The Effect of Physical Activity on Sleep Quality among Older Stroke Survivors: Secondary Analysis from a Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
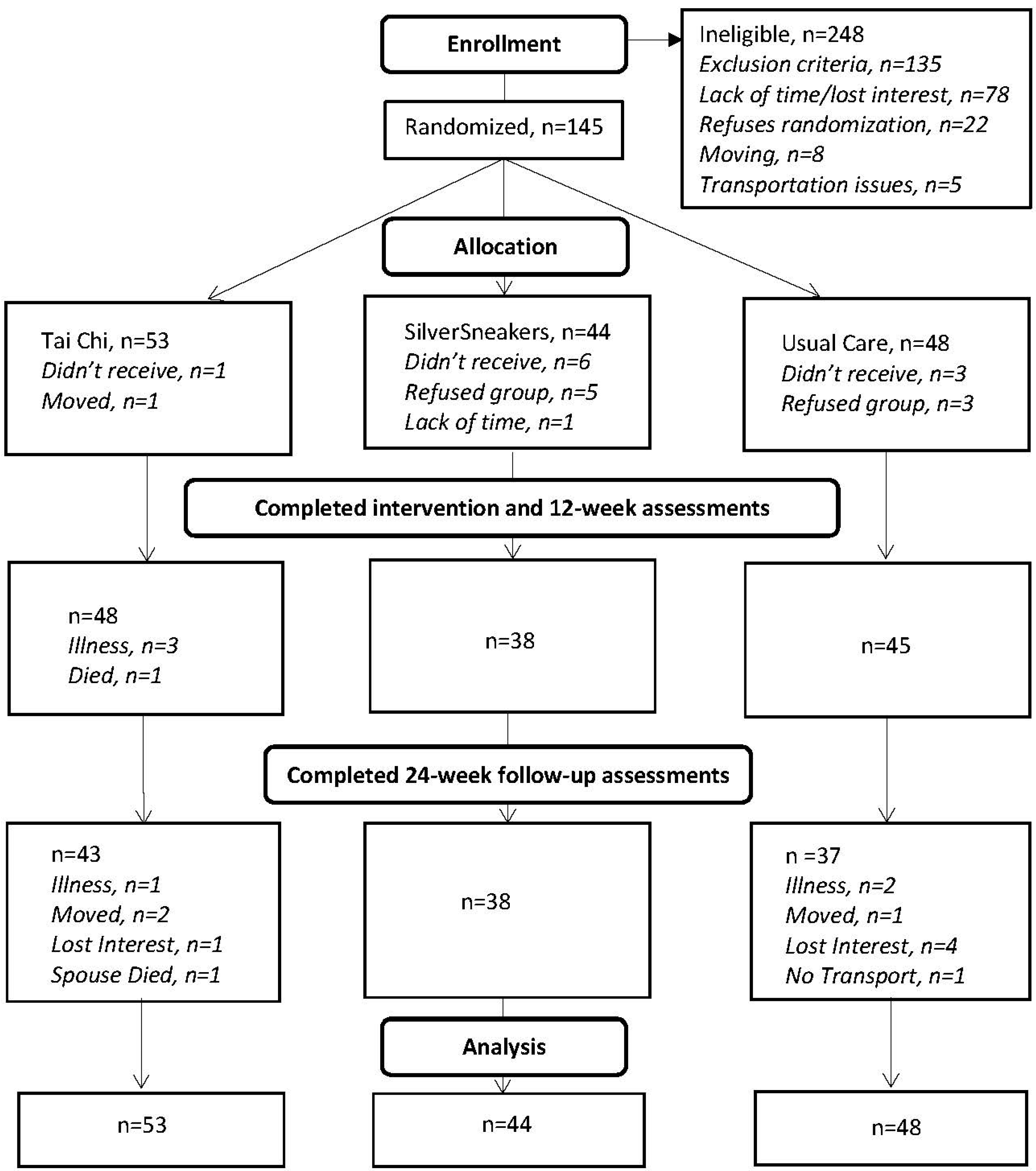
2.1. Study Background and Participants
2.2. Study Measures
Pittsburgh Sleep Quality Index (PSQI)
2.3. Statistical Analysis
3. Results
3.1. Study Sample
3.2. Sleep Quality Descriptives
3.3. Sleep Quality Group Comparisons
4. Discussion
Study Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Mixed Model Estimates of the Seven Components of the Pittsburgh Sleep Quality Index
| Sleep Quality Scores (PSQI) | Least Squares Means (SE) Physical Activity (n = 97) | Least Squares Means (SE) Control (n = 48) | Unadjusted Mean Difference (95% CI) | p-Value |
|---|---|---|---|---|
| Baseline | 0.94 (0.13) | 0.81 (0.18) | 0.13 (−0.31, 0.57) | 0.57 |
| 12 weeks | 0.91 (0.13) | 0.82 (0.18) | 0.10 (−0.35, 0.54) | 0.67 |
| 24 weeks | 0.91 (0.13) | 0.72 (0.18) | 0.19 (−0.25, 0.63) | 0.40 |
| Baseline-12 weeks | 0.02 (0.09) | −0.01 (0.13) | 0.03 (−0.28, 0.34) | 0.84 |
| Baseline-24 weeks | 0.02 (0.11) | 0.09 (0.15) | −0.06 (−0.43, 0.30) | 0.73 |
| Sleep Quality Scores (PSQI) | Least Squares Means (SE) Physical Activity (n = 97) | Least Squares Means (SE) Control (n = 48) | Unadjusted Mean Difference (95% CI) | p-Value |
|---|---|---|---|---|
| Baseline | 0.94 (0.09) | 0.96 (0.13) | −0.02 (−0.34, 0.30) | 0.90 |
| 12 weeks | 1.03 (0.09) | 0.81 (0.13) | 0.22 (−0.09, 0.53) | 0.16 |
| 24 weeks | 1.05 (0.10) | 0.92 (0.14) | 0.13 (−0.21, 0.47) | 0.45 |
| Baseline-12 weeks | −0.10 (0.09) | 0.15 (0.13) | −0.24 (−0.55, 0.07) | 0.12 |
| Baseline-24 weeks | −0.11 (0.10) | 0.04 (0.14) | −0.15 (−0.49, 0.18) | 0.37 |
| Sleep Quality Scores (PSQI) | Least Squares Means (SE) Physical Activity (n = 97) | Least Squares Means (SE) Control (n = 48) | Unadjusted Mean Difference (95% CI) | p-Value |
|---|---|---|---|---|
| Baseline | 0.41 (0.09) | 0.65 (0.13) | −0.24 (−0.54, 0.07) | 0.12 |
| 12 weeks | 0.45 (0.09) | 0.39 (0.12) | 0.06 (−0.24, 0.36) | 0.69 |
| 24 weeks | 0.42 (0.09) | 0.49 (0.13) | −0.07 (−0.39, 0.25) | 0.68 |
| Baseline-12 weeks | −0.05 (0.09) | 0.26 (0.13) | −0.30 (−0.62, 0.02) | 0.06 |
| Baseline-24 weeks | −0.02 (0.09) | 0.15 (0.12) | −0.17 (−0.47, 0.12) | 0.25 |
| Sleep Quality Scores (PSQI) | Least Squares Means (SE) Physical Activity (n = 97) | Least Squares Means (SE) Control (n = 48) | Unadjusted Mean Difference (95% CI) | p-Value |
|---|---|---|---|---|
| Baseline | 0.70 (0.11) | 0.90 (0.15) | −0.19 (−0.56, 0.17) | 0.29 |
| 12 weeks | 0.80 (0.11) | 0.75 (0.16) | 0.05 (−0.33, 0.43) | 0.80 |
| 24 weeks | 0.70 (0.11) | 0.85 (0.16) | −0.15 (−0.54, 0.23) | 0.43 |
| Baseline-12 weeks | −0.10 (0.12) | 0.15 (0.16) | −0.24 (−0.64, 0.15) | 0.22 |
| Baseline-24 weeks | 0.00 (0.12) | 0.04 (0.18) | −0.04 (−0.47, 0.39) | 0.85 |
| Sleep Quality Scores (PSQI) | Least Squares Means (SE) Physical Activity (n = 97) | Least Squares Means (SE) Control (n = 48) | Unadjusted Mean Difference (95% CI) | p-Value |
|---|---|---|---|---|
| Baseline | 1.34 (0.06) | 1.42 (0.09) | −0.08 (−0.29, 0.14) | 0.48 |
| 12 weeks | 1.34 (0.06) | 1.50 (0.08) | −0.15 (−0.35, 0.05) | 0.14 |
| 24 weeks | 1.46 (0.07) | 1.39 (0.10) | 0.07 (−0.17, 0.30) | 0.58 |
| Baseline-12 weeks | 0.00 (0.07) | −0.08 (0.09) | 0.07 (−0.15, 0.30) | 0.51 |
| Baseline-24 weeks | −0.12 (0.07) | 0.02 (0.10) | −0.14 (−0.38, 0.10) | 0.24 |
| Sleep Quality Scores (PSQI) | Least Squares Means (SE) Physical Activity (n = 97) | Least Squares Means (SE) Control (n = 48) | Unadjusted Mean Difference (95% CI) | p-Value |
|---|---|---|---|---|
| Baseline | 0.22 (0.07) | 0.35 (0.09) | −0.14 (−0.36, 0.09) | 0.23 |
| 12 weeks | 0.17 (0.07) | 0.34 (0.09) | −0.18 (−0.40, 0.04) | 0.12 |
| 24 weeks | 0.32 (0.07) | 0.14 (0.10) | 0.18 (−0.06, 0.41) | 0.14 |
| Baseline-12 weeks | 0.05 (0.06) | 0.01 (0.08) | 0.04 (−0.18, 0.25) | 0.72 |
| Baseline-24 weeks | −0.10 (0.06) | 0.21 (0.09) | −0.31 (−0.54, −0.09) | 0.01 |
| Sleep Quality Scores (PSQI) | Least Squares Means (SE) Physical Activity (n = 97) | Least Squares Means (SE) Control (n = 48) | Unadjusted Mean Difference (95% CI) | p-Value |
|---|---|---|---|---|
| Baseline | 1.27 (0.09) | 1.33 (0.12) | −0.07 (−0.37, 0.23) | 0.67 |
| 12 weeks | 1.25 (0.08) | 1.18 (0.12) | 0.07 (−0.21, 0.36) | 0.62 |
| 24 weeks | 1.19 (0.10) | 1.27 (0.14) | −0.09 (−0.42, 0.25) | 0.61 |
| Baseline-12 weeks | 0.02 (0.09) | 0.16 (0.12) | −0.14 (−0.44, 0.17) | 0.38 |
| Baseline-24 weeks | 0.08 (0.10) | 0.06 (0.14) | 0.02 (−0.32, 0.36) | 0.91 |
References
- Chandra, A.; Stone, C.R.; Du, X.; Li, W.A.; Huber, M.; Bremer, R.; Geng, X.; Ding, Y. The cerebral circulation and cerebrovascular disease III: Stroke. Brain Circ. 2017, 3, 66–77. [Google Scholar] [PubMed]
- Collaborators, G.B.D.S. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar]
- Rajsic, S.; Gothe, H.; Borba, H.H.; Sroczynski, G.; Vujicic, J.; Toell, T.; Siebert, U. Economic burden of stroke: A systematic review on post-stroke care. Eur. J. Health Econ. 2019, 20, 107–134. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- Ezeugwu, V.E.; Manns, P.J. Sleep Duration, Sedentary Behavior, Physical Activity, and Quality of Life after Inpatient Stroke Rehabilitation. J. Stroke Cerebrovasc. Dis. 2017, 26, 2004–2012. [Google Scholar] [CrossRef] [PubMed]
- Lui, S.K.; Nguyen, M.H. Elderly Stroke Rehabilitation: Overcoming the Complications and Its Associated Challenges. Curr. Gerontol. Geriatr. Res. 2018, 2018, 9853837. [Google Scholar] [CrossRef] [PubMed]
- Mutai, H.; Furukawa, T.; Araki, K.; Misawa, K.; Hanihara, T. Long-term outcome in stroke survivors after discharge from a convalescent rehabilitation ward. Psychiatry Clin. Neurosci. 2013, 67, 434–440. [Google Scholar] [CrossRef]
- Tang, W.K.; Lau, C.G.; Mok, V.; Ungvari, G.S.; Wong, K.S. Apathy and health-related quality of life in stroke. Arch. Phys. Med. Rehabil. 2014, 95, 857–861. [Google Scholar] [CrossRef]
- Khot, S.P.; Morgenstern, L.B. Sleep and Stroke. Stroke 2019, 50, 1612–1617. [Google Scholar] [CrossRef]
- Iddagoda, M.T.; Inderjeeth, C.A.; Chan, K.; Raymond, W.D. Post-stroke sleep disturbances and rehabilitation outcomes: A prospective cohort study. Intern. Med. J. 2020, 50, 208–213. [Google Scholar] [PubMed]
- Kredlow, M.A.; Capozzoli, M.C.; Hearon, B.A.; Calkins, A.W.; Otto, M.W. The effects of physical activity on sleep: A meta-analytic review. J. Behav. Med. 2015, 38, 427–449. [Google Scholar] [CrossRef]
- Cheng, H.P.; Chen, C.H.; Lin, H.S.; Wang, J.J.; Yen, M. Relationship between Walking Activity and Sleep Quality among Community-Dwelling Older Adults. J. Community Health Nurs. 2022, 39, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Wu, W.; Zou, Y.; Huang, W.; Lin, S.; Ye, J.; Lan, Y. Benefits of different combinations of aerobic and resistance exercise for improving plasma glucose and lipid metabolism and sleep quality among elderly patients with metabolic syndrome: A randomized controlled trial. Endocr. J. 2022, 69, 819–830. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- Taylor-Piliae, R.E.; Hoke, T.M.; Hepworth, J.T.; Latt, L.D.; Najafi, B.; Coull, B.M. Effect of Tai Chi on physical function, fall rates and quality of life among older stroke survivors. Arch. Phys. Med. Rehabil. 2014, 95, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Piliae, R.E.; Boros, D.; Coull, B.M. Strategies to improve recruitment and retention of older stroke survivors to a randomized clinical exercise trial. J. Stroke Cerebrovasc. Dis. 2014, 23, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Lan, C.; Chen, S.Y.; Lai, J.S.; Wong, A.M. Tai chi chuan in medicine and health promotion. Evid. Based Complement. Alternat. Med. 2013, 2013, 502131. [Google Scholar] [CrossRef]
- Nguyen, H.Q.; Ackermann, R.T.; Maciejewski, M.; Berke, E.; Patrick, M.; Williams, B.; LoGerfo, J.P. Managed-Medicare health club benefit and reduced health care costs among older adults. Prev. Chronic Dis. 2008, 5, A14. [Google Scholar] [PubMed]
- Taylor-Piliae, R.E.; Coull, B.M. Community-based Yang-style Tai Chi is safe and feasible in chronic stroke: A pilot study. Clin Rehabil. 2012, 26, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Lan, C.; Chen, S.Y.; Lai, J.S. Relative exercise intensity of Tai Chi Chuan is similar in different ages and gender. Am. J. Chin. Med. 2004, 32, 151–160. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R., Jr.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 Compendium of Physical Activities: A second update of codes and MET values. Med. Sci. Sports Exerc 2011, 43, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Carpenter, J.S.; Andrykowski, M.A. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J. Psychosom. Res. 1998, 45, 5–13. [Google Scholar] [CrossRef]
- Backhaus, J.; Junghanns, K.; Broocks, A.; Riemann, D.; Hohagen, F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J. Psychosom. Res. 2002, 53, 737–740. [Google Scholar] [CrossRef]
- Mallinckrod†, C.H.; Lane, P.W.; Schnell, D.; Peng, Y.; Mancuso, J.P. Recommendations for the Primary Analysis of Continuous Endpoints in Longitudinal Clinical Trials. Drug Inf. J. 2008, 42, 303–319. [Google Scholar] [CrossRef]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Zimet, G.D.; Powell, S.S.; Farley, G.K.; Werkman, S.; Berkoff, K.A. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 1990, 55, 610–617. [Google Scholar] [CrossRef]
- Bell, M.L.; Fairclough, D.L. Practical and statistical issues in missing data for longitudinal patient-reported outcomes. Stat. Methods Med. Res. 2014, 23, 440–459. [Google Scholar] [CrossRef]
- Molenberghs, G.; Thijs, H.; Jansen, I.; Beunckens, C.; Kenward, M.G.; Mallinckrodt, C.; Carroll, R.J. Analyzing incomplete longitudinal clinical trial data. Biostatistics 2004, 5, 445–464. [Google Scholar] [CrossRef] [PubMed]
- Mallinckrodt, C.; Lipkovich, I. Analyzing Longitudinal Clinical Trial Data: A Practical Guide; Chapman and Hall/CRC: Boca Raton, FL, USA, 2016. [Google Scholar]
- Ashbeck, E.L.; Bell, M.L. Single time point comparisons in longitudinal randomized controlled trials: Power and bias in the presence of missing data. BMC Med. Res. Methodol. 2016, 16, 43. [Google Scholar] [CrossRef]
- Amiri, S.; Hasani, J.; Satkin, M. Effect of exercise training on improving sleep disturbances: A systematic review and meta-analysis of randomized control trials. Sleep Med. 2021, 84, 205–218. [Google Scholar] [CrossRef] [PubMed]
- Du, S.; Dong, J.; Zhang, H.; Jin, S.; Xu, G.; Liu, Z.; Chen, L.; Yin, H.; Sun, Z. Taichi exercise for self-rated sleep quality in older people: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2015, 52, 368–379. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Chen, J.; Xu, G.; Duan, Y.; Huang, D.; Tang, C.; Liu, J. The Effect of Tai Chi for Improving Sleep Quality: A Systematic Review and Meta-analysis. J. Affect. Disord. 2020, 274, 1102–1112. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Sawada, M.; Noriyama, Y.; Arita, K.; Ota, T.; Sadamatsu, M.; Kiyotou, R.; Hirai, M.; Kishimoto, T. Tai Chi exercise versus rehabilitation for the elderly with cerebral vascular disorder: A single-blinded randomized controlled trial. Psychogeriatrics 2010, 10, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, A.I.; Pulsford, R.; Poltawski, L.; Forster, A.; Taylor, R.S.; Spencer, A.; Hollands, L.; James, M.; Allison, R.; Norris, M.; et al. Physical activity, sleep, and fatigue in community dwelling Stroke Survivors. Sci. Rep. 2018, 8, 7900. [Google Scholar] [CrossRef]
- Grandner, M.A.; Rosenberger, M.E. Actigraphic sleep tracking and wearables: Historical context, scientific applications and guidelines, limitations, and considerations for commercial sleep devices. In Sleep and Health; Grandner, M.A., Ed.; Academic Press: Cambridge, MA, USA, 2019; pp. 147–157. [Google Scholar]
| Characteristic | Physical Activity Intervention, n = 97 | Controls, n = 48 | p-Value # |
|---|---|---|---|
| Age, mean years (SD) | 70.8 (9.9) | 68.3 (10.3) | 0.16 |
| Women, n (%) | 43 (44.3) | 25 (52.1) | 0.38 |
| Marital Status, n (%) | 0.005 | ||
| Married/partner | 64 (66.0) | 20 (41.7) | |
| Single/divorced/widowed | 33 (34.0) | 28 (58.3) | |
| Employment Status, n (%) | 0.04 | ||
| Retired | 83 (85.6) | 33 (68.8) | |
| Full or Part-Time | 5 (5.2) | 8 (16.7) | |
| Unemployed | 9 (9.3) | 7 (14.6) | |
| Income, n (%) | 0.97 | ||
| <$50,000 per year | 79 (81.4) | 35 (72.9) | |
| ≥$50,000 per year | 18 (18.6) | 13 (27.1) | |
| Race/Ethnicity, n (%) | 0.01 | ||
| White/European-American | 82 (84.5) | 32 (66.7) | |
| Other * | 15 (15.5) | 16 (33.3) | |
| Self-Reported Health Problems, n (%) | |||
| Hypertension | 71 (73.2) | 35 (72.9) | 0.97 |
| Dyslipidemia | 61 (62.9) | 30 (62.5) | 0.96 |
| Diabetes | 29 (30.0) | 11 (22.9) | 0.38 |
| Arrhythmia | 26 (26.8) | 15 (31.3) | 0.58 |
| Major Depression | 15 (15.5) | 9 (18.8) | 0.62 |
| Asthma | 11 (11.3) | 7 (14.6) | 0.58 |
| Chronic Heart Failure | 11 (11.3) | 11 (23.4) | 0.06 |
| Previous Myocardial Infarction | 15 (15.5) | 7 (14.6) | 0.88 |
| Current Smoker | 4 (4.1) | 7 (14.6) | 0.03 |
| Sleep Quality | |||
| PSQI score, median (range = 0–21) | 6.2 (3–8) | 7.3 (4–11.5) | 0.13 |
| Poor Sleep Quality (PSQI > 5), n (%) | 47 (48.5) | 27 (56.3) | 0.38 |
| Sleep Time, mean hours/day (SD) | 7.5 (1.5) | 7.2 (1.9) | 0.25 |
| Baseline | 12-Weeks | 24-Weeks | ||||
|---|---|---|---|---|---|---|
| Physical Activity, n = 94 | Controls, n = 48 | Physical Activity, n = 85 | Controls, n = 45 | Physical Activity, n = 80 | Controls, n = 38 | |
| PSQI total score, mean (SD) | 5.69 (3.04) | 6.42 (4.11) | 5.88 (3.54) | 5.82 (3.73) | 6.03 (3.45) | 5.71 (3.70) |
| PSQI component scores, mean (SD) | ||||||
| subjective quality | 0.94 (1.27) | 0.81 (1.25) | 0.88 (1.27) | 0.84 (1.26) | 0.93 (1.27) | 0.74 (1.11) |
| latency | 0.94 (0.89) | 0.94 (0.89) | 1.04 (0.85) | 0.82 (0.91) | 1.06 (0.90) | 0.89 (0.89) |
| duration | 0.41 (0.76) | 0.65 (1.06) | 0.47 (0.88) | 0.40 (0.75) | 0.44 (0.82) | 0.47 (0.95) |
| efficiency | 0.70 (0.97) | 0.90 (1.17) | 0.80 (1.09) | 0.76 (1.00) | 0.70 (1.00) | 0.82 (1.01) |
| disturbances | 1.34 (0.59) | 1.42 (0.65) | 1.33 (0.54) | 1.49 (0.59) | 1.45 (0.61) | 1.37 (0.63) |
| medication use | 0.22 (0.58) | 0.35 (0.76) | 0.15 (0.50) | 0.33 (0.77) | 0.29 (0.68) | 0.13 (0.34) |
| daytime dysfunction | 1.27 (0.81) | 1.33 (0.95) | 1.24 (0.80) | 1.18 (0.78) | 1.16 (0.82) | 1.29 (0.96) |
| Sleep Quality Scores (PSQI) | Least Squares Means (SE) Physical Activity (n = 97) | Least Squares Means (SE) Control (n = 48) | Unadjusted Mean Difference (95% CI) | p-Value | Adjusted a Mean Difference (95% CI) | p-Value |
|---|---|---|---|---|---|---|
| Baseline | 5.67 (0.35) | 6.42 (0.50) | −0.74 (−1.94, 0.46) | 0.22 | −0.41 (−1.65, 0.82) | 0.51 |
| 12 weeks | 5.88 (0.38) | 5.79 (0.52) | 0.09 (−1.18, 1.36) | 0.89 | 0.32 (−0.95, 1.59) | 0.62 |
| 24 weeks | 6.03 (0.38) | 5.75 (0.55) | 0.28 (−1.04, 1.60) | 0.67 | 0.66 (−0.73, 2.04) | 0.35 |
| Baseline-12 weeks | −0.20 (0.31) | 0.63 (0.43) | −0.83 (−1.89, 0.23) | 0.12 | −0.73 (−1.72, 0.25) | 0.14 |
| Baseline-24 weeks | −0.36 (0.32) | 0.66 (0.45) | −1.02 (−2.12, 0.07) | 0.07 | −1.07 (−2.19, 0.05) | 0.06 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marupuru, S.; Bell, M.L.; Grandner, M.A.; Taylor-Piliae, R.E. The Effect of Physical Activity on Sleep Quality among Older Stroke Survivors: Secondary Analysis from a Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 13320. https://doi.org/10.3390/ijerph192013320
Marupuru S, Bell ML, Grandner MA, Taylor-Piliae RE. The Effect of Physical Activity on Sleep Quality among Older Stroke Survivors: Secondary Analysis from a Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(20):13320. https://doi.org/10.3390/ijerph192013320
Chicago/Turabian StyleMarupuru, Srujitha, Melanie L. Bell, Michael A. Grandner, and Ruth E. Taylor-Piliae. 2022. "The Effect of Physical Activity on Sleep Quality among Older Stroke Survivors: Secondary Analysis from a Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 20: 13320. https://doi.org/10.3390/ijerph192013320
APA StyleMarupuru, S., Bell, M. L., Grandner, M. A., & Taylor-Piliae, R. E. (2022). The Effect of Physical Activity on Sleep Quality among Older Stroke Survivors: Secondary Analysis from a Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(20), 13320. https://doi.org/10.3390/ijerph192013320







