Positive Affect Moderates the Influence of Perceived Stress on the Mental Health of Healthcare Workers during the COVID-19 Pandemic
Abstract
1. Introduction
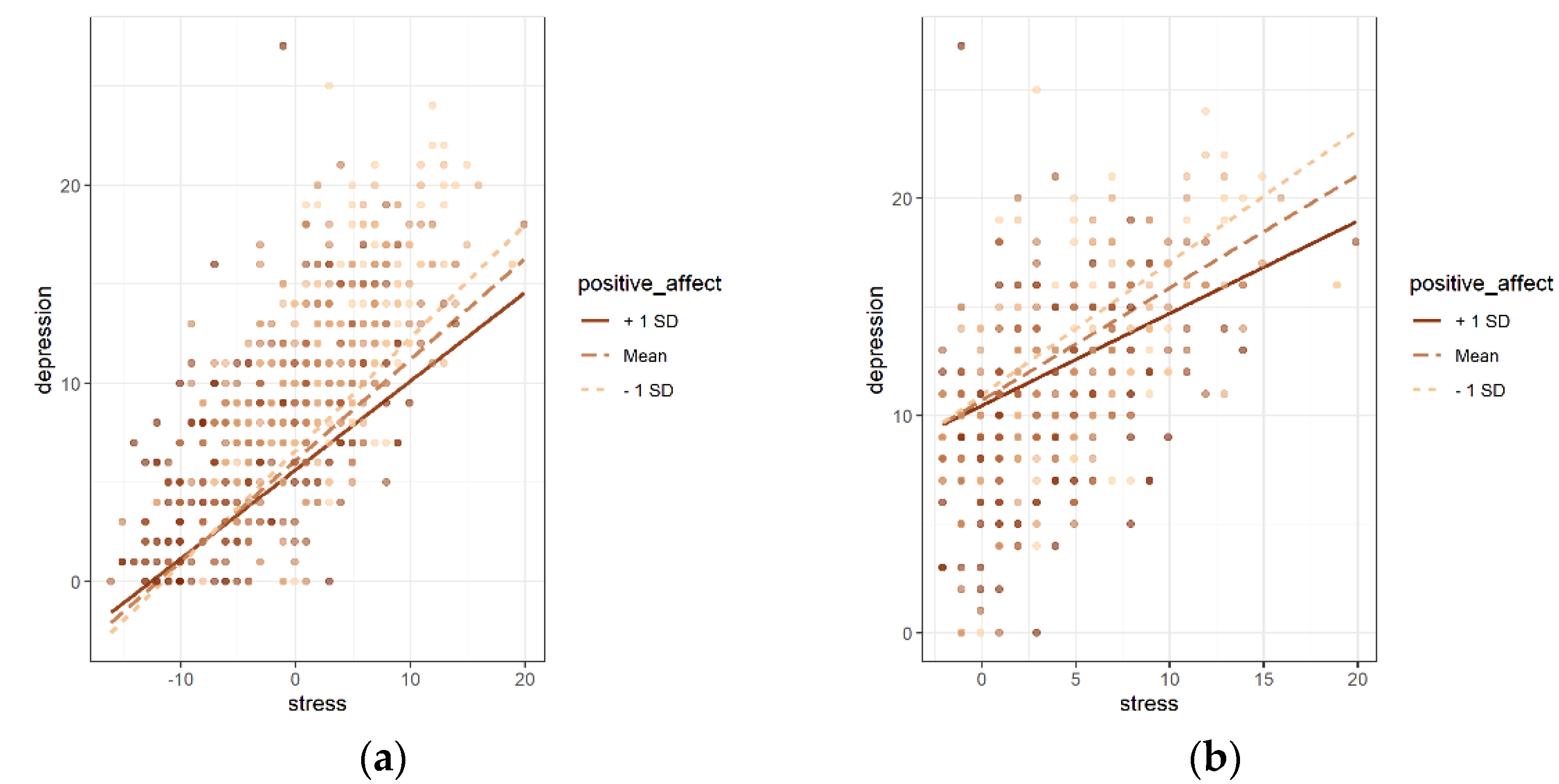
- At the total group level, positive affect could alleviate the impacts of perceived stress on psychological problems, including depression and anxiety.
- At the subgroup level, the moderating role of positive affect was different according to the level of perceived stress. Particularly, compared with the subgroup with a low level of stress, the moderating effect of positive affect on the relationship between stress and psychological problems was more significant in the high-stress subgroup.
2. Methods
2.1. Study Procedure
2.2. Participants
2.3. Measurements
2.3.1. Sociodemographic Information
2.3.2. The Positive and Negative Affect Schedule
2.3.3. Perceived Stress Scale
2.3.4. Generalized Anxiety Disorder 7-Item Scale
2.3.5. Patient Health Questionnaire-9
2.4. Statistical Analysis
3. Results
3.1. Descriptive Analyses
3.2. Average Scores and Correlations among Mental Health Measurements
3.3. Multiple Regression Analyses in the Total Group
3.4. Multiple Regression Analyses in the Subgroups
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 13 July 2022).
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Talaee, N.; Varahram, M.; Jamaati, H.; Salimi, A.; Attarchi, M.; Kazempour Dizaji, M.; Sadr, M.; Hassani, S.; Farzanegan, B.; Monjazebi, F.; et al. Stress and burnout in health care workers during COVID-19 pandemic: Validation of a questionnaire. Z. Fur Gesundh. J. Public Health 2022, 30, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Walton, M.; Murray, E.; Christian, M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 241–247. [Google Scholar] [CrossRef]
- Kang, L.; Li, Y.; Hu, S.; Chen, M.; Yang, C.; Yang, B.X.; Wang, Y.; Hu, J.; Lai, J.; Ma, X.; et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020, 7, e14. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Liu, S.; Yang, L.; Zhang, C.; Xiang, Y.T.; Liu, Z.; Hu, S.; Zhang, B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e17–e18. [Google Scholar] [CrossRef]
- Lancee, W.J.; Maunder, R.G.; Goldbloom, D.S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 2008, 59, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Y.T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef]
- Stress, A.I.o. What is Stress? Available online: http://www.stress.org/what-is-stress/ (accessed on 14 July 2022).
- Liu, Z.; Liu, R.; Zhang, Y.; Zhang, R.; Liang, L.; Wang, Y.; Wei, Y.; Zhu, R.; Wang, F. Association between perceived stress and depression among medical students during the outbreak of COVID-19: The mediating role of insomnia. J. Affect. Disord. 2021, 292, 89–94. [Google Scholar] [CrossRef]
- Heinen, I.; Bullinger, M.; Kocalevent, R.D. Perceived stress in first year medical students—Associations with personal resources and emotional distress. BMC Med. Educ. 2017, 17, 4. [Google Scholar] [CrossRef]
- Stansfeld, S.; Candy, B. Psychosocial work environment and mental health—A meta-analytic review. Scand. J. Work Environ. Health 2006, 32, 443–462. [Google Scholar] [CrossRef] [PubMed]
- Hammen, C.; Kim, E.Y.; Eberhart, N.K.; Brennan, P.A. Chronic and acute stress and the prediction of major depression in women. Depress. Anxiety 2009, 26, 718–723. [Google Scholar] [CrossRef]
- Nima, A.A.; Rosenberg, P.; Archer, T.; Garcia, D. Anxiety, affect, self-esteem, and stress: Mediation and moderation effects on depression. PLoS ONE 2013, 8, e73265. [Google Scholar] [CrossRef]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef] [PubMed]
- Said, R.M.; El-Shafei, D.A. Occupational stress, job satisfaction, and intent to leave: Nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Environ. Sci. Pollut. Res. Int. 2021, 28, 8791–8801. [Google Scholar] [CrossRef] [PubMed]
- Kebede, M.A.; Demissie, D.B.; Guddu, D.K.; Haile, M.T.; Bitew, Z.W.; Muleta, M.B. Emotional responses and perceived stressors of frontline medical staffs in case of COVID-19 treatment centers and obstetrics emergency in Ethiopia. BMC Psychiatry 2021, 21, 308. [Google Scholar] [CrossRef]
- Schneiderman, N.; Ironson, G.; Siegel, S.D. Stress and health: Psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol. 2005, 1, 607–628. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.; Psychiatry, E. Mood and Anxiety Symptom Questionnaire; University of Wisconsin-Madison: Madison, WI, USA, 1991. [Google Scholar]
- Mascaro, N.; Rosen, D. The role of existential meaning as a buffer against stress. J. Humanist. Psychol. 2006, 46, 168–190. [Google Scholar] [CrossRef]
- Aspinwall, L.G. Dealing with Adversity: Self-Regulation, Coping, Adaptation, and Health; American Psychological Association: Washington, DC, USA, 2004. [Google Scholar]
- Aspinwall, L.G. Rethinking the role of positive affect in self-regulation. Motiv. Emot. 1998, 22, 1–32. [Google Scholar] [CrossRef]
- Fredrickson, B.L. The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. Am. Psychol. 2001, 56, 218–226. [Google Scholar] [CrossRef]
- Nelson, N.A.; Bergeman, C.S. Daily Stress Processes in a Pandemic: The Effects of Worry, Age, and Affect. Gerontologist 2021, 61, 196–204. [Google Scholar] [CrossRef] [PubMed]
- García-Batista, Z.E.; Guerra-Peña, K.; Nouri Kandany, V.; Marte, M.I.; Garrido, L.E.; Cantisano-Guzmán, L.M.; Moretti, L.; Medrano, L.A. COVID-19 pandemic and health worker stress: The mediating effect of emotional regulation. PLoS ONE 2021, 16, e0259013. [Google Scholar] [CrossRef] [PubMed]
- Leger, K.A.; Charles, S.T.; Almeida, D.M. Positive Emotions Experienced on Days of Stress are Associated with Less Same Day and Next Day Negative Emotion. Affect. Sci. 2020, 1, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Theorell, T.; Hammarström, A.; Aronsson, G.; Träskman Bendz, L.; Grape, T.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Hall, C. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 2015, 15, 738. [Google Scholar] [CrossRef]
- Stowell, D.; Lewis, R.K.; Brooks, K. Perceived stress, substance use, and mental health issues among college students in the Midwest. J. Prev. Interv. Community 2021, 49, 221–234. [Google Scholar] [CrossRef]
- Sewart, A.R.; Zbozinek, T.D.; Hammen, C.; Zinbarg, R.E.; Mineka, S.; Craske, M.G. Positive Affect as a Buffer between Chronic Stress and Symptom Severity of Emotional Disorders. Clin. Psychol. Sci. A J. Assoc. Psychol. Sci. 2019, 7, 914–927. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Personal. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Cheung, D.K.; Tam, D.K.Y.; Tsang, M.H.; Zhang, D.L.W.; Lit, D.S.W. Depression, anxiety and stress in different subgroups of first-year university students from 4-year cohort data. J. Affect. Disord. 2020, 274, 305–314. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Wang, W.; Bian, Q.; Zhao, Y.; Li, X.; Wang, W.; Du, J.; Zhang, G.; Zhou, Q.; Zhao, M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2014, 36, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Xu, Y.; Yu, Y.; Peng, L.; Wu, T.; Wang, T.; Liu, B.; Xie, J.; Xu, S.; Li, M. Moderating Effect of Mindfulness on the Relationships Between Perceived Stress and Mental Health Outcomes Among Chinese Intensive Care Nurses. Front. Psychiatry 2019, 10, 260. [Google Scholar] [CrossRef] [PubMed]
- Jaccard, J.; Turrisi, R. Interaction Effects in Multiple Regression; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2003. [Google Scholar] [CrossRef]
- Zhang, Y.; Axinn, W.G. Marital Experiences and Depression in an Arranged Marriage Setting. AJS Am. J. Sociol. 2021, 126, 1439–1486. [Google Scholar] [CrossRef] [PubMed]
- Simon, R.W.; Barrett, A.E. Nonmarital romantic relationships and mental health in early adulthood: Does the association differ for women and men? J. Health Soc. Behav. 2010, 51, 168–182. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Birmingham, W.; Jones, B.Q. Is there something unique about marriage? The relative impact of marital status, relationship quality, and network social support on ambulatory blood pressure and mental health. Ann. Behav. Med. A Publ. Soc. Behav. Med. 2008, 35, 239–244. [Google Scholar] [CrossRef]
- Jang, S.N.; Kawachi, I.; Chang, J.; Boo, K.; Shin, H.G.; Lee, H.; Cho, S.I. Marital status, gender, and depression: Analysis of the baseline survey of the Korean Longitudinal Study of Ageing (KLoSA). Soc. Sci. Med. 2009, 69, 1608–1615. [Google Scholar] [CrossRef]
- Afifi, T.O.; Cox, B.J.; Enns, M.W. Mental health profiles among married, never-married, and separated/divorced mothers in a nationally representative sample. Soc. Psychiatry Psychiatr. Epidemiol. 2006, 41, 122–129. [Google Scholar] [CrossRef]
- Taylor, S.E.; Way, B.M.; Seeman, T.E. Early adversity and adult health outcomes. Dev. Psychopathol. 2011, 23, 939–954. [Google Scholar] [CrossRef]
- Schöllgen, I.; Huxhold, O.; Schmiedek, F. Emotions and physical health in the second half of life: Interindividual differences in age-related trajectories and dynamic associations according to socioeconomic status. Psychol. Aging 2012, 27, 338–352. [Google Scholar] [CrossRef]
- GebreEyesus, F.A.; Tarekegn, T.T.; Amlak, B.T.; Shiferaw, B.Z.; Emeria, M.S.; Geleta, O.T.; Terefe, T.F.; Mammo Tadereregew, M.; Jimma, M.S.; Degu, F.S.; et al. Levels and predictors of anxiety, depression, and stress during COVID-19 pandemic among frontline healthcare providers in Gurage zonal public hospitals, Southwest Ethiopia, 2020: A multicenter cross-sectional study. PLoS ONE 2021, 16, e0259906. [Google Scholar] [CrossRef]
- Selinger, C.P.; Lal, S.; Eaden, J.; Jones, D.B.; Katelaris, P.; Chapman, G.; McDonald, C.; Leong, R.W.; McLaughlin, J. Better disease specific patient knowledge is associated with greater anxiety in inflammatory bowel disease. J. Crohn’s Colitis 2013, 7, e214–e218. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Liao, J.; Liao, X.; Wu, X.; Wan, M.; Wang, C.; Ma, Q. Disease knowledge level is a noteworthy risk factor of anxiety and depression in patients with chronic obstructive pulmonary disease: A cross-sectional study. BMC Pulm. Med. 2014, 14, 92. [Google Scholar] [CrossRef] [PubMed]
- Ong, A.D.; Bergeman, C.S. The complexity of emotions in later life. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2004, 59, P117–P122. [Google Scholar] [CrossRef] [PubMed]
- Ong, A.D.; Bergeman, C.S.; Bisconti, T.L.; Wallace, K.A. Psychological resilience, positive emotions, and successful adaptation to stress in later life. J. Personal. Soc. Psychol. 2006, 91, 730–749. [Google Scholar] [CrossRef]
- Thong, I.S.K.; Tan, G.; Jensen, M.P. The buffering role of positive affect on the association between pain intensity and pain related outcomes. Scand. J. Pain 2017, 14, 91–97. [Google Scholar] [CrossRef]
- Seligman, M.E.; Steen, T.A.; Park, N.; Peterson, C. Positive psychology progress: Empirical validation of interventions. Am. Psychol. 2005, 60, 410–421. [Google Scholar] [CrossRef]
- Sin, N.L.; Lyubomirsky, S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. J. Clin. Psychol. 2009, 65, 467–487. [Google Scholar] [CrossRef]
- Clark, L.A.; Watson, D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. J. Abnorm. Psychol. 1991, 100, 316–336. [Google Scholar] [CrossRef]
- Watson, D. Differentiating the mood and anxiety disorders: A quadripartite model. Annu. Rev. Clin. Psychol. 2009, 5, 221–247. [Google Scholar] [CrossRef]
- Clark, L.A.; Watson, D.; Mineka, S. Temperament, personality, and the mood and anxiety disorders. J. Abnorm. Psychol. 1994, 103, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Yamagata, S.; Ritchie, S.J.; Barker, E.D.; Ando, J. Etiological pathways of depressive and anxiety symptoms linked to personality traits: A genetically-informative longitudinal study. J. Affect. Disord. 2021, 291, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Karaaslan, Ö.; Kantekin, Y.; Hacımusalar, Y.; Dağıstan, H. Anxiety sensitivities, anxiety and depression levels, and personality traits of patients with chronic subjective tinnitus: A case-control study. Int. J. Psychiatry Clin. Pract. 2020, 24, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wang, C.; Wang, W.; Tan, J. Trait anxiety, a personality risk factor associated with Alzheimer’s Disease. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 105, 110124. [Google Scholar] [CrossRef]
- Pompili, M.; Gibiino, S.; Innamorati, M.; Serafini, G.; Del Casale, A.; De Risio, L.; Palermo, M.; Montebovi, F.; Campi, S.; De Luca, V.; et al. Prolactin and thyroid hormone levels are associated with suicide attempts in psychiatric patients. Psychiatry Res. 2012, 200, 389–394. [Google Scholar] [CrossRef]
- Dincer, B.; Inangil, D. The effect of Emotional Freedom Techniques on nurses’ stress, anxiety, and burnout levels during the COVID-19 pandemic: A randomized controlled trial. Explore (NY) 2021, 17, 109–114. [Google Scholar] [CrossRef]
- Yıldırım, D.; Çiriş Yıldız, C. The Effect of Mindfulness-Based Breathing and Music Therapy Practice on Nurses’ Stress, Work-Related Strain, and Psychological Well-being During the COVID-19 Pandemic: A Randomized Controlled Trial. Holist. Nurs. Pract. 2022, 36, 156–165. [Google Scholar] [CrossRef]
- Chung, G.K.; Strong, C.; Chan, Y.H.; Chung, R.Y.; Chen, J.S.; Lin, Y.H.; Huang, R.Y.; Lin, C.Y.; Ko, N.Y. Psychological Distress and Protective Behaviors During the COVID-19 Pandemic Among Different Populations: Hong Kong General Population, Taiwan Healthcare Workers, and Taiwan Outpatients. Front. Med. 2022, 9, 800962. [Google Scholar] [CrossRef]
- Thakur, B.; Pathak, M. Burden of Predominant Psychological Reactions Among the Healthcare Workers and General Population During COVID-19 Pandemic Phase: A Systematic Review and Meta-Analysis. Indian J. Community Med. Off. Publ. Indian Assoc. Prev. Soc. Med. 2021, 46, 600–605. [Google Scholar] [CrossRef]
- Paolone, G.; Mazzitelli, C.; Formiga, S.; Kaitsas, F.; Breschi, L.; Mazzoni, A.; Tete, G.; Polizzi, E.; Gherlone, E.; Cantatore, G. One-year impact of COVID-19 pandemic on Italian dental professionals: A cross-sectional survey. Minerva Dent. Oral Sci. 2022, 71, 212–222. [Google Scholar] [CrossRef]
- Mavrogenis, A.F.; Scarlat, M.M. Stress, anxiety, and burnout of orthopaedic surgeons in COVID-19 pandemic. Int. Orthop. 2022, 46, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Grover, R.; Dua, P.; Juneja, S.; Chauhan, L.; Agarwal, P.; Khurana, A. “Depression, Anxiety and Stress” in a Cohort of Registered Practicing Ophthalmic Surgeons, Post Lockdown during COVID-19 Pandemic in India. Ophthalmic Epidemiol. 2021, 28, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Coifman, K.G.; Disabato, D.D.; Seah, T.H.S.; Ostrowski-Delahanty, S.; Palmieri, P.A.; Delahanty, D.L.; Gunstad, J. Boosting positive mood in medical and emergency personnel during the COVID-19 pandemic: Preliminary evidence of efficacy, feasibility and acceptability of a novel online ambulatory intervention. Occup. Environ. Med. 2021. ahead of print. [Google Scholar] [CrossRef]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H.; Wang, C.; Wang, Z.; You, Y.; et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control 2020, 48, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Liang, M.; Li, Y.; Guo, J.; Fei, D.; Wang, L.; He, L.; Sheng, C.; Cai, Y.; Li, X.; et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e15–e16. [Google Scholar] [CrossRef]
| Characteristics | Total | Positive Affect | Stress | Depression | Anxiety | ||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | N (%)/Mean ± SD | Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | Mean ± SD | p |
| Gender | 0.215 | 0.654 | 0.759 | 0.815 | |||||
| Male | 190 (28.6) | 27.6 (6.37) | 17.3 (6.76) | 9.36 (5.02) | 7.53 (4.45) | ||||
| Female | 474 (71.4) | 27.0 (6.07) | 17.0 (6.54) | 9.23 (5.02) | 7.43 (4.81) | ||||
| Education level | 0.513 | 0.183 | 0.065 | 0.036 * | |||||
| Junior high or below | 2 (0.3) | 30.0 (11.3) | 8.50 (7.78) | 1.00 (0.00) | 0.00 (0.00) | ||||
| High school and vocational school | 97 (14.6) | 26.6 (6.49) | 17.1 (6.70) | 9.24 (5.39) | 6.93 (4.62) | ||||
| College or above | 565 (85.1) | 27.2 (6.09) | 17.1 (6.57) | 9.30 (4.94) | 7.58 (4.70) | ||||
| Individual monthly income (yuan) | 0.009 **, a < c | 0.089 | 0.113 | 0.930 | |||||
| <5000 a | 146 (22.0) | 26.0 (6.04) | 17.8 (6.52) | 10.0 (5.29) | 7.58 (4.92) | ||||
| 5000–10,000 b | 315 (47.4) | 27.1 (5.85) | 17.3 (6.57) | 9.14 (4.89) | 7.40 (4.46) | ||||
| >10,000 c | 203 (30.6) | 28.0 (6.58) | 16.3 (6.66) | 8.92 (4.98) | 7.46 (4.93) | ||||
| Marital status | 0.007 **, a < b | 0.163 | 0.020 *, a > b | 0.796 | |||||
| Single a | 330 (49.8) | 26.4 (5.82) | 17.6 (6.48) | 9.82 (4.89) | 7.60 (4.37) | ||||
| Currently married b | 322 (48.6) | 27.9 (6.34) | 16.7 (6.64) | 8.79 (5.07) | 7.36 (4.98) | ||||
| Divorced or other c | 10 (1.5) | 28.6 (4.84) | 15.5 (7.52) | 7.80 (5.03) | 7.70 (5.77) | ||||
| Status of residence | 0.115 | 0.433 | 0.008 ** | 0.095 | |||||
| Living alone | 143 (21.5) | 26.4 (6.35) | 17.5 (6.28) | 10.3 (5.12) | 8.03 (4.60) | ||||
| Not living alone | 521 (78.5) | 27.4 (6.10) | 17.0 (6.69) | 8.99 (4.95) | 7.30 (4.72) | ||||
| Professional title | 0.730 | 0.305 | 0.757 | 0.408 | |||||
| Junior title | 327 (49.2) | 27.0 (5.99) | 16.7 (6.20) | 9.27 (4.88) | 7.21 (4.46) | ||||
| Intermediate title | 195 (29.4) | 27.4 (6.27) | 17.7 (7.14) | 9.09 (5.26) | 7.67 (5.12) | ||||
| Senior title | 142 (21.4) | 27.2 (6.40) | 17.1 (6.73) | 9.50 (5.01) | 7.75 (4.64) | ||||
| Variables | Variable Description Mean ± SD | Stress | Positive Affect | Anxiety | Depression |
|---|---|---|---|---|---|
| Stress | 17.08 ± 6.60 | 1.00 | |||
| Positive affect | 27.16 ± 6.16 | −0.47 *** | 1.00 | ||
| Anxiety | 7.46 ± 4.70 | 0.73 *** | −0.39 *** | 1.00 | |
| Depression | 9.26 ± 5.01 | 0.71 *** | −0.40 *** | 0.84 *** | 1.00 |
| Model1 | Model2 | Model3 | Model4 | |||||
|---|---|---|---|---|---|---|---|---|
| b | p | b | p | b | p | b | p | |
| Gender (Female) | −0.046 | 0.915 | 0.045 | 0.884 | −0.009 | 0.976 | −0.040 | 0.894 |
| Age | −0.014 | 0.794 | −0.006 | 0.885 | −0.015 | 0.695 | −0.027 | 0.483 |
| Education level (Junior high or below) | ||||||||
| High school and vocational school | 8.652 | 0.017 * | 3.434 | 0.179 | 3.400 | 0.181 | 3.746 | 0.138 |
| College or above | 9.092 | 0.011 * | 3.683 | 0.147 | 3.671 | 0.146 | 4.009 | 0.110 |
| Marital status (Single) | ||||||||
| Married | −0.456 | 0.400 | 0.046 | 0.904 | 0.141 | 0.712 | 0.177 | 0.642 |
| Divorced or other | −1.610 | 0.348 | −0.406 | 0.738 | −0.284 | 0.814 | −0.236 | 0.844 |
| Status of residence (Not living alone) | −1.006 | 0.055 | −0.921 | 0.013 * | −0.889 | 0.016 * | −0.942 | 0.010 * |
| Income (yuan, <5000) | ||||||||
| 5000–10,000 | −0.883 | 0.098 | −0.471 | 0.211 | −0.406 | 0.280 | −0.440 | 0.239 |
| >10,000 | −0.893 | 0.152 | 0.002 | 0.997 | 0.082 | 0.852 | 0.026 | 0.952 |
| Professional title (Junior title) | ||||||||
| Intermediate title | 0.557 | 0.274 | −0.429 | 0.237 | −0.392 | 0.277 | −0.464 | 0.196 |
| Senior title | 0.578 | 0.274 | 0.143 | 0.703 | 0.186 | 0.617 | 0.132 | 0.720 |
| Seniority | −0.013 | 0.771 | −0.016 | 0.610 | −0.013 | 0.667 | −0.002 | 0.955 |
| Stress (A) | 0.536 | <0.001 *** | 0.503 | <0.001 *** | 0.509 | <0.001 *** | ||
| Positive affect (B) | −0.075 | 0.004 ** | −0.078 | 0.002 ** | ||||
| A × B | −0.010 | 0.002 ** | ||||||
| Model F (p) | 1.862 (0.036) | 53.42 (<0.001) | 50.79 (<0.001) | 48.71 (<0.001) | ||||
| R2 (Δ R2) | 0.033 | 0.517 (0.484) | 0.524 (0.007) | 0.531 (0.007) | ||||
| Δ F (p) | 649.79 (<0.001) | 8.540 (0.004) | 9.867 (0.002) | |||||
| Model1 | Model2 | Model3 | Model4 | |||||
|---|---|---|---|---|---|---|---|---|
| b | p | b | p | b | p | b | p | |
| Gender (Female) | 0.026 | 0.948 | 0.115 | 0.678 | 0.075 | 0.784 | 0.066 | 0.810 |
| Age | −0.022 | 0.664 | −0.014 | 0.691 | −0.021 | 0.551 | −0.024 | 0.488 |
| Education level (Junior high or below) | ||||||||
| High school and vocational school | 7.204 | 0.034 * | 2.095 | 0.366 | 2.069 | 0.370 | 2.173 | 0.347 |
| College or above | 7.948 | 0.019 * | 2.651 | 0.249 | 2.642 | 0.249 | 2.743 | 0.232 |
| Marital status (Single) | ||||||||
| Married | 0.077 | 0.880 | 0.569 | 0.102 | 0.638 | 0.067 | 0.649 | 0.063 |
| Divorced or other | 0.186 | 0.909 | 1.365 | 0.215 | 1.454 | 0.186 | 1.468 | 0.181 |
| Status of residence (Not living alone) | −0.808 | 0.102 | −0.724 | 0.031 * | −0.701 | 0.037 * | −0.717 | 0.033 * |
| Income (yuan, <5000) | ||||||||
| 5000–10,000 | −0.333 | 0.508 | 0.070 | 0.839 | 0.118 | 0.730 | 0.108 | 0.753 |
| >10,000 | −0.328 | 0.576 | 0.548 | 0.172 | 0.607 | 0.130 | 0.590 | 0.141 |
| Professional title (Junior title) | ||||||||
| Intermediate title | 0.753 | 0.117 | −0.211 | 0.520 | −0.184 | 0.573 | −0.206 | 0.530 |
| Senior title | 0.806 | 0.106 | 0.379 | 0.263 | 0.411 | 0.224 | 0.395 | 0.243 |
| Seniority | −0.008 | 0.851 | −0.011 | 0.702 | −0.009 | 0.751 | −0.005 | 0.847 |
| Stress (A) | 0.525 | <0.001 *** | 0.501 | <0.001 *** | 0.503 | <0.001 *** | ||
| Positive affect (B) | −0.055 | 0.019 * | −0.056 | 0.017 * | ||||
| A × B | −0.003 | 0.307 | ||||||
| Model F (p) | 1.20 (0.276) | 60.68 (<0.001) | 57.14 (<0.001) | 53.40 (<0.001) | ||||
| R2 (Δ R2) | 0.022 | 0.549 (0.527) | 0.553 (0.004) | 0.554 (0.001) | ||||
| Δ F (p) | 757.58 (<0.001) | 5.533 (0.019) | 1.045 (0.307) | |||||
| Model1 | Model2 | Model3 | Model4 | |||||
|---|---|---|---|---|---|---|---|---|
| b | p | b | p | b | p | b | p | |
| Gender (Female) | 0.209 | 0.661 | 0.219 | 0.582 | 0.079 | 0.843 | 0.081 | 0.837 |
| Age | 0.052 | 0.345 | 0.017 | 0.709 | −0.004 | 0.929 | −0.010 | 0.832 |
| Education level (High school and vocational school) | ||||||||
| College or above | 0.077 | 0.901 | −0.055 | 0.916 | −0.131 | 0.799 | 0.037 | 0.943 |
| Marital status (Single) | ||||||||
| Married | −0.399 | 0.510 | −0.237 | 0.641 | −0.138 | 0.784 | 0.002 | 0.997 |
| Divorced or other | −1.609 | 0.453 | −2.008 | 0.265 | −1.959 | 0.271 | −1.801 | 0.309 |
| Status of residence (Not living alone) | −1.077 | 0.056 | −1.338 | 0.005 ** | −1.307 | 0.005 ** | −1.369 | 0.003 ** |
| Income (yuan, <5000) | ||||||||
| 5000–10,000 | −1.067 | 0.063 | −0.708 | 0.140 | −0.614 | 0.197 | −0.713 | 0.134 |
| >10,000 | −0.211 | 0.761 | 0.038 | 0.949 | 0.119 | 0.836 | 0.020 | 0.972 |
| Professional title (Junior) | ||||||||
| Intermediate title | 0.644 | 0.243 | −0.202 | 0.666 | −0.155 | 0.736 | −0.223 | 0.629 |
| Senior title | 0.096 | 0.868 | −0.315 | 0.518 | −0.307 | 0.524 | −0.325 | 0.498 |
| Seniority | −0.028 | 0.532 | 0.020 | 0.591 | 0.031 | 0.409 | 0.035 | 0.355 |
| Stress (A) | 0.568 | <0.001 *** | 0.535 | <0.001 *** | 0.487 | <0.001 *** | ||
| Positive affect (B) | −0.111 | <0.001 *** | −0.044 | 0.317 | ||||
| A × B | −0.017 | 0.024 * | ||||||
| Model F (p) | 1.10 (0.359) | 16.32 (<0.001) | 16.27 (<0.001) | 15.62 (<0.001) | ||||
| R2 (Δ R2) | 0.028 | 0.318 (0.290) | 0.336 (0.018) | 0.344 (0.008) | ||||
| Δ F (p) | 178.68 (<0.001) | 10.992 (<0.001) | 5.106 (0.024) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, X.; Luo, R.; Guo, P.; Shang, M.; Zheng, J.; Cai, Y.; Mo, P.K.H.; Lau, J.T.F.; Zhang, D.; Li, J.; et al. Positive Affect Moderates the Influence of Perceived Stress on the Mental Health of Healthcare Workers during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 13600. https://doi.org/10.3390/ijerph192013600
Wang X, Luo R, Guo P, Shang M, Zheng J, Cai Y, Mo PKH, Lau JTF, Zhang D, Li J, et al. Positive Affect Moderates the Influence of Perceived Stress on the Mental Health of Healthcare Workers during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(20):13600. https://doi.org/10.3390/ijerph192013600
Chicago/Turabian StyleWang, Xu, Rui Luo, Pengyue Guo, Menglin Shang, Jing Zheng, Yuqi Cai, Phoenix K. H. Mo, Joseph T. F. Lau, Dexing Zhang, Jinghua Li, and et al. 2022. "Positive Affect Moderates the Influence of Perceived Stress on the Mental Health of Healthcare Workers during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 20: 13600. https://doi.org/10.3390/ijerph192013600
APA StyleWang, X., Luo, R., Guo, P., Shang, M., Zheng, J., Cai, Y., Mo, P. K. H., Lau, J. T. F., Zhang, D., Li, J., & Gu, J. (2022). Positive Affect Moderates the Influence of Perceived Stress on the Mental Health of Healthcare Workers during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(20), 13600. https://doi.org/10.3390/ijerph192013600








