Predicting Physical Activity in Chinese Pregnant Women Using Multi-Theory Model: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
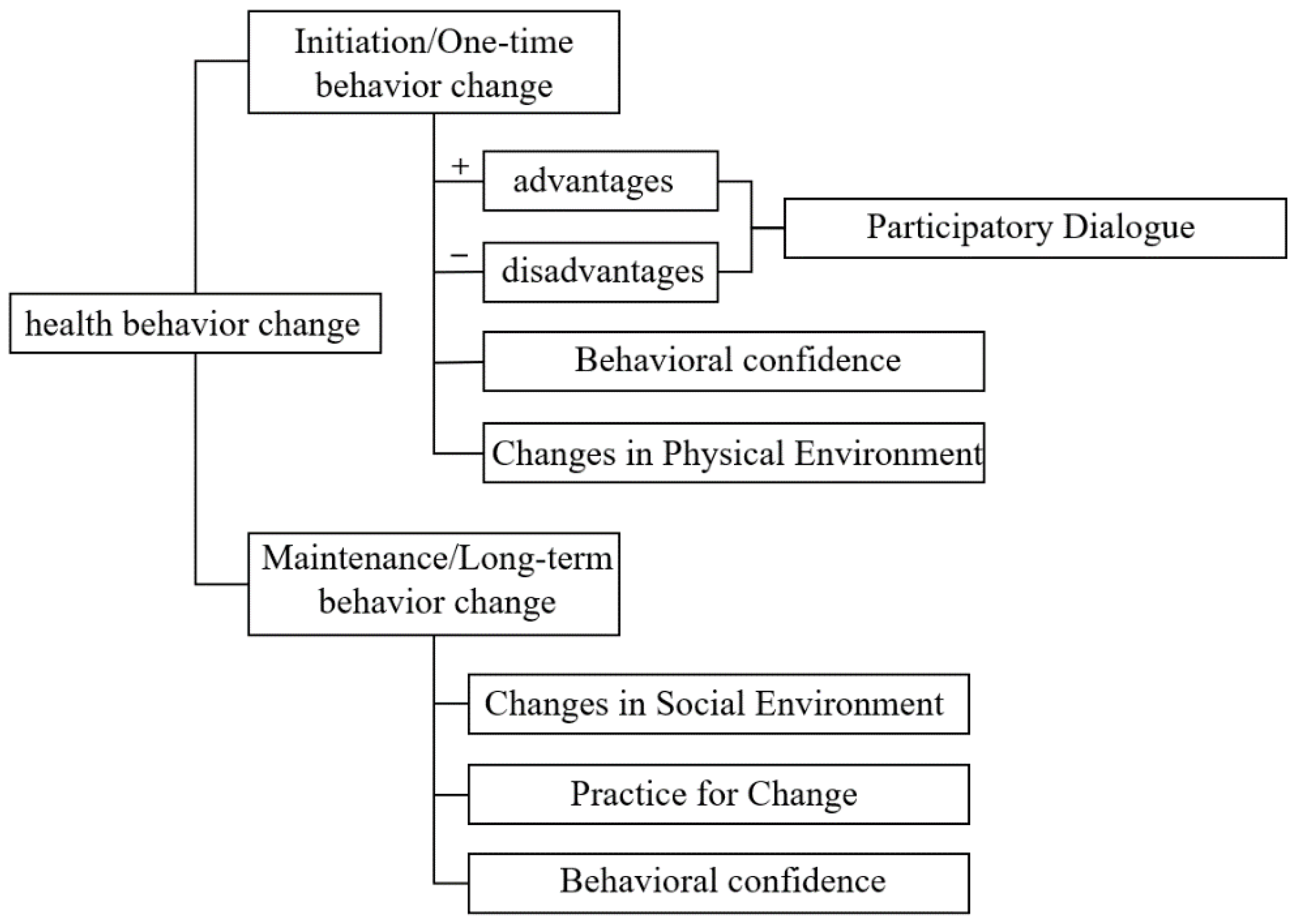
2.2. Instrument
2.2.1. General Questionnaire
2.2.2. Measuring Change in Physical Activity Questionnaire
2.3. Data Collection
2.4. Data Analysis
2.4.1. Construct Validity
2.4.2. Reliability
2.4.3. Floor/Ceiling Effect
2.5. Ethical Consideration
2.6. Sample Size
3. Results
3.1. Demographics, and Descriptive Statistics
3.2. Reliability
3.3. Validity
3.3.1. Exploratory Factor Analysis (EFA)
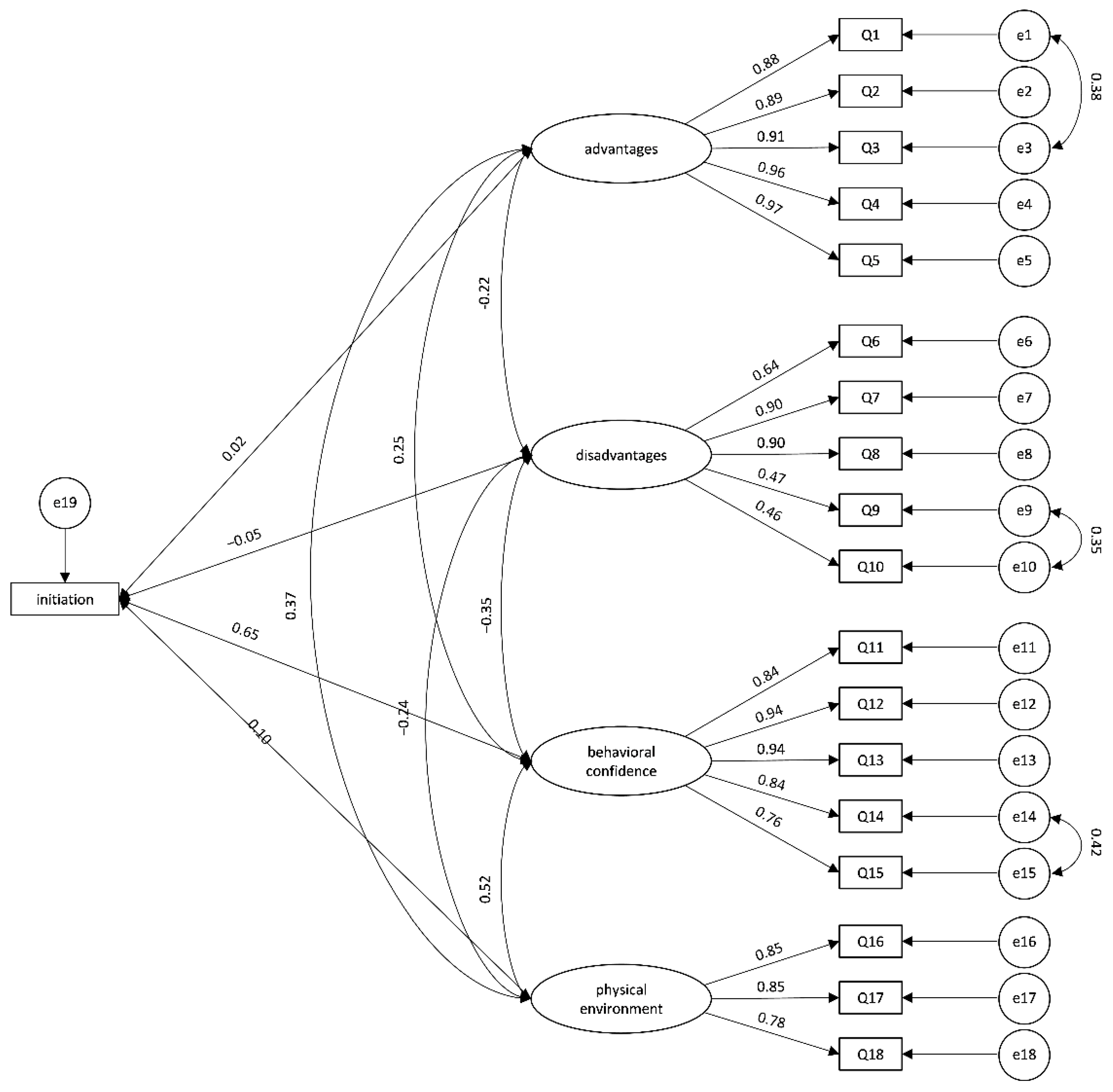
3.3.2. Confirmatory Factor Analysis (CFA)
3.4. Stepwise Multiple Regression
3.5. Ceiling/Floor Effect
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dipietro, L.; Evenson, K.R.; Bloodgood, B.; Sprow, K.; Troiano, R.P.; Piercy, K.L.; Vaux-Bjerke, A.; Powell, K.E. Benefits of Physical Activity during Pregnancy and Postpartum: An Umbrella Review. Med. Sci. Sports Exerc. 2019, 51, 1292–1302. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, A.; van der Waerden, J.; Melchior, M.; Bolze, C.; El-Khoury, F.; Pryor, L. Physical activity during pregnancy and postpartum depression: Systematic review and meta-analysis. J. Affect. Disord. 2019, 246, 29–41. [Google Scholar] [CrossRef] [PubMed]
- Barakat, R.; Refoyo, I.; Coteron, J.; Franco, E. Exercise during pregnancy has a preventative effect on excessive maternal weight gain and gestational diabetes. A randomized controlled trial. Braz. J. Phys. Ther. 2019, 23, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.W.H.; Au Yeung, E.; Law, B.M.H. Effectiveness of Physical Activity Interventions on Pregnancy-Related Outcomes among Pregnant Women: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 1840. [Google Scholar] [CrossRef]
- Savvaki, D.; Taousani, E.; Goulis, D.G.; Tsirou, E.; Voziki, E.; Douda, H.; Nikolettos, N.; Tokmakidis, S.P. Guidelines for exercise during normal pregnancy and gestational diabetes: A review of international recommendations. Hormones 2018, 17, 521–529. [Google Scholar] [CrossRef]
- Zhang, Y.; Dong, S.; Zuo, J.; Hu, X.; Zhang, H.; Zhao, Y. Physical activity level of urban pregnant women in Tianjin, China: A cross-sectional study. PLoS ONE 2014, 9, e109624. [Google Scholar] [CrossRef]
- Ning, Y.; Williams, M.A.; Dempsey, J.C.; Sorensen, T.K.; Frederick, I.O.; Luthy, D.A. Correlates of recreational physical activity in early pregnancy. J. Matern. Fetal. Neonatal. Med. 2003, 13, 385–393. [Google Scholar] [CrossRef]
- Bauer, P.W.; Broman, C.L.; Pivarnik, J.M. Exercise and pregnancy knowledge among healthcare providers. J. Women’s Health 2010, 19, 335–341. [Google Scholar] [CrossRef]
- Okafor, U.B.; Goon, D.T. Uncovering Barriers to Prenatal Physical Activity and Exercise Among South African Pregnant Women: A Cross-Sectional, Mixed-Method Analysis. Front. Public Health 2022, 10, 697386. [Google Scholar] [CrossRef]
- Nahar, V.K.; Sharma, M.; Catalano, H.P.; Ickes, M.J.; Johnson, P.; Ford, M.A. Testing multi-theory model (MTM) in predicting initiation and sustenance of physical activity behavior among college students. Health Promot. Perspect. 2016, 6, 58–65. [Google Scholar] [CrossRef]
- Sharma, M.; Khubchandani, J.; Nahar, V.K. Applying a new theory to smoking cessation: Case of multi-theory model (MTM) for health behavior change. Health Promot. Perspect. 2017, 7, 102–105. [Google Scholar] [CrossRef]
- Sharma, M.; Catalano, H.P.; Nahar, V.K.; Lingam, V.C.; Johnson, P.; Ford, M.A. Applying Multi-Theory Model (MTM) of Health Behavior Change to Predict Water Consumption Instead of Sugar-Sweetened Beverages. J. Res. Health Sci. 2017, 17, e00370. [Google Scholar]
- Hayes, T.; Sharma, M. Applying the integrated marketing communication approach to recruit and retain African American women. Health Promot. Perspect. 2021, 11, 460–466. [Google Scholar] [CrossRef]
- Sharma, M.; Asare, M.; Lakhan, R.; Kanekar, A.; Nahar, V.K.; Moonie, S. Can the Multi-Theory Model (MTM) of Health Behavior Change Explain the Intent for People to Practice Meditation? J. Evid. Based Integr. Med. 2021, 26, 1–12. [Google Scholar] [CrossRef]
- Davis, R.E.; Sharma, M.; Simon, K.E.; Wilkerson, A.H. Conceptualization of college students’ COVID-19 related mask-wearing behaviors using the Multi-Theory Model of health behavior change. Health Promot. Perspect. 2021, 11, 194–201. [Google Scholar] [CrossRef]
- Batra, K.; Sharma, M.; Dai, C.L.; Khubchandani, J. COVID-19 Booster Vaccination Hesitancy in the United States: A Multi-Theory-Model (MTM)-Based National Assessment. Vaccines 2022, 10, 758. [Google Scholar] [CrossRef]
- Sharma, M.; Davis, R.E.; Wilkerson, A.H. COVID-19 Vaccine Acceptance among College Students: A Theory-Based Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4617. [Google Scholar] [CrossRef]
- Sharma, A.; Jain, M.; Nahar, V.K.; Sharma, M. Determining predictors of change in sugar sweetened beverage consumption behaviour among university students in India. Int. J. Adolesc. Med. Health 2020, 34, 78. [Google Scholar] [CrossRef]
- Kumar, V.; Sabbarwal, B.; Jaggi, A.; Taneja, P. Effectiveness of tobacco cessation counselling and behavioural changes Using Multi Theory Model (MTM): A follow-up study. Indian J. Dent Res. 2021, 32, 56–60. [Google Scholar] [CrossRef]
- Morowatisharifabad, M.A.; Yoshany, N.; Bahri, N.; Sharma, M.; Jambarsang, S.; Karimiankakolaki, Z. Effects of an educational intervention based on the multi-theory model on promoting the quality of life in postmenopausal women: A protocol. Prz Menopauzalny 2019, 18, 153–160. [Google Scholar] [CrossRef]
- Hayes, T.; Sharma, M.; Shahbazi, M.; Sung, J.H.; Bennett, R.; Reese-Smith, J. The evaluation of a fourth-generation multi-theory model (MTM) based intervention to initiate and sustain physical activity. Health Promot. Perspect. 2019, 9, 13–23. [Google Scholar] [CrossRef]
- Sharma, M.; Batra, K.; Johansen, C.; Raich, S. Explaining Correlates of Cervical Cancer Screening among Minority Women in the United States. Pharmacy 2022, 10, 30. [Google Scholar] [CrossRef]
- Sharma, M.; Batra, K.; Davis, R.E.; Wilkerson, A.H. Explaining Handwashing Behavior in a Sample of College Students during COVID-19 Pandemic Using the Multi-Theory Model (MTM) of Health Behavior Change: A Single Institutional Cross-Sectional Survey. Healthcare 2021, 9, 55. [Google Scholar] [CrossRef]
- Sharma, M.; Batra, K.; Singh, T.P.; Dua, R.; Ickes, M.; Batra, R.; Nahar, V.K. Explaining Screen-Time Behavior Among Preschoolers in Northern India Using Multi Theory Model: A Parental Cross-Sectional Survey. Int. Q. Community Health Educ. 2021, 43, 95–104. [Google Scholar] [CrossRef]
- Metzger, B.E.; Gabbe, S.G.; Persson, B.; Buchanan, T.A.; Catalano, P.A.; Damm, P.; Dyer, A.R.; Leiva, A.; Hod, M.; Kitzmiler, J.L.; et al. International Association of Diabetes and Pregnancy Study Groups Recommendations on the Diagnosis and Classification of Hyperglycemia in Pregnancy. Diabetes Care 2010, 33, 676–682. [Google Scholar] [CrossRef]
- Jinhua, Y.; Yaoyue, L.U.O.; Xiaojian, J.; Qing, Q.I.U.; Ding, Z.; Liangrong, Z. Reliability and validity test of Chinese version of Measuring Change in Physical Activity Questionnaire in hypertensives. Chin. Nurs. Manag. 2022, 22, 43–48. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guildford Press: New York, NY, USA, 2015; pp. 155–156. [Google Scholar]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E.; Education, P. Multivariate Data Analysis: Pearson New International Edition. Pearson Schweiz Ag 2013, 3, 128–134. [Google Scholar]
- Hayes, T.; Nahar, V.K.; Sharma, M. Predicting Physical Activity Behavior in African American Females: Using Multi Theory Model. J. Res. Health Sci. 2018, 18, e00410. [Google Scholar]
- Abdolaliyan, N.; Shahnazi, H.; Kzemi, A.; Hasanzadeh, A. Determinants of the self-efficacy of physical activity for maintaining weight during pregnancy: The application of the health belief model. J. Educ. Health Promot. 2017, 6, 93. [Google Scholar]
- Kazemi, A.; Toghiyani, Z.; Nekoei-Zahraei, N. Using social cognitive theory to explain physical activity in Iranian women preparing for pregnancy. Women Health 2020, 60, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Zhu, G.; Qian, X.; Qi, L.; Xia, C.; Ming, Y.; Zeng, Z.; Liu, Y.; Yang, Y.; Zhang, M.; Zhang, H. The intention to undertake physical activity in pregnant women using the theory of planned behaviour. J. Adv. Nurs. 2020, 76, 1647–1657. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.C.; Abreu, S.; Moreira, C.; Santos, R.; Ferreira, M.; Alves, O.; Moreira, P.; Mota, J. Physical Activity Patterns During Pregnancy in a Sample of Portuguese Women: A Longitudinal Prospective Study. Iran. Red Crescent Med. J. 2016, 18, e22455. [Google Scholar] [CrossRef] [PubMed]
- Borodulin, K.M.; Evenson, K.R.; Wen, F.; Herring, A.H.; Benson, A.M. Physical activity patterns during pregnancy. Med. Sci. Sports Exerc. 2008, 40, 1901–1908. [Google Scholar] [CrossRef]
- Vietheer, A.; Kiserud, T.; Lie, R.T.; Haaland, Ø.A.; Kessler, J. Sleep and physical activity from before conception to the end of pregnancy in healthy women: A longitudinal actigraphy study. Sleep Med. 2021, 83, 89–98. [Google Scholar] [CrossRef]
- Melzer, K.; Schutz, Y.; Boulvain, M.; Kayser, B. Physical activity and pregnancy: Cardiovascular adaptations, recommendations and pregnancy outcomes. Sports Med. 2010, 40, 493–507. [Google Scholar] [CrossRef]
- Mottola, M.F.; Davenport, M.H.; Ruchat, S.M.; Davies, G.A.; Poitras, V.J.; Gray, C.E.; Jaramillo Garcia, A.; Barrowman, N.; Adamo, K.B.; Duggan, M.; et al. 2019 Canadian guideline for physical activity throughout pregnancy. Br. J. Sports Med. 2018, 52, 1339–1346. [Google Scholar] [CrossRef]
- Syed, H.; Slayman, T.; DuChene Thoma, K. ACOG Committee Opinion No. 804: Physical Activity and Exercise During Pregnancy and the Postpartum Period. Obstet. Gynaecol. 2021, 137, 375–376. [Google Scholar] [CrossRef]
- Juan, J.; Yang, H. Prevalence, Prevention, and Lifestyle Intervention of Gestational Diabetes Mellitus in China. Int. J. Environ. Res. Public Health 2020, 17, 9517. [Google Scholar] [CrossRef]
- Bacchi, E.; Bonin, C.; Zanolin, M.E.; Zambotti, F.; Livornese, D.; Donà, S.; Tosi, F.; Baldisser, G.; Ihnatava, T.; Di Sarra, D.; et al. Physical Activity Patterns in Normal-Weight and Overweight/Obese Pregnant Women. PLoS ONE 2016, 11, e0166254. [Google Scholar] [CrossRef]
- Fahrenwald, N.L.; Walker, S.N. Application of the Transtheoretical Model of behavior change to the physical activity behavior of WIC mothers. Public Health Nurs. 2003, 20, 307–317. [Google Scholar] [CrossRef]
- Haakstad, L.A.; Voldner, N.; Bø, K. Stages of change model for participation in physical activity during pregnancy. J. Pregnancy 2013, 2013, 193170. [Google Scholar] [CrossRef]
- Lee, C.F.; Chiang, I.C.; Hwang, F.M.; Chi, L.K.; Lin, H.M. Using the Theory of Planned Behavior to predict pregnant women’s intention to engage in regular exercise. Midwifery 2016, 42, 80–86. [Google Scholar] [CrossRef]
- Gaston, A.; Cramp, A. Exercise during pregnancy: A review of patterns and determinants. J. Sci. Med. Sport 2011, 14, 299–305. [Google Scholar] [CrossRef]
- Ahmadi, K.; Amiri-Farahani, L.; Haghani, S.; Hasanpoor-Azghady, S.B.; Pezaro, S. Exploring the intensity, barriers and correlates of physical activity In Iranian pregnant women: A cross-sectional study. BMJ Open Sport Exerc. Med. 2021, 7, e001020. [Google Scholar]

| Variables | n | % |
|---|---|---|
| Age (years) | ||
| <35 | 375 | 83.3 |
| ≥35 | 75 | 16.7 |
| Education | ||
| Junior high school or less | 19 | 4.2 |
| Senior high school/Specialized Secondary School | 36 | 8.0 |
| College/University | 339 | 75.3 |
| Graduate school | 56 | 12.4 |
| Nationality | ||
| Han | 441 | 98.0 |
| National minority | 9 | 2.0 |
| Religion | ||
| Atheist | 372 | 82.7 |
| Christianity | 11 | 2.4 |
| Buddhism | 37 | 8.2 |
| Other | 30 | 6.7 |
| Residence | ||
| Urban | 373 | 82.9 |
| Rural | 77 | 17.1 |
| Working Status | ||
| Employed | 410 | 91.1 |
| Student | 1 | 0.2 |
| Unemployed | 40 | 8.9 |
| Monthly family income per capita (CNY) | ||
| ≤4000 | 12 | 2.7 |
| 4000–8000 | 115 | 25.6 |
| 8000–12,000 | 156 | 34.7 |
| ≥12,000 | 167 | 37.1 |
| Pre-pregnancy BMI (kg/m2) | ||
| Underweight (<18.5) | 70 | 15.6 |
| Normal (18.5–23.9) | 321 | 71.3 |
| Overweight and Obese (≥24.0) | 59 | 13.1 |
| Pre-pregnancy exercise habit | ||
| Yes | 226 | 50.2 |
| No | 224 | 49.8 |
| Parity | ||
| 1 | 327 | 72.7 |
| >1 | 123 | 27.3 |
| Medical insurance | ||
| Yes | 411 | 91.3 |
| No | 39 | 8.7 |
| Gestation age | ||
| First trimester (≤13) | 48 | 11.8 |
| Second trimester (14–27) | 239 | 53.1 |
| Third trimester (≥28) | 163 | 36.2 |
| GDM 1 | ||
| Yes | 80 | 17.8 |
| No | 370 | 82.2 |
| Constructs | Possible Range | Observed Range | Mean (SD) | Cronbach’s Alpha |
|---|---|---|---|---|
| Initiation | 0 to 4 | 0 to 4 | 2.30(1.08) | N.A. 1 |
| Participatory Dialogue: Advantages | 0 to 20 | 0 to 20 | 16.56(4.01) | 0.960 |
| Participatory Dialogue: Disadvantages | 0 to 20 | 0 to 20 | 6.96(4.01) | 0.850 |
| Participatory Dialogue: Advantages—Disadvantages score | −20 to 20 | −20 to 20 | 9.60(6.47) | N.A. |
| Behavioral confidence | 0 to 20 | 0 to 20 | 11.31(4.74) | 0.938 |
| Change in Physical Environment | 0 to 12 | 0 to 12 | 7.22(2.91) | 0.861 |
| All constructs of Initiation Model | N.A. | N.A. | N.A. | 0.766 |
| Maintenance | 0 to 4 | 0 to 4 | 2.24(1.09) | N.A. |
| Emotional Transformation | 0 to 12 | 0 to 12 | 7.96(2.35) | 0.937 |
| Practice for Change | 0 to 12 | 0 to 12 | 4.00(2.50) | 0.834 |
| Change in Social Environment | 0 to 12 | 0 to 12 | 7.07(2.70) | 0.755 |
| All Constructs of Sustenance Model | N.A. | N.A. | N.A. | 0.863 |
| Entire Scale | N.A. | N.A. | N.A. | 0.857 |
| Item | Factor Loading | |||
|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | |
| Q4 | 0.911 | |||
| Q5 | 0.901 | |||
| Q3 | 0.881 | |||
| Q1 | 0.874 | |||
| Q2 | 0.860 | |||
| Q13 | 0.856 | |||
| Q12 | 0.840 | |||
| Q11 | 0.837 | |||
| Q14 | 0.837 | |||
| Q15 | 0.826 | |||
| Q7 | 0.843 | |||
| Q8 | 0.839 | |||
| Q6 | 0.809 | |||
| Q10 | 0.770 | |||
| Q9 | 0.718 | |||
| Q18 | 0.819 | |||
| Q17 | 0.816 | |||
| Q16 | 0.787 | |||
| Item | Factor Loading | ||
|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | |
| Q19 | 0.881 | ||
| Q20 | 0.881 | ||
| Q21 | 0.881 | ||
| Q23 | 0.836 | ||
| Q24 | 0.817 | ||
| Q22 | 0.801 | ||
| Q26 | 0.870 | ||
| Q27 | 0.776 | ||
| Q25 | 0.677 | ||
| Variables | B | SEB | β | 95% CI for B | p-Value |
|---|---|---|---|---|---|
| Participatory dialogue | 0.030 | 0.009 | 0.118 | 0.012, 0.049 | 0.002 |
| Behavioral confidence | 0.128 | 0.009 | 0.560 | 0.109, 0.146 | <0.001 |
| Changes in Physical Environment | 0.041 | 0.015 | 0.111 | 0.013, 0.070 | 0.005 |
| Gestation age | −0.192 | 0.057 | −0.112 | −0.304, −0.080 | 0.001 |
| GDM | 0.408 | 0.096 | 0.142 | 0.218.0.598 | <0.001 |
| Variables | B | SEB | β | 95% CI for B | p-Value |
|---|---|---|---|---|---|
| Emotional Transformation | 0.197 | 0.021 | 0.424 | 0.156, 0.238 | <0.001 |
| Practice for Change | 0.083 | 0.018 | 0.188 | 0.047, 0.118 | <0.001 |
| Changes in Social Environment | 0.063 | 0.016 | 0.155 | 0.031, 0.094 | <0.001 |
| Pre-pregnancy exercise habit | −0.251 | 0.074 | −0.121 | −0.396, −0.106 | 0.001 |
| GDM | 0.298 | 0.100 | 0.103 | 0.102, 0.495 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, W.; Jin, Y.; Liu, N.; Xiang, Z.; Wang, X.; Xu, P.; Guo, P.; Mao, M.; Feng, S. Predicting Physical Activity in Chinese Pregnant Women Using Multi-Theory Model: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 13383. https://doi.org/10.3390/ijerph192013383
Zhang W, Jin Y, Liu N, Xiang Z, Wang X, Xu P, Guo P, Mao M, Feng S. Predicting Physical Activity in Chinese Pregnant Women Using Multi-Theory Model: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(20):13383. https://doi.org/10.3390/ijerph192013383
Chicago/Turabian StyleZhang, Wei, Ying Jin, Ningning Liu, Zhenzhen Xiang, Xiaojuan Wang, Ping Xu, Pingping Guo, Minna Mao, and Suwen Feng. 2022. "Predicting Physical Activity in Chinese Pregnant Women Using Multi-Theory Model: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 20: 13383. https://doi.org/10.3390/ijerph192013383
APA StyleZhang, W., Jin, Y., Liu, N., Xiang, Z., Wang, X., Xu, P., Guo, P., Mao, M., & Feng, S. (2022). Predicting Physical Activity in Chinese Pregnant Women Using Multi-Theory Model: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(20), 13383. https://doi.org/10.3390/ijerph192013383






