Effect of Disease Severity, Age of Child, and Clinic No-Shows on Unscheduled Healthcare Use for Childhood Asthma at an Academic Medical Center
Abstract
1. Introduction
1.1. Literature Review and Conceptual Framework
1.2. Study Purpose and Significance
2. Methods
2.1. Data Collection: Dependent Variables (DVs)
- A user_12 is a patient who has had at least one of any the below types of healthcare encounters over past 12 months:
- ○
- Emergency department visit for asthma;
- ○
- Inpatient admission for asthma;
- ○
- Pediatric Intensive Care Unit (PICU) admission for asthma.
- A non-user_12 is a patient who had none (zero) of all the above types of encounters over past 12 months.
- A user_18 is a patient who has had at least one of any the below types of healthcare encounters over past 18 months:
- ○
- Emergency department visit for asthma;
- ○
- Inpatient admission for asthma;
- ○
- Pediatric Intensive Care Unit (PICU) admission for asthma.
- A non-user_18 is a patient who had none (zero) of all the above types of encounters over past 18 months.
- A user_24 is a patient who has had at least one of any the below types of healthcare encounters over past 24 months:
- ○
- Emergency department visit for asthma;
- ○
- Inpatient admission for asthma;
- ○
- Pediatric Intensive Care Unit (PICU) admission for asthma.
- A non-user_24 is a patient who had none (zero) of all the above types of encounters over past 24 months.
2.2. Data Collection: Independent Variables (IVs)
- Individual demographic characteristics, including age 0–<8 years, 8–<13 years, 13–<17 years, and ≥17 years); gender (male or female); race (Caucasian, African American, Hispanic, other); and insurance (Medicaid, private, other).
- Individual risk factors, including disease (asthma) severity (intermittent, mild-persistent, moderate-persistent, or severe-persistent); BMI, defined as normal (<85%), overweight (85–95%), or obese (>95%); medication adherence (yes or no); smoking (yes or no); 12-month, 18-month, and 24-month clinic no-shows (zero no-shows, 1–2 no-shows, 3–4 no-shows, >4 no-shows); 12-month and 18-month clinic appointment cancellations (zero cancellations, 1–5 cancellations, ≥6 cancellations); and 24-month clinic appointment cancellations (0–<6 cancellations, 6–10 cancellations, ≥11 cancellations). It would be relevant to note that medication adherence was defined as a yes (1) or no (0) binary variable. This was the best way to accomplish this for our study, which relied entirely on medical record documentation. For our study sample, the documentation related to medication adherence was complete to the point of being able to distinguish between whether medication adherence was present to any degree (1) or not present at all (0) for all study subjects. Beyond this, the documentation was not available to qualitatively categorize various additional levels of medication adherence (e.g., from very low to very high) reliably and consistently for all study subjects. Correspondingly, a binary definition was determined to be most appropriate for the purpose of this study.
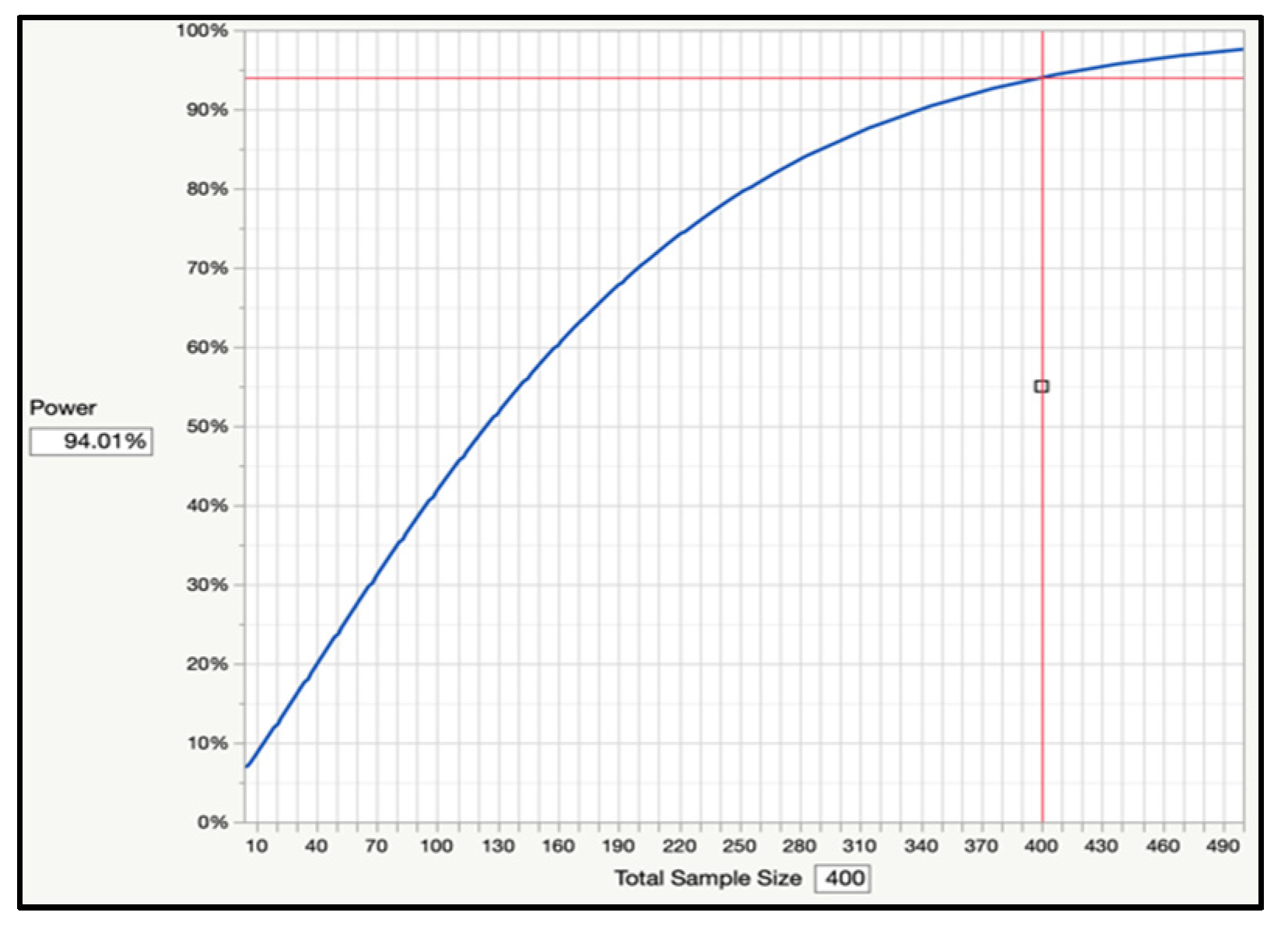
2.3. Data Analysis
3. Results
- A total of 105 children were users of unscheduled healthcare over the previous 12 months, while 305 children were non-users over the previous 12 months. In other words, 26% of the children either visited the ED or were hospitalized for asthma at least once over the previous 12 months, while 74% of the children had zero unscheduled healthcare encounters (ED or inpatient) over the previous 12 months.
- A total of 131 children were users of unscheduled healthcare over the previous 18 months, while 279 children were non-users over the previous 18 months. In other words, 32% of the children either visited the ED or were hospitalized for asthma at least once over the previous 18 months, while 68% of the children had zero unscheduled healthcare encounters (ED or inpatient) over the previous 18 months.
- A total of 147 children were users of unscheduled healthcare over the previous 24 months, while 263 children were non-users over the previous 24 months. In other words, 36% of the children either visited the ED or were hospitalized for asthma at least once over the previous 24 months, while 64% of the children had zero unscheduled healthcare encounters (ED or inpatient) over the previous 24 months.
3.1. Summary Characteristics of Study Population
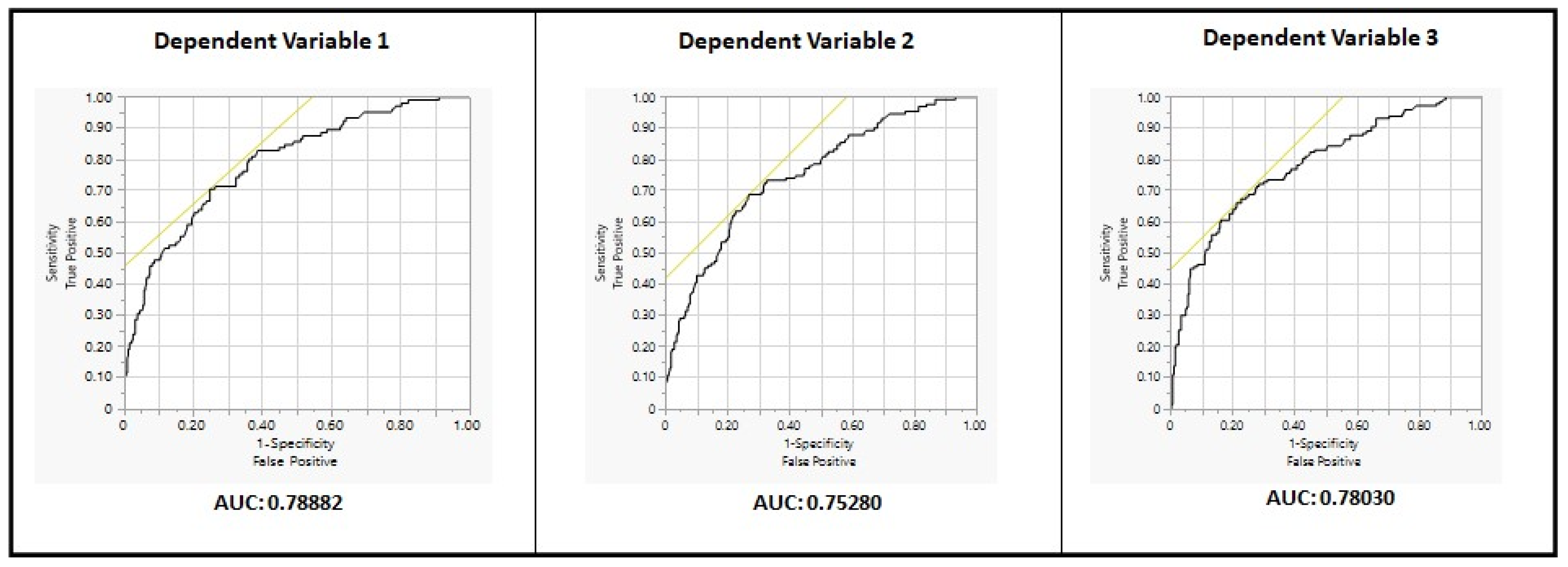
3.2. Results for Dependent Variable 1 (DV1)
3.3. Results for Dependent Variable 2 (DV2)
3.4. Results for Dependent Variable 3 (DV3)
3.5. Overall Significance of Results for DV1, DV2, and DV3
4. Discussion
4.1. Influence of Social Determinants of Health on Clinic No-Shows for Childhood Asthma
4.2. Implications for Practice
4.3. Implications for Future Research
4.4. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johnson, L.H.; Chambers, P.; Dexheimer, J.W. Asthma-related emergency department use: Current perspectives. Open Access Emerg. Med. 2016, 8, 47–55. [Google Scholar] [PubMed]
- Hurst, J.H.; Zhao, C.; Fitzpatrick, N.S.; Goldstein, B.A.; Lang, J.E. Reduced pediatric urgent asthma utilization and exacerbations during the COVID-19 pandemic. Pediatr. Pulmonol. 2021, 56, 3166–3173. [Google Scholar] [CrossRef] [PubMed]
- Inserro, A. CDC Study Puts Economic Burden of Asthma at More Than $80 Billion per Year. 2018. Available online: https://www.ajmc.com/view/cdc-study-puts-economic-burden-of-asthma-at-more-than-80-billion-per-year (accessed on 15 May 2020).
- National Institutes of Health National Asthma Education & Prevention Program. In Guidelines for the Diagnosis and Management of Asthma. Expert Panel Report 3; United States Department of Health and Human Services: Washington, DC, USA, 2007.
- Centers for Disease Control and Prevention. Asthma self-management education and environmental management: Approaches to enhancing reimbursement. In National Asthma Control Program; CDC: Atlanta, GA, USA, 2014. [Google Scholar]
- Pinnock, H.; Parke, H.L.; Panagioti, M.; Daines, L.; Pearce, G.; Epiphaniou, E.; Bower, P.; Sheikh, A.; Griffiths, C.J.; Taylor, S.J.C.; et al. Systematic meta-review of supported self-management for asthma: A healthcare perspective. BMC Med. 2017, 15, 64. [Google Scholar] [CrossRef] [PubMed]
- Pinnock, H.; Epiphaniou, E.; Pearce, G.; Parke, H.; Greenhalgh, T.; Sheikh, A.; Griffiths, C.J.; Taylor, S.J.C. Implementing supported self-management for asthma: A systematic review and suggested hierarchy of evidence of implementation studies. BMC Med. 2015, 13, 127. [Google Scholar] [CrossRef]
- Pinnock, H. Supported self-management for asthma. Breathe 2015, 11, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Pinnock, H.; Thomas, M. Does self-management prevent severe exacerbations? Curr. Opin. Pulm. Med. 2015, 21, 95–102. [Google Scholar] [CrossRef]
- Rangachari, P. A framework for measuring self-management effectiveness and healthcare use among pediatric asthma patients & families. J. Asthma Allergy 2017, 10, 111–122. [Google Scholar]
- Rangachari, P.; May, K.R.; Stepleman, L.M.; Tingen, M.S.; Looney, S.; Liang, Y.; Rockich-Winston, N.; Rethemeyer, R.K. Measurement of Key Constructs in a Holistic Framework for Assessing Self-Management Effectiveness of Pediatric Asthma. Int. J. Environ. Res. Public Health 2019, 16, 3060. [Google Scholar] [CrossRef]
- Rangachari, P.; Griffin, D.D.; Ghosh, S.; May, K.R. Demographic and Risk-Factor Differences between Users and Non-Users of Unscheduled Healthcare among Pediatric Outpatients with Persistent Asthma. Int. J. Environ. Res. Public Health 2020, 17, 2704. [Google Scholar] [CrossRef]
- Rangachari, P.; Chen, J.; Ahuja, N.; Patel, A.; Mehta, R. Demographic and Risk Factor Differences between Children with “One-Time” and “Repeat” Visits to the Emergency Department for Asthma. Int. J. Environ. Res. Public Health 2021, 18, 486. [Google Scholar] [CrossRef]
- Suruki, R.Y.; Daugherty, J.B.; Boudiaf, N.; Albers, F.C. The frequency of asthma exacerbations and healthcare utilization in patients with asthma from the UK and USA. BMC Pulm. Med. 2017, 17, 74. [Google Scholar] [CrossRef] [PubMed]
- Kenyon, C.C.; Strane, D.; Floyd, G.C.; Jacobi, E.G.; Penrose, T.J.; Ewig, J.M.; DaVeiga, S.P.; Zorc, J.J.; Rubin, D.M.; Bryant-Stephens, T.C. An Asthma Population Health Improvement Initiative for Children With Frequent Hospitalizations. Pediatrics 2020, 146, e20193108. [Google Scholar] [CrossRef] [PubMed]
- Pinto, J.M.; Wagle, S.; Navallo, L.J.; Petrova, A. Risk Factors and Outcomes Associated With Antibiotic Therapy in Children Hospitalized With Asthma Exacerbation. J. Pediatr. Pharmacol. Ther. 2022, 27, 366–372. [Google Scholar] [CrossRef]
- Nath, J.B.; Hsia, R.Y. Children’s emergency department use for asthma, 2001–2010. Acad. Pediatr. 2015, 15, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Persaud, Y.K. Using Telemedicine to Care for the Asthma Patient. Curr. Allergy Asthma Rep. 2022, 22, 43–52. [Google Scholar] [CrossRef]
- Casemiro, L.K.D.D.S.; Lopes-Júnior, L.C.; Jardim, F.A.; Sulino, M.C.; de Lima, R.A.G. Telehealth in outpatient care for children and adolescents with chronic conditions during the COVID-19 pandemic: A scoping review protocol. PLoS ONE 2022, 17, e0269821. [Google Scholar] [CrossRef]
- Perry, T.T.; Margiotta, C.A. Implementing Telehealth in Pediatric Asthma. Pediatr. Clin. N. Am. 2020, 67, 623–627. [Google Scholar] [CrossRef]
- Davies, B.; Kenia, P.; Nagakumar, P.; Gupta, A. Paediatric and adolescent asthma: A narrative review of telemedicine and emerging technologies for the post-COVID-19 era. Clin. Exp. Allergy 2021, 51, 393–401. [Google Scholar] [CrossRef]
- Young, H.N.; Len-Rios, M.E.; Brown, R.; Moreno, M.A.; Cox, E.D. How does patient-provider communication influence adherence to asthma medications? Patient Educ. Couns. 2017, 100, 696–702. [Google Scholar] [CrossRef]
- McGovern, C.M.; Redmond, M.; Arcoleo, K.; Stukus, D.R. A missed primary care appointment correlates with a subsequent emergency department visit among children with asthma. J. Asthma 2017, 54, 977–982. [Google Scholar] [CrossRef]
- Roberts, W.; Kim, E.J.; Martinez JUwemedimo, O.T. Associations of adverse social determinants of health with missed well-child visits and the role of caregiver social support. J. Adv. Pediatr. Child Health 2021, 4, 067–072. [Google Scholar] [CrossRef]
- Seid, M. Barriers to care and primary care for vulnerable children with asthma. Pediatrics 2008, 122, 994–1002. [Google Scholar] [CrossRef] [PubMed]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression, 2nd ed.; John Wiley & Sons: New York, NY, USA, 2000. [Google Scholar]
- Tom, J.O.; Mangione-Smith, R.; Grossman, D.C.; Solomon, C.; Tseng, C.W. Well-childcare visits and risk of ambulatory care-sensitive hospitalizations. Am. J. Manag. Care 2013, 19, 354–360. [Google Scholar] [PubMed]
- Tom, J.O.; Tseng, C.W.; Davis, J.; Solomon, C.; Zhou, C.; Mangione-Smith, R. Missed well childcare visits, low continuity of care, and risk of ambulatory care sensitive hospitalizations in young children. Arch. Pediatr. Adolesc. Med. 2010, 164, 1052–1058. [Google Scholar] [CrossRef] [PubMed]
- Chung, E.K.; Siegel, B.S.; Garg, A.; Conroy, K.; Gross, R.S.; Long, D.A.; Lewis, G.; Osman, C.J.; Messito, M.J.; Wade, R.; et al. Screening for Social Determinants of Health Among Children and Families Living in Poverty: A Guide for Clinicians. Curr. Probl. Pediatr. Adolesc. Health Care 2016, 46, 135–153. [Google Scholar] [CrossRef]
- Singh, G.K.; Siahpush, M.; Kogan, M.D. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Aff. (Millwood) 2010, 29, 503–512. [Google Scholar] [CrossRef]
- Krieger, J.; Higgins, D.L. Housing and health: Time again for public health action. Am. J. Public Health 2002, 92, 758–768. [Google Scholar] [CrossRef]
- Lampard, A.M.; Franckle, R.L.; Davison, K.K. Maternal depression and childhood obesity: A systematic review. Prev. Med. 2014, 59, 60–67. [Google Scholar] [CrossRef]
- Scheckner, B.; Arcoleo, K.; Feldman, J.M. The effect of parental social support and acculturation on childhood asthma control. J. Asthma 2015, 52, 606–613. [Google Scholar] [CrossRef]
- Van Houten, L.; Deegan, K.; Siemer, M.; Walsh, S. A Telehealth Initiative to Decrease No-Show Rates in a Pediatric Asthma Mobile Clinic. J. Pediatr. Nurs. 2021, 59, 143–150. [Google Scholar] [CrossRef]
- Garg, A.; Toy, S.; Tripodis, Y.; Silverstein, M.; Freeman, E. Addressing social determinants of health at well childcare visits: A cluster RCT. Pediatrics 2005, 135, e296–e304. [Google Scholar] [CrossRef] [PubMed]
- O’Gurek, D.T.; Henke, C. A Practical Approach to Screening for Social Determinants of Health. Fam. Pract. Manag. 2018, 25, 7–12. [Google Scholar] [PubMed]
- Gottlieb, L.M.; Hessler, D.; Long, D.; Laves, E.; Burns, A.R.; Amaya, A.; Sweeney, P.; Schudel, C.; Adler, N.E. Effects of Social Needs Screening and In-Person Service Navigation on Child Health: A Randomized Clinical Trial. JAMA Pediatr. 2016, 170, e162521. [Google Scholar] [CrossRef]
- Fleury, M.J.; Ngui, A.N.; Bamvita, J.M.; Grenier, G.; Caron, J. Predictors of healthcare service utilization for mental health reasons. Int. J. Environ. Res. Public Health 2014, 11, 10559–10586. [Google Scholar] [CrossRef]
- Sullivan, K.; Thakur, N. Structural and Social Determinants of Health in Asthma: A Scoping Review of Literature Published Between 2014 and 2019. Curr. Allergy Asthma Rep. 2020, 20, 5. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.; Gray, M.; Burns, C.; Owens, L.; Woolfenden, S.; Lingam, R.; Jaffe, A.; Homaira, N. Community-based interventions for childhood asthma using comprehensive approaches: A systematic review and meta-analysis. Allergy Asthma Clin. Immunol. 2021, 17, 19. [Google Scholar] [CrossRef] [PubMed]
- Burns, R.R.; Alpern, E.R.; Rodean, J.; Canares, T.; Lee, B.R.; Hall, M.; Montalbano, A. Factors Associated With Urgent Care Reliance and Outpatient Health Care Use Among Children Enrolled in Medicaid. JAMA Netw. Open. 2020, 3, e204185. [Google Scholar] [CrossRef]
- Asthma and Allergy Foundation of America. Asthma Capitals: Top 100 National Ranking. Available online: https://www.aafa.org/asthma-capitals-top-100-cities-ranking/ (accessed on 1 June 2020).
- Fetherling, J.T. Vilfredo Pareto’s 80/20 Hypothesis Applies to Healthcare. 2016. Available online: https://www.perceptionhealth.com/research/80-20-pareto-lives-in-healthcare (accessed on 15 June 2020).
| Parameter | N | % |
|---|---|---|
| DV 1 (12 Months) | ||
| User | 105 | 26% |
| Non-User | 305 | 74% |
| Total | 410 | 100% |
| DV 2 (18 Months) | ||
| User | 131 | 32% |
| Non-User | 279 | 68% |
| Total | 410 | 100% |
| DV 3 (24 Months) | ||
| User | 147 | 36% |
| Non-User | 263 | 64% |
| Total | 410 | 100% |
| Individual Demographics (IVs) | ||
| Age: 0–<8 years | 205 | 50% |
| Age: 8–<13 years | 141 | 34% |
| Age: 13–<17 years | 47 | 11% |
| Age: ≥17 years | 17 | 4% |
| Total | 410 | 100% |
| Gender: Male | 271 | 66% |
| Gender: Female | 139 | 34% |
| Total | 410 | 100% |
| Race: Caucasian | 135 | 33% |
| Race: African American | 223 | 54% |
| Race: Hispanic | 21 | 5% |
| Race: Other | 31 | 8% |
| Total | 410 | 100% |
| Insurance: Medicaid | 231 | 56% |
| Insurance: Private | 175 | 43% |
| Insurance: Other | 4 | 1% |
| Total | 410 | 100% |
| Individual Risk Factors (IVs) | ||
| Asthma Severity: Intermittent | 58 | 14% |
| Asthma Severity: Mild-Persistent | 212 | 52% |
| Asthma Severity: Moderate-Persistent | 118 | 29% |
| Asthma Severity: Severe-Persistent | 22 | 5% |
| Total | 410 | 100% |
| BMI: Normal | 239 | 58% |
| BMI: Overweight | 59 | 14% |
| BMI: Obese | 112 | 27% |
| Total | 410 | 100% |
| Medication Adherence: Yes | 320 | 78% |
| Medication Adherence: No | 90 | 22% |
| Total | 410 | 100% |
| Smoking: Yes | 72 | 18% |
| Smoking: No | 338 | 82% |
| Total | 410 | 100% |
| Clinic No-Shows: 0 (Zero) | 341 | 83% |
| Clinic No-Shows: 1–2 | 53 | 13% |
| Clinic No-Shows: 3–4 | 8 | 2% |
| Clinic No-Shows: >4 | 8 | 2% |
| Total | 410 | 100% |
| Clinic Cancellations: 0 (Zero) | 218 | 53% |
| Clinic Cancellations: 1–5 | 182 | 44% |
| Clinic Cancellations: ≥6 | 10 | 2% |
| Total | 410 | 100% |
| (A) | ||||||
| Whole Model Test | ||||||
| Model | Log Likelihood | DF | Chi Square | Prob > Chi Sq | ||
| Difference | 47.73091 | 21 | 95.46182 | <0.0001 * | ||
| Full | 185.5326 | |||||
| Reduced | 233.26351 | |||||
| Parameter Estimates | ||||||
| Term | Estimate | Std Error | Chi Square | Prob > Chi Sq | Lower 95% | Upper 95% |
| Intercept | 3.10925547 | 286.18073 | 0 | 0.9913 | −1.337641 | 564.01317 |
| Asthma Severity (Severe-Persistent) | 1.00766313 | 0.4202947 | 5.75 | 0.0165 * | 0.1822147 | 1.8481486 |
| Asthma Severity (Moderate-Persistent) | 0.73348999 | 0.2345889 | 9.78 | 0.0018 * | 0.2761057 | 1.1990824 |
| Asthma Severity (Mild-Persistent) | −0.8439822 | 0.2479135 | 11.59 | 0.0007 * | −1.335839 | −0.360113 |
| Age (17 years or more) | −0.3849129 | 0.5031052 | 0.59 | 0.4442 | −1.458727 | 0.5515176 |
| Age (13 to <17 years) | −0.425855 | 0.3792272 | 1.26 | 0.2615 | −1.207428 | 0.2944103 |
| Age (8 to <13 years) | 0.26933076 | 0.2647422 | 1.03 | 0.309 | −0.242509 | 0.801635 |
| Gender (Female) | 0.19893506 | 0.1379018 | 2.08 | 0.1491 | −0.072656 | 0.4694543 |
| Race (African American) | −0.0912106 | 0.2567094 | 0.13 | 0.7224 | −0.590236 | 0.4222511 |
| Race (Hispanic) | 0.25553467 | 0.472329 | 0.29 | 0.5885 | −0.730232 | 1.1475258 |
| Race (Other) | −0.2024715 | 0.4405372 | 0.21 | 0.6458 | −1.134801 | 0.6189104 |
| Insurance (Other) | −0.1254631 | 0.8980123 | 0.02 | 0.8889 | −2.291412 | 1.5013845 |
| Insurance (Medicaid) | 0.26627943 | 0.4706286 | 0.32 | 0.5715 | −0.594814 | 1.3755291 |
| BMI (85%–95%) | −0.0760498 | 0.2736893 | 0.08 | 0.7811 | −0.634293 | 0.4452441 |
| BMI (>95%) | −0.2592004 | 0.2333955 | 1.23 | 0.2668 | −0.726666 | 0.1929795 |
| Medication Adherence (Yes) | −0.1082721 | 0.1593159 | 0.46 | 0.4968 | −0.416859 | 0.2100099 |
| Smoking (Yes) | 0.06674975 | 0.1729105 | 0.15 | 0.6995 | −0.280879 | 0.400096 |
| 12-Month Clinic No-Shows (>4) | 12.3212843 | 858.5404 | 0 | 0.9885 | 1.0119037 | 1695.0295 |
| 12-Month Clinic No-Shows (3–4) | −3.5081953 | 286.18072 | 0 | 0.9902 | −564.4121 | 0.8880258 |
| 12-Month Clinic No-Shows (1–2) | −4.2117577 | 286.18031 | 0 | 0.9883 | −565.1149 | 556.69135 |
| 12-Month Clinic Cancellations (>6) | −0.135352 | 0.5865781 | 0.05 | 0.8175 | −1.379394 | 0.9998991 |
| 12-Month Clinic Cancellations (1–5) | 0.49501316 | 0.3187117 | 2.41 | 0.1204 | −0.121688 | 1.1594346 |
| Effect Likelihood Ratio Tests | ||||||
| Source | N parm | DF | L-R Chi Square | Prob > Chi Sq | ||
| Asthma Severity | 3 | 3 | 34.3119365 | <0.0001 * | ||
| Age | 3 | 3 | 5.27815849 | 0.1525 | ||
| Gender | 1 | 1 | 2.06868437 | 0.1504 | ||
| Race | 3 | 3 | 0.51852276 | 0.9148 | ||
| Insurance | 2 | 2 | 2.04399283 | 0.3599 | ||
| BMI | 2 | 2 | 3.75236926 | 0.1532 | ||
| Medication Adherence | 1 | 1 | 0.45657801 | 0.4992 | ||
| Smoking | 1 | 1 | 0.14775536 | 0.7007 | ||
| 12-Month Clinic No-Shows | 3 | 3 | 14.0359689 | 0.0029 * | ||
| 12-Month Clinic Cancellations | 2 | 2 | 9.28535975 | 0.0096 * | ||
| Notes: For log odds of 1/0 (user/non-user); confidence limits are likelihood-based. | ||||||
| (B) | ||||||
| Odds Ratios for Asthma Severity | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Severe-Persistent | Intermittent | 6.7182928 | 0.0051 * | 1.77393 | 25.443766 | |
| Moderate-Persistent | Intermittent | 5.1072492 | 0.0005 * | 2.03754 | 12.801709 | |
| Mild-Persistent | Intermittent | 1.0546287 | 0.91 | 0.4193492 | 2.6523043 | |
| Severe-Persistent | Mild-Persistent | 6.370292 | 0.0015 * | 2.0244327 | 20.045428 | |
| Moderate-Persistent | Mild-Persistent | 4.8426988 | <0.0001 * | 2.6266546 | 8.9283653 | |
| Severe-Persistent | Moderate-Persistent | 1.3154425 | 0.6268 | 0.4356032 | 3.9723971 | |
| Odds Ratios for Age | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| ≥17 years | 0–<8 years | 0.3959965 | 0.1752 | 0.1037825 | 1.5109793 | |
| 13–<17 years | 0–<8 years | 0.3801109 | 0.0531 | 0.1426082 | 1.013156 | |
| 8–<13 years | 0–<8 years | 0.7617732 | 0.3671 | 0.42171 | 1.3760603 | |
| ≥17 years | 8–<13 years | 0.5198351 | 0.3412 | 0.1351193 | 1.9999255 | |
| 13–<17 years | 8–<13 years | 0.4989817 | 0.1661 | 0.1865546 | 1.3346374 | |
| ≥17 years | 13–<17 years | 1.0417919 | 0.9581 | 0.2258901 | 4.8046826 | |
| Odds Ratios for Gender | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Female | Male | 1.4886507 | 0.1491 | 0.8670186 | 2.5559785 | |
| Odds Ratios for Race | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Hispanic | African American | 1.4144564 | 0.5775 | 0.4175866 | 4.7910713 | |
| Other | African American | 0.8947053 | 0.8481 | 0.2865822 | 2.7932566 | |
| Other | Hispanic | 0.6325436 | 0.5696 | 0.1304904 | 3.0662121 | |
| African American | White | 0.8786593 | 0.6788 | 0.4763782 | 1.6206494 | |
| Hispanic | White | 1.2428253 | 0.7358 | 0.351526 | 4.3940263 | |
| Other | White | 0.7861411 | 0.6838 | 0.2469147 | 2.5029608 | |
| Odds Ratios for Insurance | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Other | Medicaid | 0.6758781 | 0.7723 | 0.0475925 | 9.598397 | |
| Other | Private | 1.0154718 | 0.991 | 0.0712492 | 14.472914 | |
| Medicaid | Private | 1.502448 | 0.1573 | 0.8546733 | 2.6411849 | |
| Odds Ratios for BMI | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Overweight | Normal | 0.6627881 | 0.319 | 0.2951565 | 1.4883226 | |
| Obese | Normal | 0.5518657 | 0.0718 | 0.2888932 | 1.0542155 | |
| Obese | Overweight | 0.8326427 | 0.697 | 0.3311887 | 2.0933498 | |
| Odds Ratios for Medication Adherence | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Yes | No | 0.805297 | 0.4968 | 0.4312571 | 1.5037509 | |
| Odds Ratios for Smoking | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| No | Yes | 0.8750279 | 0.6995 | 0.4442818 | 1.7233967 | |
| Odds Ratios for Clinic No-Shows Over Previous 12 Months | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| >4 | 0 (Zero) | 22356230 | 0.9882 | 0 | . | |
| 3–4 | 0 (Zero) | 2.9836162 | 0.1908 | 0.5800966 | 15.34566 | |
| 1–2 | 0 (Zero) | 1.4763511 | 0.2926 | 0.7146973 | 3.0497003 | |
| >4 | 1–2 | 15142896 | 0.9885 | 0 | . | |
| 3–4 | 1–2 | 2.0209394 | 0.4125 | 0.375618 | 10.87327 | |
| >4 | 3–4 | 7492998.2 | 0.989 | 0 | . | |
| Odds Ratios for Clinic Cancellations Over Previous 12 Months | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| ≥6 | 0 (Zero) | 1.2514578 | 0.8031 | 0.2146779 | 7.2953341 | |
| 1–5 | 0 (Zero) | 2.3506087 | 0.0028 * | 1.3430675 | 4.1139863 | |
| ≥6 | 1–5 | 0.5323974 | 0.4754 | 0.0942852 | 3.0062721 | |
| * Statistically significant at the alpha = 0.05 level Note: Normal approximations used for ratio confidence limits effects | ||||||
| Note: Tests and confidence intervals on odds ratios are Wald based | ||||||
| (A) | ||||||
| Whole Model Test | ||||||
| Model | Log Likelihood | DF | Chi Square | Prob > Chi Sq | ||
| Difference | 41.66268 | 21 | 83.32535 | <0.0001 * | ||
| Full | 215.20282 | |||||
| Reduced | 256.8655 | |||||
| Parameter Estimates | ||||||
| Term | Estimate | Std Error | Chi Square | Prob > Chi Sq | Lower 95% | Upper 95% |
| Intercept | 3.81066446 | 463.17797 | 0 | 0.9934 | −0.807645 | 911.622812 |
| Asthma Severity (Severe-Persistent) | 0.88484924 | 0.4111501 | 4.63 | 0.0314 * | 0.082496 | 1.71312545 |
| Asthma Severity (Moderate-Persistent) | 0.64232011 | 0.2240972 | 8.22 | 0.0042 * | 0.20337465 | 1.08481296 |
| Asthma Severity (Mild-Persistent) | −0.5811561 | 0.2252614 | 6.66 | 0.0099 * | −1.0265903 | −0.1404289 |
| Age (17 years or more) | −0.2516179 | 0.4551622 | 0.31 | 0.5804 | −1.2026226 | 0.61172251 |
| Age (13 to <17 years) | −0.6228092 | 0.3595594 | 3 | 0.0832 | −1.3661091 | 0.05658379 |
| Age (8 to <13 years) | 0.30290465 | 0.243885 | 1.54 | 0.2142 | −0.1695335 | 0.79091998 |
| Gender (Female) | 0.14081023 | 0.1261681 | 1.25 | 0.2644 | −0.1077524 | 0.38790043 |
| Race (African American) | 0.08930488 | 0.2314633 | 0.15 | 0.6996 | −0.3610562 | 0.55047594 |
| Race (Hispanic) | 0.09610884 | 0.4274907 | 0.05 | 0.8221 | −0.7885718 | 0.90885011 |
| Race (Other) | −0.0425634 | 0.3849673 | 0.01 | 0.912 | −0.8396313 | 0.68663044 |
| Insurance (Other) | −0.1824744 | 0.8544395 | 0.05 | 0.8309 | −2.2945646 | 1.34496685 |
| Insurance (Medicaid) | 0.22120023 | 0.4450133 | 0.25 | 0.6191 | −0.5833937 | 1.29788571 |
| BMI (85%–95%) | 0.02552395 | 0.2432243 | 0.01 | 0.9164 | −0.4653271 | 0.49311991 |
| BMI (>95%) | −0.245739 | 0.2052649 | 1.43 | 0.2312 | −0.6542757 | 0.15321765 |
| Medication Adherence (Yes) | −0.1213201 | 0.1465945 | 0.68 | 0.4079 | −0.4063745 | 0.17003355 |
| Smoking (Yes) | 0.12812873 | 0.1568931 | 0.67 | 0.4141 | −0.1840971 | 0.43310822 |
| 18-Month Clinic No-Shows (>4) | 12.659048 | 1389.533 | 0 | 0.9927 | −2710.7756 | 2736.09371 |
| 18-Month Clinic No-Shows (3–4) | −3.3340158 | 463.17793 | 0 | 0.9943 | −911.14608 | 904.478051 |
| 18-Month Clinic No-Shows (1–2) | −4.529019 | 463.17777 | 0 | 0.9922 | −912.34076 | 903.282722 |
| 18-Month Clinic Cancellations (>6) | 0.31241103 | 0.3844156 | 0.66 | 0.4164 | −0.4447229 | 1.08317702 |
| 18-Month Clinic Cancellations (1–5) | 0.07647871 | 0.2303683 | 0.11 | 0.7399 | −0.381499 | 0.5284306 |
| Effect Likelihood Ratio Tests | ||||||
| Source | N parm | DF | L-R Chi Square | Prob > Chi Sq | ||
| Asthma Severity | 3 | 3 | 27.6008402 | <0.0001 * | ||
| Age | 3 | 3 | 7.97179927 | 0.0466 * | ||
| Gender | 1 | 1 | 1.23964425 | 0.2655 | ||
| Race | 3 | 3 | 0.6985804 | 0.8735 | ||
| Insurance | 2 | 2 | 1.09013917 | 0.5798 | ||
| BMI | 2 | 2 | 2.62511381 | 0.2691 | ||
| Medication Adherence | 1 | 1 | 0.67794164 | 0.4103 | ||
| Smoking | 1 | 1 | 0.65971892 | 0.4167 | ||
| 18-Month Clinic No-Shows | 3 | 3 | 12.7120747 | 0.0053 * | ||
| 18-Month Clinic Cancellations | 2 | 2 | 3.69393572 | 0.1577 | ||
| Notes: For log odds of 1/0 (user/non-user); confidence limits are likelihood-based. | ||||||
| (B) | ||||||
| Odds Ratios for Asthma Severity | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Severe-Persistent | Intermittent | 6.2392658 | 0.0047 * | 1.7521237 | 22.217859 | |
| Moderate-Persistent | Intermittent | 4.8955831 | 0.0002 * | 2.1155993 | 11.328579 | |
| Mild-Persistent | Intermittent | 1.4403083 | 0.3822 | 0.6354456 | 3.2646192 | |
| Severe-Persistent | Mild-Persistent | 4.3318959 | 0.0095 * | 1.4309161 | 13.114201 | |
| Moderate-Persistent | Mild-Persistent | 3.3989827 | <0.0001 * | 1.947435 | 5.9324618 | |
| Severe-Persistent | Moderate-Persistent | 1.2744684 | 0.6623 | 0.4291828 | 3.7845638 | |
| Odds Ratios for Age | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| ≥17 years | 0–<8 years | 0.4390507 | 0.1829 | 0.1307521 | 1.474283 | |
| 13–<17 years | 0–<8 years | 0.3029064 | 0.0123 * | 0.1189042 | 0.7716487 | |
| 8–<13 years | 0–<8 years | 0.7644354 | 0.3243 | 0.4480939 | 1.3041048 | |
| ≥17 years | 8–<13 years | 0.5743464 | 0.3728 | 0.1696332 | 1.9446298 | |
| 13–<17 years | 8–<13 years | 0.3962485 | 0.0536 | 0.1548002 | 1.0142939 | |
| ≥17 years | 13–<17 years | 1.4494603 | 0.6043 | 0.3560495 | 5.9006823 | |
| Odds Ratios for Gender | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Female | Male | 1.3252756 | 0.2644 | 0.808197 | 2.1731774 | |
| Odds Ratios for Race | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Hispanic | African American | 1.0068272 | 0.9904 | 0.3318184 | 3.0549875 | |
| Other | African American | 0.8764564 | 0.7953 | 0.3236867 | 2.3732078 | |
| Other | Hispanic | 0.8705133 | 0.8465 | 0.2137911 | 3.5445512 | |
| African American | White | 1.2613155 | 0.4151 | 0.7216654 | 2.2045072 | |
| Hispanic | White | 1.2699267 | 0.6832 | 0.4030005 | 4.0017658 | |
| Other | White | 1.1054881 | 0.8462 | 0.4014029 | 3.0445812 | |
| Odds Ratios for Insurance | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Other | Medicaid | 0.6678614 | 0.7538 | 0.0535905 | 8.3230928 | |
| Other | Private | 0.8661055 | 0.9112 | 0.0692616 | 10.83052 | |
| Medicaid | Private | 1.2968342 | 0.3082 | 0.7866082 | 2.1380135 | |
| Odds Ratios for BMI | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Overweight | Normal | 0.8230889 | 0.5984 | 0.398812 | 1.6987333 | |
| Obese | Normal | 0.6275361 | 0.1112 | 0.3536754 | 1.1134547 | |
| Obese | Overweight | 0.762416 | 0.5135 | 0.3379288 | 1.7201204 | |
| Odds Ratios for Medication Adherence | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Yes | No | 0.7845537 | 0.4079 | 0.4416312 | 1.3937524 | |
| Odds Ratios for Smoking | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Yes | No | 1.2920853 | 0.4141 | 0.6985475 | 2.3899371 | |
| Odds Ratios for Clinic No-Shows Over Previous 18 Months | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| >4 | 0 (Zero) | 38074722 | 0.9925 | 0 | . | |
| 3–4 | 0 (Zero) | 4.3145687 | 0.0403 * | 1.0666393 | 17.452482 | |
| 1–2 | 0 (Zero) | 1.3060329 | 0.4537 | 0.6495346 | 2.6260679 | |
| >4 | 1–2 | 29152958 | 0.9926 | 0 | . | |
| 3–4 | 1–2 | 3.3035682 | 0.109 | 0.7662447 | 14.242922 | |
| >4 | 3–4 | 8824687.7 | 0.9931 | 0 | . | |
| Odds Ratios for Clinic Cancellations Over Previous 18 Months | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| ≥6 | 0 (Zero) | 2.0163738 | 0.2387 | 0.6279514 | 6.4746466 | |
| 1–5 | 0 (Zero) | 1.5926009 | 0.0789 | 0.9476413 | 2.6765164 | |
| ≥6 | 1–5 | 1.2660886 | 0.6883 | 0.3998737 | 4.008717 | |
| * Statistically significant at the alpha = 0.05 level Note: Normal approximations used for ratio confidence limits effects | ||||||
| Note: Tests and confidence intervals on odds ratios are Wald based | ||||||
| (A) | ||||||
| Whole Model Test | ||||||
| Model | Log Likelihood | DF | Chi Square | Prob > Chi Sq | ||
| Difference | 50.60995 | 21 | 101.2199 | <0.0001 * | ||
| Full | 216.94438 | |||||
| Reduced | 267.55433 | |||||
| Parameter Estimates | ||||||
| Term | Estimate | Std Error | Chi Square | Prob > Chi Sq | Lower 95% | Upper 95% |
| Intercept | −0.5862596 | 0.5550046 | 1.12 | 0.2908 | −1.8124974 | 0.44749185 |
| Asthma Severity (Severe-Persistent) | 1.81645034 | 0.4676356 | 15.09 | 0.0001 * | 0.9489207 | 2.80622487 |
| Asthma Severity (Moderate-Persistent) | 0.51041062 | 0.2308243 | 4.89 | 0.0270 * | 0.05099225 | 0.96076985 |
| Asthma Severity (Mild-Persistent) | −0.9350318 | 0.2441205 | 14.67 | 0.0001 * | −1.4266689 | −0.4649346 |
| Age (17 years or more) | −0.6083886 | 0.4797115 | 1.61 | 0.2047 | −1.6013847 | 0.30829146 |
| Age (13 to <17 years) | −0.6625515 | 0.345434 | 3.68 | 0.0551 | −1.3635104 | −0.0006684 |
| Age (8 to <13 years) | 0.50453293 | 0.2489767 | 4.11 | 0.0427 * | 0.02440269 | 1.00475046 |
| Gender (Female) | 0.09898491 | 0.1267119 | 0.61 | 0.4347 | −0.1504002 | 0.34736271 |
| Race (African American) | 0.37411119 | 0.2269068 | 2.72 | 0.0992 | −0.066627 | 0.82656267 |
| Race (Hispanic) | −0.1604753 | 0.4305123 | 0.14 | 0.7093 | −1.0508162 | 0.65913693 |
| Race (Other) | −0.0708666 | 0.377069 | 0.04 | 0.8509 | −0.8427195 | 0.64912982 |
| Insurance (Other) | −0.2546501 | 0.916096 | 0.08 | 0.781 | −2.4528227 | 1.36168909 |
| Insurance (Medicaid) | 0.30675852 | 0.4748893 | 0.42 | 0.5183 | −0.539296 | 1.4278081 |
| BMI (85%–95%) | 0.09283277 | 0.2364316 | 0.15 | 0.6946 | −0.3791806 | 0.55152427 |
| BMI (>95%) | −0.3011504 | 0.2018629 | 2.23 | 0.1357 | −0.7028651 | 0.09082505 |
| Medication Adherence (Yes) | −0.2076972 | 0.1459336 | 2.03 | 0.1547 | −0.4939261 | 0.07973125 |
| Smoking (Yes) | 0.25713526 | 0.1576219 | 2.66 | 0.1028 | −0.0528441 | 0.56685475 |
| 24-Month Clinic No-Shows (>4) | 0.39793737 | 0.3136794 | 1.61 | 0.2046 | −0.2138095 | 1.0228706 |
| 24-Month Clinic No-Shows (3–4) | −0.1139315 | 0.275805 | 0.17 | 0.6795 | −0.6635257 | 0.42195555 |
| 24-Month Clinic No-Shows (1–2) | 0.054728 | 0.2015985 | 0.07 | 0.786 | −0.3409418 | 0.45100075 |
| 24-Month Clinic Cancellations (>11) | 0.04404362 | 0.2478175 | 0.03 | 0.8589 | −0.4471906 | 0.52808413 |
| 24-Month Clinic Cancellations (6–10) | 0.25921714 | 0.1961435 | 1.75 | 0.1863 | −0.1243559 | 0.64638514 |
| Effect Likelihood Ratio Tests | ||||||
| Source | N parm | DF | L-R Chi Square | Prob > Chi Sq | ||
| Asthma Severity | 3 | 3 | 47.1578898 | <0.0001 * | ||
| Age | 3 | 3 | 13.5841515 | 0.0035 * | ||
| Gender | 1 | 1 | 0.60885158 | 0.4352 | ||
| Race | 3 | 3 | 3.99857532 | 0.2616 | ||
| Insurance | 2 | 2 | 2.09934652 | 0.3501 | ||
| BMI | 2 | 2 | 3.15275762 | 0.2067 | ||
| Medication Adherence | 1 | 1 | 2.01356905 | 0.1559 | ||
| Smoking | 1 | 1 | 2.64865666 | 0.1036 | ||
| 24-Month Clinic No-Shows | 3 | 3 | 3.4257436 | 0.3305 | ||
| 24-Month Clinic Cancellations | 2 | 2 | 3.79600814 | 0.1499 | ||
| Notes: For log odds of 1/0 (user/non-user); confidence limits are likelihood-based. | ||||||
| (B) | ||||||
| Odds Ratios for Asthma Severity | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Severe-Persistent | Intermittent | 24.73649 | <0.0001 * | 6.0844816 | 100.56632 | |
| Moderate-Persistent | Intermittent | 6.7008859 | <0.0001 * | 2.8733485 | 15.627019 | |
| Mild-Persistent | Intermittent | 1.5790087 | 0.2772 | 0.6926698 | 3.5995053 | |
| Severe-Persistent | Mild-Persistent | 15.665834 | <0.0001 * | 4.4047056 | 55.717315 | |
| Moderate-Persistent | Mild-Persistent | 4.2437295 | <0.0001 * | 2.4136762 | 7.461332 | |
| Severe-Persistent | Moderate-Persistent | 3.6915252 | 0.0350 * | 1.0959504 | 12.434284 | |
| Odds Ratios for Age | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| ≥17 years | 0–<8 years | 0.2528912 | 0.0363 * | 0.0698011 | 0.9162321 | |
| 13–<17 years | 0–<8 years | 0.2395583 | 0.0018 * | 0.0975783 | 0.5881244 | |
| 8–<13 years | 0–<8 years | 0.7696078 | 0.3389 | 0.4499779 | 1.3162783 | |
| ≥17 years | 8–<13 years | 0.3285975 | 0.091 | 0.0903994 | 1.194437 | |
| 13–<17 years | 8–<13 years | 0.3112732 | 0.0112 * | 0.126299 | 0.7671554 | |
| ≥17 years | 13–<17 years | 1.0556565 | 0.9406 | 0.2541272 | 4.3852474 | |
| Odds Ratios for Gender | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Female | Male | 1.2189256 | 0.4347 | 0.7417585 | 2.0030504 | |
| Odds Ratios for Race | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Hispanic | African American | 0.5859115 | 0.3477 | 0.1919701 | 1.7882588 | |
| Other | African American | 0.6408385 | 0.3669 | 0.2437878 | 1.6845549 | |
| Other | Hispanic | 1.0937463 | 0.9 | 0.2704439 | 4.423397 | |
| African American | White | 1.6767887 | 0.0662 | 0.9659637 | 2.9106895 | |
| Hispanic | White | 0.9824498 | 0.9761 | 0.3083857 | 3.1298716 | |
| Other | White | 1.0745508 | 0.8874 | 0.3972145 | 2.9068914 | |
| Odds Ratios for Insurance | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Other | Medicaid | 0.570405 | 0.6841 | 0.0381792 | 8.5219704 | |
| Other | Private | 0.8166524 | 0.8833 | 0.0545961 | 12.215549 | |
| Medicaid | Private | 1.4317062 | 0.1559 | 0.8721007 | 2.3503969 | |
| Odds Ratios for BMI | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Overweight | Normal | 0.890934 | 0.7489 | 0.4392349 | 1.8071502 | |
| Obese | Normal | 0.6008151 | 0.0801 | 0.3395754 | 1.0630298 | |
| Obese | Overweight | 0.6743654 | 0.3302 | 0.3051265 | 1.4904265 | |
| Odds Ratios for Medication Adherence | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| Yes | No | 0.6600799 | 0.1547 | 0.3725278 | 1.1695918 | |
| Odds Ratios for Smoking | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| No | Yes | 0.5979366 | 0.1028 | 0.3223437 | 1.1091521 | |
| Odds Ratios for Clinic No-Shows Over Previous 24 Months | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| >4 | 0 (Zero) | 2.0889702 | 0.1096 | 0.8473165 | 5.1501372 | |
| 3–4 | 0 (Zero) | 1.2520752 | 0.5788 | 0.5661519 | 2.7690313 | |
| 1–2 | 0 (Zero) | 1.4821027 | 0.1579 | 0.8584516 | 2.5588264 | |
| >4 | 1–2 | 1.4094638 | 0.4365 | 0.5937748 | 3.345693 | |
| 3–4 | 1–2 | 0.8447965 | 0.6665 | 0.3922674 | 1.8193741 | |
| >4 | 3–4 | 1.6684064 | 0.3058 | 0.6263267 | 4.4442938 | |
| Odds Ratios for Clinic Cancellations Over Previous 24 Months | ||||||
| Level1 | /Level2 | Odds Ratio | Prob > Chi Sq | Lower 95% | Upper 95% | |
| ≥11 | 1–5 | 1.4152474 | 0.3763 | 0.6556921 | 3.0546736 | |
| 6–10 | 1–6 | 1.7550159 | 0.0541 | 0.9902116 | 3.1105277 | |
| ≥11 | 6–10 | 0.8064015 | 0.5962 | 0.3638245 | 1.7873547 | |
| * Statistically significant at the alpha = 0.05 level Note: Normal approximations used for ratio confidence limits effects | ||||||
| Note: Tests and confidence intervals on odds ratios are Wald based | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rangachari, P.; Parvez, I.; LaFontaine, A.-A.; Mejias, C.; Thawer, F.; Chen, J.; Pathak, N.; Mehta, R. Effect of Disease Severity, Age of Child, and Clinic No-Shows on Unscheduled Healthcare Use for Childhood Asthma at an Academic Medical Center. Int. J. Environ. Res. Public Health 2023, 20, 1508. https://doi.org/10.3390/ijerph20021508
Rangachari P, Parvez I, LaFontaine A-A, Mejias C, Thawer F, Chen J, Pathak N, Mehta R. Effect of Disease Severity, Age of Child, and Clinic No-Shows on Unscheduled Healthcare Use for Childhood Asthma at an Academic Medical Center. International Journal of Environmental Research and Public Health. 2023; 20(2):1508. https://doi.org/10.3390/ijerph20021508
Chicago/Turabian StyleRangachari, Pavani, Imran Parvez, Audrey-Ann LaFontaine, Christopher Mejias, Fahim Thawer, Jie Chen, Niharika Pathak, and Renuka Mehta. 2023. "Effect of Disease Severity, Age of Child, and Clinic No-Shows on Unscheduled Healthcare Use for Childhood Asthma at an Academic Medical Center" International Journal of Environmental Research and Public Health 20, no. 2: 1508. https://doi.org/10.3390/ijerph20021508
APA StyleRangachari, P., Parvez, I., LaFontaine, A.-A., Mejias, C., Thawer, F., Chen, J., Pathak, N., & Mehta, R. (2023). Effect of Disease Severity, Age of Child, and Clinic No-Shows on Unscheduled Healthcare Use for Childhood Asthma at an Academic Medical Center. International Journal of Environmental Research and Public Health, 20(2), 1508. https://doi.org/10.3390/ijerph20021508






