Prevalence of Antimicrobial Prescribing in Long-Term Care Facilities in a Local Health Authority of Northern Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Source Population
2.2. Questionnaire and Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- European Union (EU) Eurostat. Healthcare Resource Statistics—Beds; Eurostat: Luxembourg. 2017. Available online: http://ec.europa.eu/eurostat/statistics-explained/index.php/Healthcare_resource_statistics_-_beds (accessed on 27 January 2022).
- World Health Organisation (WHO). A System of Health Accounts; WHO: Geneva, Switzerland, 2011. Available online: http://www.who.int/health-accounts/methodology/sha2011.pdf (accessed on 27 January 2022).
- Istituto Nazionale di Statistica (ISTAT). Demographic Indicators; ISTAT Publishing: Rome, Italy, 2022; Available online: http://dati.istat.it/Index.aspx?QueryId=18462 (accessed on 27 January 2022).
- Istituto Nazionale di Statistica (ISTAT). I Presidi Residenziali Socio-Assistenziali e Sociosanitari; ISTAT Publishing: Rome, Italy, 2018; Available online: https://www.istat.it/it/archivio/215522 (accessed on 27 January 2022).
- Eurostat Statistics Explained. Population Age Structure by Major Age Groups, 2005 and 2015 (% of Total Population); Eurostat: Luxembourg, 2016. Available online: http://ec.europa.eu/eurostat/statistics-explained/index.php/File:Populat (accessed on 27 January 2022).
- Kojima, G. Frailty as a predictor of disabilities among community-dwelling older people: A systematic review and meta-analysis. Disabil. Rehabil. 2017, 39, 1897–1908. [Google Scholar] [CrossRef] [PubMed]
- Haenen, A.P.J.; Verhoef, L.P.; Beckers, A.; Gijsbers, E.F.; Alblas, J.; Huis, A.; Hulscher, M.E.; de Greeff, S.C. Surveillance of infections in long-term care facilities (LTCFs): The impact of participation during multiple years on healthcare-associated infection incidence. Epidemiol. Infect. 2019, 147, e266. [Google Scholar] [CrossRef]
- Lindsay, E.N. Infection Control in Long-Term Care Facilities. Clin. Infect. Dis. 2000, 31, 752–756. [Google Scholar] [CrossRef]
- van Buul, L.W.; van der Steen, J.T.; Veenhuizen, R.B.; Achterberg, W.P.; Schellevis, F.G.; Essink, R.T.; van Benthem, B.H.; Natsch, S.; Hertogh, C.M. Antibiotic use and resistance in long term care facilities. J. Am. Med. Dir. Assoc. 2012, 13, 568.e1–568.e13. [Google Scholar] [CrossRef] [PubMed]
- Fagan, M.; Mæhlen, M.; Lindbæk, M.; Build, D. Antibiotic prescribing in nursing homes in an area with low prevalence of antibiotic resistance: Compliance with national guidelines. Scand. J. Prim. Health Care 2012, 30, 10–15. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jump, R.L.P.; Crnich, C.J.; Mody, L.; Bradley, S.F.; Nicolle, L.E.; Yoshikawa, T.T. Infectious Diseases in Older Adults of Long-Term Care Facilities: Update on Approach to Diagnosis and Management. J. Am. Geriatr. Soc. 2018, 66, 789–803. [Google Scholar] [CrossRef]
- Brown, K.A.; Khanafer, N.; Daneman, N.; Fisman, D.N. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob. Agents Chemother. 2013, 57, 2326–2332. [Google Scholar] [CrossRef] [PubMed]
- Marston, H.D.; Dixon, D.M.; Knisely, J.M.; Palmore, T.N.; Fauci, A.S. Antimicrobial Resistance. JAMA 2016, 316, 1193–1204. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Surveillance of ANTIMICROBIAL RESISTANCE IN EUROPE—ANNUAL REPORT of the European Antimicrobial Resistance Surveillance Network (EARS-Net) 2017; ECDC: Stockholm, Sweden, 2018; Available online: https://www.ecdc.europa.eu/en/antimicrobial-resistance/surveillance-and-disease-data/data-ecdc (accessed on 25 March 2021).
- Rice, L.B. Antimicrobial Stewardship and Antimicrobial Resistance. Med. Clin. N. Am. 2018, 102, 805–818. [Google Scholar] [CrossRef] [PubMed]
- Neudorf, U.; Boehlcke, K.; Schade, M. Healthcare-associated infections in long-term care facilities (HALT) in Frankfurt am Main, Germany, January to March 2011. Eurosurveillance 2012, 17, 20256. [Google Scholar]
- Plachouras, D.; Kärki, T.; Hansen, S.; Hopkins, S.; Lyytikäinen, O.; Moro, M.L.; Reilly, J.; Zarb, P.; Zingg, W.; Kinross, P.; et al. Antimicrobial use in European acute care hospitals: Results from the second point prevalence survey (PPS) of healthcare-associated infections and antimicrobial use, 2016 to 2017. Eurosurveillance 2018, 23, 1800393, Erratum in Eurosurveillance 2018, 23, 15–28. [Google Scholar] [CrossRef] [PubMed]
- Ripabelli, G.; Scalzo, A.; Mariano, A.; Sammarco, M.L.; Tamburro, M.; Collaborative Group for HAIs Point Prevalence Surveys in Molise Region. Healthcare-associated infections point prevalence survey and antimicrobials use in acute care hospitals (PPS 2016–2017) and long-term care facilities (HALT-3): A comprehensive report of the first experience in Molise Region, Central Italy, and targeted intervention strategies. J. Infect. Public Health 2019, 12, 509–515. [Google Scholar] [CrossRef]
- UK Health Security AgencyEnglish Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR). Report 2017 UK. 2018. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/656611/ESPAUR_report_2017.pdf. (accessed on 24 April 2022).
- France, G.; Taroni, F.; Donatini, A. The Italian health-care system. Health Econ. 2005, 14 (Suppl. S1), S187–S202. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Long-Term Care Facilities. April–May 2013; ECDC: Stockholm, Sweden, 2014; Available online: https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/healthcare-associated-infections-point-prevalence-survey-long-term-care-facilities-2013.pdf (accessed on 24 April 2022).
- Rummukainen, M.L.; Mäkelä, M.; Noro, A.; Finne-Soveri, H.; Lyytikäinen, O. Assessing prevalence of antimicrobial use and infections using the minimal data set in Finnish long-term care facilities. Am. J. Infect. Control 2013, 41, e35–e37. [Google Scholar] [CrossRef] [PubMed]
- Stepan, D.; Ušaj, L.; Petek Šter, M.; Smolinger Galun, M.; Smole, H.; Beović, B. Antimicrobial prescribing in long-term care facilities: A nationwide point-prevalence study, Slovenia, 2016. Eurosurveillance 2018, 23, 1800100. [Google Scholar] [CrossRef]
- Tandan, M.; Burns, K.; Murphy, H.; Hennessy, S.; Cormican, M.; Vellinga, A. Antimicrobial prescribing and infections in long-term care facilities (LTCF): A multilevel analysis of the HALT 2016 study, Ireland, 2017. Eurosurveillance 2018, 23, 1800278. [Google Scholar] [CrossRef]
- Ricchizzi, E.; Latour, K.; Kärki, T.; Buttazzi, R.; Jans, B.; Moro, M.L.; Nakitanda, O.A.; Plachouras, D.; Monnet, D.L.; Suetens, C.; et al. Antimicrobial use in European long-term care facilities: Results from the third point prevalence survey of healthcare-associated infections and antimicrobial use, 2016 to 2017. Eurosurveillance 2018, 23, 1800394. [Google Scholar] [CrossRef]
- Falcone, M.; Paul, M.; Yahav, D.; Orlando, G.; Tiseo, G.; Prendki, V.; Güerri-Fernández, R.; Gavazzi, G.; Mutters, N.T.; Cookson, B.; et al. Antimicrobial consumption and impact of antimicrobial stewardship programmes in long-term care facilities. Clin. Microbiol. Infect. 2019, 25, 562–569. [Google Scholar] [CrossRef]
- Latour, K.; Catry, B.; Bronx, E.; Vankerckhoven, V.; Muller, A.; Stroobants, R.; Goossens, H.; Jans, B.; European Surveillance of Antimicrobial Consumption Project Group. Indications for antimicrobial prescribing in European nursing homes: Results from a point prevalence survey. Pharmacoepidemiol. Drug Saf. 2012, 21, 937–944. [Google Scholar] [CrossRef]
- Wu, L.D.; Walker, S.A.; Ellingsen, M.; Palma, L.; Simor, A.; Daneman, N. Antibiotic Use and Need for Antimicrobial Stewardship in Long-Term Care. Can. J. Hosp. Pharm. 2015, 68, 445–449, Erratum in Can. J. Hosp. Pharm. 2017, 70, 224. [Google Scholar] [CrossRef]
- Héquet, D.; Kessler, S.; Rettenmund, G.; Lemmenmeier, E.; Qalla-Widmer, L.; Gardiol, C.; Münzer, T.; Schlegel, M.; Petignat, C.; Kohler, P. Healthcare-associated infections and antibiotic use in long-term care residents from two geographical regions in Switzerland. J. Hosp. Infect. 2021, 117, 172–178. [Google Scholar] [CrossRef] [PubMed]
- de Lastours, V.; Fantin, B. Impact of fluoroquinolones on human microbiota. Focus on the emergence of antibiotic resistance. Future Microbiol. 2015, 10, 1241–1255. [Google Scholar] [CrossRef] [PubMed]
- van Buul, L.W.; Veenhuizen, R.B.; Achterberg, W.P.; Schellevis, F.G.; Essink, R.T.; de Greeff, S.C.; Natsch, S.; van der Steen, J.T.; Hertogh, C.M. Antibiotic prescribing in Dutch nursing homes: How appropriate is it? J. Am. Med. Dir. Assoc. 2015, 16, 229–237. [Google Scholar] [CrossRef]
- CDC. The Core Elements of Antibiotic Stewardship for Nursing Homes; US Department of Health and Human Services, CDC: Atlanta, GA, USA, 2015. Available online: http://www.cdc.gov/longtermcare/index.html (accessed on 10 October 2022).
- Parnham, M.J.; Erakovic Haber, V.; Giamarellos-Bourboulis, E.J.; Peretti, G.; Verleden, G.M.; Vos, R. Azithromycin: Mechanisms of action and their relevance for clinical applications. Pharmacol. Ther. 2014, 143, 225–245. [Google Scholar] [CrossRef] [PubMed]
- Ayerbe, L.; Risco-Risco, C.; Forgnone, I.; Pérez-Piñar, M.; Ayis, S. Azithromycin in patients with COVID-19: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2022, 77, 303–309. [Google Scholar] [CrossRef]
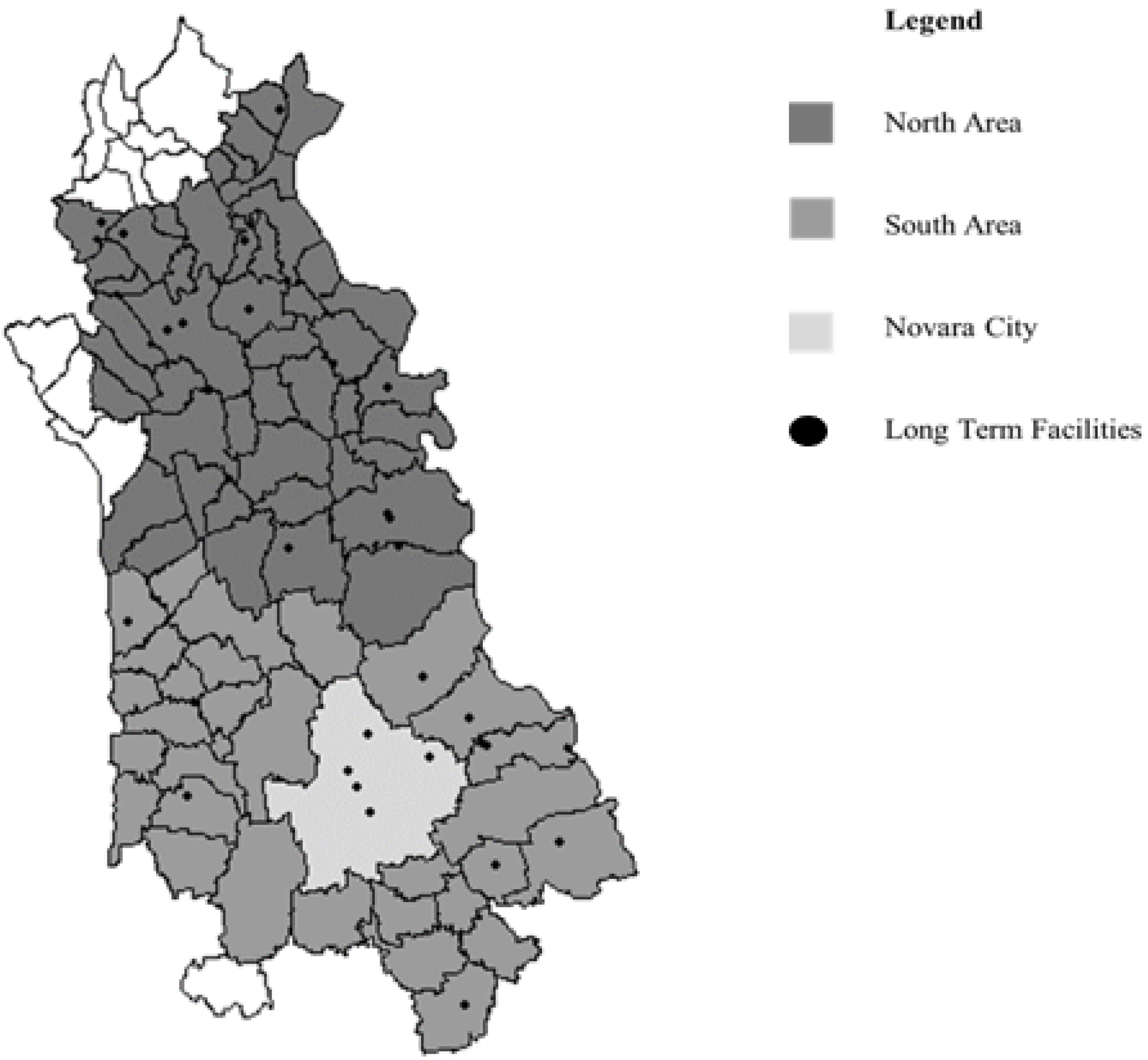

| N = 25 | |
|---|---|
| District, N (%) | |
| North area | 14 (56%) |
| South area | 8 (32%) |
| Novara city | 3 (12%) |
| N° of available beds, median (IQR) | 58 (35–65) |
| N° of occupied beds, median (IQR) | 41 (33–57) |
| N° medical assistants, median (IQR) | 16 (13–20) |
| N° of nurses, median (IQR) | 4 (3–5) |
| N° of physicians, median (IQR) | 1 (1–1) |
| Antibiotic Users N = 26 | |
|---|---|
| N (%) | |
| Infection site | |
| Others | 1 (4.55) |
| Skin/wound | 1 (4.55) |
| Surgical site | 1 (4.55) |
| Gastrointestinal tract | 1 (4.55) |
| Genital tract | 1 (4.55) |
| Respiratory tract | 13 (59.09) |
| Urinary tract | 4 (18.18) |
| Missing | 4 |
| Test to evaluate infection | |
| No | 15 (62.50) |
| Yes | 9 (37.50) |
| Missing | 2 |
| Test material | |
| Expectoration | 6 (66.67) |
| Feces/recap swab | 1 (11.11) |
| Urine | 2 (22.22) |
| Missing | 17 |
| Agent | |
| Klebsiella pneumoniae | 1 (12.50) |
| SARS-CoV-2 | 6 (75.00) |
| Others | 1 (12.50) |
| Missing | 18 |
| Compound | |
| Amoxicillin and beta-lactamase inhibitor | 5 (22.73) |
| Azithromycin | 4 (18.18) |
| Cefixime | 1 (4.55) |
| Ceftriaxone | 1 (4.55) |
| Ciprofloxacin | 1 (4.55) |
| Clarithromycin | 1 (4.55) |
| Fosfomycin | 1 (4.55) |
| Gentamicin | 1 (4.55) |
| Levofloxacin | 2 (9.09) |
| Teicoplanin | 1 (4.55) |
| Sulfamethoxazole and trimethoprim | 1 (4.55) |
| Vancomycin | 1 (4.55) |
| Missing | 6 |
| Route of administration | |
| Intravenous | 2 (7.69) |
| Intramuscular | 2 (7.69) |
| Oral | 22 (84.62) |
| Therapy type | |
| Other | 1 (4.00) |
| Empirical | 16 (64.00) |
| Targeted | 5 (20.00) |
| Preventive | 3 (12.00) |
| Missing | 1 |
| Treatment duration (days) | 6 (5–8) |
| Variable | Antibiotic Use | |||
|---|---|---|---|---|
| No N = 1015 | Yes N = 25 | Total N = 1040 | Chi-Squared Test p-Value | |
| N (%) | N (%) | N (%) | ||
| Sex | ||||
| Males | 234 (23.08) | 10 (40.00) | 244 (23.48) | 0.0486 |
| Females | 780 (76.92) | 15 (60.00) | 795 (76.52) | |
| Missing | 1 | 0 | 1 | |
| Age, mean (SD) | 84.59 (9.82) | 84.36 (7.46) | 84.58 (9.77) | 0.9159 ^ |
| Urinary incontinence | ||||
| No | 252 (23.84) | 4 (16.00) | 256 (24.62) | 0.3114 |
| Yes | 763 (75.17) | 21 (84.00) | 784 (75.38) | |
| Bowel incontinence | ||||
| No | 419 (41.28) | 9 (36.00) | 428 (41.15) | 0.5861 |
| Yes | 596 (58.72) | 16 (64.00) | 612 (58.85) | |
| Dementia | ||||
| No | 471 (49.01) | 13 (52.00) | 484 (49.09) | 0.7679 |
| Yes | 490 (50.99) | 12 (48.00) | 502 (50.91) | |
| Missing | 54 | 0 | 54 | |
| Pressure sores | ||||
| No | 955 (94.18) | 22 (88.00) | 977 (94.03) | 0.1974 |
| Yes | 59 (5.82) | 3 (12.00) | 62 (5.97) | |
| Missing | 1 | 0 | 1 | |
| Other wounds | ||||
| No | 976 (96.16) | 22 (88.00) | 998 (95.96) | 0.0759 * |
| Yes | 39 (3.84) | 3 (12.00) | 42 (4.04) | |
| Wheelchair | ||||
| No | 396 (39.01) | 14 (56.00) | 410 (39.42) | 0.0860 |
| Yes | 619 (60.99) | 11 (44.00) | 630 (60.58) | |
| Immobilized patient | ||||
| No | 993 (97.93) | 17 (68.00) | 1010 (97.40) | <0.0001 * |
| Yes | 21 (2.07) | 6 (24.00) | 27 (2.60) | |
| Missing | 1 | 2 | 3 | |
| Nasogastric probe | ||||
| No | 1009 (99.41) | 25 (10.00) | 1034 (99.42) | 1.0000* |
| Yes | 6 (0.59) | 0 (0.00) | 6 (0.58) | |
| Central venous catheter | ||||
| No | 1014 (99.90) | 24 (96.00) | 1038 (99.81) | 0.0475 * |
| Yes | 1 (0.10) | 1 (4.00) | 2 (0.19) | |
| Peripheral venous catheter | ||||
| No | 988 (97.44) | 19 (82.61) | 1007 (97.11) | 0.0034 * |
| Yes | 26 (2.56) | 4 (17.39) | 30 (2.89) | |
| Missing | 1 | 2 | 3 | |
| Urinary catheter | ||||
| No | 953 (93.89) | 18 (72.00) | 971 (93.37) | 0.0008 * |
| Yes | 62 (6.11) | 7 (28.00) | 69 (6.63) | |
| Dialysis | ||||
| No | 1011 (99.61) | 25 (10.00) | 1036 (99.62) | 1.0000 * |
| Yes | 4 (0.39) | 0 (0.00) | 4 (0.38) | |
| Hospitalization (48 h before the interview) | ||||
| No | 1009 (99.41) | 24 (96.00) | 1033 (99.33) | 0.1570 * |
| Yes | 6 (0.59) | 1 (4.00) | 7 (0.67) | |
| Previous surgery (30–90 days before the interview) | ||||
| No | 1005 (99.21) | 24 (96.00) | 1029 (99.13) | 0.1977 * |
| Yes | 8 (0.79) | 1 (4.00) | 9 (0.87) | |
| Missing | 2 | 0 | 2 | |
| Infection or colonization | ||||
| No infection/colonization | 953 (95.78) | 5 (20.00) | 958 (93.92) | <0.0001 * |
| Colonization | 2 (0.20) | 0 (0.00) | 2 (0.20) | |
| Probable infection/colonization | 32 (3.22) | 11 (44.00) | 43 (4.22) | |
| Confirmed infection/colonization | 8 (0.80) | 9 (36.00) | 17 (1.67) | |
| Missing | 20 | 0 | 20 | |
| Antibiotic Users | Total | |||
|---|---|---|---|---|
| N = 26 | N = 1040 | |||
| N | N | Prevalence (p) | 95%CI | |
| Sex | ||||
| Males | 10 | 244 | 4.10% | 4.07–4.13 |
| Females | 15 | 795 | 1.89% | 1.88–1.89 |
| Immobilized patient | ||||
| No | 17 | 1010 | 1.68% | 1.68–1.69 |
| Yes | 2 | 27 | 7.41% | 6.91–7.91 |
| Central venous catheter | ||||
| No | 24 | 1038 | 2.31% | 2.31–2.32 |
| Yes | 1 | 2 | 50.00% | 25.5–74.50 |
| Peripheral venous catheter | ||||
| No | 19 | 1007 | 1.89% | 1.88–1.89 |
| Yes | 4 | 30 | 13.33% | 12.58–14.09 |
| Urinary catheter | ||||
| No | 18 | 971 | 1.85% | 1.85–1.86 |
| Yes | 7 | 69 | 10.14% | 9.89–10.40 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarro, A.; Di Nardo, F.; Andreoletti, M.; Airoldi, C.; Scotti, L.; Panella, M. Prevalence of Antimicrobial Prescribing in Long-Term Care Facilities in a Local Health Authority of Northern Italy. Int. J. Environ. Res. Public Health 2022, 19, 13412. https://doi.org/10.3390/ijerph192013412
Sarro A, Di Nardo F, Andreoletti M, Airoldi C, Scotti L, Panella M. Prevalence of Antimicrobial Prescribing in Long-Term Care Facilities in a Local Health Authority of Northern Italy. International Journal of Environmental Research and Public Health. 2022; 19(20):13412. https://doi.org/10.3390/ijerph192013412
Chicago/Turabian StyleSarro, Andrea, Francesco Di Nardo, Michela Andreoletti, Chiara Airoldi, Lorenza Scotti, and Massimiliano Panella. 2022. "Prevalence of Antimicrobial Prescribing in Long-Term Care Facilities in a Local Health Authority of Northern Italy" International Journal of Environmental Research and Public Health 19, no. 20: 13412. https://doi.org/10.3390/ijerph192013412
APA StyleSarro, A., Di Nardo, F., Andreoletti, M., Airoldi, C., Scotti, L., & Panella, M. (2022). Prevalence of Antimicrobial Prescribing in Long-Term Care Facilities in a Local Health Authority of Northern Italy. International Journal of Environmental Research and Public Health, 19(20), 13412. https://doi.org/10.3390/ijerph192013412








