Validation of the Novel Interprofessional Shared Decision-Making Questionnaire to Facilitate Multidisciplinary Team Building in Patient-Centered Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Measurements
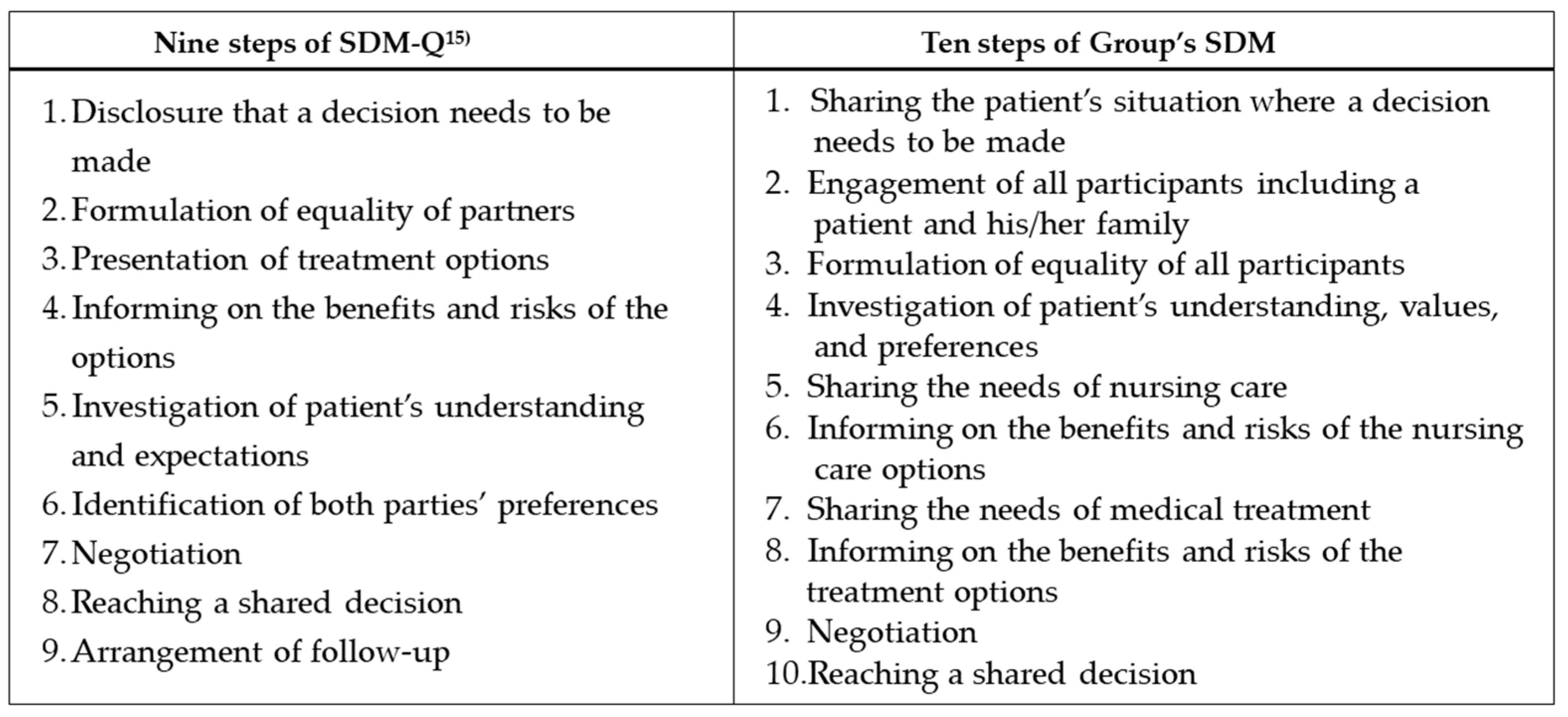
2.2.1. Identification of Elements Needed for the Interprofessional SDM Measure (Group’s SDM)
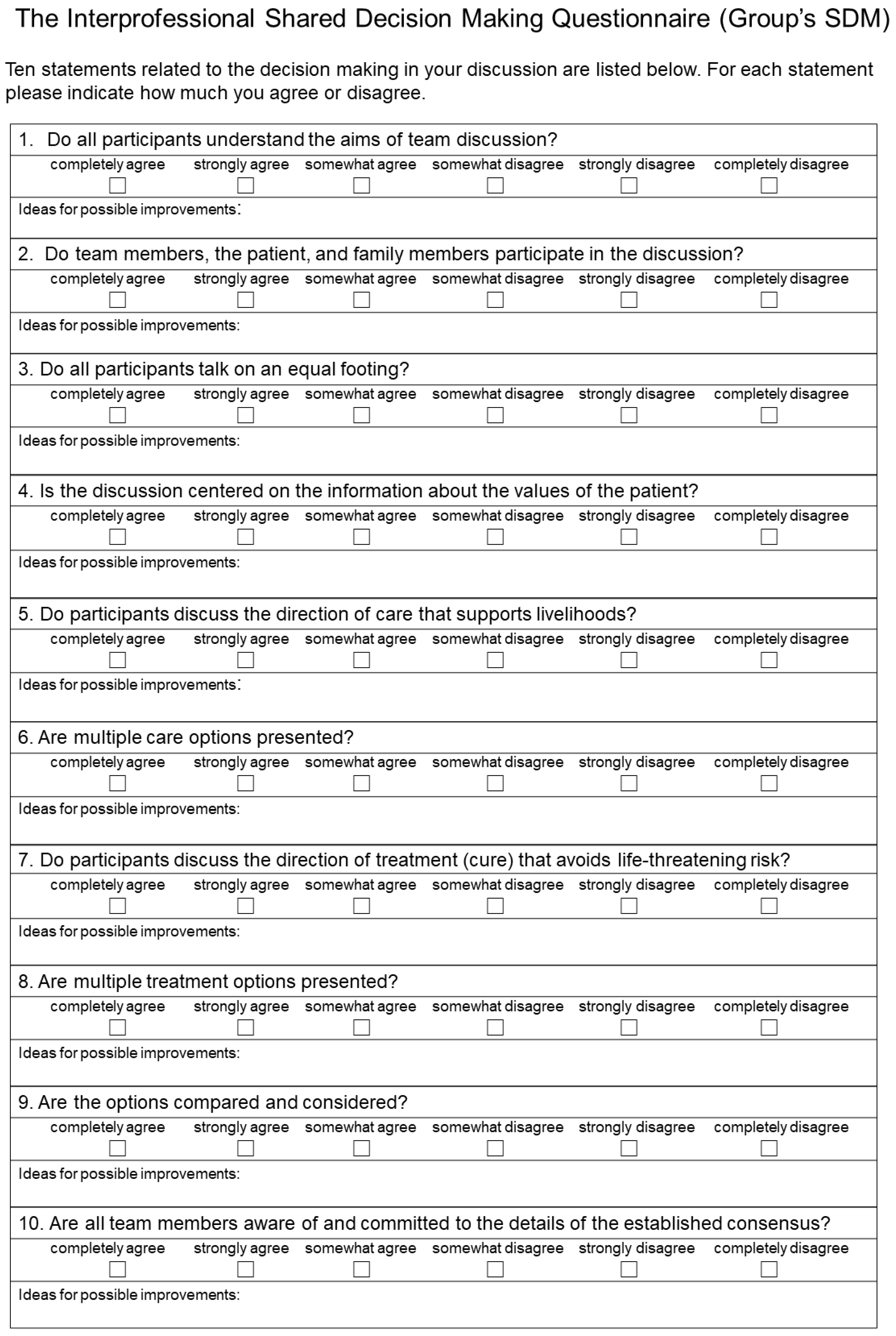
2.2.2. Interprofessional SDM Measure (Group’s SDM)
2.3. Participants and Ethical Considerations
2.4. Setting and Data Collections
2.5. Statistical Analyses
3. Results
3.1. Subsection
3.2. Exploratory Factor Analysis
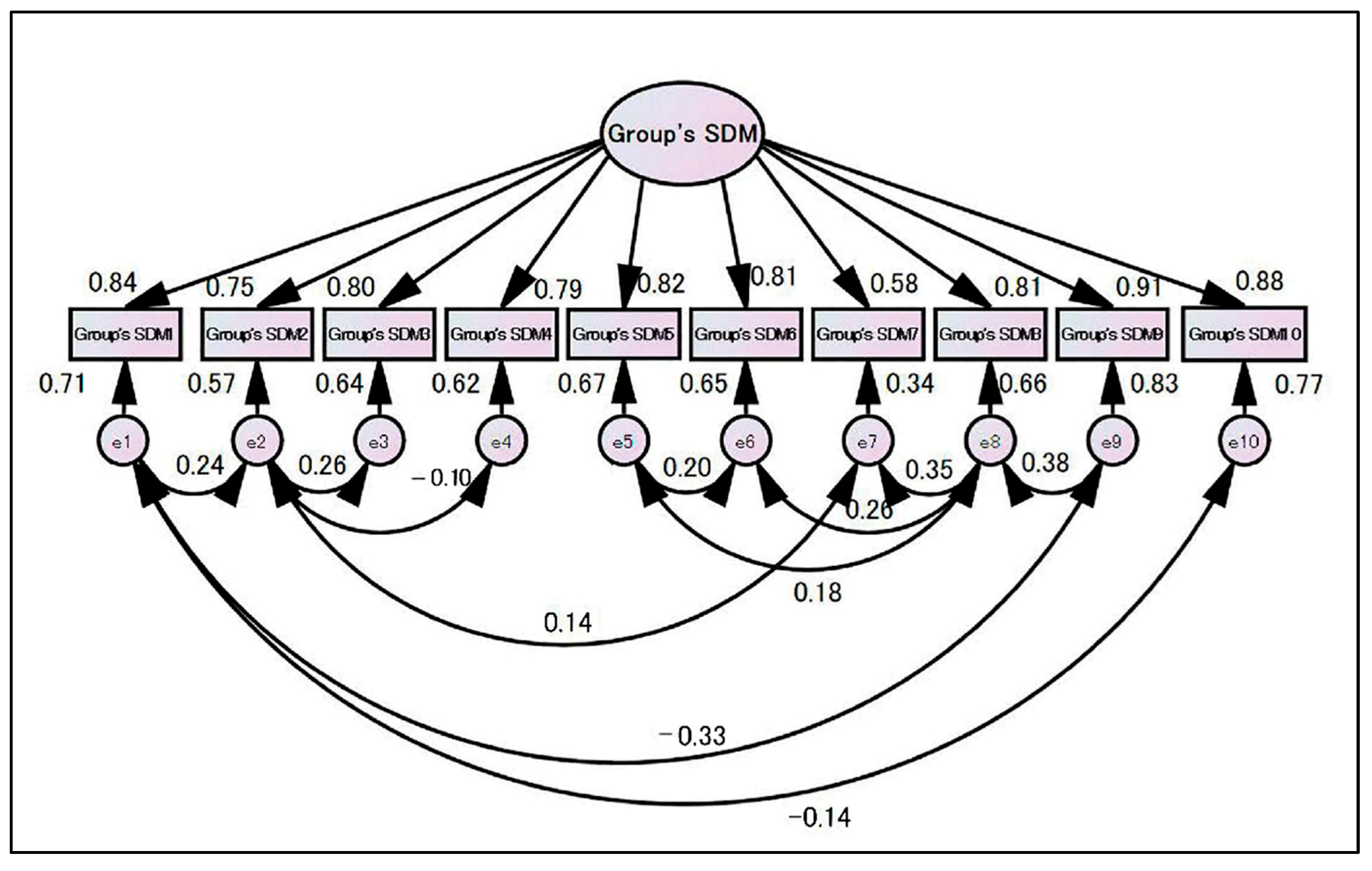
3.3. Confirmatory Factor Analysis
3.4. Reliability Analysis
4. Discussion
4.1. Group’s SDM Measure Structure
4.2. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Japan Geriatrics Society Subcommittee on End-of-Life Issues and New Coronavirus Countermeasure Team; Kuzuya, M.; Aita, K.; Katayama, Y.; Katsuya, T.; Nishikawa, M.; Hirahara, S.; Miura, H.; Yanagawa, M.; Arai, H.; et al. The Japan Geriatrics Society consensus statement “recommendations for older persons to receive the best medical and long-term care during the COVID-19 outbreak-considering the timing of advance care planning implementation. Geriatr. Gerontol. Int. 2020, 20, 1112–1119. [Google Scholar]
- Okada, K.; Tsuchiya, K.; Sakai, K.; Kuragano, T.; Uchida, A.; Tsuruya, K.; Tomo, T.; Hamada, C.; Fukagawa, M.; Kawaguchi, Y.; et al. Shared decision making for the initiation and continuation of dialysis: A proposal from the Japanese Society for Dialysis Therapy. Ren. Replace. Ther. 2021, 7, 56. [Google Scholar] [CrossRef]
- Brown, S.L.; Salmon, P. Reconciling the theory and reality of shared decision-making: A “matching” approach to practitioner leadership. Health Expect. 2019, 22, 275–283. [Google Scholar] [CrossRef]
- Bravo, P.; Harter, M.; McCaffery, K.; Giguere, A.; Hahlweg, P.; Elwyn, G. Editorial: 20 years after the start of international Shared Decision-Making activities: Is it time to celebrate? Probably… Z. Evidenz Fortbild. Qual. Gesundh. 2022, 171, 1–4. [Google Scholar] [CrossRef]
- Shared Decision Making, NICE Guideline. No. 197. Available online: https://www.ncbi.nlm.nih.gov/books/NBK572428/ (accessed on 13 October 2022).
- Coronado-Vazquez, V.; Canet-Fajas, C.; Delgado-Marroquin, M.T.; Magallon-Botaya, R.; Romero-Martin, M.; Gomez-Salgado, J. Interventions to facilitate shared decision-making using decision aids with patients in Primary Health Care: A systematic review. Medicine 2020, 99, e21389. [Google Scholar] [CrossRef]
- Shay, L.A.; Lafata, J.E. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med. Decis. Mak. 2015, 35, 114–131. [Google Scholar] [CrossRef]
- Zolnierek, K.B.; Dimatteo, M.R. Physician communication and patient adherence to treatment: A meta-analysis. Med. Care 2009, 47, 826–834. [Google Scholar] [CrossRef]
- Carmona, C.; Crutwell, J.; Burnham, M.; Polak, L. Shared decision-making: Summary of NICE guidance. BMJ 2021, 373, n1430. [Google Scholar] [CrossRef]
- Kuosmanen, L.; Hupli, M.; Ahtiluoto, S.; Haavisto, E. Patient participation in shared decision-making in palliative care—An integrative review. J. Clin. Nurs. 2021, 30, 3415–3428. [Google Scholar] [CrossRef]
- Mertens, F.; Debrulle, Z.; Lindskog, E.; Deliens, L.; Deveugele, M.; Pype, P. Healthcare professionals’ experiences of inter-professional collaboration during patient’s transfers between care settings in palliative care: A focus group study. Palliat. Med. 2021, 35, 355–366. [Google Scholar] [CrossRef]
- Bauchetet, C.; Preaubert-Sicaud, C.; Ceccaldi, J.; Farsi, F.; Donadey, F.L.; Jaulmes, D.; Altmeyer, A.; Fontaine, G.; Gineston, L.; Loureiro, E.; et al. Recommendations for the implementation of multi-professional staffs (MPS) in care services. Bull. Cancer 2020, 107, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Voogdt-Pruis, H.R.; Ras, T.; van der Dussen, L.; Benjaminsen, S.; Goossens, P.H.; Raats, I.; Boss, G.; van Hoef, E.F.M.; Lindhout, M.; Tjon, A.T.M.R.S.; et al. Improvement of shared decision making in integrated stroke care: A before and after evaluation using a questionnaire survey. BMC Health Serv. Res. 2019, 19, 936. [Google Scholar] [CrossRef] [PubMed]
- MacInnes, J.; Gadsby, E.; Reynolds, J.; Mateu, N.C.; Lette, M.; Ristl, C.; Billings, J. Exploring the Team Climate of Health and Social Care Professionals Implementing Integrated Care for Older People in Europe. Int. J. Integr. Care 2020, 20, 3. [Google Scholar] [CrossRef] [PubMed]
- Kriston, L.; Scholl, I.; Hölzel, L.; Simon, D.; Loh, A.; Härter, M. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ. Couns. 2010, 80, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Scholl, I.; Kriston, L.; Dirmaier, J.; Buchholz, A.; Härter, M. Development and psychometric properties of the Shared Decision Making Questionnaire--physician version (SDM-Q-Doc). Patient Educ. Couns. 2012, 88, 284–290. [Google Scholar] [CrossRef]
- Elwyn, G.; Hutchings, H.; Edwards, A.; Rapport, F.; Wensing, M.; Cheung, W.Y.; Grol, R. The OPTION scale: Measuring the extent that clinicians involve patients in decision-making tasks. Health Expect. 2005, 8, 34–42. [Google Scholar] [CrossRef]
- Goto, Y.; Miura, H.; Son, D.; Arai, H.; Kriston, L.; Scholl, I.; Härter, M.; Sato, K.; Kusaba, T. Psychometric Evaluation of the Japanese 9-Item Shared Decision-Making Questionnaire and Its Association with Decision Conflict and Patient Factors in Japanese Primary Care. JMA J. 2020, 3, 208–215. [Google Scholar]
- Goto, Y.; Miura, H.; Son, D.; Scholl, I.; Kriston, L.; Harter, M.; Sato, K.; Kusaba, T.; Arai, H. Association between physicians’ and patients’ perspectives of shared decision making in primary care settings in Japan: The impact of environmental factors. PLoS ONE 2021, 16, e0246518. [Google Scholar] [CrossRef]
- Goto, Y.; Yamaguchi, Y.; Onishi, J.; Arai, H.; Harter, M.; Scholl, I.; Kriston, L.; Miura, H. Adapting the patient and physician versions of the 9-item shared decision making questionnaire for other healthcare providers in Japan. BMC Med. Inform. Decis. Mak. 2021, 21, 314. [Google Scholar] [CrossRef]
- Korner, M.; Ehrhardt, H.; Steger, A.K.; Bengel, J. Interprofessional SDM train-the-trainer program “Fit for SDM”: Provider satisfaction and impact on participation. Patient Educ. Couns. 2012, 89, 122–128. [Google Scholar] [CrossRef]
- Goto, Y.; Miura, H.; Yamaguchi, Y.; Onishi, J. Evaluation of an advance care planning training program for practice professionals in Japan incorporating shared decision making skills training: A prospective study of a curricular intervention. BMC Palliat. Care 2022, 21, 135. [Google Scholar]
- Makoul, G.; Clayman, M.L. An integrative model of shared decision making in medical encounters. Patient Educ. Couns. 2006, 60, 301–312. [Google Scholar] [CrossRef]
- University Medical Center Hamburg-Eppendorf. SDM-Q-9 / SDM-Q-Doc. The 9-Item Shared Decision Making Questionnaire. Available online: http://www.patient-als-partner.de/index.php?article_id=20&clang=2/ (accessed on 13 October 2022).
- Goto, Y.; Miura, H. Using the Soft Systems Methodology to Link Healthcare and Long-Term Care Delivery Systems: A Case Study of Community Policy Coordinator Activities in Japan. Int. J. Environ. Res. Public Health 2022, 19, 8462. [Google Scholar] [CrossRef]
- Lidwine, B.M.; Cecilia, A.C.P.; Donald, L.P.; Jordi, A.; Lex, M.B.; Henrica, C.W.d.V.; Caroline, B.T. COSMIN Study Design Checklist for Patient-Reported Outcome Measurement Instruments Version July 2019. Available online: https://www.cosmin.nl/wp-content/uploads/COSMIN-study-designing-checklist_final.pdf (accessed on 13 October 2022).
- Kaiser, H. An index of factorial simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Charness, G.; Sutter, M. Groups make better self-interested decisions. J. Econ. Perspect. 2012, 26, 157–176. [Google Scholar] [CrossRef]
- Patel, M.M.; Moseley, T.W.; Nia, E.S.; Perez, F.; Kapoor, M.M.; Whitman, G.J. Team Science: A Practical Approach to Starting Collaborative Projects. J. Breast Imaging 2021, 3, 721–726. [Google Scholar] [CrossRef]
- Tebes, J.K.; Thai, N.D. Interdisciplinary team science and the public: Steps toward a participatory team science. Am. Psychol. 2018, 73, 549–562. [Google Scholar] [CrossRef]
- Steele, K.; Stefánsson, H.O. Decision Theory. The Stanford Encyclopedia of Philosophy; Stanford University: Stanford, CA, USA, 2015. [Google Scholar]
- Shafir, E.; LeBoeuf, R.A. Rationality. Annu. Rev. Psychol. 2002, 53, 491–517. [Google Scholar] [CrossRef]
- Inthorn, J. Fuzziness and Medicine: Philosophical Reflections and Application Systems in Health Care. A Companion Volume to Sadegh-Zadeh’s Handbook of Analytical Philosophy of Medicine; Springer: Berlin/Heidelberg, Germany, 2013; pp. 85–95. [Google Scholar]
- Hsiao, C.Y.; Wu, J.C.; Lin, P.C.; Yang, P.Y.; Liao, F.; Guo, S.L.; Hou, W.H. Effectiveness of interprofessional shared decision-making training: A mixed-method study. Patient Educ. Couns. 2022, 105, 3287–3297. [Google Scholar] [CrossRef]
- Bennett, L.M.; Gadlin, H. Collaboration and Team Science: From Theory to Practice. J. Investig. Med. 2012, 60, 768–775. [Google Scholar] [CrossRef]
- Hoefel, L.; O’Connor, A.M.; Lewis, K.B.; Boland, L.; Sikora, L.; Hu, J.; Stacey, D. 20th Anniversary Update of the Ottawa Decision Support Framework Part 1: A Systematic Review of the Decisional Needs of People Making Health or Social Decisions. Med. Decis. Mak. 2020, 40, 555–581. [Google Scholar] [CrossRef]


| Specialization | Number of People | Percentage (%) |
|---|---|---|
| Nurse | 86 | 50 |
| Physician | 28 | 16 |
| MSW | 18 | 11 |
| Care Manager | 14 | 8 |
| Therapist | 8 | 5 |
| Counselor | 4 | 2 |
| Public Health Nurse | 4 | 2 |
| Pharmacist | 3 | 2 |
| Care Worker | 2 | 1 |
| Registered Dietitian | 1 | 1 |
| Other | 3 | 2 |
| Total | 171 | 100 |
| Years of Clinical Experience as a Specialist | Number of People | Percentage (%) |
|---|---|---|
| <5 years | 20 | 12 |
| ≥5 to <10 years | 20 | 12 |
| ≥10 to <15 years | 24 | 14 |
| ≥15 to <20 years | 33 | 19 |
| ≥20 to <25 years | 37 | 21 |
| ≥25 years | 37 | 22 |
| Total | 171 | 100 |
| Median | Mean | SD | Minimum | Maximum | Corrected Item’s Total Correlation Coefficient | |
|---|---|---|---|---|---|---|
| Group’s SDM 1 | 8.00 | 6.96 | 2.404 | 0 | 10 | 0.809 |
| Group’s SDM 2 | 8.00 | 7.38 | 2.163 | 2 | 10 | 0.77 |
| Group’s SDM 3 | 8.00 | 7.97 | 1.994 | 2 | 10 | 0.773 |
| Group’s SDM 4 | 8.00 | 7.85 | 2.306 | 0 | 10 | 0.742 |
| Group’s SDM 5 | 8.00 | 7.15 | 2.389 | 0 | 10 | 0.813 |
| Group’s SDM 6 | 8.00 | 7.49 | 2.213 | 0 | 10 | 0.801 |
| Group’s SDM 7 | 6.00 | 6.44 | 2.366 | 0 | 10 | 0.605 |
| Group’s SDM 8 | 8.00 | 7.22 | 2.164 | 0 | 10 | 0.842 |
| Group’s SDM 9 | 8.00 | 7.99 | 2.028 | 0 | 10 | 0.861 |
| Group’s SDM 10 | 8.00 | 7.50 | 2.292 | 0 | 10 | 0.827 |
| Factor Loadings | Communality | |
|---|---|---|
| Group’s SDM 1 | 0.83 | 0.69 |
| Group’s SDM 2 | 0.79 | 0.66 |
| Group’s SDM 3 | 0.80 | 0.67 |
| Group’s SDM 4 | 0.77 | 0.61 |
| Group’s SDM 5 | 0.84 | 0.68 |
| Group’s SDM 6 | 0.82 | 0.69 |
| Group’s SDM 7 | 0.62 | 0.48 |
| Group’s SDM 8 | 0.86 | 0.79 |
| Group’s SDM 9 | 0.89 | 0.82 |
| Group’s SDM 10 | 0.85 | 0.72 |
| Eigenvalue | 6.90 | |
| % of Total variance | 68.94 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goto, Y.; Miura, H. Validation of the Novel Interprofessional Shared Decision-Making Questionnaire to Facilitate Multidisciplinary Team Building in Patient-Centered Care. Int. J. Environ. Res. Public Health 2022, 19, 15349. https://doi.org/10.3390/ijerph192215349
Goto Y, Miura H. Validation of the Novel Interprofessional Shared Decision-Making Questionnaire to Facilitate Multidisciplinary Team Building in Patient-Centered Care. International Journal of Environmental Research and Public Health. 2022; 19(22):15349. https://doi.org/10.3390/ijerph192215349
Chicago/Turabian StyleGoto, Yuko, and Hisayuki Miura. 2022. "Validation of the Novel Interprofessional Shared Decision-Making Questionnaire to Facilitate Multidisciplinary Team Building in Patient-Centered Care" International Journal of Environmental Research and Public Health 19, no. 22: 15349. https://doi.org/10.3390/ijerph192215349
APA StyleGoto, Y., & Miura, H. (2022). Validation of the Novel Interprofessional Shared Decision-Making Questionnaire to Facilitate Multidisciplinary Team Building in Patient-Centered Care. International Journal of Environmental Research and Public Health, 19(22), 15349. https://doi.org/10.3390/ijerph192215349






