.nlm.nih.gov/34064143/ (accessed on 12 July 2022). [CrossRef] [PubMed]
- Lauring, A.S.; Hodcroft, E.B. Genetic Variants of SARS-CoV-2—What Do They Mean? J. Am. Med. Assoc. 2021, 325, 529–531. [Google Scholar] [CrossRef] [PubMed]
- Gazzetta Ufficiale—Delibera del Consiglio dei Ministri 31 Gennaio 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/02/01/20A00737/sg (accessed on 12 July 2022).
- Giovanetti, M.; Benvenuto, D.; Angeletti, S.; Ciccozzi, M. The first two cases of 2019-nCoV in Italy: Where they come from? J. Med. Virol. 2020, 92, 518–521. Available online: https://pubmed.ncbi.nlm.nih.gov/32022275/ (accessed on 12 July 2022). [CrossRef]
- Alicandro, G.; Remuzzi, G.; la Vecchia, C. Italy’s first wave of the COVID-19 pandemic has ended: No excess mortality in May, 2020. Lancet 2020, 396, e27–e28. Available online: http://www.thelancet.com/article/S0140673620318651/fulltext (accessed on 12 July 2022). [CrossRef]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. Available online: https://pubmed.ncbi.nlm.nih.gov/32178769/ (accessed on 12 July 2022). [CrossRef]
- First Coronavirus Death in Italy Sends 10 Towns into Lockdown. Available online: https://nypost.com/2020/02/22/first-coronavirus-death-in-italy-forces-10-towns-into-lockdown/ (accessed on 12 July 2022).
- Montomoli, E.; Apolone, G.; Manenti, A.; Boeri, M.; Suatoni, P.; Sabia, F.; Marchianò, A.; Bollati, V.; Pastorino, U.; Sozzi, G. Timeline of SARS-CoV-2 Spread in Italy: Results from an Independent Serological Retesting. Viruses 2021, 14, 61. Available online: http://www.ncbi.nlm.nih.gov/pubmed/35062265 (accessed on 12 July 2022). [CrossRef]
- Apolone, G.; Montomoli, E.; Manenti, A.; Boeri, M.; Sabia, F.; Hyseni, I.; Mazzini, L.; Martinuzzi, D.; Cantone, L.; Milanese, G.; et al. Unexpected detection of SARS-CoV-2 antibodies in the prepandemic period in Italy. Tumori 2021, 107, 446–451. Available online: https://pubmed.ncbi.nlm.nih.gov/33176598/ (accessed on 12 July 2022). [CrossRef]
- Russo, L.; Anastassopoulou, C.; Tsakris, A.; Bifulco, G.N.; Campana, E.F.; Toraldo, G.; Siettos, C. Tracing day-zero and forecasting the COVID-19 outbreak in Lombardy, Italy: A compartmental modelling and numerical optimization approach. PLoS ONE 2020, 15, e0240649. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0240649 (accessed on 12 July 2022). [CrossRef]
- I Primi due Casi Confermati in Italia—ISS [Internet]. Available online: https://www.iss.it/covid-19-primo-piano/-/asset_publisher/yX1afjCDBkWH/content/i-primi-due-casi-confermati-in-italia (accessed on 12 July 2022).
- Veera Krishna, M. Mathematical modelling on diffusion and control of COVID–19. Infect. Dis. Model. 2020, 5, 588–597. [Google Scholar] [CrossRef]
- La Rosa, G.; Mancini, P.; Ferraro, G.B.; Veneri, C.; Iaconelli, M.; Bonadonna, L.; Lucentini, L.; Suffredini, E. SARS-CoV-2 has been circulating in northern Italy since December 2019: Evidence from environmental monitoring. Sci. Total Environ. 2021, 750, 141711. [Google Scholar] [CrossRef]
- Rudan, I. A cascade of causes that led to the COVID-19 tragedy in Italy and in other European Union countries. J. Glob. Health 2020, 10, 010335. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7125421/ (accessed on 13 July 2022). [CrossRef]
- Alfano, V. COVID-19 Diffusion Before Awareness: The Role of Football Match Attendance in Italy. J. Sports Econ. 2021, 23, 503–523. Available online: https://journals.sagepub.com/doi/full/10.1177/15270025211067786?casa_token=aqwEstoR1YQAAAAA%3As7NjW4jvEep9zYi7TBNQ5iPlUAIUj3AGY0u57OXbwdV4IFrWU-E_3vjbsj-kpqY_NnLDdH2HkUg7b6Q (accessed on 13 July 2022). [CrossRef]
- Ministero della Salute Direzione Generale della Prevenzione Sanitaria—0001997-22/01/2020-DGPRE-D. 2020. Available online: http://www.salute.gov.it/portale/malattieInfettive/dettaglioContenutiMalattieInfettive.jsp?lingua=ital (accessed on 13 July 2022).
- Gazzetta Ufficiale—Ordinanza n. 640 27 Febbraio 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/02/28/20A01348/sg (accessed on 13 July 2022).
- COVID-19 Italia—Desktop. Available online: https://opendatadpc.maps.arcgis.com/apps/dashboards/b0c68bce2cce478eaac82fe38d4138b1 (accessed on 12 July 2022).
- Carinci, F. COVID-19: Preparedness, decentralisation, and the hunt for patient zero. BMJ 2020, 368, 28. Available online: https://www.bmj.com/content/368/bmj.m799 (accessed on 12 July 2022). [CrossRef]
- Anastassopoulou, C.; Siettos, C.; Russo, L.; Vrioni, G.; Tsakris, A. Lessons from the devastating impact of the first COVID-19 wave in Italy. Pathog. Glob. Health 2021, 115, 211–212. Available online: https://www.tandfonline.com/doi/abs/10.1080/20477724.2021.1894399 (accessed on 12 July 2022). [CrossRef]
- OxCGRT [Internet]. Available online: https://covidtracker.bsg.ox.ac.uk/stringency-scatter (accessed on 13 July 2022).
- Gazzetta Ufficiale—Raccolta degli Atti Recanti Misure Urgenti in Materia di Contenimento e Gestione dell’Emergenza Epidemiologica da COVID-19. Available online: https://www.gazzettaufficiale.it/dettaglioArea/12 (accessed on 13 July 2022).
- Micheli, V.; Mancon, A.; Malara, A.; Mileto, D.; Villani, P.G.; Rizzo, A.; Pagani, C.; Alquati, O.; Gismondo, M.R. What was behind the first recognition and characterization of autochthonous SARS-CoV-2 transmission in Italy: The impact on European scenario. Clin. Case Rep. 2021, 9, e04154. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/ccr3.4154 (accessed on 13 July 2022). [CrossRef]
- Aristei, L.; D’Ambrosio, F.; Villani, L.; Rossi, M.F.; Daniele, A.; Amantea, C.; Damiani, G.; Laurenti, P.; Ricciardi, W.; Gualano, M.R.; et al. Public Health Regulations and Policies Dealing with Preparedness and Emergency Management: The Experience of the COVID-19 Pandemic in Italy. Int. J. Environ. Res. Public Health 2022, 19, 1091. Available online: https://www.mdpi.com/1660-4601/19/3/1091/htm (accessed on 14 July 2022). [PubMed]
- Cepiku, D.; Giordano, F.; Bovaird, T.; Loeffler, E. New development: Managing the COVID-19 pandemic—From a hospital-centred model of care to a community co-production approach. Public Money Manag. 2020, 41, 77–80. Available online: https://www.tandfonline.com/doi/abs/10.1080/09540962.2020.1821445 (accessed on 13 July 2022). [CrossRef]
- Coronavirus in Italia, i Dati e la Mappa. Available online: https://lab24.ilsole24ore.com/coronavirus/ (accessed on 13 July 2022).
- Vinceti, M.; Filippini, T.; Rothman, K.J.; di Federico, S.; Orsini, N. SARS-CoV-2 infection incidence during the first and second COVID-19 waves in Italy. Environ. Res. 2021, 197, 111097. Available online: https://pubmed.ncbi.nlm.nih.gov/33811866/ (accessed on 13 July 2022). [CrossRef] [PubMed]
- Lilleri, D.; Zavaglio, F.; Gabanti, E.; Gerna, G.; Arbustini, E. Analysis of the SARS-CoV-2 epidemic in Italy: The role of local and interventional factors in the control of the epidemic. PLoS ONE 2020, 15, e0242305. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0242305 (accessed on 13 July 2022). [CrossRef] [PubMed]
- Park, Y.J.; Choe, Y.J.; Park, O.; Park, S.Y.; Kim, Y.M.; Kim, J.; Kweon, S.; Woo, Y.; Gwack, J.; Kim, S.S.; et al. Contact Tracing during Coronavirus Disease Outbreak, South Korea, 2020. Emerg. Infect. Dis. 2020, 26, 2465–2468. Available online: https://pubmed.ncbi.nlm.nih.gov/32673193/ (accessed on 15 July 2022). [PubMed]
- Immuni—Sito Ufficiale. Available online: https://www.immuni.italia.it/ (accessed on 15 July 2022).
- Ussai, S.; Pistis, M.; Missoni, E.; Formenti, B.; Armocida, B.; Pedrazzi, T.; Castelli, F.; Monasta, L.; Lauria, B.; Mariani, I. “Immuni” and the National Health System: Lessons Learnt from the COVID-19 Digital Contact Tracing in Italy. Int. J. Environ. Res. Public Health 2022, 19, 7529. Available online: https://pubmed.ncbi.nlm.nih.gov/35742778/ (accessed on 15 July 2022). [CrossRef] [PubMed]
- Chirico, F.; Sacco, A.; Nucera, G.; Magnavita, N. Coronavirus disease 2019: The second wave in Italy. J. Health Res. 2021, 35, 359–363. [Google Scholar] [CrossRef]
- Indolfi, C.; Spaccarotella, C. The Outbreak of COVID-19 in Italy: Fighting the Pandemic. JACC Case Rep. 2020, 2, 1414–1418. Available online: https://pubmed.ncbi.nlm.nih.gov/32835287/ (accessed on 13 July 2022). [CrossRef] [PubMed]
- COVID-19, dall’Iss un Nuovo Rapporto sulla Telemedicina Rivolto agli Operatori e ai Manager Sanitari Coinvolti nell’Emergenza. Available online: https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?menu=notizie&id=4503 (accessed on 13 July 2022).
- Luzi, L.; Carruba, M.; Crialesi, R.; Da Empoli, S.; Dagani, R.; Lovati, E.; Nicolucci, A.; Berra, C.C.; Cipponeri, E.; Vaccaro, K.; et al. Telemedicine and urban diabetes during COVID-19 pandemic in Milano, Italy during lock-down: Epidemiological and sociodemographic picture. Acta Diabetol. 2021, 58, 919–927. Available online: https://pubmed.ncbi.nlm.nih.gov/33740123/ (accessed on 13 July 2022). [CrossRef] [PubMed]
- Indini, A.; Pinotti, G.; Artioli, F.; Aschele, C.; Bernardi, D.; Butera, A.; Defraia, E.; Fasola, G.; Gamucci, T.; Giordano, M.; et al. Management of patients with cancer during the COVID-19 pandemic: The Italian perspective on the second wave. Eur. J. Cancer 2021, 148, 112–116. Available online: https://pubmed.ncbi.nlm.nih.gov/33743478/ (accessed on 13 July 2022). [CrossRef]
- de Filippis, G.; Cavazzana, L.; Gimigliano, A.; Piacenza, M.; Vimercati, S. COVID-19 pandemic: A frontline hospital reorganization to cope with therapeutic and diagnostic emergency. Pharmacol. Res. 2020, 161, 105160. Available online: https://pubmed.ncbi.nlm.nih.gov/32810626/ (accessed on 13 July 2022). [CrossRef]
- Portacci, A.; Carpagnano, G.E.; Tummolo, M.G.; Santomasi, C.; Palma, L.; Fasano, D.; Resta, E.; Lozupone, M.; Solfrizzi, V.; Panza, F.; et al. COVID-19 clinical phenotypes and short-term outcomes: Differences between the first and the second wave of pandemic in Italy. Expert Rev. Respir. Med. 2021, 15, 1619–1625. Available online: https://pubmed.ncbi.nlm.nih.gov/34311634/ (accessed on 13 July 2022). [CrossRef]
- Gazzetta Ufficiale—Decreto-Legge 14 Agosto 2020, n. 104. Available online: https://www.gazzettaufficiale.it/eli/id/2020/08/14/20G00122/sg (accessed on 13 July 2022).
- Gazzetta Ufficiale—Decreto del Presidente del Consiglio dei Ministri 7 Agosto 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/08/08/20A04399/sg (accessed on 13 July 2022).
- Gazzetta Ufficiale—Decreto del Presidente del Consiglio dei Ministri 24 Settembre 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/12/04/20A06526/sg (accessed on 13 July 2022).
- Gazzetta Ufficiale—Ordinanza 21 Settembre 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/09/21/20A05139/sg (accessed on 13 July 2022).
- Gazzetta Ufficiale—Decreto del Presidente del Consiglio dei Ministri 18 Ottobre 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/10/18/20A05727/sg (accessed on 13 July 2022).
- RegioneLombardia—Ordinanza n. 620 16 Ottobre 2020. Available online: https://www.regione.lombardia.it/wps/wcm/connect/8273fc8e-743e-4642-b941-cbcdbdd81721/ORDINANZA_620_del_16_ottobre_2020.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-8273fc8e-743e-4642-b941-cbcdbdd81721-nkPmXvH (accessed on 13 July 2022).
- Gazzetta Ufficiale—Decreto del Presidente del Consiglio dei Ministri 3 Novembre 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/11/04/20A06109/sg (accessed on 13 July 2022).
- Andrea, M.; Gianluca, F.; Paolo, S.; Massimo, A.; Mennini, F.S. The impact of Covid-19 vaccination on the Italian healthcare system: A scenario analysis. medRxiv 2021. medRxiv:2021.06.08.21258561. Available online: https://www.medrxiv.org/content/10.1101/2021.06.08.21258561v1 (accessed on 13 July 2022).
- Gazzetta Ufficiale—Ordinanza 13 Novembre 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/11/14/20A06292/sg (accessed on 13 July 2022).
- Bontempi, E. The europe second wave of COVID-19 infection and the Italy “strange” situation. Environ. Res. 2021, 193, 110476. Available online: https://pubmed.ncbi.nlm.nih.gov/33221311/ (accessed on 13 July 2022). [CrossRef]
- Elia, F.; Vallelonga, F. “Pandemic fatigue” or something worse? Recenti Prog. Med. 2020, 111, 788–789. Available online: https://pubmed.ncbi.nlm.nih.gov/33362178/ (accessed on 13 July 2022).
- Adam, D. The pandemic’s true death toll: Millions more than official counts. Nature 2022, 601, 312–315. [Google Scholar] [CrossRef]
- Heaton, P.M. The COVID-19 Vaccine-Development Multiverse. New Engl. J. Med. 2020, 383, 1986–1988. Available online: https://www.nejm.org/doi/full/10.1056/NEJMe2025111 (accessed on 13 July 2022). [CrossRef] [PubMed]
- Vaccine Day il 27 Dicembre in Tutta Italia e in Europa. Available online: https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?id=5242 (accessed on 13 July 2022).
- Ministero della Salute. Piano Vaccini Anti COVID-19. Available online: https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?id=5452&area=nuovoCoronavirus&menu=vuoto (accessed on 13 July 2022).
- Gazzetta Ufficiale—Decreto-Legge 18 Dicembre 2020, n. 172. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2020-12-18&atto.codiceRedazionale=20G00196 (accessed on 13 July 2022).
- WHO. Pandemic Fatigue Reinvigorating the Public to Prevent COVID-19. 2020. Available online: http://apps.who.int/bookorders (accessed on 13 July 2022).
- Meacci, L.; Primicerio, M. Pandemic fatigue impact on COVID-19 spread: A mathematical modelling answer to the Italian scenario. Results Phys. 2021, 31, 104895. [Google Scholar] [CrossRef] [PubMed]
- Circolare Ministero della Salute n. 42164 del 24 Dicembre 2020. Available online: https://www.certifico.com/news/274-news/12430-circolare-ministero-della-salute-n-42164-del-24-dicembre-2020 (accessed on 14 July 2022).
- National COVID-19 Vaccination Plan. Available online: https://www.epicentro.iss.it/en/vaccines/covid-19-vaccination-plan (accessed on 14 July 2022).
- Campagna Vaccinazione anti COVID-19, il Piano Strategico Nazionale. Available online: https://www.governo.it/it/approfondimento/campagna-vaccinazione-anti-covid-19/16000 (accessed on 14 July 2022).
- Vitiello, A.; Ferrara, F.; Troiano, V.; la Porta, R. COVID-19 vaccines and decreased transmission of SARS-CoV-2. Inflammopharmacology 2021, 29, 1357–1360. Available online: https://link.springer.com/article/10.1007/s10787-021-00847-2 (accessed on 14 July 2022). [CrossRef] [PubMed]
- Agenzia Italiana del Farmaco. Farmacovigilanza su Vaccini COVID-19. Available online: https://www.aifa.gov.it/farmacovigilanza-vaccini-covid-19 (accessed on 14 July 2022).
- Pastorino, R.; Pezzullo, A.M.; Villani, L.; Causio, F.A.; Axfors, C.; Contopoulos-Ioannidis, D.G.; Boccia, S.; Ioannidis, J.P. Change in age distribution of COVID-19 deaths with the introduction of COVID-19 vaccination. Environ. Res. 2022, 204, 112342. Available online: https://pubmed.ncbi.nlm.nih.gov/34748775/ (accessed on 14 July 2022). [CrossRef]
- Gazzetta Ufficiale—Decreto-Legge 18 Maggio 2021, n. 65. Available online: https://www.gazzettaufficiale.it/eli/id/2021/05/18/21G00078/SG (accessed on 14 July 2022).
- Gazzetta Ufficiale—Ordinanza 2 Aprile 2021. Available online: https://www.gazzettaufficiale.it/eli/id/2021/04/03/21A02151/sg (accessed on 14 July 2022).
- Beccia, F.; Amantea, C.; Rossi, M.F.; Daniele, A.; Santoro, P.E.; Borrelli, I.; Marazza, M.; Boccia, S.; Ricciardi, W.; Moscato, U. Legal resposability of vaccinating doctor. G. Ital. Di Med. Del Lav. Ed Ergon. 2021, 43, 93–98. [Google Scholar]
- Gazzetta Ufficiale—Decreto-Legge 1 Aprile 2021, n. 44. Available online: https://www.gazzettaufficiale.it/eli/id/2021/04/01/21G00056/sg (accessed on 14 July 2022).
- Moccia, G.; Carpinelli, L.; Savarese, G.; de Caro, F. Vaccine Hesitancy and the Green Digital Pass: A Study on Adherence to the Italian COVID-19 Vaccination Campaign. Int. J. Environ. Res. Public Health 2022, 19, 2970. Available online: https://pubmed.ncbi.nlm.nih.gov/35270662/ (accessed on 15 July 2022). [CrossRef]
- Gazzetta Ufficiale—Decreto-Legge 10 Settembre 2021, n. 121. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2021-09-10&atto.codiceRedazionale=21G00133&elenco30giorni=false (accessed on 15 July 2022).
- Gazzetta Ufficiale—Ordinanza 30 Agosto 2021. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2021-09-01&atto.codiceRedazionale=21A05230&elenco30giorni=false (accessed on 15 July 2022).
- Stefanizzi, P.; Bianchi, F.P.; Brescia, N.; Ferorelli, D.; Tafuri, S. Vaccination strategies between compulsion and incentives. The Italian Green Pass experience. Expert Rev. Vaccines 2022, 21, 423–425. Available online: https://pubmed.ncbi.nlm.nih.gov/34962214/ (accessed on 15 July 2022). [CrossRef]
- Gurdasani, D.; Alwan, N.A.; Greenhalgh, T.; Hyde, Z.; Johnson, L.; McKee, M.; Michie, S.; Prather, K.A.; Rasmussen, S.D.; Reicher, S.; et al. School reopening without robust COVID-19 mitigation risks accelerating the pandemic. Lancet 2021, 397, 1177–1178. Available online: https://pubmed.ncbi.nlm.nih.gov/33713595/ (accessed on 15 July 2022). [CrossRef]
- Parker, J.; Boles, C.; Egnot, N.; Sundermann, A.; Fleeger, A. Return to normal operations: COVID-19 mitigation strategies for workplaces. Toxicol. Ind Health 2020, 36, 711–717. [Google Scholar] [CrossRef]
- lo Moro, G.; Sinigaglia, T.; Bert, F.; Savatteri, A.; Gualano, M.R.; Siliquini, R. Reopening schools during the COVID-19 pandemic: Overview and rapid systematic review of guidelines and recommendations on preventive measures and the management of cases. Int. J. Environ. Res. Public Health 2020, 17, 8839. [Google Scholar] [CrossRef]
- Vermund, S.H.; Pitzer, V.E. Asymptomatic Transmission and the Infection Fatality Risk for COVID-19: Implications for School Reopening. Clin. Infect. Dis. 2021, 72, 1493–1496. Available online: https://pubmed.ncbi.nlm.nih.gov/32584967/ (accessed on 15 July 2022). [CrossRef] [PubMed]
- Chotpitayasunondh, T.; Fischer, T.K.; Heraud, J.M.; Hurt, A.C.; Monto, A.S.; Osterhaus, A.; Shu, Y.; Tam, J.S. Influenza and COVID-19: What does co-existence mean? Influenza Other Respir. Viruses 2021, 15, 407–412. Available online: https://pubmed.ncbi.nlm.nih.gov/33128444/ (accessed on 15 July 2022). [CrossRef] [PubMed]
- Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ (accessed on 14 July 2022).
- Rapporto ISS COVID-19 n. 4/2021—Indicazioni ad Interim sulle Misure di Prevenzione e Controllo delle Infezioni da SARS-CoV-2 in Tema di Varianti e Vaccinazione Anti COVID-19. Versione del 13 Marzo 2021—ISS. Available online: https://www.iss.it/rapporti-covid-19/-/asset_publisher/btw1J82wtYzH/content/id/5659920 (accessed on 14 July 2022).
- Loconsole, D.; Centrone, F.; Morcavallo, C.; Campanella, S.; Sallustio, A.; Accogli, M.; Fortunato, F.; Parisi, A.; Chironna, M. Rapid Spread of the SARS-CoV-2 Variant of Concern 202012/01 in Southern Italy (December 2020–March 2021). Int. J. Environ. Res. Public Health 2021, 18, 4766. Available online: https://www.mdpi.com/1660-4601/18/9/4766/htm (accessed on 14 July 2022). [CrossRef] [PubMed]
- Flash Survey COVID-19—ISS. Available online: https://www.iss.it/web/guest/comunicati-stampa (accessed on 20 October 2022).
- Sarini, M.; Actis Grosso, R.; Magrin, M.E.; Mari, S.; Olivero, N.; Paganin, G.; Simbula, S. A Cluster Analysis of the Acceptance of a Contact Tracing App—The Identification of Profiles for the Italian Immuni Contact Tracing App. Healthcare 2022, 10, 888. [Google Scholar] [CrossRef] [PubMed]
- Campanozzi, L.L.; Tambone, V.; Ciccozzi, M. A Lesson from the Green Pass Experience in Italy: A Narrative Review. Vaccines 2022, 10, 1483. Available online: https://pubmed.ncbi.nlm.nih.gov/36146561/ (accessed on 18 October 2022). [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beccia, F.; Di Pilla, A.; Causio, F.A.; Federico, B.; Specchia, M.L.; Favaretti, C.; Boccia, S.; Damiani, G. Narrative Review of the COVID-19 Pandemic’s First Two Years in Italy. Int. J. Environ. Res. Public Health 2022, 19, 15443. https://doi.org/10.3390/ijerph192315443
Beccia F, Di Pilla A, Causio FA, Federico B, Specchia ML, Favaretti C, Boccia S, Damiani G. Narrative Review of the COVID-19 Pandemic’s First Two Years in Italy. International Journal of Environmental Research and Public Health. 2022; 19(23):15443. https://doi.org/10.3390/ijerph192315443
Chicago/Turabian StyleBeccia, Flavia, Andrea Di Pilla, Francesco Andrea Causio, Bruno Federico, Maria Lucia Specchia, Carlo Favaretti, Stefania Boccia, and Gianfranco Damiani. 2022. "Narrative Review of the COVID-19 Pandemic’s First Two Years in Italy" International Journal of Environmental Research and Public Health 19, no. 23: 15443. https://doi.org/10.3390/ijerph192315443
APA StyleBeccia, F., Di Pilla, A., Causio, F. A., Federico, B., Specchia, M. L., Favaretti, C., Boccia, S., & Damiani, G. (2022). Narrative Review of the COVID-19 Pandemic’s First Two Years in Italy. International Journal of Environmental Research and Public Health, 19(23), 15443. https://doi.org/10.3390/ijerph192315443









