Parents’ Experiences of Direct and Indirect Implications of Sleep Quality on the Health of Children with ADHD: A Qualitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
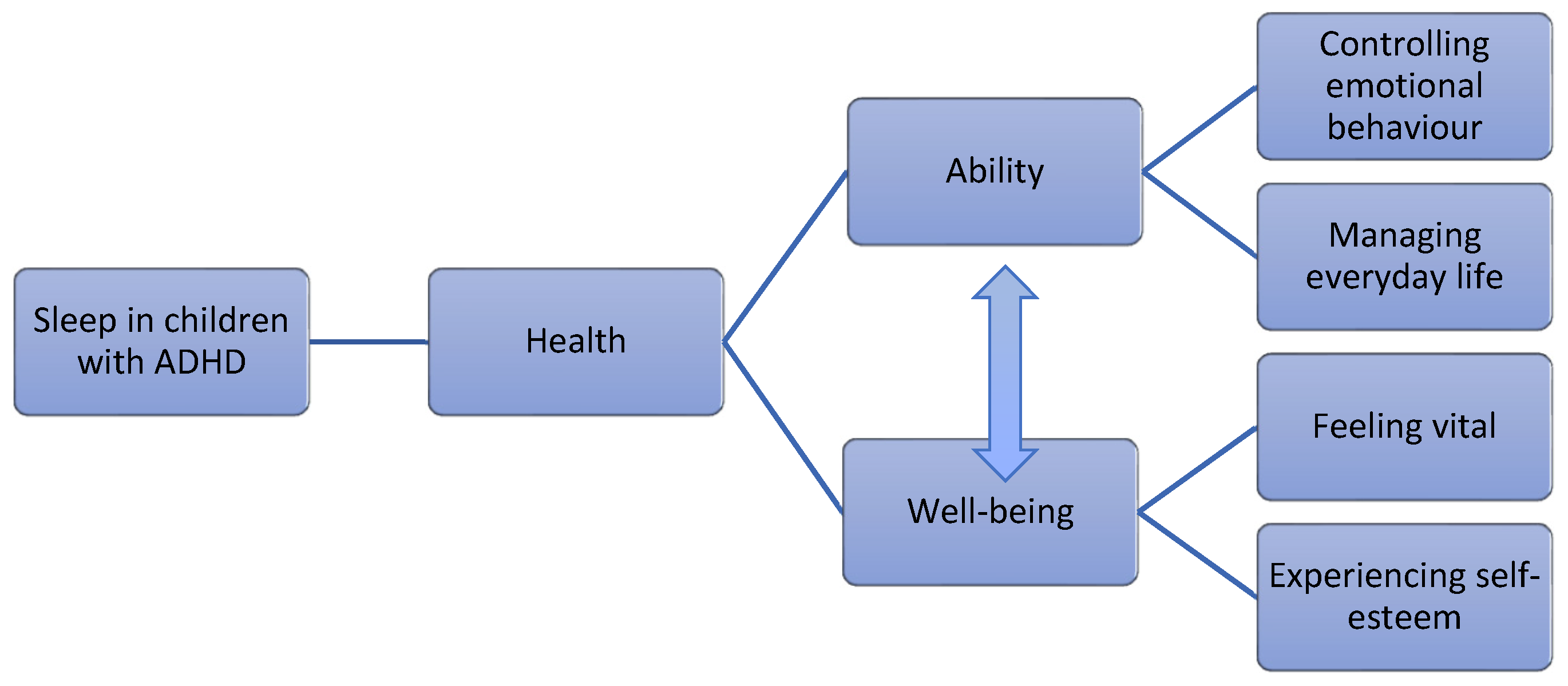
3. Results
3.1. Ability
3.1.1. Controlling Emotional Behaviour
If she hasn’t slept well, you notice that she’s more tired and grumpy. Not as cooperative. She doesn’t want to do as we say. But then she’s very, very stubborn in any case, most of the time. It gets 10 times worse if she hasn’t slept properly.(Parent no. 7)
The days go by. It’s not a constant battle all the time about what to do or any argument; rather, you complement each other more at home, including the children. NN can be involved in activities that one has planned for oneself, it’s not just focusing and planning around him, because that’s how it was for a while. You prepared everything so it wouldn’t turn into a conflict or so he wouldn’t get angry. Now that he can handle setbacks, it’s easier to slow down, oneself, and take it a bit more as it comes.(Parent no. 21)
I think that it (sleep) means a lot, I think that with poorer sleep he would have been angrier, and when he’s angrier he gets more hyperactive, and then he gets unsettled and then he’ll do something stupid, and then it creates a bit of anxiety, so I think it has a great impact.(Parent no. 17)
She loses touch with reality completely. It’s all about her at that moment, everything is focused on her. She can’t consider anyone else in that situation, it’s just panic all over. It’s obvious when you’re looking at her.(Parent no. 10)
3.1.2. Managing Everyday Life
You can do more things together because he has more strength, more energy and a greater desire to do things. A lot of the time he wants to come along when you’re going somewhere. I can’t take more than a few steps outside the door before “Mum, I want to come along”. He wants to help out more. It used to be a burden having to do a lot of things by ourselves. Now we get a break when he wants to help out. Come along to the shop and carry groceries and things like that.(Parent no. 15)
Even if he is unsettled the next day, he would probably have been even more worried if he hadn’t had any sleep. So, it still feels like you’re helping, helping him with mental recovery and balance, as much balance that you can have when you’re seven and have ADHD, but it becomes a tool that can help him to function better.(Parent no. 17)
I think that he would be able to manage the surrounding world. Have better margins, and better ability to concentrate with better sleep. I’m thinking that it’s connected to learning as well. I think sleep is really important. So, all the bits of the puzzle, so to speak. You must combine all the factors to make it work.(Parent no. 2)
3.2. Well-Being
3.2.1. Feeling Vital
He falls asleep at a reasonable time and gets up by himself in the morning and sort of wakes me up and asks when he has to go to school. He thinks that school was fun today. Yesterday he said that school is fun. One can tell that something has changed.(Parent no. 12)
I think that, at school, she holds it all together, as well as she can. But when she gets home, then she’s ready to drop. So it’s mainly at home that it will come out. But I definitely think it has an effect, everything is much harder in a way. With concentration and holding it together and interacting with friends, everything gets so much harder.(Parent no. 8)
You can sit and talk to him in different way, just like he has woken up, somehow. Matured, probably, it feels like that. But sensing that sleep affects so much as a whole, both brain and body. That he is present in a different way.(Parent no. 3)
[She] started to hang out so much more with friends. Before it was more like, after school, she just wanted to lie in bed and take it easy and play a little bit. But now she hardly has time to sit still, she wants to do things.(Parent no. 9)
But if you’re not really tired, then it’s easy for your thoughts to wander, it spins and spins and you keep thinking, then you can’t really sleep. My experience is that if you exhaust yourself properly and let the body work regularly you will fall asleep easier, it will happen quicker, and you’ll sleep better. It’s a win-win.(Parent no. 19)
I can see above all that his worry is…that is what I’m basing this on. That it’s such a difference. […] It’s gone. It’s kind of, well, almost completely gone all day, I can say. Otherwise, he can be, not what I would call worried, but energy stressed. But this worrying over everything.(Parent no. 3)
He used to move around a lot in the bed, and then he was completely knackered at night, and then we had a messy night. And then we had that cycle every day, every night.(Parent no. 17)
3.2.2. Experiencing Self-Esteem
But it’s not that many days now that you get the call from school anymore. […]. It used to be more often and then it was really, we have even sat down with the school, and what are we going to do so she can cope all day.(Parent no. 5)
Yes, he loves to play with Lego, for example. After getting a good night’s sleep he can sit by himself for ages, but if he’s tired or hungry, then he gets grumpy over the slightest thing. He has a harder time understanding the instructions and finds it harder to focus. You can see, when he’s alert, that he thinks things over before letting the feelings come up.(Parent no. 14)
But one thing that has become problematic is that everyone is having sleepovers more often. He wanted to have a sleepover but didn’t manage to do it. It has become difficult for him. It has really been driving this, that we’re now trying to get him closer to being able to fall asleep by himself.(Parent no. 4)
4. Discussion
4.1. Ability
4.2. Well-Being
4.3. Methodological Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Medic, G.; Wille, M.; Hemels, M. Short- and Long-Term Health Consequences of Sleep Disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Hershner, S. Sleep and Academic Performance: Measuring the Impact of Sleep. Curr. Opin. Behav. Sci. 2020, 33, 51–56. [Google Scholar] [CrossRef]
- Lemola, S.; Räikkönen, K.; Scheier, M.F.; Matthews, K.A.; Pesonen, A.-K.; Heinonen, K.; Lahti, J.; Komsi, N.; Paavonen, J.E.; Kajantie, E. Sleep Quantity, Quality and Optimism in Children: Sleep and Optimism in Children. J. Sleep Res. 2011, 20, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Grünwald, J.; Schlarb, A. Relationship between Subtypes and Symptoms of ADHD, Insomnia, and Nightmares in Connection with Quality of Life in Children. Neuropsychiatr. Dis. Treat. 2017, 13, 2341–2350. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, L.J.; Wainer, A.; Engstrom, E.; Pepa, L.; Mindell, J.A. Seeing the Whole Elephant: A Scoping Review of Behavioral Treatments for Pediatric Insomnia. Sleep Med. Rev. 2021, 56, 101410. [Google Scholar] [CrossRef] [PubMed]
- Stormark, K.M.; Fosse, H.E.; Pallesen, S.; Hysing, M. The Association between Sleep Problems and Academic Performance in Primary School-Aged Children: Findings from a Norwegian Longitudinal Population-Based Study. PLoS ONE 2019, 14, e0224139. [Google Scholar] [CrossRef]
- Martin, C.A.; Papadopoulos, N.; Chellew, T.; Rinehart, N.J.; Sciberras, E. Associations between Parenting Stress, Parent Mental Health and Child Sleep Problems for Children with ADHD and ASD: Systematic Review. Res. Dev. Disabil. 2019, 93, 103463. [Google Scholar] [CrossRef] [PubMed]
- Bondopadhyay, U.; Diaz-Orueta, U.; Coogan, A.N. A Systematic Review of Sleep and Circadian Rhythms in Children with Attention Deficit Hyperactivity Disorder. J. Atten. Disord. 2022, 26, 149–224. [Google Scholar] [CrossRef]
- Becker, S.P.; Cusick, C.N.; Sidol, C.A.; Epstein, J.N.; Tamm, L. The Impact of Comorbid Mental Health Symptoms and Sex on Sleep Functioning in Children with ADHD. Eur. Child Adolesc. Psychiatry 2018, 27, 353–365. [Google Scholar] [CrossRef]
- Sung, V.; Hiscock, H.; Sciberras, E.; Efron, D. Sleep Problems in Children With Attention-Deficit/Hyperactivity Disorder: Prevalence and the Effect on the Child and Family. Arch. Pediatr. Adolesc. Med. 2008, 162, 336. [Google Scholar] [CrossRef]
- Quach, J.; Hiscock, H.; Wake, M. Sleep Problems and Mental Health in Primary School New Entrants: Cross-Sectional Community-Based Study: Sleep and Mental Health at School Entry. J. Paediatr. Child Health 2012, 48, 1076–1081. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Zimmerman, A.W. Sleep in Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder. Semin. Pediatr. Neurol. 2015, 22, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.P.; Froehlich, T.E.; Epstein, J.N. Effects of Methylphenidate on Sleep Functioning in Children with Attention-Deficit/Hyperactivity Disorder. J. Dev. Behav. Pediatr. 2016, 37, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Blunden, S.L.; Milte, C.M.; Sinn, N. Diet and Sleep in Children with Attention Deficit Hyperactivity Disorder: Preliminary Data in Australian Children. J. Child Health Care 2011, 15, 14–24. [Google Scholar] [CrossRef]
- San Mauro Martín, I.; Blumenfeld Olivares, J.A.; Garicano Vilar, E.; Echeverry López, M.; García Bernat, M.; Quevedo Santos, Y.; Blanco López, M.; Elortegui Pascual, P.; Borregon Rivilla, E.; Rincón Barrado, M. Nutritional and Environmental Factors in Attention-Deficit Hyperactivity Disorder (ADHD): A Cross-Sectional Study. Nutr. Neurosci. 2018, 21, 641–647. [Google Scholar] [CrossRef]
- Tong, L.; Xiong, X.; Tan, H. Attention-Deficit/Hyperactivity Disorder and Lifestyle-Related Behaviors in Children. PLoS ONE 2016, 11, e0163434. [Google Scholar] [CrossRef]
- Malhotra, S.; Kancherla, B.S. Continued Challenges for Parents and Clinicians in Maintaining Sleep Health for Children with ADHD during the COVID-19 Pandemic. J. Clin. Sleep Med. 2021, 17, 1749–1750. [Google Scholar] [CrossRef]
- Tegnell, A. The Swedish public health response to COVID-19. APMIS 2021, 129, 320–323. [Google Scholar] [CrossRef]
- Kimland, E.E.; Bardage, C.; Collin, J.; Järleborg, A.; Ljung, R.; Iliadou, A.N. Pediatric Use of Prescribed Melatonin in Sweden 2006–2017: A Register Based Study. Eur. Child Adolesc. Psychiatry 2021, 30, 1339–1350. [Google Scholar] [CrossRef]
- Abdelgadir, I.S.; Gordon, M.A.; Akobeng, A.K. Melatonin for the Management of Sleep Problems in Children with Neurodevelopmental Disorders: A Systematic Review and Meta-Analysis. Arch. Dis. Child. 2018, 103, 1155–1162. [Google Scholar] [CrossRef]
- Nikles, J.; Mitchell, G.K.; de Miranda Araújo, R.; Harris, T.; Heussler, H.S.; Punja, S.; Vohra, S.; Senior, H.E.J. A Systematic Review of the Effectiveness of Sleep Hygiene in Children with ADHD. Psychol. Health Med. 2020, 25, 497–518. [Google Scholar] [CrossRef] [PubMed]
- Bériault, M.; Turgeon, L.; Labrosse, M.; Berthiaume, C.; Verreault, M.; Berthiaume, C.; Godbout, R. Comorbidity of ADHD and Anxiety Disorders in School-Age Children: Impact on Sleep and Response to a Cognitive-Behavioral Treatment. J. Atten. Disord. 2018, 22, 414–424. [Google Scholar] [CrossRef] [PubMed]
- Beresford, B.; McDaid, C.; Parker, A.; Scantlebury, A.; Spiers, G.; Fairhurst, C.; Hewitt, C.; Wright, K.; Dawson, V.; Elphick, H.; et al. Pharmacological and Non-Pharmacological Interventions for Non-Respiratory Sleep Disturbance in Children with Neurodisabilities: A Systematic Review. Health Technol. Assess. 2018, 22, 1–296. [Google Scholar] [CrossRef] [PubMed]
- Martins, R.; Scalco, J.C.; Junior, G.J.F.; da Silva Gerente, J.G.; da Lapa Costa, M.; Beltrame, T.S. Sleep Disturbance in Children with Attention-Deficit Hyperactivity Disorder: A Systematic Review. Sleep Sci. 2019, 12, 295. [Google Scholar] [PubMed]
- Graneheim, U.H.; Lindgren, B.-M.; Lundman, B. Methodological Challenges in Qualitative Content Analysis: A Discussion Paper. Nurse Educ. Today 2017, 56, 29–34. [Google Scholar] [CrossRef]
- Tengland, P.-A. A Two-Dimensional Theory of Health. Theor. Med. Bioeth. 2007, 28, 257–284. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Larsson, I.; Aili, K.; Nygren, J.M.; Johansson, P.; Jarbin, H.; Svedberg, P. SLEEP: Intervention with Weighted Blankets for Children with Attention Deficit Hyperactivity Disorder (ADHD) and Sleep Problems: Study Protocol for a Randomised Control Trial. BMJ Open 2022, 12, e047509. [Google Scholar] [CrossRef]
- World Medical Association (WMA). Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. Jahrb. Wiss. Ethik 2013, 14, 233–238. [Google Scholar]
- Swedish Research Council. Good Research Practice. 2017. Available online: https://www.vr.se/download/18.5639980c162791bbfe697882/1555334908942/Good-Research-Practice_VR_2017.pdf (accessed on 13 September 2022).
- Sanabra, M.; Gómez-Hinojosa, T.; Grau, N.; Alda, J.A. Deficient Emotional Self-Regulation and Sleep Problems in ADHD with and without Pharmacological Treatment. J. Atten. Disord. 2022, 26, 426–433. [Google Scholar] [CrossRef]
- Bunford, N.; Evans, S.W.; Wymbs, F. ADHD and Emotion Dysregulation Among Children and Adolescents. Clin. Child Fam. Psychol. Rev. 2015, 18, 185–217. [Google Scholar] [CrossRef] [PubMed]
- Mancini, V.O.; Althorpe, K.E.; Chen, W. Do Motor Coordination and Sleep Difficulties Predict Peer Functioning in Children and Adolescents with Attention-deficit and Hyperactivity Disorder after Accounting for Existing ADHD Symptomology? Br. J. Dev. Psychol. 2020, 38, 442–457. [Google Scholar] [CrossRef] [PubMed]
- Hoza, B. Peer Functioning in Children With ADHD. J. Pediatr. Psychol. 2007, 32, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Mrug, S.; Molina, B.S.G.; Hoza, B.; Gerdes, A.C.; Hinshaw, S.P.; Hechtman, L.; Arnold, L.E. Peer Rejection and Friendships in Children with Attention-Deficit/Hyperactivity Disorder: Contributions to Long-Term Outcomes. J. Abnorm. Child Psychol. 2012, 40, 1013–1026. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.P.; Langberg, J.M.; Evans, S.W. Sleep Problems Predict Comorbid Externalizing Behaviors and Depression in Young Adolescents with Attention-Deficit/Hyperactivity Disorder. Eur. Child Adolesc. Psychiatry 2015, 24, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Keshavarzi, Z.; Bajoghli, H.; Mohamadi, M.R.; Salmanian, M.; Kirov, R.; Gerber, M.; Holsboer-Trachsler, E.; Brand, S. In a Randomized Case–Control Trial with 10-Years Olds Suffering from Attention Deficit/Hyperactivity Disorder (ADHD) Sleep and Psychological Functioning Improved during a 12-Week Sleep-Training Program. World J. Biol. Psychiatry 2014, 15, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Wehmeier, P.M.; Schacht, A.; Barkley, R.A. Social and Emotional Impairment in Children and Adolescents with ADHD and the Impact on Quality of Life. J. Adolesc. Health 2010, 46, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Maoz, H.; Gvirts, H.Z.; Sheffer, M.; Bloch, Y. Theory of Mind and Empathy in Children with ADHD. J. Atten. Disord. 2019, 23, 1331–1338. [Google Scholar] [CrossRef]
- Arnold, L.E.; Hodgkins, P.; Kahle, J.; Madhoo, M.; Kewley, G. Long-Term Outcomes of ADHD: Academic Achievement and Performance. J. Atten. Disord. 2020, 24, 73–85. [Google Scholar] [CrossRef]
- Newark, P.E.; Elsässer, M.; Stieglitz, R.-D. Self-Esteem, Self-Efficacy, and Resources in Adults With ADHD. J. Atten. Disord. 2016, 20, 279–290. [Google Scholar] [CrossRef]
- García Bacete, F.J.; Marande, G.; Mikami, A.Y. Evaluation of a Multi-Component and Multi-Agent Intervention to Improve Classroom Social Relationships among Early Elementary School-Age Children. J. Sch. Psychol. 2019, 77, 124–138. [Google Scholar] [CrossRef]
- Sciberras, E.; Lycett, K.; Efron, D.; Mensah, F.; Gerner, B.; Hiscock, H. Anxiety in Children With Attention-Deficit/Hyperactivity Disorder. Pediatrics 2014, 133, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Wild, L.G.; Flisher, A.J.; Bhana, A.; Lombard, C. Associations among Adolescent Risk Behaviours and Self-Esteem in Six Domains: Self-Esteem and Adolescent Risk Behaviours. J. Child Psychol. Psychiatry 2004, 45, 1454–1467. [Google Scholar] [CrossRef] [PubMed]
- Shenton, A.K. Strategies for Ensuring Trustworthiness in Qualitative Research Projects. Educ. Inf. 2004, 22, 63–75. [Google Scholar] [CrossRef]
| Variable | Parents (n = 21) |
|---|---|
| Sex, female/male (n) | 16/5 |
| Age in years, median (range) | 39 (32–48) |
| Civil Status, co-habiting/living alone (n) | 17/4 |
| Educational level, lower secondary/upper secondary/university (n) | 2/8/11 |
| Employment, full time/part-time/unemployed/sick leave (n) | 12/7/1/1 |
| Native-born/foreign-born (n) | 19/2 |
| Place of residence, city/countryside (n) | 7/14 |
| Age of the child in years, median (range) | 9 (6–13) |
| Sex of the child, female/male (n) | 8/11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harris, U.; Svedberg, P.; Aili, K.; Nygren, J.M.; Larsson, I. Parents’ Experiences of Direct and Indirect Implications of Sleep Quality on the Health of Children with ADHD: A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 15099. https://doi.org/10.3390/ijerph192215099
Harris U, Svedberg P, Aili K, Nygren JM, Larsson I. Parents’ Experiences of Direct and Indirect Implications of Sleep Quality on the Health of Children with ADHD: A Qualitative Study. International Journal of Environmental Research and Public Health. 2022; 19(22):15099. https://doi.org/10.3390/ijerph192215099
Chicago/Turabian StyleHarris, Ulrika, Petra Svedberg, Katarina Aili, Jens M. Nygren, and Ingrid Larsson. 2022. "Parents’ Experiences of Direct and Indirect Implications of Sleep Quality on the Health of Children with ADHD: A Qualitative Study" International Journal of Environmental Research and Public Health 19, no. 22: 15099. https://doi.org/10.3390/ijerph192215099
APA StyleHarris, U., Svedberg, P., Aili, K., Nygren, J. M., & Larsson, I. (2022). Parents’ Experiences of Direct and Indirect Implications of Sleep Quality on the Health of Children with ADHD: A Qualitative Study. International Journal of Environmental Research and Public Health, 19(22), 15099. https://doi.org/10.3390/ijerph192215099







