Development of a Japanese Healthy Diet Index: The Fukushima Health Management Survey 2011
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Dietary Intake Assessment
2.3. Statistical Analysis
2.3.1. Missing Dietary Data
2.3.2. Polychoric Coefficients for Food Items
2.3.3. Derivation of Dietary Patterns
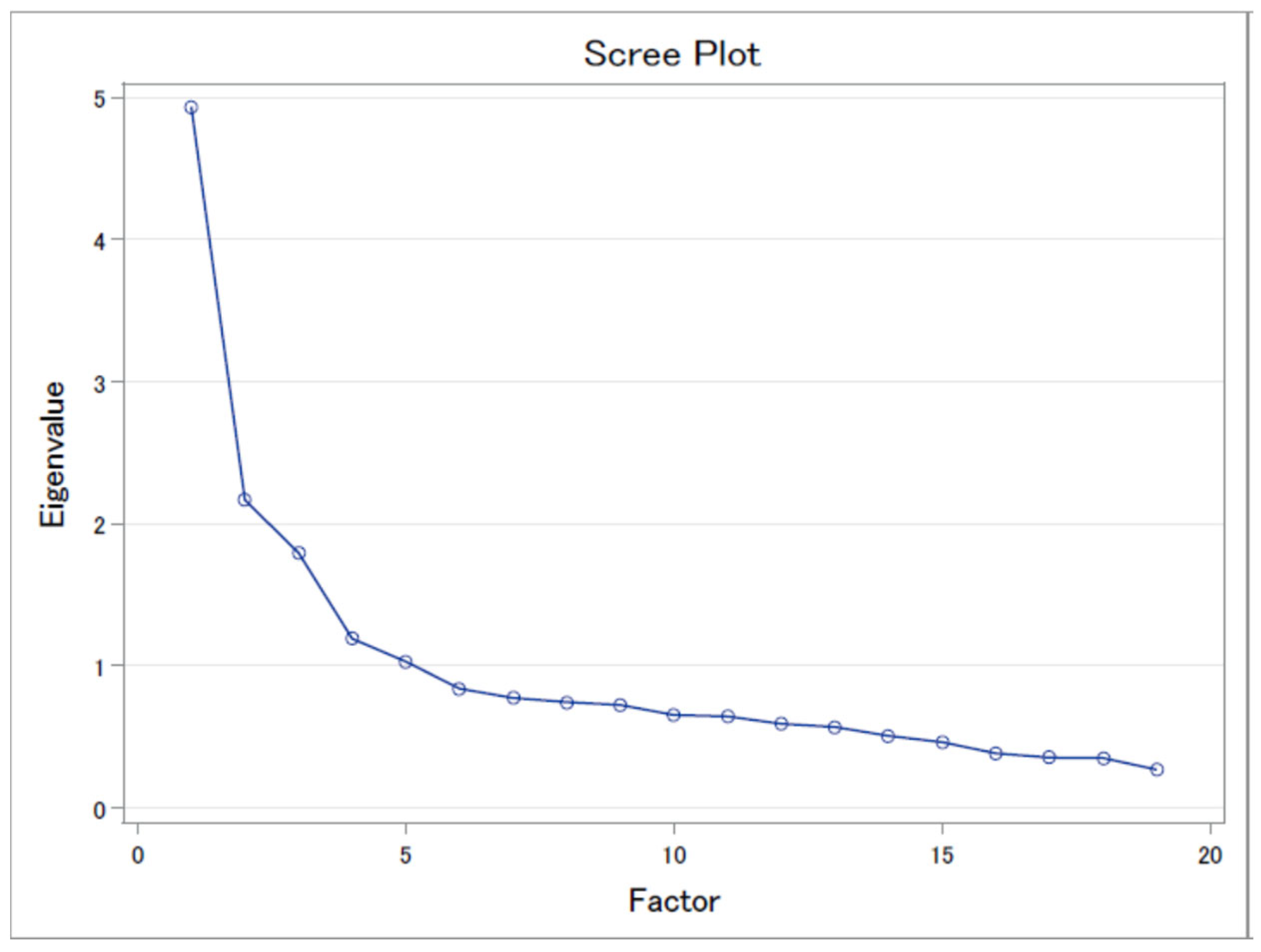
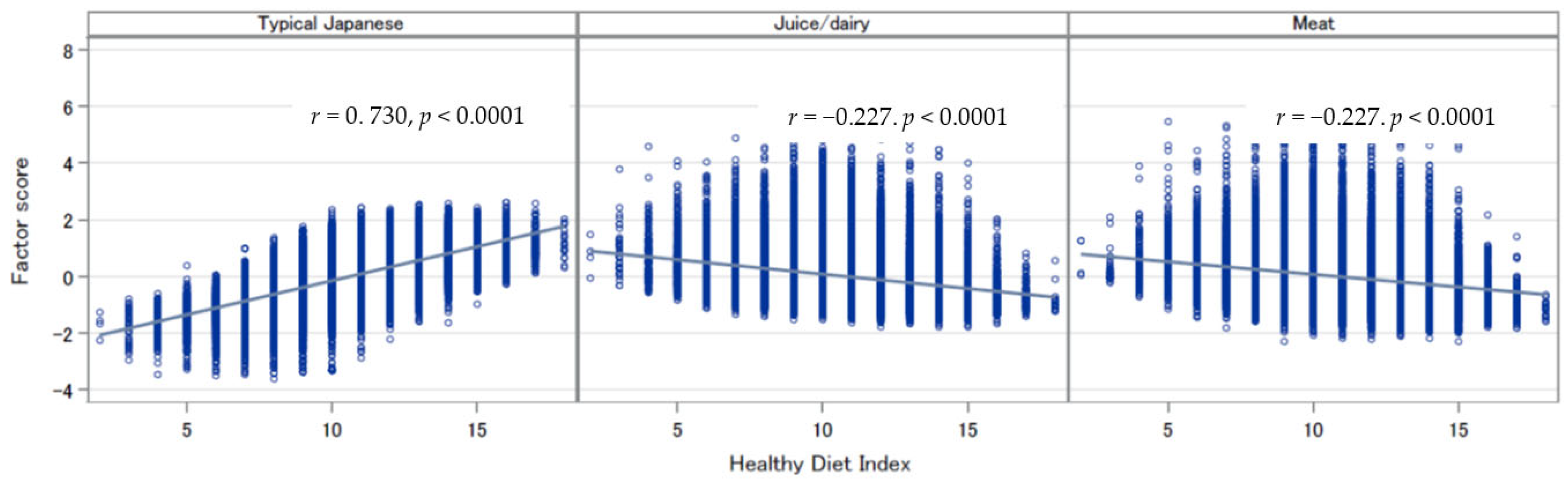
2.3.4. HDI
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schwingshackl, L.; Bogensberger, B.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet 2018, 118, 74–100.e11. [Google Scholar] [CrossRef] [PubMed]
- Lassale, C.; Batty, G.D.; Baghdadli, A.; Jacka, F.; Sanchez-Villegas, A.; Kivimaki, M.; Akbaraly, T. Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol. Psychiatry 2019, 24, 965–986. [Google Scholar] [CrossRef] [PubMed]
- Shivappa, N.; Godos, J.; Hebert, J.R.; Wirth, M.D.; Piuri, G.; Speciani, A.F.; Grosso, G. Dietary Inflammatory Index and Colorectal Cancer Risk-A Meta-Analysis. Nutrients 2017, 9, 1043. [Google Scholar] [CrossRef] [PubMed]
- Petimar, J.; Smith-Warner, S.A.; Fung, T.T.; Rosner, B.; Chan, A.T.; Hu, F.B.; Giovannucci, E.L.; Tabung, F.K. Recommendation-based dietary indexes and risk of colorectal cancer in the Nurses' Health Study and Health Professionals Follow-up Study. Am. J. Clin. Nutr. 2018, 108, 1092–1103. [Google Scholar] [CrossRef] [PubMed]
- Chiuve, S.E.; Fung, T.T.; Rimm, E.B.; Hu, F.B.; McCullough, M.L.; Wang, M.; Stampfer, M.J.; Willett, W.C. Alternative dietary indices both strongly predict risk of chronic disease. J. Nutr. 2012, 142, 1009–1018. [Google Scholar] [CrossRef]
- Lim, K.Y.; Chen, I.C.; Chan, Y.C.; Cheong, I.F.; Wang, Y.Y.; Jian, Z.R.; Lee, S.D.; Chou, C.C.; Yang, F.L. Novel Healthy Eating Index to Examine Daily Food Guides Adherence and Frailty in Older Taiwanese. Nutrients 2021, 13, 4210. [Google Scholar] [CrossRef]
- Nakamura, T. Nutritional policies and dietary guidelines in Japan. Asia Pac. J. Clin. Nutr. 2011, 20, 452–454. [Google Scholar]
- Murphy, S.P.; Barr, S.I. Food guides reflect similarities and differences in dietary guidance in three countries (Japan, Canada, and the United States). Nutr. Rev. 2007, 65, 141–148. [Google Scholar] [CrossRef]
- Waijers, P.M.; Feskens, E.J.; Ocke, M.C. A critical review of predefined diet quality scores. Br. J. Nutr. 2007, 97, 219–231. [Google Scholar] [CrossRef]
- Kennedy, E. Dietary diversity, diet quality, and body weight regulation. Nutr. Rev. 2004, 62 Pt. 2, S78–S81. [Google Scholar] [CrossRef]
- Ma, E.; Ohira, T.; Yasumura, S.; Nakano, H.; Eguchi, E.; Miyazaki, M.; Hosoya, M.; Sakai, A.; Takahashi, A.; Ohira, H.; et al. Dietary Patterns and Progression of Impaired Kidney Function in Japanese Adults: A Longitudinal Analysis for the Fukushima Health Management Survey, 2011–2015. Nutrients 2021, 13, 168. [Google Scholar] [CrossRef]
- Ma, E.; Ohira, T.; Sakai, A.; Yasumura, S.; Takahashi, A.; Kazama, J.; Shimabukuro, M.; Nakano, H.; Okazaki, K.; Maeda, M.; et al. Associations between Dietary Patterns and Cardiometabolic Risks in Japan: A Cross-Sectional Study from the Fukushima Health Management Survey, 2011–2015. Nutrients 2020, 12, 129. [Google Scholar] [CrossRef]
- Kurotani, K.; Akter, S.; Kashino, I.; Goto, A.; Mizoue, T.; Noda, M.; Sasazuki, S.; Sawada, N.; Tsugane, S.; Japan Public Health Center based Prospective Study, G. Quality of diet and mortality among Japanese men and women: Japan Public Health Center based prospective study. BMJ 2016, 352, i1209. [Google Scholar] [CrossRef]
- Tomata, Y.; Zhang, S.; Kaiho, Y.; Tanji, F.; Sugawara, Y.; Tsuji, I. Nutritional characteristics of the Japanese diet: A cross-sectional study of the correlation between Japanese Diet Index and nutrient intake among community-based elderly Japanese. Nutrition 2019, 57, 115–121. [Google Scholar] [CrossRef]
- Yasumura, S.; Hosoya, M.; Yamashita, S.; Kamiya, K.; Abe, M.; Akashi, M.; Kodama, K.; Ozasa, K.; Fukushima Health Management Survey Group. Study protocol for the Fukushima Health Management Survey. J. Epidemiol. 2012, 22, 375–383. [Google Scholar] [CrossRef]
- Yasumura, S.; Ohira, T.; Ishikawa, T.; Shimura, H.; Sakai, A.; Maeda, M.; Miura, I.; Fujimori, K.; Ohto, H.; Kamiya, K. Achievements and Current Status of the Fukushima Health Management Survey. J. Epidemiol. 2022; in press. [Google Scholar]
- Sauvaget, C.; Allen, N.; Hayashi, M.; Spencer, E.; Nagano, J. Validation of a food frequency questionnaire in the Hiroshima/Nagasaki Life Span Study. J. Epidemiol. 2002, 12, 394–401. [Google Scholar] [CrossRef]
- Zhang, W.; Ohira, T.; Abe, M.; Kamiya, K.; Yamashita, S.; Yasumura, S.; Ohtsuru, A.; Masaharu, M.; Harigane, M.; Horikoshi, N.; et al. Evacuation after the Great East Japan Earthquake was associated with poor dietary intake: The Fukushima Health Management Survey. J. Epidemiol. 2017, 27, 14–23. [Google Scholar] [CrossRef]
- Luger, E.; Aspalter, R.; Luger, M.; Longin, R.; Rieder, A.; Dorner, T.E. Changes of dietary patterns during participation in a web-based weight-reduction programme. Public Health Nutr. 2016, 19, 1211–1221. [Google Scholar] [CrossRef][Green Version]
- Lin, J.; Fung, T.T.; Hu, F.B.; Curhan, G.C. Association of dietary patterns with albuminuria and kidney function decline in older white women: A subgroup analysis from the Nurses' Health Study. Am. J. Kidney Dis. 2011, 57, 245–254. [Google Scholar] [CrossRef]
- Tomata, Y.; Watanabe, T.; Sugawara, Y.; Chou, W.T.; Kakizaki, M.; Tsuji, I. Dietary patterns and incident functional disability in elderly Japanese: The Ohsaki Cohort 2006 study. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 8. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Tereza da Silva, J.; Bersch-Ferreira, A.C.; Torreglosa, C.R.; Weber, B.; Levy, R.B. Development of a dietary index based on the Brazilian Cardioprotective Nutritional Program (BALANCE). Nutr. J. 2018, 17, 49. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, E. Putting the pyramid into action: The Healthy Eating Index and Food Quality Score. Asia Pac. J. Clin. Nutr. 2008, 17 (Suppl. S1), 70–74. [Google Scholar] [PubMed]
- Drewnowski, A. The Nutrient Rich Foods Index helps to identify healthy, affordable foods. Am. J. Clin. Nutr. 2010, 91, 1095S–1101S. [Google Scholar] [CrossRef]
- Kotemori, A.; Sawada, N.; Iwasaki, M.; Yamaji, T.; Shivappa, N.; Hebert, J.R.; Ishihara, J.; Inoue, M.; Tsugane, S. Dietary Inflammatory Index Is Associated with Inflammation in Japanese Men. Front. Nutr. 2021, 8, 604296. [Google Scholar] [CrossRef]
- Abe, S.; Zhang, S.; Tomata, Y.; Tsuduki, T.; Sugawara, Y.; Tsuji, I. Japanese diet and survival time: The Ohsaki Cohort 1994 study. Clin. Nutr. 2019, 39, 298–303. [Google Scholar] [CrossRef]
- Matsuyama, S.; Sawada, N.; Tomata, Y.; Zhang, S.; Goto, A.; Yamaji, T.; Iwasaki, M.; Inoue, M.; Tsuji, I.; Tsugane, S.; et al. Association between adherence to the Japanese diet and all-cause and cause-specific mortality: The Japan Public Health Center-based Prospective Study. Eur. J. Nutr. 2021, 60, 1327–1336. [Google Scholar] [CrossRef]
- Suzuki, K.; Shivappa, N.; Kawado, M.; Yamada, H.; Hashimoto, S.; Wakai, K.; Iso, H.; Okada, E.; Fujii, R.; Hebert, J.R.; et al. Association between dietary inflammatory index and serum C-reactive protein concentrations in the Japan Collaborative Cohort Study. Nagoya J. Med. Sci. 2020, 82, 237–249. [Google Scholar]
- Nishimura, T.; Murakami, K.; Livingstone, M.B.; Sasaki, S.; Uenishi, K.; Japan Dietetic Students’ Study for Nutrition and Biomarkers Group. Adherence to the food-based Japanese dietary guidelines in relation to metabolic risk factors in young Japanese women. Br. J. Nutr. 2015, 114, 645–653. [Google Scholar] [CrossRef]
- Sakai, H.; Murakami, K.; Kobayashi, S.; Suga, H.; Sasaki, S.; Three-generation Study of Women on Diets and Health Study Group. Food-based diet quality score in relation to depressive symptoms in young and middle-aged Japanese women. Br. J. Nutr. 2017, 117, 1674–1681. [Google Scholar] [CrossRef]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef]
- Suzuki, N.; Goto, Y.; Ota, H.; Kito, K.; Mano, F.; Joo, E.; Ikeda, K.; Inagaki, N.; Nakayama, T. Characteristics of the Japanese Diet Described in Epidemiologic Publications: A Qualitative Systematic Review. J. Nutr. Sci. Vitaminol. 2018, 64, 129–137. [Google Scholar] [CrossRef]
- Crozier, S.R.; Robinson, S.M.; Godfrey, K.M.; Cooper, C.; Inskip, H.M. Women's dietary patterns change little from before to during pregnancy. J. Nutr. 2009, 139, 1956–1963. [Google Scholar] [CrossRef]
- Htun, N.C.; Suga, H.; Imai, S.; Shimizu, W.; Ishikawa-Takata, K.; Takimoto, H. Dietary pattern and its association with blood pressure and blood lipid profiles among Japanese adults in the 2012 Japan National Health and Nutrition Survey. Asia Pac. J. Clin. Nutr. 2018, 27, 1048–1061. [Google Scholar]
- Nanri, H.; Hara, M.; Nishida, Y.; Shimanoe, C.; Nakamura, K.; Higaki, Y.; Imaizumi, T.; Taguchi, N.; Sakamoto, T.; Horita, M.; et al. Dietary patterns and serum gamma-glutamyl transferase in Japanese men and women. J. Epidemiol. 2015, 25, 378–386. [Google Scholar] [CrossRef]
- Okubo, H.; Murakami, K.; Sasaki, S.; Kim, M.K.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Relative validity of dietary patterns derived from a self-administered diet history questionnaire using factor analysis among Japanese adults. Public Health Nutr. 2010, 13, 1080–1089. [Google Scholar] [CrossRef]
- Nishi, N.; Yoshimura, E.; Ishikawa-Takata, K.; Tsuboyama-Kasaoka, N.; Kubota, T.; Miyachi, M.; Tokudome, S.; Yokoyama, Y.; Sakata, K.; Kobayashi, S.; et al. Relationship of living conditions with dietary patterns among survivors of the great East Japan earthquake. J. Epidemiol. 2013, 23, 376–381. [Google Scholar] [CrossRef]
- Ito, T.; Kawakami, R.; Tanisawa, K.; Miyawaki, R.; Ishii, K.; Torii, S.; Suzuki, K.; Sakamoto, S.; Muraoka, I.; Oka, K.; et al. Dietary patterns and abdominal obesity in middle-aged and elderly Japanese adults: Waseda Alumni's Sports, Exercise, Daily Activity, Sedentariness and Health Study (WASEDA'S Health Study). Nutrition 2019, 58, 149–155. [Google Scholar] [CrossRef]
- Sadakane, A.; Tsutsumi, A.; Gotoh, T.; Ishikawa, S.; Ojima, T.; Kario, K.; Nakamura, Y.; Kayaba, K. Dietary patterns and levels of blood pressure and serum lipids in a Japanese population. J. Epidemiol. 2008, 18, 58–67. [Google Scholar] [CrossRef]
- Olinto, M.T.; Willett, W.C.; Gigante, D.P.; Victora, C.G. Sociodemographic and lifestyle characteristics in relation to dietary patterns among young Brazilian adults. Public Health Nutr. 2011, 14, 150–159. [Google Scholar] [CrossRef]
- Yanagihara, H.; Hatakeyama, Y.; Iwasaki, T. Coordination by registered dieticians for nutritional and dietary support in disaster in Japan. West. Pac. Surveill. Response J. 2012, 3, 46–51. [Google Scholar] [CrossRef]
- Zhang, W.; Ohira, T.; Yasumura, S.; Maeda, M.; Otsuru, A.; Harigane, M.; Horikoshi, N.; Suzuki, Y.; Yabe, H.; Nagai, M.; et al. Effects of socioeconomic factors on cardiovascular-related symptoms among residents in Fukushima after the Great East Japan Earthquake: A cross-sectional study using data from the Fukushima Health Management Survey. BMJ Open 2017, 7, e014077. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ohira, T.; Nakano, H.; Nagai, M.; Yumiya, Y.; Zhang, W.; Uemura, M.; Sakai, A.; Hashimoto, S.; Fukushima Health Management Survey Group. Changes in Cardiovascular Risk Factors After the Great East Japan Earthquake. Asia Pac. J. Public Health 2017, 29 (Suppl. S2), 47S–55S. [Google Scholar] [CrossRef] [PubMed]
- Tsuboyama-Kasaoka, N.; Hoshi, Y.; Onodera, K.; Mizuno, S.; Sako, K. What factors were important for dietary improvement in emergency shelters after the Great East Japan Earthquake? Asia Pac. J. Clin. Nutr. 2014, 23, 159–166. [Google Scholar]
- Descatha, A.; Roquelaure, Y.; Evanoff, B.; Niedhammer, I.; Chastang, J.F.; Mariot, C.; Ha, C.; Imbernon, E.; Goldberg, M.; Leclerc, A. Selected questions on biomechanical exposures for surveillance of upper-limb work-related musculoskeletal disorders. Int. Arch. Occup. Environ. Health 2007, 81, 1–8. [Google Scholar] [CrossRef]
- Patterson, E.; Warnberg, J.; Poortvliet, E.; Kearney, J.M.; Sjostrom, M. Dietary energy density as a marker of dietary quality in Swedish children and adolescents: The European Youth Heart Study. Eur. J. Clin. Nutr. 2010, 64, 356–363. [Google Scholar] [CrossRef]
| Three Patterns | |||
|---|---|---|---|
| Foods and Food Groups | Typical Japanese | Juice/Dairy | Meat |
| White vegetable | 0.74 | 0.10 | 0.19 |
| Miso soup | 0.72 | −0.09 | −0.08 |
| Green vegetable | 0.70 | 0.18 | 0.18 |
| Tofu | 0.70 | 0.16 | 0.03 |
| Red/yellow vegetable | 0.68 | 0.25 | 0.25 |
| Rice | 0.60 | −0.22 | 0.03 |
| Fish | 0.60 | 0.05 | 0.16 |
| Fruit | 0.55 | 0.41 | −0.07 |
| Fermented bean | 0.50 | 0.17 | −0.14 |
| Vegetable juice | −0.02 | 0.75 | 0.08 |
| Fruit juice | −0.04 | 0.72 | 0.15 |
| Soymilk | 0.08 | 0.62 | 0.01 |
| Yogurt | 0.27 | 0.57 | −0.02 |
| Boiled bean | 0.48 | 0.45 | 0.01 |
| Milk | 0.22 | 0.42 | 0.04 |
| Bread | −0.15 | 0.32 | 0.32 |
| Beef/pork | 0.15 | −0.04 | 0.79 |
| Chicken | 0.14 | 0.09 | 0.74 |
| Ham/sausage | 0.04 | 0.07 | 0.73 |
| Variance explained (%) | 4.20 | 2.67 | 2.03 |
| Food Groups | Score Assigned | Score Assigned | ||
|---|---|---|---|---|
| White vegetable | <median | 0 | ≥median | 1 |
| Green vegetable | <median | 0 | ≥median | 1 |
| Tofu | <median | 0 | ≥median | 1 |
| Miso soup | <median | 0 | ≥median | 1 |
| Red/yellow vegetable | <median | 0 | ≥median | 1 |
| Fish | <median | 0 | ≥median | 1 |
| Fermented bean | <median | 0 | ≥median | 1 |
| Fruit | <median | 0.5 | ≥median | 1 |
| Boiled bean | <median | 0.5 | ≥median | 1 |
| Rice | <median | 0 | ≥median | 1 |
| Vegetable juice | <median | 1 | ≥median | 0 |
| Fruit juice | <median | 1 | ≥median | 0 |
| Yogurt | <median | 1 | ≥median | 0 |
| Soybean milk | <median | 1 | ≥median | 0 |
| Bread | <median | 1 | ≥median | 0 |
| Milk | <median | 1 | ≥median | 0 |
| Beef/pork | <median | 1 | ≥median | 0 |
| Ham | <median | 1 | ≥median | 0 |
| Chicken | <median | 1 | ≥median | 0 |
| All Participants (n = 57,824) | Men (n = 26,028) | Women (n = 31,796) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| % | Mean * | SE | % | Mean * | SE | % | Mean * | SE | |
| Sex | |||||||||
| Men | 9.56 | 0.03 | – | – | |||||
| Women | 9.74 | 0.03 | – | – | |||||
| p-value ** | <0.0001 | ||||||||
| Age (years) | |||||||||
| 16–29 | 12.2 | 8.09 | 0.04 | 11.5 | 8.03 | 0.06 | 12.8 | 8.13 | 0.05 |
| 30–39 | 14.6 | 8.74 | 0.04 | 13.5 | 8.63 | 0.05 | 15.6 | 8.80 | 0.05 |
| 40–49 | 13.5 | 9.15 | 0.04 | 12.7 | 9.03 | 0.05 | 14.2 | 9.20 | 0.05 |
| 50–59 | 18.6 | 10.04 | 0.03 | 18.7 | 9.82 | 0.05 | 18.5 | 10.15 | 0.05 |
| 60–69 | 22.2 | 10.77 | 0.03 | 24.4 | 10.59 | 0.04 | 20.4 | 10.84 | 0.05 |
| 70–84 | 18.9 | 11.14 | 0.03 | 19.3 | 11.04 | 0.05 | 18.6 | 11.14 | 0.05 |
| p-value ** | <0.0001 | <0.0001 | <0.0001 | ||||||
| Educational level | |||||||||
| Elementary/junior high school | 21.4 | 9.70 | 0.03 | 23.2 | 9.68 | 0.04 | 19.9 | 9.64 | 0.05 |
| High school | 51.7 | 9.61 | 0.03 | 52.5 | 9.50 | 0.04 | 51.0 | 9.63 | 0.04 |
| Vocational college | 17.7 | 9.62 | 0.03 | 11.1 | 9.49 | 0.05 | 23.2 | 9.74 | 0.05 |
| Undergraduate/graduate | 9.2 | 9.68 | 0.04 | 13.3 | 9.41 | 0.05 | 5.9 | 9.82 | 0.07 |
| p-value ** | 0.002 | <0.0001 | 0.001 | ||||||
| Health condition | |||||||||
| Good | 18.6 | 9.83 | 0.03 | 22.0 | 9.72 | 0.05 | 15.9 | 9.88 | 0.05 |
| Normal | 63.1 | 9.65 | 0.03 | 60.6 | 9.53 | 0.04 | 65.2 | 9.69 | 0.04 |
| Poor | 18.3 | 9.48 | 0.03 | 17.4 | 9.32 | 0.04 | 19.0 | 9.56 | 0.05 |
| p-value ** | <0.0001 | <0.0001 | <0.0001 | ||||||
| Smoking | |||||||||
| No | 55.8 | 9.71 | 0.03 | 27.4 | 9.51 | 0.04 | 79.1 | 9.83 | 0.04 |
| Former | 21.8 | 9.69 | 0.03 | 37.1 | 9.60 | 0.04 | 9.3 | 9.67 | 0.05 |
| Current | 22.4 | 9.57 | 0.03 | 35.5 | 9.46 | 0.04 | 11.6 | 9.63 | 0.05 |
| p-value ** | <0.0001 | 0.001 | <0.0001 | ||||||
| Alcohol drinking | |||||||||
| No | 50.9 | 9.61 | 0.02 | 29.6 | 9.39 | 0.04 | 68.3 | 9.73 | 0.03 |
| Former | 3.3 | 9.57 | 0.06 | 5.0 | 9.45 | 0.07 | 2.0 | 9.62 | 0.10 |
| Current | 45.8 | 9.78 | 0.02 | 65.5 | 9.72 | 0.03 | 29.7 | 9.77 | 0.03 |
| p-value ** | <0.0001 | <0.0001 | 0.169 | ||||||
| Physical activity | |||||||||
| Everyday | 13.6 | 9.89 | 0.04 | 16.4 | 9.78 | 0.05 | 11.4 | 9.92 | 0.05 |
| 2–4 times/day | 19.1 | 9.69 | 0.03 | 19.1 | 9.55 | 0.05 | 19.0 | 9.74 | 0.05 |
| 1 time/day | 13.8 | 9.53 | 0.03 | 14.7 | 9.37 | 0.05 | 13.0 | 9.63 | 0.05 |
| No | 53.5 | 9.51 | 0.03 | 49.8 | 9.39 | 0.04 | 56.6 | 9.55 | 0.04 |
| p-value ** | <0.0001 | <0.0001 | <0.0001 | ||||||
| Depression | |||||||||
| Weak (K6 < 13) | 85.8 | 9.68 | 0.02 | 88.2 | 9.53 | 0.03 | 83.8 | 9.74 | 0.04 |
| Strong (K6 ≥ 13) | 14.2 | 9.63 | 0.03 | 11.8 | 9.51 | 0.05 | 16.2 | 9.68 | 0.05 |
| p-value ** | 0.086 | 0.609 | 0.07 | ||||||
| Change of residence | |||||||||
| Own/relatives’ house | 54.1 | 9.76 | 0.03 | 53.2 | 9.66 | 0.04 | 54.9 | 9.78 | 0.04 |
| Shelter/temporary/rent | 45.9 | 9.55 | 0.03 | 46.8 | 9.39 | 0.04 | 45.1 | 9.64 | 0.04 |
| p-value ** | <0.0001 | <0.0001 | <0.0001 | ||||||
| Health Diet Index Score (Quartiles) | p Trend | ||||
|---|---|---|---|---|---|
| Q1 (Low) | Q2 | Q3 | Q4 (High) | ||
| Index score | <8 | 8–<10 | 10–<12 | ≥12 | |
| Number of participants | 6567 | 8403 | 10,482 | 9380 | |
| Overweight (BMI ≥ 25 (kg/m2) | 2023 | 2636 | 3411 | 3066 | |
| Model 1 | 1.00 (Reference) | 0.92 (0.86, 0.99) | 0.89 (0.83, 0.96) | 0.81 (0.75, 0.87) | <0.001 |
| Model 2 | 1.00 (Reference) | 0.95 (0.88, 1.02) | 0.93 (0.86, 1.00) | 0.87 (0.80, 0.94) | <0.001 |
| Large waist circumference (men ≥ 85 cm/women ≥ 90 cm) | 1587 | 1028 | 2704 | 3291 | |
| Model 1 | 1.00 (Reference) | 1.04 (0.96, 1.02) | 0.98 (0.91, 1.06) | 0.99 (0.92, 1.07) | 0.411 |
| Model 2 | 1.00 (Reference) | 0.99 (0.91, 1.09) | 0.91 (0.83, 0.99) | 0.89 (0.81, 0.97) | 0.001 |
| Hypertension * | 1674 | 2887 | 4600 | 4984 | |
| Model 1 | 1.00 (Reference) | 0.94 (0.80, 1.11) | 0.91 (0.80, 1.04) | 1.01 (0.89, 1.15) | 0.98 |
| Model 2 | 1.00 (Reference) | 0.92 (0.78, 1.08) | 0.89 (0.78, 1.02) | 0.99 (0.87, 1.13) | 0.936 |
| Diabetes mellitus ** | 406 | 699 | 1013 | 1138 | |
| Model 1 | 1.00 (Reference) | 0.73 (0.57, 0.95) | 0.73 (0.57, 0.93) | 0.79 (0.62, 1.00) | 0.221 |
| Model 2 | 1.00 (Reference) | 0.77 (0.59, 1.00) | 0.77 (0.60, 0.99) | 0.85 (0.67, 1.10) | 0.571 |
| Dyslipidemia # | 2856 | 3979 | 5546 | 5252 | |
| Model 1 | 1.00 (Reference) | 0.84 (0.77, 0.92) | 0.81 (0.74, 0.88) | 0.70 (0.64, 0.77) | <0.0001 |
| Model 2 | 1.00 (Reference) | 0.85 (0.77, 0.92) | 0.82 (0.75, 0.89) | 0.73 (0.66, 0.80) | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, E.; Ohira, T.; Yasumura, S.; Hosoya, M.; Miyazaki, M.; Okazaki, K.; Nagao, M.; Hayashi, F.; Nakano, H.; Eguchi, E.; et al. Development of a Japanese Healthy Diet Index: The Fukushima Health Management Survey 2011. Int. J. Environ. Res. Public Health 2022, 19, 14858. https://doi.org/10.3390/ijerph192214858
Ma E, Ohira T, Yasumura S, Hosoya M, Miyazaki M, Okazaki K, Nagao M, Hayashi F, Nakano H, Eguchi E, et al. Development of a Japanese Healthy Diet Index: The Fukushima Health Management Survey 2011. International Journal of Environmental Research and Public Health. 2022; 19(22):14858. https://doi.org/10.3390/ijerph192214858
Chicago/Turabian StyleMa, Enbo, Tetsuya Ohira, Seiji Yasumura, Mitsuaki Hosoya, Makoto Miyazaki, Kanako Okazaki, Masanori Nagao, Fumikazu Hayashi, Hironori Nakano, Eri Eguchi, and et al. 2022. "Development of a Japanese Healthy Diet Index: The Fukushima Health Management Survey 2011" International Journal of Environmental Research and Public Health 19, no. 22: 14858. https://doi.org/10.3390/ijerph192214858
APA StyleMa, E., Ohira, T., Yasumura, S., Hosoya, M., Miyazaki, M., Okazaki, K., Nagao, M., Hayashi, F., Nakano, H., Eguchi, E., Funakubo, N., Shimabukuro, M., Yabe, H., Maeda, M., Ohto, H., & Kamiya, K. (2022). Development of a Japanese Healthy Diet Index: The Fukushima Health Management Survey 2011. International Journal of Environmental Research and Public Health, 19(22), 14858. https://doi.org/10.3390/ijerph192214858







